Abstract
Purpose
The purpose was to examine the characteristics of children who use hospice care.
Design and Methods
Using the Andersen Model of Health Services Use, California Medicaid administrative databases were analyzed to describe the characteristics of 76 children in hospice.
Results
The predisposing, enabling, and need characteristics of children were identified. Children who used hospice were a diverse group with community resources that enable them to access care, while presenting with serious health needs. Children enrolled in hospice were more likely older (15–20 years of age), resided nearer a pediatric hospice, and had a serious health condition such as neuromuscular disease with multiple comorbidities.
Practice Implications
With this knowledge, pediatric nurses can improve their clinical practice by targeting conversations with families and children most in need of hospice care.
In the United States, there are approximately 44,000 pediatric deaths each year (Hamilton et al., 2013). Many of these children die with a serious health condition and yet, are never enrolled in hospice care. In fact, fewer than 10% of children utilize hospice at end of life (Lindley & Lyon, 2013). Pediatric hospice care is medical and supportive care services for dying children and their families that is delivered by a multidisciplinary team of clinicians in the home, hospital, or dedicated facility (Institute of Medicine, 2003). The physical and psychosocial benefits to using pediatric hospice care at end of life are documented (Dickens, 2010) and supported by the Institute of Medicine (2003), American Academy of Pediatricians (2013), and the National Association of Neonatal Nurses (2010).
The decision to enroll in pediatric hospice is, however, often complicated by families’ acceptance of death and clinicians’ knowledge of hospice and ability to assess the last 6 months of life (Dabbs et al., 2007; Davies et al., 2008). However, there is emerging evidence that the characteristics of the child may also influence whether or not they are enrolled in hospice care (Lyon et al., 2008; Knapp et al., 2009; Thienprayoon et al., 2013). For example, demographics factors such as the child’s gender and age may represent biological imperatives that influence the use of pediatric hospice care. At the same time, children and families with available pediatric hospice providers in their community may be more likely to enroll in pediatric hospice care than children who lack those resources in their community. Furthermore, health conditions with a defined disease trajectory such as cancer may enable clinicians to estimate the last 6 months of life required for hospice enrollment. Understanding the children who use hospice care services is important, if utilization of pediatric hospice care is to expand. Therefore, the purpose of this study was to examine the characteristics of children utilizing hospice care.
Conceptual Framework
Drawing on the literature from adult and pediatric hospice studies, this study used a conceptual framework based on the Andersen Behavioral Healthcare Utilization Model to explain the relationship between child characteristics and hospice use (Lindley, under review). The Andersen model was developed to assist in understanding why individuals use health services, to define and measure equitable access to health care, and to aide in developing policies to promote equitable access to care (Andersen, 1968). The Andersen model presupposed that health care utilization is a function of the disposition of an individual to use services (predisposing characteristics), factors that enable or impede use (enabling characteristics), and an individual’s need for services (need characteristics). These characteristics are considered the most immediate and important causes of health care utilization (Andersen, 1968).
Children are predisposed to using healthcare services based on demographics, family position within the social structure, and family beliefs in the benefits of health services. Evidence suggests that demographic factors influencing hospice use include gender (Hardy et al., 2011; Karikari-Martin et al., 2012; Keating et al., 2006; Knapp et al., 2009; Mack et al., 2013) and age (Hardy et al., 2011; Karikari-Martin et al., 2012; Keating et al., 2006; 2007; Knapp et al., 2009; Lyon et al., 2008; Mack et al., 2013). In the Andersen model, social structures are a broad array of factors that determine the status of a person in the community often based on the racial and ethnic composition of a community (Andersen, 1968). Race and ethnicity were included in the model because a child’s and their family’s race and ethnicity may represent social supports that influence pediatric hospice use (Colon et al., 2003; Givens et al., 2010; Hardy et al., 2011; Karikari-Martin et al., 2012; Ngo-Metzger et al., 2008). Health beliefs include attitudes, values, and knowledge that children and families have about health and health services, which influence their use of health services. Although there is limited evidence, previous experience of the child and family with long-term care, including home health experience, may facilitate enrollment into hospice care for children.
