Abstract
Background: Balancing career and family obligations poses challenges to medical school faculty and contributes to dissatisfaction and attrition from academics. We examined the relationship between family setting and responsibilities, rank, and career and work–life satisfaction for faculty in a large U.S. medical school.
Methods: Baseline faculty surveys were analyzed from the first year of a 4-year National Institutes of Health–funded study to evaluate awareness, knowledge, attitudes, and use of family friendly policies and career satisfaction. The study focus was on the impact of family responsibilities and characteristics of the faculty position (rank, clinical vs. nonclinical, and academic series) in multivariate comparisons between primary predictors and outcomes of interest.
Results: Both clinical and family responsibilities for children under 18 play a major and interacting role in satisfaction with career and work–life balance. Clinical faculty respondents without children at home reported significantly greater career satisfaction and better work–life balance than their nonclinical counterparts. Nonclinical faculty respondents with children reported greater satisfaction and better balance than counterparts without family responsibilities. However, the advantage in career satisfaction and work–life balance for clinical faculty respondents disappeared for those with responsibility for young children. No gender-based differences were noted in the results or across faculty rank for respondents; however, for women, reaching associate professor resulted in greater career satisfaction.
Conclusion: This study suggests that both work-related factors and family responsibilities influence satisfaction with career and work–life balance, but the predictors appear to interact in complex and nuanced ways. Further research is needed to delineate more clearly these interactions and to explore other factors that may play important additional roles.
Introduction
A significant number of medical school faculty—males and females—are raising children under 18 years of age while trying to advance their academic careers. This reflects a growing trend in many Western countries for females to delay childbearing as they pursue educational and career goals. Changing societal values, increasing gender equity, accessible and effective contraception, and recently, economic pressures, have all contributed to this trend.1–4
Balancing childcare and family responsibilities nonetheless has been widely reported to be challenging in the context of an academic medical career with long hours due to patient care responsibilities and on-call assignments, high expectations for research productivity in an increasingly competitive funding environment, and many teaching assignments, as well as committee work and activities in professional societies and organizations that are necessary to demonstrate a local/regional/national reputation required for academic advancement. In a published survey from another academic medical institution, a substantial proportion of both males and females reported that conflicts between work and family might contribute to a decision to leave academic medicine or the institution, with females (32%) reporting this more frequently than males (18%).5 Conflicts between work and family also influence family formation and faculty satisfaction, the latter being a strong predictor of leaving a position in academic medicine.6,7 Females are more likely than males to leave academic medicine before achieving the rank of full professor, despite the fact that greater numbers of females initially enter into careers in academic medicine.7,8 Findings from a study of University of California (UC) faculty may provide some insight into this retention phenomenon, showing that a female faculty member was less likely to make tenure than a male if she had a child within 5 years of taking a tenure-track faculty position.9 Available data from other sources also suggest that the academic productivity of early career female faculty in medicine is adversely and differentially affected by child-rearing responsibilities. Indeed, female faculty with children overwhelmingly believe that their career progress and productivity has been slowed by having children.10 Frustration with progress and productivity as well as the strains of having to “do it all” by balancing career and family may contribute to a female faculty member's decision to leave a faculty position.
Female faculty, however, may be the canaries in the coalmine. In recent years, the issue of satisfaction with work–family balance has become increasingly important and potentially problematic for males, too, due to changing expectations about gender equity in the home and the role of fatherhood.11,12 We have previously reported that the younger generation (age <50 years) of male medical academics have lower career satisfaction than older males and females of all ages. Thus, work–family conflict is not just a women's issue, since young males are at growing risk for career dissatisfaction and retention issues too.13 Replacing faculty due to dissatisfaction has a financial impact that is not insignificant. One academic medical center estimated that in 2004 the cost to replace a clinical faculty member could range from $115,000 to over $400,000, depending on specialty.14 Loss of clinical faculty also has a negative impact on funds available for research, since this mission often receives large subsidies from clinical activity,15,16 in addition to having a negative impact on the academic teaching mission, ostensibly a medical school's primary purpose for existence.17 Work–life conflict can lead to physician burnout, and burnout has been shown to increase medical errors.18,19 Therefore, the financial, academic, and clinical quality incentives to improve clinical faculty satisfaction, retention, and performance are substantial.15,16,20
To reduce work–life conflict and facilitate faculty recruitment and retention, the majority of medical schools have developed flexibility policies aimed at improving work–family compatibility.21 Surveys conducted by the American Association of Medical Colleges (AAMC) have demonstrated considerable growth in adoption of flexibility policies by Liaison Committee on Medical EducationLCME-accredited medical schools. In 1983, only 26% of medical schools offered probationary periods beyond 8 years for clinical or basic science faculty. By 2008, this had grown to 45% of schools offering this opportunity to basic science faculty and 50% to clinical faculty.19 The 2008 survey also demonstrated that the majority of schools provide policies to stop the tenure clock for child care (83%), medical disability (80%), or care of an ill family member (77%), though only a minority offer this opportunity for faculty with a large administrative load (32%) or for those pursuing an advanced degree (26%). These percentages had not changed significantly from 2002, nor had the percentages of medical schools offering opportunities for part-time employment (approximately one-third) while on a tenure-eligible track.19 A more recent study of U.S. News & World Report's top 10 medical schools showed that flexible career policies exist at each, but that there is considerable variation among the policies.22 Our previous work has shown that our own school's flexibility policies are important to faculty satisfaction, though they are underutilized and do not fully address faculty needs.23 Low use of flexibility policies has also been noted nationally.24 We found that there are many barriers to using policies, including financial barriers, concerns about perception of commitment to career, and concerns about burdening colleagues.23 Given this underutilization of flexibility policies and the rigors of the academic culture, we hypothesize that (1) demanding family responsibilities adversely affect faculty career satisfaction, and (2) satisfaction is lowest among those faculty members who have less flexibility due to clinical demands, lower seniority, or unstable funding. To explore these hypotheses, in this report we examined the relationship of faculty career satisfaction and work–life integration to family care responsibilities and demographics (age, gender, marital status). Our goal was to understand more fully the characteristics of faculty at risk for low career satisfaction and work/family life balance in order to target efforts to improve workplace policies, support more female faculty so that they may attain the ranks of full professorship, and improve faculty retention for both genders.
