Abstract
Psychosocial factors are increasingly recognized as risk indicators for coronary artery disease (CAD) prognosis, and they are likely interrelated. The objective of this study is to simultaneously test the relationship between key psychosocial constructs as independent factor scores, and recurrent events in CAD patients. One thousand two hundred and sixty eight CAD outpatients of 97 cardiologists were surveyed at two points. Recurrent events or hospitalization in the intervening 9 months were reported. Factor analysis of items from the Hospital Anxiety and Depression Scale, Perceived Stress Scale, the ENRICHD Social Support Inventory, and Hostile Attitudes Scale was performed, to generate orthogonal factor scores. With adjustment for prognostic variables, logistic regression analysis was performed to examine the relationship between these factor scores and recurrent events. Factor analysis resulted in a six-factor solution: hostility, stress, anxiety, depressive symptoms, support and resilience. Logistic regression revealed that functional status and anxiety, with a trend for depressive symptoms, were related to experiencing a recurrent event. In this simultaneous test of psychosocial constructs hypothesized to relate to cardiac prognosis, anxiety may be a particularly hazardous psychosocial factor. While replication is warranted, efforts to investigate the potential benefits of screening and investigate treatments is needed.
Keywords: Coronary artery disease, Recurrent coronary events, Anxiety, Depression, Stress, Social Support
Coronary artery disease (CAD) is the leading cause of morbidity and mortality worldwide (Organization for Economic Cooperation and Development, 2001; World Health Organization, 2006). While traditional risk factors for CAD development and prognosis are well known, psychosocial factors are also increasingly being recognized (Rozanski, Blumenthal, Davidson, Saab, & Kubzansky, 2005). For instance, numerous studies have shown the presence of depression to be related to a two-to-three-fold increase in the risk of mortality or non-fatal cardiac events among individuals with established CAD (Barth, Schumacher, & Herrmann-Lingen, 2004; Lett et al., 2004; van Melle et al., 2004). In fact, reviews of the literature have identified five psychosocial factors in particular which are related to CAD outcomes: depression, anxiety, stress, social support / isolation, and hostility / type A personality (Albus et al., 2005; Kuper, Marmot, & Hemingway, 2002; Smith & Ruiz, 2002).
These constructs have often been indentified as risk factors in separate investigations. This is limited for several reasons. First, these factors often co-occur (Lane, Carroll, Ring, Beevers, & Lip, 2002; Thurston & Kubzansky, 2007). Second, some of their symptoms or features, and the content of the assessment tools with which they are measured, may overlap (Suls & Bunde, 2005). Third, the prognostic importance of these factors cannot be compared. Suls and Bunde (2005) called for the examination of multiple psychosocial risk factors and their relationship to one another, as opposed to investigating individual risk factors (Bleil, Gianaros, Jennings, Flory, & Manuck, 2008; Rozanski et al., 2005; Suls & Bunde, 2005). There are only 4 studies to our knowledge (Ahern et al., 1990; Angerer et al., 2000; Frasure-Smith & Lesperance, 2003; Welin, Lappas, & Wilhelmsen, 2000) that have simultaneously tested more than 2 of these main psychosocial risk factors in relation to CAD prognosis, with only 1 study simultaneously testing the relationship between these 5 key psychosocial risk factors and CAD outcome (Frasure-Smith & Lesperance, 2003). The reason that such research has not been undertaken is multifactorial, but includes the need for consideration that the correlation among these constructs can lead to biased estimates and inflated standard errors in linear models. Indeed Frasure-Smith and Lesperance (2003) used factor analysis to test the importance of underlying independent psychosocial dimensions in relation to cardiac mortality. The purpose of this study was to build on their work by simultaneously testing the importance of these five constructs in relation to recurrent cardiac events or re-hospitalizations 9-months post-cardiac hospitalization, using uncorrelated measures and while controlling for other prognostic indicators.