In addition, family and community enabling resources must be present in order for children and families to use health services. An important family resource that enables families to pay for health care utilization, including hospice care, is health insurance (McCarthy et al., 2003; Mack et al., 2013; Thienprayoon et al., 2013). The model suggests that Medicaid eligibility type and private insurance were related to pediatric hospice use. Children and families must also have access to pediatric hospice providers in their community. In other words, health care services must be available and accessible to people where they live and people must have a means and know-how to get to these services (Carlson et al., 2010; Jenkins et al., 2009; Madigan et al., 2009; Virnig et al., 2006). Thus, community hospice resources were included in the model.
Finally, there must be a need to use the health service, in order for it to be used. Establishing a need for health care services may be based on professional judgment about the child’s health. There is a general consensus in the literature that clinically-evaluated need for hospice care is driven by the child’s diagnosis (Hardy et al., 2001; Jenkins et al., 2009; Keating et al., 2006; 2007; Knapp et al., 2009; Mack et al., 2013; McCarthy et al., 2003; Ngo-Metzger et al., 2008; Ramsey & Chin, 2012; Thienprayoon et al., 2013). A need for health care services may also be based on how children and their families view the child’s health, so comorbidities was included in the model (Keating et al., 2006; 2007; Mack et al., 2013).
Methods
Design and Data Sources
Two administrative data sets were used in this secondary, descriptive study: the California Medicaid program’s Medicaid Analytic Extract files and the California Office of Statewide Health Planning and Development State Utilization Data File of Home Health Agencies and Hospice Facilities. The 2007 and 2008 Medicaid Analytic Extract files consist of individual records for those enrolled in the California Medicaid program (Hennessy et al., 2007). The data, which are the most current available, contain eligibility information, summary claims, payment data, and detail data on services, payment, and diagnoses. The Medicaid data set is compiled and administered by the Center for Medicare and Medicaid Services.
The 2007 and 2008 State Utilization Data File of Home Health Agencies and Hospice Facilities were publicly available from the California Office of Statewide Health Planning and Development (California Office of Statewide Health Planning and Development, 2006). The files contain survey data on hospices and home health agencies licensed in the state of California. Agency administrators were asked a list of questions about organizational demographics, services, patients, payment sources, and financials. California was selected for the study because it had the largest number of children enrolled in Medicaid (Kaiser Family Foundation, 2012). Data from 2007 and 2008 were used because 2007 was the first year the Medicaid files included the Social Security Administration date of death.
Sample
There were 3,162 children who met the study eligibility criteria: children between the ages of 0 to 20 years, decedents who died between January 1, 2007 and December 31, 2008, and children who were enrolled in the California Medicaid program for any part of their last year of life. Children were included if they used hospice care during the study time period. Duplicates and children who were not California residents were excluded from the sample. Children who died from an accident or injury were also excluded. The final sample size was 76 children. The University of Tennessee at Knoxville Institutional Review Board reviewed and approved this study.
Measures
Groups of variables were created based on the conceptual framework: predisposing, enabling, and need characteristics.
Predisposing characteristics
Demographic characteristics of the child included age at death and gender. Age was categorized in the Medicaid data as less than 1 year, 1 to 5 years, 6 to 15 years, and 15 to 20 years. A binary variable was created for gender (0 = male, 1 = female). Social support was operationalized as race and ethnicity. Categories were created for Caucasian, Hispanic, and other races (e.g., Asian American, African American, Native American). Healthcare knowledge was defined as whether or not the family had experience with home health care prior to the hospice admission.
Enabling characteristics
Family resources included two variables. First, the child’s Medicaid eligibility type was operationalized as whether or not a child was eligible for Medicaid coverage because of their disability status. Second, whether or not the family had private health insurance, along with the child’s Medicaid coverage. A community resource variable was created using geocoded child (i.e., county of residence) and hospice (i.e., latitude and longitude coordinates) data for pediatric hospice resource. Pediatric hospice resources was defined geographically as whether the child resided in the California county of a community-based pediatric hospice provider.
Need characteristics
The clinically-evaluated need for hospice care was defined as the child’s diagnosis. A binary variable was created for each of the following complex chronic conditions: neuromuscular (brain/spinal cord malformation, intellectual disability, CNS disease, cerebral palsy, epilepsy, muscular dystrophy), cardiovascular (heart malformations, cardiomyopathies, and dysrhythmias), cancer, congenital anomalies (chromosomal abnormalities, bone/joint abnormalities, diaphragm/abdominal abnormalities, other abnormalities) (Feudtner et al., 2001). For perceived need by the children and families for hospice care, the number of complex chronic conditions or comorbities was counted for each child and categorized them as 0–1, 2, and 3+.