Methods
The data for this analysis come from the baseline survey of the first of a 4-year National Institutes of Health (NIH)–funded study to evaluate the awareness, knowledge, attitudes, and use of family friendly policies and career satisfaction in the School of Medicine (SOM) at University of California–Davis. A 53-item Work, Family, and Satisfaction Survey was utilized for this study and adapted from a 125-item survey instrument that utilized survey domains and parameters based on the institution's prior Sloan award. Use of this instrument has been validated in over 10,000 faculty participants and is available for unrestricted use from the Clear Picture Corporation in partnership with the Alfred P. Sloan Foundation. The survey was enhanced with additional demographic variables necessary for the analyses proposed. In addition, survey domains adapted from the AAMC's Collaborative on Academic Careers in Higher Education satisfaction survey were included to demonstrate our efforts to capture and assess parameters pertinent to career satisfaction with comparative relevance to the AAMC survey instrument. The Work, Family, and Satisfaction Survey utilized for these studies assessed faculty's experience with use of and intention to use policies; awareness of options (leave for mothers/fathers, personal disability, tenure clock stoppage, part-time appointments); barriers to use of policies; and career satisfaction as previously described23 and briefly summarized in Table 1. Additionally, the survey assessed faculty demographics including gender and age. The survey was constructed using Survey Monkey® and was administered electronically for a 3-week period in the spring of 2010 by e-mail to all faculty in the SOM. Two e-mail reminders were sent to faculty who had not yet completed the survey prior to the survey close date. Completion rates were tracked to minimize excessive reminders. Participation was voluntary and responses were confidential. Baseline (year 1) responses were utilized for these studies. The study and survey were approved by the institutional review board.
Table 1.
Summary of University of California, Davis, School of Medicine Family Friendly Policies
| Birth or adoption leave | ASMD | Tenure clock stoppage | Post-tenure deferrals | Part-time work | Salary | Protections | |
|---|---|---|---|---|---|---|---|
| Policy | 12 weeks | 12 weeks per child | 1 year per child, 2 years max | One year per child | May request, permanent or temporary | No salary reductions or restrictions; full disability protections; costs covered by departments | No prejudice or penalty |
ASMD, active service modified duties; for a faculty member with 50% or more responsibility for care of a new child.
The outcomes of interest were as follows: satisfaction with work–life balance rated on a scale of 1–5, where 1=very dissatisfied and 5=very satisfied; overall career satisfaction rated on a scale of 1–5; satisfaction with existing family friendly policies rated on a scale of 1–5; whether or not the respondent has concerns about the way they would be viewed by colleagues if they were to make use of family friendly policies (yes/no); and whether or not the respondent thought that existing family friendly policies were fairly implemented in their department (yes/no).
Previous publications from our group have addressed overall gender differences in faculty satisfaction with career and work–life balance, as well as gender–generation interactions.13,23 The current analysis addresses the impact of family responsibilities and three characteristics of the faculty position: rank, clinical versus nonclinical duties, and academic series (reflecting whether the funding source is primarily state-guaranteed funding, grants and contracts, or clinical revenues, a marker for security of funding and potential job-related stress.) UC Davis has a number of faculty tracks. For the purposes of this study, respondents were dichotomized into “clinical” and “nonclinical” tracks. The distinction was made on the basis of the primary academic responsibility and time allocation of faculty activities for each of the tracks. Any faculty with clinical responsibilities were classed as “clinical faculty,” including a small group who also have research responsibilities. The remaining “nonclinical faculty” includes those with research, teaching, administrative duties, or a combination, but no clinical duties. We also examined personal characteristics that might confound or modify the association between family responsibilities and career outcomes: age, gender, and marital status. Categories for family care responsibility (FCR) were made after examining the self-reported intensity of family demand (average number of hours per week of care provided) for more detailed subgroups. We combined subgroups with similar levels of demand, resulting in the following three groups: FCR1, no family care responsibilities; FCR2, children not living at home and/or other family care responsibilities, which could include caring for an ill spouse, elder parent, or other; and FCR 3, children under 18 at home, possibly in addition to other family care responsibilities.
The model selection process started with descriptive summaries and then pairwise assessment of the association between every predictor (primary and confounders) and every outcome of interest. For categorical predictors, differences in outcome were estimated relative to a reference category, generally chosen to have the least family and clinical responsibilities, lower academic rank, and to be the most numerous demographic category. Effect modifications among primary predictors and between primary predictors and potential confounders were then considered. The first full model for any particular outcome contained all four primary predictors, any confounder that made an impact greater than 10% on the coefficient for any primary predictor in univariate models, and any significant interaction terms from simpler models for the outcome in question. Effect modification terms were removed from the model until only significant effect modification terms remained. Satisfaction scores were treated as continuous variables and were modeled with linear regression. Outcomes with binary answers were modeled with logistic regression.
Results
Respondents
The study was administered to all faculty in the School of Medicine (full- and part-time faculty); however, the percentage of part-time faculty in the school is relatively small (<20%). Volunteer clinical faculty were not included in the surveys, as they are ineligible for faculty leave policies. A total of 325 respondents completed the surveys; overall, 42% of faculty had complete data and could be included in one or more models (Table 2). The demographics of the population of respondents, as previously published,13,23 are summarized in Table 3 and generally reflect the school as a whole,25 though the respondents tended to be slightly older, white, and female. Nearly 40% of respondents were female, as compared with 30% female faculty overall in the school. Just over half of respondents were over the age of 50 years, slightly higher than the school's percentage of faculty older than 50 years (45%). Three-quarters were Caucasian, as compared with 63% of our medical school faculty. The rank of respondents was similar to the general faculty population: one-third were assistant professors (vs. 32% in the school overall), 25% were associate professors (school, 25%), and 42% were full professors (school, 43%). Half of the respondents were in primarily clinical tracks; the majority had full-time appointments; half had been at the institution for 10 years or less; the majority (males and females) were married or in committed relationships; and more females (35%) than males (14%) were childless (p<0.001). More than half of the respondents had children under 18 living at home, and another 30% had other family responsibilities. There were few significant demographic differences between respondents and nonrespondents; there were fewer males (62% vs. 69%), fewer assistant professors (31% vs. 41%), and fewer clinical professors (21% vs. 28%) among respondents.