Methods
Design & Procedure
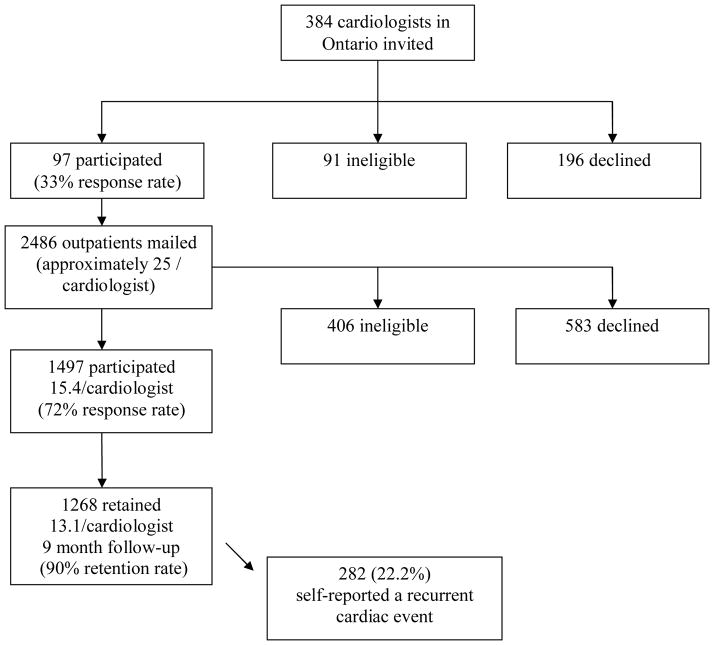
This study was a secondary analysis of data obtained from a larger longitudinal observational study examining access to cardiac rehabilitation (Grace et al., 2008). Upon receiving ethics approval from participating institutions, 384 non-pediatric cardiologists from major centres in Ontario were identified through the Canadian Medical Directory Online (www.mdselect.com) and were mailed an invitation to participate in the study. Consenting cardiologists’ offices were then visited by a research assistant to obtain a retrospective, consecutive sample of approximately 25 each of their recent CAD outpatients through coordination with the office administrative assistant. With informed consent by patients, basic clinical data was extracted from medical charts and patients were mailed a self-report survey including assessment of psychosocial variables. A second follow up survey was mailed to patients nine months later which assessed self-reported recurrent cardiac events and hospitalizations (see Figure 1).
Figure 1.
Participant recruitment flow diagram.
Participants
Ninety-seven cardiologists consented to participate in the study (14; 14.4% women, mean graduation year 1982 ± 8.57; 33% response rate). Ninety-one cardiologists were ineligible. Reasons for ineligibility included: treats only non-CAD patients (n=57; 62.6%), no outpatient practice (n=12; 13.2%), incorrect physician address/no longer in practice (n=9; 9.9%), retired from clinical practice (n=2; 2.2%) or other reasons such as the physician was on sabbatical or maternity leave, left the country, illness, or had an independent practice which was not covered under hospital ethics approval (n=11; 12.1%).
From the participating cardiologists, 1268 patients consented to participate in the study and were retained at follow up. Characteristics of participating, ineligible and declining patients, along with retained and declining participants at the follow-up assessment are reported elsewhere (Grace et al., 2008). CAD diagnosis was confirmed based on indication in patient chart of detailed history, focused physical examination, diagnostic ECG changes (i.e., Q waves, and/or ST-T segment changes), and/or troponin levels above the 99th percentile of normal. Patients who had undergone percutaneous coronary intervention (PCI) or coronary artery bypass grafting were also eligible.
Measures
Dependent Variable – Recurrent event
The dependent variable of interest was whether patients self-reported a recurrent cardiac event or procedure, or hospital or emergency room admission in the intervening 9 months on the follow-up survey. Participants were asked whether they had experienced a recurrent cardiac event or procedure (yes/no), and if yes to list it. The nature of recurrent cardiac events were reported in open-ended fashion, and coded. Similarly patients were asked to report the number of hospital or emergency room visits since the in-hospital survey was completed. A composite ‘recurrent event’ variable was computed to represent presence of any self-reported recurrent cardiac event, procedure or admission (yes/no).
Independent Variables
Age and sex among other clinical characteristics such as presence of dyslipidemia, hypertension, family history of cardiac disease, diabetes, obesity, and medications were extracted from patient charts. The baseline survey included forced-choice questions regarding sociodemographic characteristics and risk factors such as smoking status. In addition, the Duke Activity Status Index (DASI; Hlatky et al., 1989) was administered as an indicator of functional status. The DASI is a brief 12-item, self-administered survey. Participants were questioned about their ability to perform common activities of daily living, such as personal care, ambulation, household tasks, sexual function, and recreational activities, which are each associated with specific metabolic equivalents (METs). This is a valid and commonly used tool, which correlates highly with peak oxygen uptake (Nelson et al., 1991). Higher scores on the DASI correspond with a greater functional capacity.
Four psychometrically-validated psychosocial scales which are well-established and often used in the cardiac literature were also administered. These scales assess the five psychosocial factors previously identified as having a role in CAD prognosis (Hemingway & Marmot, 1999; Rozanski et al., 2005; Smith & Ruiz, 2002). Specifically, the Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983) was administered in the baseline survey. The ENRICHD Social Support Inventory (ESSI; Mitchell et al., 2003), the Cook-Medley Hostility Scale (HAS; Scherwitz, Perkins, Chesney, & Hughes, 1991), and the Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983) were administered in the follow-up survey. Details regarding each of these measures are provided below. Means, standard deviations, and Cronbach’s alphas for each of these scales are provided in Table 2.
Table 2.