Data Analysis
The primary aim of the study was to describe children who used hospice care. Using pooled, cross-sectional data, descriptive statistics including mean, frequency, minimum, and maximum were calculated for predisposing, enabling, and need characteristics. Descriptive analyses were conducted using Stata 11.0 (StataCorp LP, College Station, TX). Data analysis also includes visualization using ArcMap in ArcGIS version10.1 (ESRI, Redlands, CA) to create a map showing the pediatric hospice resources. Cloropleth mapping techniques were used to display the residential counties where children were enrolled in hospice care during the two-year study period. The cloropleth maps used shading to show county variation in the number of children enrolled in hospice care. Points on the map were used to illustrate the location of pediatric hospice care providers, in order to assess the presence of a community pediatric hospice resource. Reference points for the major metropolitan cities and state capital were also included on the map (i.e., San Diego, Los Angeles, San Jose, Sacramento).
Results
Predisposing characteristics
Table 1 displays the predisposing characteristics of the children. Although all age groups utilized hospice services, 15 to 20 year olds had the highest (29.0%) hospice use. Typically, more girls (54.0%) enrolled in hospice care compared to boys. Children who were Hispanic (39.5%) and other races (40.8%) predominantly utilized hospice care. Approximately a quarter (21.1%) of the sample had been admitted to home health care prior to their hospice enrollment.
Table 1.
Predisposing Characteristics of Children (N=76)
| Characteristics | n | Percentage |
|---|---|---|
| Demographics | ||
| Age | ||
| Less than 1 year | 16 | 21.05% |
| 1 to 5 years | 19 | 25.00% |
| 6 to 14 years | 19 | 25.00% |
| 15 to 20 years | 22 | 28.95% |
| Gender | ||
| Male | 35 | 46.05% |
| Female | 41 | 53.95% |
| Social Support | ||
| Race and Ethnicity | ||
| Caucasian | 12 | 15.79% |
| Hispanic | 30 | 39.47% |
| Other Race/Ethnicity | 34 | 44.74% |
| Health Care Knowledge | ||
| Home Health Experience | 16 | 21.05% |
Enabling Characteristics
The child’s enabling characteristics are indicated in Table 2. Children were generally eligible for Medicaid because of their nondisability status (71.1%), and 93.2% had no additional private health insurance coverage.
Table 2.
Enabling Characteristics of Children (N=76)
| Characteristics | n | Percentage |
|---|---|---|
| Family Resources | ||
| Medicaid Eligibility Type | ||
| Disabled | 22 | 28.95% |
| Not Disabled | 54 | 71.05% |
| Private Insurance | ||
| No | 71 | 93.42% |
Figure 1 displays the map of pediatric hospice resources in the community. California has 58 counties and children who utilized hospice care resided in 21 of the counties (36%) Seven counties had one child enrolled in hospice care. There were 10 counties where 2 to 5 children used hospice care. Counties with 6 to 15 children enrolled in hospice. In addition, pediatric hospice providers were present in 28 counties (48%). A majority of children (96%) in the study resided in a county with a pediatric hospice provider. There were 16 counties (28%), which were generally in major metropolitan areas, that had multiple hospices that provided care for children.
Figure 1.
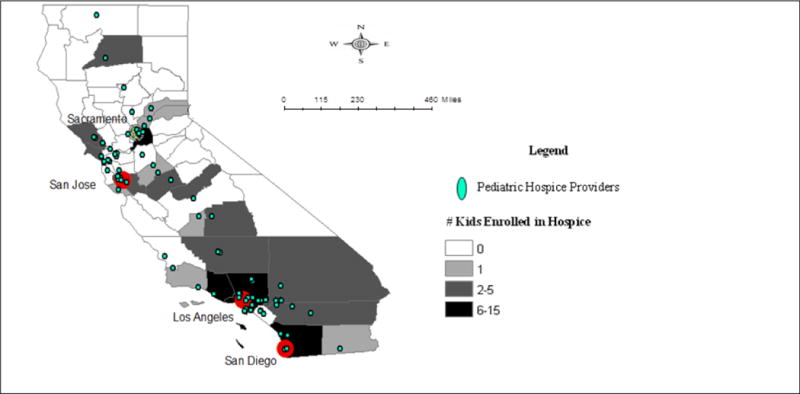
Pediatric Hospice Resources by County, 2007–2008
Need Characteristics
The need characteristics of children are summarized in Table 3. The children who used hospice were most often diagnosed with neuromuscular diseases (54.0%) and infrequently with congenital problems (17.1%). Cancer diagnoses were present in 42.1% of the children, followed by cardiovascular (27.6%). A majority of children had multiple comorbidities (54.0%). It was common for the children in the sample to have at least two complex chronic conditions (31.6%).