Table 2.
Descriptive Summary of Sample for N=325 Faculty Respondents Included in One or More Models
| Description of samplea | |
|---|---|
| Primary predictors | |
| Family care responsibilities, number, (%) by category | |
| No family care responsibilities | 43 (14.0%) |
| Children not living at home and/or other family care responsibilities which can include caring for an ill spouse, elder, etc. | 92 (30.0%) |
| Children under 18 at home, possibly in addition to other family care responsibilities | 172 (56.0%) |
| Rank, number (%) by category | |
| Assistant professor | 99 (31.4%) |
| Associate professor | 77 (24.4%) |
| Full professor | 139 (44.1%) |
| Clinical vs. non-clinical specialty, number (%) by category | |
| Nonclinical (basic scientist in clinical or nonclinical department) | 97 (31.5%) |
| Clinical (surgery/medicine/hospital-based specialty) | 211 (68.5)% |
| Potential confounders/effect modifiers | |
| Sex, number (%) female | 120 (38.1%) |
| Age, number (%) by category | |
| Younger generation (born 1961 or after) | 163 (53.1%) |
| Older generation (born 1925–1960) | 144 (46.9%) |
| Marital status, number (%) by category | |
| Single, divorced, or widowed | 35 (11.2%) |
| Married, other committed | 277 (88.8%) |
| Level of demand of family responsibilities (demand) on scale of 1–5 (1, not at all demanding; 5, extremely demanding), mean (±SD) | 2.6 (±1.1) |
| Outcome variables | |
| Work–life balance on scale of 1–5 (5, highest), mean (±SD) | 3.4 (±1.3) |
| Career satisfaction on scale of 1–5 (5,highest), mean (±SD) | 3.8 (±1.1) |
| Policy satisfaction on scale of 1–5 (5, highest), mean (±SD) | 3.4 (±1.1) |
| Concerned about colleague reaction, number (%) yes | 128 (46.2%) |
| Implemented fairly, number (%) yes | 198 (78.0%) |
Not all respondents were included in every category, so values may not total 325.
SD, standard deviation.
Table 3.
Demographics of Survey Respondents
| Characteristic | Demographic | Respondentsa |
|---|---|---|
| Gender | ||
| Male | 195 (61.9)b | |
| Female | 120 (38.1) | |
| Age (years) | ||
| Under 50 | 163 (53.1) | |
| 50–67 | 133 (43.3) | |
| 68–84 | 11 (3.6) | |
| Race/ethnicity | ||
| Hispanic | 13 (4.5) | |
| Caucasian | 230 (77.7) | |
| African American | 4 (1.4) | |
| Asian | 62 (20.9) | |
| Other | 0 | |
| Rank | ||
| Assistant professor | 99 (31.4)b | |
| Associate professor | 77 (24.4) | |
| Full professor | 139 (44.1) | |
| Series | ||
| Professorial | 94 (29.8) | |
| In residence | 34 (10.8) | |
| Clinical | 94 (29.8) | |
| HS clinical professor | 66 (21)b | |
| Adjunct | 25 (7.9) | |
| Don't know | 2 (0.6) | |
| Appointment | ||
| Part time (%) | 19 (6) | |
| Full time (%) | 294 (93) | |
| Other (%) | 3 (0.9) | |
| Length of faculty appointment | ||
| 1–5 years | 116 (36.6) | |
| 6–10 years | 78 (24.6) | |
| 11–15 years | 42 (13.2) | |
| 16–20 years | 33 (10.4) | |
| 20+ years | 48 (15.1) | |
| Specialty | ||
| Surgery/surgical specialty | 55 (16.9) | |
| Medicine/medicine subspecialty | 100 (30.8) | |
| Hospital-based specialty (i.e., pathology, radiology, emergency medicine, anesthesiology, radiation oncology, etc.) | 56 (17.2) | |
| Basic scientist in clinical department | 46 (14.2) | |
| Basic scientist in nonclinical department | 51 (15.7) | |
| NA | 17 (5.2) | |
Overall N=325.
Not all respondents were included in every category, so values may not total 325.
Compared with nonrespondents, fewer respondent were males (62% vs. 69%), assistant professors (31% vs. 41%), and clinical professors (21% vs. 28%).
HS, Health Sciences; NA, not applicable.
The survey respondents reported good satisfaction with work–life balance (mean 3.4 on a scale of 1–5, with 5 being the highest), career (mean 3.8), and policies (mean 3.4), but there was substantial variation. Almost half were concerned about colleague reaction if they took family leave, but most felt the policies were implemented fairly. Regression models assessed differences in satisfaction compared with reference categories, identified as faculty with no family care responsibilities, nonclinicians, and assistant professors; for demographics, males, faculty under 40 years of age, and single, divorced, or widowed were used as reference categories. Academic series (whether salary support was provided primarily by state guaranteed funding, soft money from grants and contracts, or clinical revenues) was considered as a potential influence on satisfaction but found not to be significantly associated with any measure of satisfaction or with other predictors, so was omitted from multivariate models.