Means and standard deviations of psychosocial variables by recurrent events.
| Recurrent Event (n=282) | No Recurrent Event (n=986) | Total (N=1268) | Cronbach’s Alpha | |
|---|---|---|---|---|
| Stress (PSS) | 20.60±5.47 | 19.02±5.35 | 19.38±5.42* | 0.41 |
| Depression Subscale (HADS) | 5.16±3.87 | 3.67±3.35 | 4.02±3.53* | 0.83 |
| Anxiety Subscale (HADS) | 6.58±4.38 | 5.12±3.92 | 5.44±4.06* | 0.87 |
| Social Support (ESSI) | 27.78±6.72 | 28.48±6.02 | 28.36±6.17 | 0.87 |
| Hostility (HAS) | 60.13±19.21 | 58.39±18.20 | 58.86±18.56 | 0.87 |
p < .001
PSS = Perceived Stress Scale
HADS = Hospital Anxiety and Depression Scale
ESSI = ENRICHD Social Support Inventory
HAS = Hostile Attitudes Scale
The PSS (Cohen et al., 1983) is used to examine the degree to which situations in one’s life are appraised as stressful. The 10-item version of this self-report scale shows adequate psychometric properties. Items are all scored on a 5–point Likert scale with responses ranging from 0 (never) to 5 (always), with higher total scores denoting greater levels of perceived stress.
The ESSI (Mitchell et al., 2003) was developed and validated in a randomized controlled intervention trial in post-MI patients. It includes items regarding structural, tangible and emotional aspects of support found to be predictive of outcome in cardiac patients. It is a 7-item scale, where 6 items are scored on a 5-point Likert scale ranging from 1 (none of the time) to 5 (all of the time). All of the items are then summed, with higher a score indicting greater levels of social support.
The HAS (Scherwitz et al., 1991) measures hostile attitudes. This scale has been reported to have adequate reliability and construct validity (Helmer, Ragland, & Syme, 1991; Smith & Frohm, 1985). The HAS consists of 18-items where responses are scored on a Likert scale which ranges from 1 (strongly disagree) to 7 (strongly agree). Higher scores are indicative of greater hostility.
The HADS (Zigmond & Snaith, 1983), a reliable and well-validated scale (Bjelland, Dahl, Haug, & Neckelmann, 2002), was used to assess anxiety and depressive symptoms. The HADS has been widely used as an anxiety and depression screening measure in hospital settings and has previously been used in cardiac research as it is perceived to assess depressive symptoms without confounding of somatic symptoms (Bjelland et al., 2002). The HADS is a 14-item self-report questionnaire which provides scores for two subscales: anxiety and depressive symptomatology. Each of the subscales were measured through 7 items that are rated on a 4-point Likert scale. Total scores for each subscale range from 0 to 21. A subscale score below 8 indicates the ‘normal’ range of subthreshold symptoms, a score of 9 to 10 represents moderate anxiety or depressive symptoms, while a score of 11 or greater represents severe symptoms (Zigmond & Snaith, 1983).
Statistical Analysis
The software package SPSS 15.0 (SPSS Inc., 2008) was used for statistical analyses. Sociodemographic and clinical differences between patients who reported a recurrent event and those who did not were assessed using student t-tests and chi-square tests, as appropriate.
Because the psychosocial factors investigated in this study are all highly correlated (rs ranged from .11 to .66, ps<.05), a maximum-likelihood factor analysis was conducted, including all items from the four scales. This ensures that the resulting factors are independent or orthogonal to each other, thus avoiding the problem of multicollinearity in the logistic regression analysis. This approach also increases the reliability and validity of each construct. The Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy (.93) and Bartlett’s test of sphericity (df = 1176, p≤0.001) supported the decision to use factor analysis. The number of factors retained for the analysis was based on scree plot analysis and the Kaiser criterion. The number of factors retained was verified by running the factor analysis with the number of factors above and below the break in the scree plot to ensure the analysis with the fewest cross-loadings was used. Varimax rotation was used to simplify and clean the structure of the data (Costello & Osborne, 2005) and factor loadings ≥ 0.4 were used for interpretation. Factor scores for each subject were then computed. These scores were representative of subjects’ predicted values for each factor and were treated as continuous variables.
Significant sociodemographic and clinical variables, and the psychosocial factor scores from the factor analysis were then entered into a logistic regression model to determine predictors of recurrent cardiac events or re-hospitalizations (yes/no). Sociodemographic and clinical variables shown to differentiate between patients experiencing a recurrent event were entered at the first step. All psychosocial factors scores were entered in the second step.
Results
Of the 1268 participants in the study, 282 (22.6%) reported experiencing a recurrent cardiac event (n=115; 40.8%), or hospital/emergency room readmission (n=167; 59.2%) during the 9 months between the baseline and follow-up surveys. Recurrent cardiac events reported by participants were as follows: PCI (n=26;9.2%), dysrhythmias (n=11;3.9%), angina (n=9;3.2%), myocardial infarction (n=8;2.8%), coronary artery bypass grafting (n=8; 2.8%), pacemaker implantation (n=8;2.8%), defibrillator implantation (n=6;2.1%), heart failure (n=6;2.1%), severe chest tightness/dizziness (n=4;1.4%), stroke or transient ischemic attack (n=4;1.4%), and cardiac ablation (n=4; 1.4%). Nine (3.2%) patients reported two or more cardiac events and/or procedures, and 12 (4.3%) patients reported other cardiac events or procedures.