Table 3.
Need Characteristics of Children (N=76)
| Characteristics | n | Percentage |
|---|---|---|
| Clinically Evaluated Need | ||
| Diagnosis | ||
| Neuromuscular | 41 | 53.95% |
| Cardiovascular | 21 | 27.63% |
| Cancer | 32 | 42.11% |
| Congenital | 13 | 17.11% |
| Perceived Need | ||
| Comorbities | ||
| 0–1 | 35 | 46.05% |
| 2 | 24 | 31.58% |
| 3+ | 17 | 22.37% |
Discussion
The goal of this study was to examine the characteristics of children who utilized hospice care. Using the Andersen Behavioral Model of Health Service Use as a guide, the study sought to describe the predisposing, enabling, and need characteristics of children. This study showed that children who use hospice are a diverse group with community resources that enable them to access care, while presenting with serious health needs.
Predisposing Characteristics
This study found that most children in the sample were adolescent girls from other racial/ethnic backgrounds such as Asian American and Native American. An interesting finding was that children enrolled in hospice were generally between the ages of 15 and 20 years. This was consistent with national reports and the other researchers who also found that children above 15 years were more commonly enrolled in hospice care compared to younger children (Knapp et al., 2009; Lyon et al., 2008; National Hospice and Palliative Care Organization, 2009), and it suggests adolescents may be more predisposed to using hospice care. One possible explanation is that adolescents may be more likely to share their thoughts and feelings about end-of-life care, compared to younger children (Lyon et al., 2004), and ultimately establish advanced care planning that includes decisions about hospice care (Lyon et al., 2013). Alternatively, hospices may have the ability to provide care to older children. Hospices may have adult equipment and supplies readily available that can be used in the care of these older children (Orloff, 2001), and their staff (i.e., nurses, physicians) may be able to translate their knowledge of adult hospice care to this age group more easily, as compared to toddlers and infants (Lindley et al., 2012). Future research might continue to explore the differences in hospice use among age groups.
Enabling Characteristics
The study showed that children often resided in a county where pediatric hospice care was provided, which suggests that access to community resources may enable children and families to utilize hospice. This finding is consistent with adult hospice work of Jenkins et al. (2009) and Carlson et al. (2010), who found that most adults resided near a hospice. It may be possible that the recent growth in the hospice industry increased geographic accessibility to hospice care for children (Thompson et al., 2012). Additional research is required, however, to determine the extent to which the community hospice resources are available for children who do not enroll in hospice care.
Need Characteristics
The analysis also demonstrated that the need for hospice care was based on the child’s serious health condition at end of life. The results of this study suggest that clinically-evaluated need for hospice care may be greatest among children with neuromuscular health conditions. Contrary to other researchers, who have only examined cancer as a common diagnosis among patients who used hospice (Thienprayoon et al., 2013: Mack et al., 2013: Ramsey et al., 2012; Hardy et al., 2011), the study revealed that children in hospice care often had neuromuscular conditions such as cerebral palsy, muscular dystrophy, and brain/spinal cord malformation. The findings are also contrary to industry reports that showed neuromuscular conditions second to cancer in the cause of pediatric deaths (National Hospice and Palliative Care Organization, 2009), and vital statistics data that reported cerebrovascular disease was the sixth most common cause of death among children (Hamilton et al., 2013). It may be that specialists or pediatricians who care for children with neuromuscular conditions have an understanding of pediatric hospice and are more likely to refer patients to hospice than specialists in other fields (Thompson et al., 2009). Additional research in the referral patterns of pediatric specialists is warranted to better understand why children with certain health conditions may not be using hospice care.