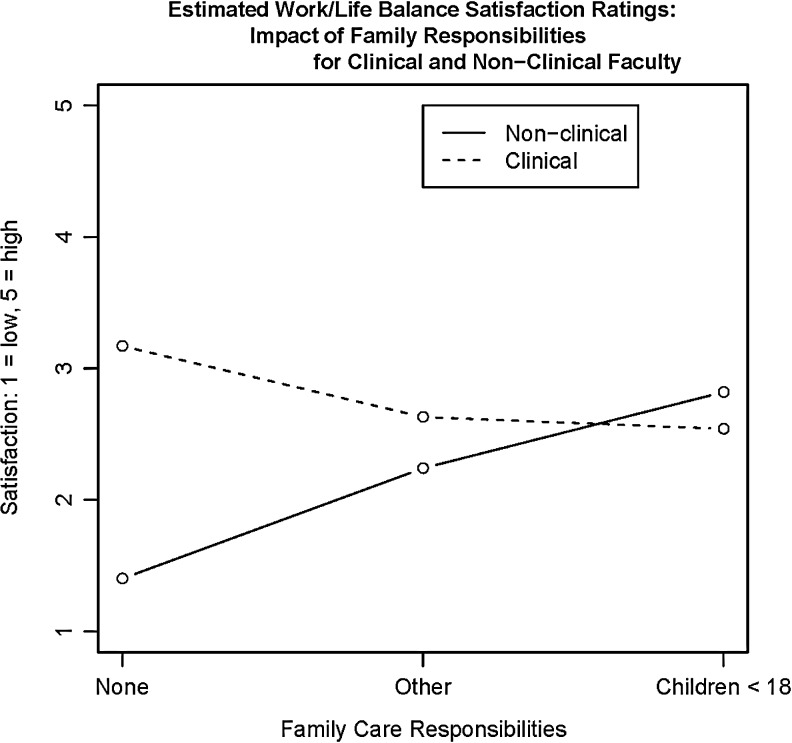
Satisfaction with work–life balance
We found that there was not a consistent overall difference in satisfaction with work–life balance between respondents in clinical and those in nonclinical positions, nor was there a consistent difference between those with and without children. Instead, we found that caring for children and working in a clinical position were individually associated with substantially improved reported work–life balance as long as they were not combined, but the dual responsibility of caring for children plus working in a clinical position led to less reported satisfaction with work–life balance. For faculty respondents without children, working in a clinical position was associated with significantly higher reported satisfaction with work–life balance than working in a nonclinical position (1.77-point increase on a 1–5 scale, 5 being highest, p=0.01), Table 4. For faculty respondents in a nonclinical role, caring for children under 18 years old was associated with significantly better work–life balance (1.14-point increase, p=0.01). Among faculty respondents with a clinical position; however, satisfaction with work–life balance was 0.91 points lower for those caring with children under 18. The difference in reported satisfaction with work–life balance between clinical and nonclinical faculty caring for children was highly significant (2.05-point negative impact on satisfaction with work–life balance, p=0.001). Thus, reported satisfaction with work–life balance increased with family engagement for nonclinical faculty respondents but decreased for clinical faculty respondents (Fig. 1).
Table 4.
Faculty Family Care Responsibilities and Impact on Work–Life Balance Satisfaction, Career Satisfaction, and Satisfaction with Family Friendly Policies
| Work–life balance satisfaction | Career satisfaction | Policy satisfaction | |||||||
|---|---|---|---|---|---|---|---|---|---|
| (n=246) | (n=251) | (n=192) | |||||||
| Estimate | 95% CI | Pr(>|t|) | Estimate | 95% CI | Pr(>|t|) | Estimate | 95% CI | Pr(>|t|) | |
| Reference meansa | 1.40 | (0.12, 269) | 0.03 | 2.64 | (1.55,373) | <0.001 | 1.50 | (0.13,2.88) | 0.03 |
| Personal factors | |||||||||
| Family care: non-children | 0.84 | (−0.34, 2.01) | 0.16 | 0.77 | (−0.18, 1.71) | 0.11 | 0.71 | (−0.51, 1.92) | 0.25 |
| Family care: children | 1.14 | (0.29, 2.55) | 0.01 | 1.27 | (0.36, 2.18) | 0.001 | 1.36 | (0.19, 2.53) | 0.02 |
| Female | −0.01 | (−0.36, 0.35) | 0.97 | −0.23 | (−0.72, 0.27) | 0.37 | 0.11 | (−0.46, 0.68) | 0.69 |
| Married/committed | 0.33 | (−0.21, 0.88) | 0.23 | 0.27 | (−0.20, 0.74) | 0.25 | 0.66 | (0.04, 1.28) | 0.04 |
| Intensity of family demand | −0.06 | (−0.25, 0.12) | 0.49 | −0.09 | (−0.25, 0.07) | 0.24 | −0.09 | (−0.26, 0.08) | 0.28 |
| Younger generation (born after 1961) | 0.40 | (−0.07, 0.87) | 0.09 | 0.16 | (−0.24, 0.56) | 0.44 | 0.11 | (−0.34, 0.57) | 0.62 |
| Work-related factors | |||||||||
| Clinical vs. non-clinical | 1.77 | (0.53, 3.02) | 0.01 | 1.82 | (0.80, 2.83) | <0.001 | 1.45 | (0.14, 2.76) | 0.02 |
| Associate professor | 0.52 | (0.06, 0.97) | 0.03 | −0.37 | (−0.90, 0.17) | 0.18 | −0.19 | (−0.81, 0.44) | 0.56 |
| Full professor | 0.61 | (0.08, 1.14) | 0.02 | 0.35 | (−0.20, 0.90) | 0.21 | 0.41 | (−0.21, 1.03) | 0.19 |
| Modification of personal factors by work factorsb | |||||||||
| Clinical/family care (non-children) | −1.38 | (−2.73, −0.02) | 0.047 | −1.51 | (−2.63, −0.40) | 0.01 | −1.02 | (−2.46, 0.41) | 0.16 |
| Clinical/family care (children) | −2.05 | (−3.31, −0.80) | 0.001 | −1.67 | (−2.69, −0.40) | 0.002 | −1.62 | (−2.94, −0.31) | 0.02 |
| Associate professor, female | – | – | – | 1.16 | (0.42, 1.91) | 0.002 | 0.90 | (0.07, 1.74) | 0.03 |
| Full professor, female | – | – | – | 0.12 | (−0.57, 0.81) | 0.73 | −0.38 | (−1.15, 0.40) | 0.34 |
Estimated mean change in score on scale of 1–5 (5=most satisfied), compared with reference category, with 95% confidence interval (95% CI) for Estimate. The rank–gender interaction for the work–life balance outcome has been left blank, as it did not meet the criteria set forth for inclusion in the model, and was therefore not included.
Reference categories for comparisons: Assistant professors in nonclinical appointments; older generation, male, unmarried, with no family responsibilities and low family demand.
Effect modification estimates show how the effects of family or personal characteristics differ for faculty members in specific work categories compared with those in the reference categories. Only those statistically significant for at least one outcome are shown.
Numbers in bold indicate statistically significant values.
FIG. 1.
Estimated mean satisfaction levels for work–life balance for clinical and nonclinical faculty by level of family care responsibilities (none, children under 18 years old at home, other). Estimates are based on regression model adjusted for age, gender, marital status, academic rank, and intensity of family demand (model coefficients shown in Table 4).