Participant characteristics are reported in Table 1. Participants who reported a recurrent event (including admissions) were significantly more likely to be female, and significantly less likely to be employed than participants who did not report a recurrent event or hospitalization. Clinical characteristics of participants were also examined. Those with diabetes mellitus and lower functional status were significantly more likely to have experienced a recurrent event.
Table 1.
Baseline characteristics of retained participants by occurrence of recurrent event.
| Recurrent Event (n=282, 22.2%) | No Recurrent Event (n=986, 77.8%) | Total (N=1268) | |
|---|---|---|---|
| Sociodemographic Characteristics | |||
| Age (mean±SD) | 66.94±11.56 | 66.02±11.05 | 66.28±11.16 |
| Sex (% female) | 98 (34.8%) | 255 (26.4%) | 358 (28.2%)*** |
| Marital Status (% Married) | 192 (68.6%) | 705 (73.4%) | 910 (72.3%) |
| Work Status (% FT/PT) | 75 (26.8%) | 327 (34.0%) | 406 (32.3%)* |
| Education (% > HS) | 142 (51.1%) | 523 (54.9%) | 670 (53.7%) |
| Family Income (>$50,000CAD/year) | 113 (44.5%) | 441 (49.8%) | 560 (48.5%) |
| Ethnicity (%white) | 235 (83.3%) | 843 (87.2%) | 1094 (86.3%) |
| Clinical Characteristics | |||
| Dyslipidemia (%yes) | 158 (56.0%) | 578 (59.8%) | 748 (59.0%) |
| Hypertension (%yes) | 164 (58.2%) | 599 (62.2%) | 773 (61.2%) |
| Family history of heart disease (%yes) | 153 (54.3%) | 579 (59.9%) | 745 (58.8%) |
| Diabetes Mellitus (%yes) | 87 (30.9%) | 225 (23.3%) | 317 (25.1%)* |
| Obesity (%yes) | 120 (43.5%) | 445 (46.5%) | 574 (46.0%) |
| Activity Status (mean±SD) | 31.72 ± 15.81 | 38.72 ± 15.54 | 36.40±16.20*** |
| Smoking Status (%current) | 22 (7.9%) | 80 (8.2%) | 102 (8.1%) |
| Beta-Blockers (%yes) | 222 (80.4%) | 736 (78.5%) | 976 (79.2%) |
p < .05;
p<= .01;
p < .001
Percentages take into account missing data for some variables.
SD = Standard Deviation
FT/PT = Full Time/Part Time
HS = High School
CAD = Canadian dollars
Mean scores, standard deviations and Cronbach’s alphas for the five psychosocial variables are presented in Table 2 by recurrence / re-hospitalization. Patients who experienced a recurrent event had significantly higher HADS Anxiety, HADS Depression and PSS scores compared to those who did not report a recurrent event.
A table reporting the factor loadings from the rotated component matrix of the maximum-likelihood factor analysis of all items from the five scales is available as supplementary material for interested readers at www.yorku.ca/sgrace. A six-factor solution was extracted and explained 50.24% of the total variance and 43.78% of the common variance in scores. Based on the items that loaded on each factor, the six factors were labeled as: (1) hostility, (2) social support, (3) stress, (4) depressive symptoms, (5) anxiety, and lastly (6) resilience. Items from each scale remained intact, except in the case of the PSS, where two factors resulted. Cronbach’s alphas for each of the factors were as follows: hostility, 0.87; social support, 0.87; stress, 0.74; depressive symptoms, 0.84; anxiety, 0.87; and resilience, 0.78.
A logistic regression analysis predicting self-reported recurrent event or hospitalization with sex, work status, activity status and diabetes (first block) and the factor scores (second block) was conducted. Both blocks of the model were significant (p<.001 and p=.04, respectively), as was the overall model (p<.001). Unadjusted and adjusted odds ratios (OR) with 95% confidence intervals (CI) are displayed in Table 3. After adjustment, lower activity status and anxiety were significantly associated with reporting a recurrent event or re-hospitalization, with a trend for depressive symptoms.
Table 3.
Unadjusted and adjusted Odds Ratios and 95% Confidence Intervals for psychosocial factor scores in relation to self-reported recurrent event, N=1268.