This study also found that children using hospice care predominately had multiple comorbities, which are additional health conditions a child may have, along with their primary diagnosis. The finding that 54% of the children in the sample had 2 or more complex chronic conditions suggests a medically-fragile child. Several researchers have noted that patients enrolled in hospice frequently have multiple comorbities, which may represent a significant need for hospice care as multiple body functions begin to fail at end of life (Keating et al., 2006; 2007; Mack et al., 2013; Givens et al., 2010).
There are several limitations to this study. First, this was an analysis of fee-for-service Medicaid patients, so the findings are not generalizable to other insurance types. Results may differ for children enrolled in private insurance or uninsured. Second, this study focused on California. Although California has the highest number of children enrolled in Medicaid (Kaiser Family Foundation, 2012), a study of one state limits generalizability of the findings to other states. Third, there is a potential for selection bias associated with infant enrollment into Medicaid. The paper work requirement for Medicaid enrollment coupled with the short lifespan of infants may limit the number of infants enrolled in Medicaid, even though they consistently have the highest mortality rate among children (Hamilton et al., 2013).
How might this information affect nursing practice?
Despite the study limitations, the study has clinical implications for pediatric nurses caring for seriously-ill children. Understanding who uses hospice care may assist advanced practice nurses in identifying patients in their clinical practice who might benefit from hospice care. Nurse can use this information to target educational opportunities with the medical team, child, and family. For example, families and children with serious neuromuscular conditions might benefit from a conversation about advanced care planning and how hospice care might fit the needs and wishes of the child and family in that advanced care plan. Information on conducting these conversations can be found on the National Institute of Nursing Research website (http://www.ninr.nih.gov/newsandinformation/conversationsmatter). Additional information on pediatric hospice care standards of practice (http://www.nhpco.org/quality/nhpco%E2%80%99s-standards-pediatric-care) and training resources (http://www.nhpco.org/education-online-learning/pediatric-care) is available through the National Hospice and Palliative Care Organization.
In conclusion, understanding who is using pediatric hospice care is essential for advancing knowledge and compassion among pediatric nurses. This study showed that children in hospice care were generally predisposed based on age and race/ethnicity, were enabled to use hospice because of family and community resources, and often had a need for hospice because of the medical condition. With this knowledge, pediatric nurses can improve their clinical practice by targeting conversations with families and children most in need of hospice care. Ultimately, the knowledge of who is using hospice care should improve care for children and their families at end of life.
Acknowledgments
Special thanks to Beth Schewe for her assistance with the manuscript.
Funding: This publication was made possible by Grant Number K01NR014490 from the National Institute of Nursing Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Nursing Research or National Institutes of Health.
Footnotes
Conflict of Interest: The authors report no actual or potential conflicts of interests.
References
- Andersen R. A behavioral model of families’ use of health services. Chicago, IL: Center for Health Administration Studies; 1968. [Google Scholar]
- American Academy of Pediatrics. Policy statement: Pediatric palliative care and hospice care commitments, guidelines, and recommendations. Pediatrics. 2013;132:996–72. doi: 10.1542/peds.2013-2731. [DOI] [PubMed] [Google Scholar]
- California Office of Statewide Health Planning & Development. Documentation: The state utilization data file of home health agency and hospice facilities, calendar year 2006. Sacramento, CA: Health Information Resource Center; 2006. [Google Scholar]