No other personal characteristics (age, gender, marital status, or reported family demand) were significantly associated with reported satisfaction with work–life balance. In terms of work-related factors, associate professors and full professor respondents reported greater work–life balance satisfaction than assistant professors (approximately half a point; p=0.03, p=0.02, respectively).
Satisfaction with career
We found a similar clinical–children interaction with regard to career satisfaction as we did for work–life balance satisfaction: both a clinical position and having children under age 18 years were associated with improved satisfaction among respondents, but the combination of the two did not doubly improve satisfaction. Clinical faculty without children reported higher career satisfaction (1.82-point increase, p<0.001; Table 4), whereas clinical faculty with children reported a very slight increase in career satisfaction (0.20-point increase) that did not reach statistical significance. Nonclinical faculty respondents with children under 18 experienced higher career satisfaction (1.27-point increase, p=0.001; Table 4). However, faculty respondents in a clinical role with children reported 0.40 points lower career satisfaction than their counterparts without children, representing a 1.67-point (p=0.002) negative impact on career satisfaction for clinical faculty for combining children with career. In addition, while other family care (non-children) responsibilities were not reported to be significantly associated with any additional benefit on career satisfaction (0.77-point increase, p=0.11), respondents with such responsibilities in clinical positions reported a significant reduction in career satisfaction (1.51-point decrease, p=0.01). Nonclinical faculty respondents without any other family care responsibilities (non-children) reported the lowest career satisfaction compared with other groups of faculty respondents.
Female respondents did not differ in career satisfaction from male respondents with similar family and career attributes, except that female respondents at the associate professor level were significantly more satisfied with career than their male counterparts (1.16-point increase, p=0.002).
Satisfaction with career flexibility policies
Respondents caring for children under age 18 years and clinical faculty respondents both reported higher satisfaction with family friendly policies, but respondents with the combination of caring for children under age 18 and a clinical faculty position reported less satisfaction with career flexibility policies. In the absence of children, faculty respondents in clinical roles reported higher satisfaction than those in nonclinical roles (1.45-point increase, p=0.02; Table 4). In nonclinical roles, faculty respondents caring for children under 18 had higher satisfaction with family friendly policies than faculty respondents without children (1.36-point increase, p=0.02.) Faculty respondents with both children under 18 years old and clinical positions reported less satisfaction with policies than clinical faculty without children (0.26 points lower, nonsignificant [NS]) and nonclinical faculty with children (0.17 points lower, NS). Faculty respondents with neither children nor a clinical role reported being least satisfied with career flexibility policies.
Married faculty respondents or those in a committed relationship were more satisfied with policies than were unmarried respondents (0.66 points, p=0.04). Female associate professor respondents were more satisfied with family friendly policies than their male counterparts (0.90-point increase, p=0.03).
Concern about colleague reaction to policy use
Faculty respondents with children at home were only one-third as likely to be concerned about colleague reaction to policy use as those respondents without family responsibilities (odds ratio=0.33, p=0.053). In respondents, higher levels of family demand predicted concern about colleague reaction independently of other personal factors, and as the self-reported demand of family care increased, there were increasing odds of concern about colleague reaction to policy use (odds ratio=1.75, p<0.001). These findings suggest that for respondents, lower levels of concern about colleagues' reactions may be limited to faculty members whose childcare responsibilities place fewer demands on them. There were no significant differences between male and female respondents in concern about colleague reaction to policy use, and no work-related factors were associated with this concern.
Perception of policy fairness
Respondents reported no significant associations between either personal or work-related predictors or the perception of fairness in policy implementation, with three-quarters of faculty respondents reporting that policies were fairly implemented (Tables 2, 5). Female respondents were similar to male respondents in their perception of fairness in policy implementation.
Table 5.
Faculty Family Care Responsibilities and Impact on Potential Barriers: Concern About Colleague Reactions and Fairness of Implementation
| Concerned about colleague reaction (yes/no) | Implemented fairly (yes/no) | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | Pr(>|z|) | OR | 95% CI | Pr(>|z|) | |
| Personal factors | ||||||
| Family care: non-children | 0.63 | (0.22, 1.77) | 0.38 | 0.98 | (0.30, 3.27) | 0.98 |
| Family care: children | 0.34 | (0.12, 1.01) | 0.053 | 1.41 | (0.38, 5.14) | 0.61 |
| Female | 1.49 | (0.82, 2.70) | 0.19 | 0.82 | (0.40, 1.70) | 0.6 |
| Married/committed | 1.48 | (0.57, 3.80) | 0.42 | 1.52 | (0.56, 4.18) | 0.41 |
| Level of family demand | 1.78 | (1.28, 2.47) | <0.001 | 0.84 | (0.57, 1.22) | 0.35 |
| Younger generation (born after 1961) | 1.83 | (0.78, 4.30) | 0.17 | 1.89 | (0.67, 5.28) | 0.23 |
| Work-related factors | ||||||
| Clinical vs. nonclinical | 0.8 | (0.44, 1.45) | 0.46 | 0.68 | (0.32, 1.43) | 0.31 |
| Associate professor | 1.25 | (0.56, 2.79) | 0.58 | 1.57 | (0.60, 4.12) | 0.36 |
| Full professor | 1.27 | (0.51, 3.17) | 0.61 | 2.21 | (0.73, 6.69) | 0.16 |
Estimated odds ratio (ORs) and 95% confidence intervals for reporting concern about reaction of colleagues to use of family friendly policies (n=227) and fairness of implementation (n=211), compared with reference category.
Reference categories for comparisons: assistant professors in nonclinical appointments, funding from state full-time equivalent (tenure), older generation, male, unmarried, with no family responsibilities and low family demand.
Numbers in bold indicate statistically significant values.