| B | Unadjusted OR (95% CI) | B | Adjusted OR (95% CI) | |
|---|---|---|---|---|
| Female Sex | 0.397 | 1.49 (1.12–1.98)** | -.0.042 | .96 (.67–1.37) |
| Work Status (FT/PT) | 0.343 | 1.41 (1.05–1.90)* | 0.165 | 1.18 (.83–1.68) |
| Functional Capacity (DASI) | −0.029 | .97 (.96-.98)*** | −0.019 | .98 (.97-.99)*** |
| Diabetes | 0.346 | 1.41 (1.05–1.91)* | 0.202 | 1.22 (.86–1.75) |
| Hostility | 0.08 | 1.08 (.92–1.27) | 0.071 | 1.07 (.91–1.27) |
| Social Support | −0.043 | .96 (.82–1.11) | −0.055 | .95 (.81–1.11) |
| Stress | 0.127 | 1.14 (.96–1.34) | 0.103 | 1.11 (.94–1.31) |
| Depressive Symptoms | 0.326 | 1.39 (1.18–1.63)*** | 0.153 | 1.17 (.98–1.40) |
| Anxiety | 0.236 | 1.27 (1.07–1.49)** | 0.204 | 1.23 (1.03–1.46)* |
| Resilience | 0.067 | 1.07 (.90–1.28) | −0.036 | .97 (.80–1.16) |
OR = Odds Ratio
CI = Confidence Interval
FT/PT= full-time or part-time
DASI = Duke Activity Status Index
p≤0.05;
p≤0.01;
p≤0.001
Adjusted R2 = 0.062
Discussion
This study simultaneously compared key psychosocial predictors of recurrent events in a broad sample of cardiac patients, namely social support, stress, hostility, resilience, anxiety and depressive symptoms. A review by Suls and Bunde (2005) urged the discontinuation of testing independent risk factors for their prognostic importance, and highlighted the importance of examining multiple risk factors simultaneously. The current study is the first study to our knowledge to compare key psychosocial constructs simultaneously by using factor analysis of individual items of well-established scales to ensure the constructs are distinct and uncorrelated. Such a test would generally be contraindicated due to multicollinearity concerns, but by using orthogonal factor scores this problem was overcome. Other studies have dichotomized scores to overcome issues of multicollinearity (Angerer et al., 2000; Welin et al., 2000), but this reduces variability.
Results from adjusted analyses revealed that cardiac patients with greater anxiety may be more likely to experience a recurrent event than patients without elevated symptoms, with a similar trend for depressive symptoms. None of the other psychosocial factors were significantly related to outcome. These results are somewhat inconsistent with the only other study of all five psychosocial factors (Frasure-Smith & Lesperance, 2003). They showed that depressive symptoms as assessed by the Beck Depression Inventory and anxiety as assessed by the State-Trait Anxiety Inventory were both significantly related to long-term cardiac mortality, although these relationships did not hold after adjustment for clinical variables. Clearly further investigation into other psychosocial constructs related to cardiac prognosis is needed. The use of structural equation modeling, a statistical technique which reduces measurement error in order to estimate true relationships among constructs, including latent variables, may advance our knowledge in this regard.
Results of the factor analysis revealed that for all but one scale, items from each measure remained intact. This lends credence to the psychometric properties of these scales and their discriminant validity. However, the factor analysis revealed a sixth factor, which we interpreted as resilience. This factor was derived from items in the PSS. Indeed there has been interest in the role of protective psychological factors, such as resilience, in CAD prognosis (Chen et al., 2006; Garnefski, Kraaij, Schroevers, & Somsen, 2008; Petrie, Buick, Weinman, & Booth, 1999). This study however suggests that such protective factors are not significantly related to self-reported recurrent events. Overall, the findings from this factor analysis suggest that perhaps these psychosocial constructs are not overlapping, and perhaps a smaller number of factors cannot adequately account for the association between psychological distress and cardiovascular disease prognosis. Clearly, replication is warranted.
These results are particularly important if one considers that anxiety and depression are common and often co-occur (Gorman, 1996; Lane et al., 2002). For instance, depression has been reported among 15–30% of heart attack survivors (Thombs et al., 2006), while anxiety has been reported in approximately one-third of cardiac patients at the time of their event (Grace, Abbey, Irvine, Shnek, & Stewart, 2004). Moreover, several studies have shown that approximately 50% of patients with depression also show symptoms of anxiety (Lane et al., 2002). Future research is warranted to test whether the presence of both anxiety and depressive symptoms has an additive or synergistic effect on prognosis.
Overall results suggest that the HADS is a useful tool to identify patients who may be at increased risk of experiencing a recurrent cardiac event or hospitalization. However, mean scores among patients who reported recurrent events did not meet clinical cut-offs indicative of elevated symptomatology. Indeed, a dose-response relationship between depressive symptoms and outcomes has been established (Lesperance, Frasure-Smith, Talajic, & Bourassa, 2002). Future research should aim to identify more conservative clinical cut-offs, or to identify cut-offs specific to the co-occurrence of depressive and anxiety symptoms for clinical purposes.
The identification of cardiac patients experiencing psychosocial distress remains a worthy goal, however whether all of these constructs have prognostic significance is questionable. Moreover, there is as of yet no evidence that treating symptoms of elevated anxiety or depression results in better outcomes for cardiac patients (Berkman et al., 2003; Glassman et al., 2002).