- Carlson M, Bradley E, Du Q, Morrison RS. Geographic access to hospice in the United States. Journal of Palliative Medicine. 2010;13:1331–1338. doi: 10.1089/jpm.2010.0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colon M, Lyke J. Comparison of hospice use by European Americans, African Americans, and Latinos: A follow-up study. American Journal of Hospice and Palliative Medicine. 2013 doi: 10.1177/1049909113511143. Epub. [DOI] [PubMed] [Google Scholar]
- Dabbs D, Butterworth L, Hall E. Tender mercies: Increasing access to hospice services for children with life-threatening conditions. The American Journal of Maternal Child Nursing. 2007;32(5):311–319. doi: 10.1097/01.NMC.0000288003.10500.00. [DOI] [PubMed] [Google Scholar]
- Davies B, Sehring SA, Partridge J, Cooper B, Hughes A, Philp JC, Amidi-Nouri A, Kramer RF. Barriers to palliative care for children: Perceptions of pediatric health care providers. Pediatrics. 2008;121(2):282–288. doi: 10.1542/peds.2006-3153. [DOI] [PubMed] [Google Scholar]
- Dickens DS. Comparing pediatric deaths with and without hospice support. Pediatric Blood Cancer. 2010;54(5):746–750. doi: 10.1002/pbc.22413. [DOI] [PubMed] [Google Scholar]
- Givens JL, Tjia J, Zhou C, Emanuel E, Ash AS. Racial and ethnic differences in hospice use among patients with heart failure. Archives of Internal Medicine. 2010;170:427–432. doi: 10.1001/archinternmed.2009.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton BE, Hoyert DL, Martin JA, Strobino DM, Guyer B. Annual summary of vital statistics: 2010–2011. Pediatrics. 2013;131(3):548–558. doi: 10.1542/peds.2012-3769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy D, Chan W, Liu C, Cormier JN, Xia R, Bruera E, Du XL. Racial disparities in the use of hospice services according to geographic residence and socioeconomic status in an elderly cohort with non-small cell lung cancer. Cancer. 2011;117(7):1506–1515. doi: 10.1002/cncr.25669. [DOI] [PubMed] [Google Scholar]
- Hennessy S, Leonard CE, Palumbo CM, Newcomb C, Bilker WB. Quality of Medicaid and Medicare data obtained through Centers for Medicare and Medicaid Services (CMS) Medical Care. 2007;45(12):1216–1220. doi: 10.1097/MLR.0b013e318148435. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. When children die: Improving palliative and end-of-life care for children and their families. Washington, D.C.: National Academy Press; 2003. [Google Scholar]
- Jenkins T, Chapman K, Harshbarger D, Townsend MS. Hospice use among cancer decedents in Alabama, 2002–2005. Preventing Chronic Disease. 2009;6:1–8. [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation. State Health Facts Online – Distribution of Medicaid Enrollees by Enrollment Group FY2009. 2012 Retrieved on August 24, 2012 from http://www.statehealthfacts.org/comparemaptable.jsp?ind=200&cat=4. Accessed August 24, 2012.
- Karikari-Martin P, McCann JJ, Hebert LE, Haffer SC, Phillips M. Do community and caregiver factors influence hospice use at the end of life among older adults with Alzheimer disease. Journal of Hospice and Palliative Nursing. 2012;14(3):225–237. doi: 10.1097/NJH.0b013e3182433a15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keating NL, Herrinton LJ, Zaslavsky AM, Liu L, Ayanian J. Variations in hospice use among cancer patients. Journal of the National Cancer Institute. 2006;98:1053–1059. doi: 10.1093/jnci/djj298. [DOI] [PubMed] [Google Scholar]
- Keating NL, Landrum MB, Guadagnoli E, Winer E, Avanian J. Care in the months before death and hospice enrollment among older women with advanced breast cancer. Journal of General Internal Medicine. 2007;23:11–18. doi: 10.1007/s11606-007-0422-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knapp C, Shenkman E, Marcu M, Madden V, Terza J. Pediatric palliative care: Describing hospice users and identifying factors that affect hospice expenditures. Journal of Palliative Medicine. 2009;12:1–7. doi: 10.1089/jpm.2009.9657. [DOI] [PubMed] [Google Scholar]
- Lindley LC. The development of a conceptual model for studying pediatric hospice use. Journal of Social Work in End-Of-Life & Palliative Care (Manuscript submitted for publication) [Google Scholar]