Discussion
Our study suggests that in our survey respondents, highly demanding family responsibilities (defined as having children under 18 at home) did not adversely affect career satisfaction, nor was satisfaction consistently lower among those faculty members with less flexibility in their careers, as we had hypothesized. Surprisingly, nonclinical faculty respondents, both males and females, with young children reported higher satisfaction with work–life balance and career than those without children. When comparing clinical versus nonclinical faculty respondents, clinical faculty without family responsibilities reported significantly greater satisfaction with work–life balance and career than their nonclinical counterparts; this difference, however, was not maintained for those respondents with children. A family leave for multiple months can adversely affect grant-funded work, create a disadvantage to obtaining additional funding, and make it difficult to maintain a laboratory, while in clinical medicine, it is possible in many departments or sections for other faculty to provide cross coverage, potentially minimizing the impact to the clinical service. The potential impact of children on clinical faculty in departments that cannot provide cross coverage is an important aspect that needs to be considered. In addition, development of a clinical practice and reputation (needed for promotion and career advancement), developing respect within a department, and establishment of a secure income can be significantly impacted by needing to take time off. Security of income is also a factor worthy of consideration. According to the AAMC's Faculty Forward Survey, salary is not a significant factor in career satisfaction, but salary source may be a factor influencing satisfaction for clinical versus nonclinical faculty.26 Since clinical income is a fairly secure salary source, it may positively influence faculty satisfaction. The majority of our research-intensive faculty are supported almost entirely by grant funds, which are becoming more difficult to obtain, creating more insecurity and adversely affecting this group's career satisfaction. As new clinical reimbursement patterns are implemented due to national healthcare reform, clinical income will likely diminish and become a less secure salary source for all physicians,27 including academic clinical faculty. Differences in career satisfaction between clinical and nonclinical faculty may therefore narrow.
It was also interesting that nonclinical faculty respondents with children reported higher satisfaction with work–life balance than those without children. Also surprising was that both female and male nonclinical faculty respondents with children reported experiencing the same level of satisfaction, and females did not report greater challenges in maintaining work–life balance. It may be that nonclinical faculty may find it easier to arrange teaching and research schedules and can better meet the needs of small children at home by having greater control of schedules and work hours.28,29 Notably, neither male nor female clinical faculty respondents with children benefitted from the dual increases in satisfaction associated with clinical work for their childless clinical counterparts and associated with children for their nonclinical counterparts. Instead, both male and female clinical faculty respondents with children reported a similar level of satisfaction to that of nonclinical faculty with children. We interpret this finding to suggest that the challenges of balancing childcare responsibilities with clinical faculty roles affects both fathers and mothers, to a degree that outweighs the increased satisfaction reported by parents in nonclinical faculty roles. Our findings are consistent in many ways with other published studies that have linked children to faculty satisfaction. Gender-based differences, however, were uncommon in our study, in contrast to a multi-institutional study of 24 medical schools that provided summary conclusions that gender-based disparities in satisfaction were linked to family responsibilities.30 Other studies have shown that females with children have less institutional support,31 fewer publications,10,32–34 slower self-perceived career progress, and lower career satisfaction.30 These factors may all contribute to the lower satisfaction reported by clinical faculty with children in our study, and thus may be more broadly applicable than just to females in our school.
Many family friendly policies were originally implemented as one accommodation to allow females an equal chance to succeed in academia by providing childbearing leaves. AAMC medical school faculty benchmarking data continues to report a great disparity in the proportion of female versus male full professors,26 and the likelihood for parity in the near future appears to be low if the current rate of change is maintained. However, lack of role models and other factors are also implicated in the lack of parity and career satisfaction for females,35–37 and it should not be assumed that family friendly policies alone would have a significant impact on satisfaction and/or academic success. The impact of these policies on promotion also remains to be determined. In addition, when discussing career flexibility policy existence and use, it is necessary to recognize the important role of institutional culture. Whereas great headway has been made in flexible policies for faculty, there is still a lag in cultural acceptance of those policies—the academic medicine culture at institutions is a powerful force in mitigating acceptance.
Our study found that female faculty respondents report greater career satisfaction than male respondents once they reach the associate professor level. The associate professor level represents a major transition in our university and most academic medical schools; at our institution, equal numbers of male and female faculty separate from the university before reaching the level of associate professor, but fewer females are hired at higher levels. Thus, the females at this level represent a select subset that have either been retained successfully from the assistant professor level at our own school or have been recruited from a smaller pool of female associate professors at other institutions. Our study suggests that the rewards and challenges facing academics early in their career may be more similar for males and females in the same discipline than they are for faculty of the same gender but in clinical compared with nonclinical tracks. The differential impact on satisfaction with career and family may affect both fathers and mothers in the clinical faculty track similarly, but their career choices, especially around the transition to associate professor, may differ. Fewer females with children may choose to stay in academic clinical medicine, with those who stay at the associate professor level being those who have been able to manage the difficult balance more successfully.
Another dimension of family formation that is important to consider is childlessness. Although childlessness may be a deliberate choice for many, there is a rise in involuntary childlessness in Western countries due to postponement of parenthood in order to accomplish academic and career goals.38,39 As we note in Results, our survey revealed that substantially more females than males were childless in our SOM (35% vs. 14%, p<0.001). The long educational and training paths for medical school faculty raises challenges for female faculty in the timing of family formation and likely makes infertility and involuntary childlessness even greater potential issues that compound the challenges shared by faculty in all disciplines, including attaining promotion in set time periods, establishing and maintaining a successful research program, and real and perceived barriers to the use of family friendly policies.10,40–43 Policies that reduce the incompatibility between work and the roles of parenthood, such as leaves for child bearing and rearing and availability of on-site childcare, have been shown to lead to younger ages at first birth1,8 and may reduce childlessness and optimize faculty health, workplace performance, career satisfaction, and retention of diverse faculty.