Limitations
There are several limitations to this study, related to design, measurement and generalizability. With regard to design, the psychosocial scales were administered at 2 different time points. In particular, assessment of social support, hostility, anxiety and depressive symptoms was concurrent with outcome assessment. Thus, this analysis was cross-sectional in design and no causal conclusions can be drawn. Cautious interpretation of the results is advocated, considering that the direction of effect cannot be determined. Clearly, the recurrence of a cardiac event is often a stressful experience which may itself promote increased depression and anxiety. With regard to measurement, both the dependent and independent variables were assessed via self-report, which is subject to bias. In future studies, the use of clinical interviews to assess psychosocial variables such as depression and anxiety according to diagnostic criteria, and use of objective means to ascertain recurrent events such as verification through administrative data is warranted.
Moreover, replication is warranted with other measures of social support, stress and hostility in particular to determine whether the results are a function of the measures administered. For instance, assessment of specific domains such as job stress / strain or marital stress should be conducted as those have been shown to have a stronger link to outcome than a general stress measure. In addition, this study did not compare an exhaustive list of factors shown in the literature to relate to outcome in cardiac samples, such as Type D personality (Pedersen & Denollet, 2003). While in this study patients were asked to report recurrent cardiac events and hospital admissions, future studies may wish to examine the relation of psychosocial factors to a more homogeneously-defined set of major adverse clinical events tied to biologically-plausible mechanistic explanations for the linkage to the psychosocial factors.
Finally, with regard to generalizability, there may be concern due to response bias in the sample, most notably due to the low physician response rate (33%). A study of general practitioners in England reported survey non-responders to be older, less likely to be involved in teaching and potentially having different knowledge, attitudes or beliefs regarding the research outcome of interest (Stocks & Gunnell, 2000). However, the preponderance of literature regarding physician response rates does quell concern over threats to generalizability. In a review of 24 studies, it was demonstrated that non-response bias may be less of a concern in physician samples (Kellerman & Herold, 2001). Survey representativeness was established by comparing the characteristics of physician respondents to the first mailing, to respondents to subsequent mailings and late respondents (considered to be a proxy for non-respondents). Studies in the review found little difference in income, area and type of practice, or physician gender and age among responders to early versus late mailings. This lead Kellerman and Herold to conclude that “physicians as a group are more homogeneous regarding knowledge, training attitudes, and behavior than the general population. Variation that does exist among physicians may not be as associated with willingness to respond or survey content as in the general population…” (p. 65). In addition, this study was a secondary analysis, and while cardiologists were informed that patient surveys included psychosocial scales, the purpose of the larger study was to understand secondary prevention. Therefore, the low response rate of cardiologists may not have greatly affected the generalizability of results.
The overall results of this study suggest that psychosocial factors may play a role in cardiac disease progression. Anxiety, and perhaps depressive symptoms, may be the more important psychosocial risk factors to consider in the prognosis of CAD patients when compared to stress, hostility and social isolation. Future replication is needed using sophisticated statistical approaches to test these multiple psychosocial constructs using different measurement tools in relation to hard cardiac endpoints before we can draw definitive conclusions about the role of psychosocial factors in cardiac prognosis.
Supplementary Material
Acknowledgments
This study was funded by the Canadian Institutes of Health (CIHR) grant # MOP-74431. K Grewal is supported by a CIHR Canada Graduate Scholarship Masters Award, S Gravely-Witte is supported by a CIHR doctoral fellowship, and S Grace is supported by a CIHR New Investigator Award.
Footnotes
There are no conflicts of interest to disclose.
Contributor Information
Keerat Grewal, York University, Faculty of Health, 4700 Keele St., Toronto, Ontario, M3J 1P3.
Shannon Gravely-Witte, York University, Faculty of Health, 4700 Keele St., Toronto, Ontario, M3J 1P3, +1 (416) 736-2100 x.20575, Fax: +1 (416) 736-5774.
Donna E. Stewart, University Health Network, Toronto General Hospital, Women’s Health Program, EN7-230, +1 (416) 340-4800, +1 (416) 340-4185.
Sherry L. Grace, York University, Faculty of Health, 368 Bethune, 4700 Keele St, Toronto, ON M3J 1P3, Phone: +1 (416) 736-2100 x.22364, Fax: +1 (416) 736-5774.