- Lindley LC, Lyon ME. A profile of children with complex chronic conditions at end of life among Medicaid-beneficiaries: Implications for healthcare reform. Journal of Palliative Medicine. 2013;16(11):1388–1393. doi: 10.1089/jpm.2013.0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley LC, Mixer S, Mack J. Profit status and the delivery of hospice care for infants: The mediating role of pediatric knowledge. Journal of Palliative Medicine. 2012;15(12):1369–1373. doi: 10.1089/jpm.2012.0214. [DOI] [PubMed] [Google Scholar]
- Lyon ME, Jacobs S, Briggs L, Cheng YI, Wang J. Family-centered advance care planning for teens with cancer. JAMA Pediatrics. 2013;167(5):460–467. doi: 10.1001/jamapediatrics.2013.943. [DOI] [PubMed] [Google Scholar]
- Lyon ME, McCabe MA, Patel KM, D’Angelo LJ. What do adolescents want? An exploratory study regarding end-of-life decision-making. Journal of Adolescent Health. 2004;35(6):529.e1–6. doi: 10.1016/j.jadohealth.2004.02.009. [DOI] [PubMed] [Google Scholar]
- Lyon M, Williams P, Woods E, Hutton N, Butler A, Siblinga E, Oleske JM. Do-not-resuscitate orders and/or hospice care, psychological health, and quality of life among children/adolescents with acquired immune deficiency syndrome. Journal of Palliative Medicine. 2008;11:459–469. doi: 10.1089/jpm.2007.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mack JW, Chen K, Boscoe FP, Gesten FC, Roohan PJ, Weeks JC, Schrag D. Underuse of hospice care by Medicaid-insured patients with stage IV lung cancer in New York and California. Journal of Clinical Oncology. 2013;31:2569–2579. doi: 10.1200/JCO.2012.45.9271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madigan EA, Wiencek CA, Vander Schrier AL. Patterns of community-based end-of-life care in rural areas of the united states. Policy, Politics, & Nursing Practice. 2009;10(1):71–81. doi: 10.1177/1527154409333861. [DOI] [PubMed] [Google Scholar]
- McCarthy EP, Burns RB, Ngo-Metzger Q, Davis RB, Phillips RS. Hospice use among Medicare managed care and fee-for-service patients dying with cancer. JAMA. 2003;289:2238–2245. doi: 10.1001/jama.289.17.2238. [DOI] [PubMed] [Google Scholar]
- National Association of Neonatal Nurses. Position statement: Palliative care for newborns and infants. 2010 doi: 10.1097/ANC.0b013e31820022a8. Retrieved on February 1, 2014 from http://www.nann.org/…/Palliative_Care-final2-in_new_template_01-07-11.pdf. [DOI] [PubMed]
- National Hospice & Palliative Care Organization. NHPCO facts and figures: Pediatric palliative and hospice care in America. 2009 Retrieved on January 10, 2014 from http://www.nhpco.org/files/public/quality/Pediatric_Facts-Figures.pdf.
- Ngo-Metzger Q, Phillips RS, McCarthy EP. Ethic disparities in hospice use among Asian-American and Pacific Islander patients dying with cancer. Journal of the American Geriatrics Society. 2008;56:139–144. doi: 10.1111/j.1532-5415.2007.01510.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orloff S. Incorporating children in an adult hospice program. In: Armstrong-Dailey A, Zarbock S, editors. Hospice care for children. Oxford: Oxford University press; 2001. pp. 353–377. [Google Scholar]
- Ramsey SJ, Chin SH. Disparity in hospice utilization by African American patients with cancer. American Journal of Hospice and Palliative Medicine. 2012;29:346–354. doi: 10.1177/1049909111423804. [DOI] [PubMed] [Google Scholar]
- Thienprayoon R, Lee SC, Leonard D, Winick N. Racial and ethnic difference in hospice enrollment among children with cancer. Pediatric Blood Cancer. 2013;60:1662–1666. doi: 10.1002/pbc.24590. [DOI] [PubMed] [Google Scholar]
- Thompson JW, Carlson MD, Bradley EH. US hospice industry experienced considerable turbulence from changes in ownership, growth, and shift to for-profit status. Health Affairs. 2012;31(6):1286–1293. doi: 10.1377/hlthaff.2011.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson LA, Knapp C, Madden V, Shenkman E. Pediatricians’ perceptions of and preferred timing for pediatric palliative care. Pediatrics. 2009;123(5):e777–782. doi: 10.1542/peds.2008-2721. [DOI] [PubMed] [Google Scholar]
- Virnig B, Ma H, Hartman L, Moscovice I, Carlin B. Access to home-based hospice care for rural populations: Identification of areas lacking service. Journal of Palliative Medicine. 2006;9:1292–1299. doi: 10.1089/jpm.2006.9.1292. [DOI] [PubMed] [Google Scholar]