Our study has a number of limitations. The response rate to the faculty surveys was 42%, leaving open the possibility of substantial response bias. However, no single standard has been established for physician surveys, and the response rate among academic physicians and other faculty reported here is only slightly lower than the previous published response rate from the Association of American Medical Colleges (AAMC) Faculty Forward Survey26 and equivalent to that required by the American Council on Education and the Sloan Foundation for their recent awards for medical school career flexibility surveys.44 Our survey respondents were broadly similar to the faculty composition of our school of medicine in age, gender, academic rank, and series. In addition, the demographics for gender and rank within our school and our survey respondents are very similar to data for medical schools reported by the AAMC, though we have slightly more females who are associate professors and slightly fewer females who are full professors.8 The survey we used for this study was developed for the goals of a larger, parent study and may not have included some important variables that could play a significant role in understanding the characteristics of faculty at risk for low career satisfaction and work–family conflict, as detailed below. The survey also did not use skip logic or branching, as this was not a functionality in Survey Monkey for the scenarios posed in the surveys. Therefore, every faculty member was provided the opportunity to answer every question on both awareness and usage. It is also possible that the categories of family care responsibility miss key elements of demand such as more information about spouse/partner including work full time or part time, degree of flexible work hours for spouse/partner, and other responsibilities such as care for special needs children, aging parents, or other relatives and that there are important additional work-related variables that are not included and would further explain satisfaction with work–life balance such as certain qualities of the school leadership, department culture, access to mentoring, access to team-based research, and average number of hours in the typical work week. In addition, this is a single institution study and therefore the results may be significantly impacted by a number of factors including the overall culture of the SOM at the University of California, Davis, the economic climate of the school, the definition of the tracks, the promotion criteria, and the work–life policies, and some of these variables may be institution specific. However, there is enough in common with other medical schools that our work should be generalizable, add to the discussion, and encourage others to take this line of research to the next level.
Conclusion
Further research is necessary to understand the full scope of predictors of satisfaction with work–life balance and to determine what changes can be made to improve the ability of both clinical and nonclinical faculty to have both successful careers and rewarding family lives. It may be that there are challenges inherent to the practice of clinical academic medicine that are fundamentally at odds with balancing family care responsibilities, but there are likely adjustments that can be made to lessen the conflict (e.g., job sharing, extending time to tenure, on-site childcare, paternity leaves, etc.). The degree of career satisfaction of faculty with young children, and of female faculty who have reached the associate professor level, might be a sign that family friendly policies are achieving their goals, although the real measure may be changes in retention and promotion of female faculty over the next few decades. The widespread perception that policies are implemented fairly is an encouraging sign that faculty would support continued efforts to expand access to family friendly policies. In recognition of changing social norms about family structure, perhaps more emphasis needs to be placed on the “family” in “family friendly” policies, supporting male and female faculty in the care of children and family members through older ages, and recognizing that fathers also have an important role to play at home. Our findings suggest that clinical faculty with young families are at special risk of struggling with work–life balance. We lose more females than males to academic medical careers around the period of transition to associate professor, and family friendly interventions may not only benefit both males and females, but may also help us to retain females as well as make it possible for both fathers and mothers in the clinical faculty to have the increased satisfaction that children bring to the lives of their nonclinical counterparts. The authors recognize, however, that it is not just the existence or nonexistence of policies that underlies career success, satisfaction, and retention. There are other important factors at play that include communication from leadership, transparency in process, awareness of policies, bias at institutions, and the culture of the institution.
In summary, the issue of work–life balance is one of the most pressing challenges facing academic faculty and medical schools across the country. Our work contributes to the literature in that it examines the associations among family care responsibilities with a variety of other factors that may influence career satisfaction and work–life balance and provides a number of important and unanticipated findings. The results advance our understanding of what is clearly a complex issue and one that needs ongoing evidence-based discussion.
Acknowledgments
This work was supported by NIH award GM 088336 in partnership with the Office of Women's Health Research (OWHR), with the goal of supporting research on causal factors and interventions that promote and support the careers of women in biomedical and behavioral science and engineering. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of General Medical Sciences or the National Institutes of Health. This publication was also made possible by the Frances Lazda Endowment in Women's Cardiovascular Medicine to ACV. The authors also wish to thank Cris Warford, BS, and Hassan Baxi, MA, for technical assistance in the conduct of these studies and Yueju Li, MS, for additional statistical analysis.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Mills M, Rindfuss RR, McDonald P, te Velde E; ESHRE Reproduction and Society Task Force. Why do people postpone parenthood? Reasons and social policy incentives. Hum Reprod Update 2011;17:848–860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hardy JB, Astone NM, Brooks-Gunn J, Shapiro S, Miller TL. Like mother, like child: Intergenerational patterns of age at first birth and associations with childhood and adolescent characteristics and adult outcomes in the second generation. Dev Psychol 1998;34:1220–1232 [DOI] [PubMed] [Google Scholar]
- 3.Miller AR. Motherhood delay and the human capital of the next generation. Am Econ Rev 2009;99:154–158 [Google Scholar]
- 4.Taniguchi H. Work and family: The timing of childbearing and women's wages. J Marriage Fam 1999;61:1008–1020 [Google Scholar]