References
- Ahern DK, Gorkin L, Anderson JL, Tierney C, Hallstrom A, Ewart C, et al. Biobehavioral variables and mortality or cardiac arrest in the cardiac arrhythmia pilot study (CAPS) The American Journal of Cardiology. 1990;66(1):59–62. doi: 10.1016/0002-9149(90)90736-K. [DOI] [PubMed] [Google Scholar]
- Albus C, De Backer G, Bages N, Deter HC, Herrmann-Lingen C, Oldenburg B, et al. Psychosocial factors in coronary heart disease - scientific evidence and recommendations for clinical practice. Gesundheitswesen. 2005;67(1):1–8. doi: 10.1097/01.hjr.0000116823.84388.6c. [DOI] [PubMed] [Google Scholar]
- Angerer P, Siebert U, Kothny W, Muhlbauer D, Mudra H, von Schacky C. Impact of social support, cynical hostility and anger expression on progression of coronary atherosclerosis. Journal of the American College of Cardiology. 2000;36(6):1781–1788. doi: 10.1016/S0735-1097(00)00944-X. [DOI] [PubMed] [Google Scholar]
- Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: A meta-analysis. Psychosomatic Medicine. 2004;66(6):802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: The enhancing recovery in coronary heart disease patients (ENRICHD) randomized trial. The Journal of the American Medical Association. 2003;289(23):3106–3116. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale. an updated literature review. Journal of Psychosomatic Research. 2002;52(2):69–77. doi: 10.1016/S0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- Bleil ME, Gianaros PJ, Jennings JR, Flory JD, Manuck SB. Trait negative affect: Toward an integrated model of understanding psychological risk for impairment in cardiac autonomic function. Psychosomatic Medicine. 2008;70(3):328–337. doi: 10.1097/PSY.0b013e31816baefa. [DOI] [PubMed] [Google Scholar]
- Chen R, Kumar S, Timmis A, Feder G, Yaqoob MM, Hemingway H. Comparison of the relation between renal impairment, angiographic coronary artery disease, and long-term mortality in women versus men. The American Journal of Cardiology. 2006;97(5):630–632. doi: 10.1016/j.amjcard.2005.09.102. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- Costello AB, Osborne JW. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Practical Assessment Research & Evaluation. 2005;10(7):1–9. [Google Scholar]
- Frasure-Smith N, Lesperance F. Depression and other psychological risks following myocardial infarction. Archives of General Psychiatry. 2003;60(6):627–636. doi: 10.1001/archpsyc.60.6.627. [DOI] [PubMed] [Google Scholar]
- Garnefski N, Kraaij V, Schroevers MJ, Somsen GA. Post-traumatic growth after a myocardial infarction: A matter of personality, psychological health, or cognitive coping? Journal of Clinical Psychology in Medical Settings. 2008;15(4):270–277. doi: 10.1007/s10880-008-9136-5. [DOI] [PubMed] [Google Scholar]
- Glassman AH, O’Connor CM, Califf RM, Swedberg K, Schwartz P, Bigger JT, Jr, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. Journal of the American Medical Association. 2002;288(6):701–709. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- Gorman JM. Comorbid depression and anxiety spectrum disorders. Depression and Anxiety. 1996;4(4):160–168. doi: 10.1002/(SICI)1520-6394(1996)4:4<160::AID-DA2>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- Grace SL, Gravely-Witte S, Brual J, Suskin N, Higginson L, Alter D, et al. Contribution of patient and physician factors to cardiac rehabilitation referral: A prospective multi-level study. Nature Clinical Practice Cardiovascular Medicine. 2008;5(10):653–662. doi: 10.1038/ncpcardio1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace SL, Abbey SE, Irvine J, Shnek ZM, Stewart DE. Prospective examination of anxiety persistence and its relationship to cardiac symptoms and recurrent cardiac events. Psychotherapy and Psychosomatics. 2004;73(6):344–352. doi: 10.1159/000080387. [DOI] [PubMed] [Google Scholar]
- Helmer DC, Ragland DR, Syme SL. Hostility and coronary artery disease. American Journal of Epidemiology. 1991;133(2):112–122. doi: 10.1093/oxfordjournals.aje.a115850. [DOI] [PubMed] [Google Scholar]
- Hemingway H, Marmot M. Evidence based cardiology: Psychosocial factors in the aetiology and prognosis of coronary heart disease. Systematic review of prospective cohort studies. British Medical Journal. 1999;318(7196):1460–1467. doi: 10.1136/bmj.318.7196.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hlatky MA, Boineau RE, Higginbotham MB, Lee KL, Mark DB, Califf RM, et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index) The American Journal of Cardiology. 1989;64(10):651–654. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- Kellerman SE, Herold J. Physician response to surveys. A review of the literature. American Journal of Preventive Medicine. 2001;20(1):61–67. doi: 10.1016/S0749-3797(00)00258-0. [DOI] [PubMed] [Google Scholar]
- Kuper H, Marmot M, Hemingway H. Systematic review of prospective cohort studies of psychosocial factors in the etiology and prognosis of coronary heart disease. Seminars in Vascular Medicine. 2002;2(3):267–314. doi: 10.1055/s-2002-35401. [DOI] [PubMed] [Google Scholar]