- 5.Shollen SL, Bland CJ, Finstad DA, Taylor AL. Organizational climate and family life: How these factors affect the status of women faculty at one medical school. Acad Med 2009;84:87–94 [DOI] [PubMed] [Google Scholar]
- 6.Smart JC. A causal model of faculty turnover intentions. Res High Educ 1990;31:405–424 [Google Scholar]
- 7.Nonemaker L. Women physicians in academic medicine: New insights from cohort studies. N Engl J Med 2000;342:399–405 [DOI] [PubMed] [Google Scholar]
- 8.Alexander H, Lang J. The long-term retention and attrition of U.S. medical school faculty. AAMC Analysis in Brief 2008;8(4) [Google Scholar]
- 9.Osborn EH, Ernster VL, Martin JB. Women's attitudes toward careers in academic medicine at the University of California, San Francisco. Acad Med 1992;67:59–62 [DOI] [PubMed] [Google Scholar]
- 10.Mason MA, Goulden M. Do babies matter (part II)? Closing the baby gap. Academe 2004;90:21–27 [Google Scholar]
- 11.Aumann K, Galinsky E, Mattos K. Times are changing: Gender and generation at work and home. 2008 National Study of the Changing Workforce. New York: Families and Work Institute, 2009 [Google Scholar]
- 12.Harrington B, Van Deusen F, Ladge J. The new dad: Exploring fatherhood within a career context. Boston: Boston College Center for Work and Family, 2010 [Google Scholar]
- 13.Howell LP, Beckett LA, Nettiksimmons J, Villablanca AC. Generational and gender perspectives on career flexibility: Ensuring the faculty workforce of the future. Am J Med 2012;125:719–728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Waldman JD, Kelly F, Arora S, Smith HL. The shocking cost of turnover in health care. Health Care Manage Rev 2004;29:2–7 [DOI] [PubMed] [Google Scholar]
- 15.Jones RF, Sanderson SC. Clinical revenues used to support the academic mission of medical schools, 1992–93. Acad Med 1996;71:299–307 [DOI] [PubMed] [Google Scholar]
- 16.Krakower JY, Coble TY, Williams DJ, Jones RF. Review of US medical school finances, 1998–1999. JAMA 2000;284:1127–1129 [DOI] [PubMed] [Google Scholar]
- 17.Papp KK, Aucott JN, Aron DC. The problem of retaining clinical teachers. Perspect Biol Med 2001;44:402–413 [DOI] [PubMed] [Google Scholar]
- 18.Dyrbye LN, Shanafelt TD, Balch CM, Satele D, Sloan J, Freischlag J. Relationship between work-home conflicts and burnout among American surgeons: A comparison by sex. Arch Surg 2011;146:211–217 [DOI] [PubMed] [Google Scholar]
- 19.Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. AnnSurg 2010;251:995–1000 [DOI] [PubMed] [Google Scholar]
- 20.Schloss EP, Flanagan DM, Culler CL, Wright AL. Some hidden costs of faculty turnover in clinical departments in one academic medical center. Acad Med 2009;84:32–36 [DOI] [PubMed] [Google Scholar]
- 21.Bunton SA, Correice A.M. Evolving workplace flexibility for U.S. medical school tenure-track faculty. Acad Med 2011;86:481–485 [DOI] [PubMed] [Google Scholar]
- 22.Bristol MN, Abbuhl S, Cappola AR, Sonnad SS. Work-life policies for faculty at the top ten medical schools. J Womens Health (Larchmt) 2008;17:1311–1320 [DOI] [PubMed] [Google Scholar]
- 23.Villablanca AC, Beckett L, Nettiksimmons J, Howell LP. Career flexibility and family-friendly policies: An NIH-funded study to enhance women's careers in biomedical sciences. J Womens Health (Larchmt) 2011;20:1485–1496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bunton SA, Mallon WT. The continued evolution of faculty appointment and tenure policies at U.S. medical schools. Acad Med 2007;82:281–289 [DOI] [PubMed] [Google Scholar]
- 25.AAMC FAculty Roster Benchmark Reports. Available at https://services.aamc.org/idsreports/index.cfm?fuseaction=main.Home&perspectiveCode=IDSRFR Accessed November21, 2014
- 26.Bunton SA, Correice AM, Mallon WT. Clinical faculty satisfaction with the academic medicine workplace. Washington, DC: Association of American Medical Colleges, 2011 [Google Scholar]
- 27.Rosenthal MB, Frank RG, Li Z, Epstein AM. Early experience with pay-for-performance: From concept to practice. JAMA 2005;294:1788–1793 [DOI] [PubMed] [Google Scholar]
- 28.Curtis JW. Balancing work and family for faculty. Academe 2004;90:21–23 [Google Scholar]
- 29.Keeton K, Fenner DE, Johnson TR, Hayward RA. Predictors of physician career satisfaction, work–life balance, and burnout. Obstet Gynecol 2007;109:949–955 [DOI] [PubMed] [Google Scholar]
- 30.Carr PL, Ash AS, Friedman RH, et al. Relation of family responsibilities and gender to the productivity and career satisfaction of medical faculty. Ann Intern Med 1998:532–538 [DOI] [PubMed] [Google Scholar]
- 31.Long Je. From scarcity to visibility: Gender differences in the careers of doctoral scientists and engineers. Washington, DC: National Academy Press, 2001 [Google Scholar]
- 32.Bentley RJ, Blackburn RT. Two decades of gain for female faculty. Teach Coll Rec 1992;93:697–709 [Google Scholar]
- 33.Ward KB, Grant L. Gender and academic publishing. In: Smart J, ed. Higher education: Handbook of theory and research. Bronx, NY: Agathon Press, 1995:172–212 [Google Scholar]
- 34.Zucherman He. The careers of men and women scientists: A review of current research. In: Zuckerman H, Cole J, Bruer T, eds. The outer circle: Women in the scientific community. New Haven: Yale University Press, 1991:27–56 [Google Scholar]
- 35.Levinson W, Kaufman K, Clark B, Tolle SW. Mentors and role models for women in academic medicine. West JMed 1991;154:423–426 [PMC free article] [PubMed] [Google Scholar]
- 36.Sambunjak D, Marusic A. Mentoring: What's in a name? JAMA 2009;302:2591–2592 [DOI] [PubMed] [Google Scholar]
- 37.Jackson VA, Palepu A, Szalacha L, Caswell C, Carr PL, Inui T. “Having the right chemistry”: A qualitative study of mentoring in academic medicine. Acad Med 2003;78:328–334 [DOI] [PubMed] [Google Scholar]
- 38.Peterson BD, Pirritano M, Tucker L, Lampic C. Fertility awareness and parenting attitudes among American male and female undergraduate university students. Hum Reprod 2012;27:1375–1382 [DOI] [PubMed] [Google Scholar]
- 39.te Velde E, Habema D, Leridon H, Eijkemans M. The effect of postponement of first motherhood on permanent involuntary childlessness and total fertility rate in six European countries since the 1970s. Hum Reprod 2012;27:1179–1183 [DOI] [PubMed] [Google Scholar]
- 40.Cropsey KL, Masho SW, Shiang R, Sikka V, Kornstein SG, Hampton CL. Why do faculty leave? Reasons for attrition of women and minority faculty from a medical school: Four year results. J Womens Health 2008;17:1111–1118 [DOI] [PubMed] [Google Scholar]
- 41.Jagsi R, Guancial EA, Worobey CC, et al. The “gender gap” in authorship of academic medical literature—a 35-year perspective. N Engl J Med 2006;355:281–287 [DOI] [PubMed] [Google Scholar]
- 42.Williams J. Unbending gender: Why family and work conflict and what to do about it. Oxford: Oxford University Press, 1999 [Google Scholar]
- 43.Robinson GE. Stresses on women physicians: Consequences and coping techniques. Depress Anxiety 2003;17:180–189 [DOI] [PubMed] [Google Scholar]
- 44.Families and Work Institute (FWI) and the Society for Human Resource Management (SHRM). When work works: About the award. 2014. Available at www.whenworkworks.org/about-the-award Accessed October9, 2014