- Lane D, Carroll D, Ring C, Beevers DG, Lip GYH. The prevalence and persistence of depression and anxiety following myocardial infarction. British Journal of Health Psychology. 2002;7(1):11–21. doi: 10.1348/135910702169321. [DOI] [PubMed] [Google Scholar]
- Lesperance F, Frasure-Smith N, Talajic M, Bourassa MG. Five-year risk of cardiac mortality in relation to initial severity and one-year changes in depression symptoms after myocardial infarction. Circulation. 2002;105(9):1049–1053. doi: 10.1161/hc0902.104707. [DOI] [PubMed] [Google Scholar]
- Lett HS, Blumenthal JA, Babyak MA, Sherwood A, Strauman T, Robins C, et al. Depression as a risk factor for coronary artery disease: Evidence, mechanisms, and treatment. Psychosomatic Medicine. 2004;66(3):305–315. doi: 10.1097/01.psy.0000126207.43307.c0. [DOI] [PubMed] [Google Scholar]
- Mitchell PH, Powell L, Blumenthal J, Norten J, Ironson G, Pitula CR, et al. A short social support measure for patients recovering from myocardial infarction: The ENRICHD Social Support Inventory. Journal of Cardiopulmonary Rehabilitation. 2003;23(6):398–403. doi: 10.1097/00008483-200311000-00001. [DOI] [PubMed] [Google Scholar]
- Nelson CL, Herndon JE, Mark DB, Pryor DB, Califf RM, Hlatky MA. Relation of clinical and angiographic factors to functional capacity as measured by the Duke Activity Status Index. The American Journal of Cardiology. 1991;68(9):973–975. doi: 10.1016/0002-9149(91)90423-I. [DOI] [PubMed] [Google Scholar]
- Organization for Economic Cooperation and Development. International mortality data. 2001. [Google Scholar]
- Pedersen SS, Denollet J. Type D personality, cardiac events, and impaired quality of life: A review. European Journal of Cardiovascular Prevention and Rehabilitation. 2003;10(4):241–248. doi: 10.1097/00149831-200308000-00005. [DOI] [PubMed] [Google Scholar]
- Petrie KJ, Buick DL, Weinman J, Booth RJ. Positive effects of illness reported by myocardial infarction and breast cancer patients. Journal of Psychosomatic Research. 1999;47(6):537–543. doi: 10.1016/S0022-3999(99)00054-9. [DOI] [PubMed] [Google Scholar]
- Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: The emerging field of behavioral cardiology. Journal of the American College of Cardiology. 2005;45(5):637–651. doi: 10.1016/S1073-5437(08)70272-9. [DOI] [PubMed] [Google Scholar]
- Scherwitz L, Perkins L, Chesney M, Hughes G. Cook-Medley hostility scale and subsets: Relationship to demographic and psychosocial characteristics in young adults in the CARDIA study. Psychosomatic Medicine. 1991;53:36–49. doi: 10.1097/00006842-199101000-00004. [DOI] [PubMed] [Google Scholar]
- Smith TW, Frohm KD. What’s so unhealthy about hostility? Construct validity and psychosocial correlates of the Cook and Medley Ho scale. Health Psychology. 1985;4(6):503–520. doi: 10.1037/0278-6133.4.6.503. [DOI] [PubMed] [Google Scholar]
- Smith TW, Ruiz JM. Psychosocial influences on the development and course of coronary heart disease: Current status and implications for research and practice. Journal of Consulting and Clinical Psychology. 2002;70(3):548–568. doi: 10.1037/0022-006X.70.3.548. [DOI] [PubMed] [Google Scholar]
- SPSS Inc. SPSS for Windows. SPSS Inc; Chicago, Illinois: 2008. [Google Scholar]
- Stocks N, Gunnell D. What are the characteristics of general practitioners who routinely do not return postal questionnaires: A cross sectional study. Journal of Epidemiology and Community Health. 2000;54(12):940–941. doi: 10.1136/jech.54.12.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suls J, Bunde J. Anger, anxiety, and depression as risk factors for cardiovascular disease: The problems and implications of overlapping affective dispositions. Psychological Bulletin. 2005;131(2):260–300. doi: 10.1037/0033-2909.131.2.260. [DOI] [PubMed] [Google Scholar]
- Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, et al. Prevalence of depression in survivors of acute myocardial infarction. Journal of General Internal Medicine. 2006;21(1):30–38. doi: 10.1111/j.1525-1497.2005.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thurston RC, Kubzansky LD. Multiple sources of psychosocial disadvantage and risk of coronary heart disease. Psychosomatic Medicine. 2007;69(8):748–755. doi: 10.1097/PSY.0b013e31815772a3. [DOI] [PubMed] [Google Scholar]
- van Melle JP, de Jonge P, Spijkerman TA, Tijssen JG, Ormel J, van Veldhuisen DJ, et al. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: A meta-analysis. Psychosomatic Medicine. 2004;66(6):814–822. doi: 10.1097/01.psy.0000146294.82810.9c. [DOI] [PubMed] [Google Scholar]
- Welin C, Lappas G, Wilhelmsen L. Independent importance of psychosocial factors for prognosis after myocardial infarction. Journal of Internal Medicine. 2000;247(6):629–639. doi: 10.1046/j.1365-2796.2000.00694.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Measuring the global burden of disease and risk factors, 1990–2001. In: Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL, editors. Global burden of disease and risk factors. New York: Oxford University Press; 2006. [Google Scholar]
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.