Abstract
The most prevalent non-communicable disease globally, namely cardiovascular disease (CVD), is also the leading cause of mortality, with over 80% of the deaths occurring in low- and middle-income countries. To lessen the impact of CVDs on individuals and societies, a comprehensive approach is needed. Cardiac rehabilitation (CR) involves delivery of structured exercise, education and risk reduction, in a cost-effective manner. Robust evidence demonstrates it reduces mortality up to 25%, improves functional capacity, as well as decreases re-hospitalization. Despite its benefits, and clinical practice guideline recommendations to refer cardiac patients, CR programs are grossly under-used. Worldwide, there is low availability of CR; only 38.8% of countries globally have CR programs. Specifically, 68.0% of high-income and 23% of LMICs (28.2% for middle- and 8.3% for low-income countries) have CR. CR density estimates ranged from 1 program per 0.1–6.4 million inhabitants. CR availability is much lower than that of other evidence-based secondary prevention therapies, such as revascularization and pharmacological therapies. Multi-level strategies to augment CR capacity and availability at national and international levels such as supportive public health policies, systematic referral strategies, and alternative models of delivery are needed.
Introduction
Cardiovascular disease (CVD) is the most prevalent non-communicable disease and the leading cause of mortality globally.1 With increasing CVD prevalence, the burden of CVD is growing significantly, particularly in low- and middle-income countries (LMICs)2,3 (Box 1). Indeed, more than 80% of the CVD deaths occur in LMICs.1 Over the next few decades, 23 million people per year will die due to CVD.1,4
Box 1. Definitions.
High-, middle-, and low-income countries
Countries are classified according to 2012 Gross National Income per capita.
Low-income: $1,035 or less;
Middle-income: $1,036 – $12,615
Lower middle income: $1,036 – $4,085
Upper middle income: $4,086 – $12,615
High-income: $12,616 or more
Source: The World Bank.3 http://data.worldbank.org/about/country-classifications
Disability Adjusted Life Years (DALYS)
The World Health Organization defines DALYs as “The sum of years of potential life lost due to premature mortality and the years of productive life lost due to disability.” World Health Organization. 7
According to the World Economic Forum,4 in 2010, there were 62.5 million new cases of CVD, of which 24.2 million were attributed to ischemic heart disease (Table 1). By 2030, the number of new CVD cases is expected to grow to 84 million, of which 32.3 million will be ischemic heart disease cases.4
Table 1.
Cardiovascular disease incidence and cost (in 1000s) worldwide
| Year | Total cost (billions of US$) | CHF incidence | IHD incidence | Stroke incidence |
|---|---|---|---|---|
| 2010 | 863 | 10,072 | 24,167 | 28,299 |
| 2015 | 906 | 10,821 | 25,933 | 30,370 |
| 2020 | 957 | 11,830 | 28,284 | 33,122 |
| 2025 | 1,002 | 12,754 | 30,369 | 35,571 |
| 2030 | 1,044 | 13,637 | 32,339 | 37,886 |
| Total, all years, 2010–2030 | 20,032 |
Source: (Bloom et al., 2011) 4
Abbreviations: IHD, ischemic heart disease; CHF, congestive heart failure; US, United States
Patients with established CVD have a high risk of consequent major events, such as fatal and non-fatal myocardial infarction.5 Accordingly, CVD is also the leading cause of disability globally.6 It is responsible for 10% disability-adjusted life years (DALYs; Box 1 for definition7) lost worldwide, accounting for 10% of the DALYs lost in LMICs, and 18% of DALYs lost in high-income countries.1 For example, 47 million DALYs globally were lost because of coronary heart disease (CHD), and this figure is expected to increase to 82 million DALYs in 2020.8
With regard to CVD prevalence worldwide, currently, there is no standardized source for this information. However, Murray and Lopez (1996)9 estimated the prevalence of acute myocardial infarction in 1990 as 501,000 cases worldwide. Recently, the Global Burden of Disease Study 2010 estimated the global prevalence of angina due to ischemic heart disease as 111.7 million individuals or 1.62% of the total world’s population.10 To provide more insight about the number of individuals living with CVD, available data from selected high and middle-income countries are shown in Table 2. Caution however is warranted in interpreting and comparing these estimates, due to variability in prevalence operationalization.
Table 2.
Prevalence of cardiovascular disease for selected countries
| Country (year) | Prevalence (million) | Disease |
|---|---|---|
| Australia (2009)11 | 3.7 | CVD |
| Brazil (2008)12 | 6.7 | heart disease |
| Canada (2007)13 | 1.3 | heart disease |
| China (2010)14 | 235 | CVD |
| India (NA)15 | 45 | CHD |
| United States (2010)16 | 15.4 | CHD |
Abbreviations: CHD, coronary heart disease; CVD, cardiovascular disease; NA, not available.
As a global response to the emerging non-communicable disease burden including CVD, the World Health Organization (WHO) has set a global target for reduction of “premature deaths from non-communicable diseases by 25% by 2025”.17 All 194 WHO Member States endorsed this target during the 65th World Health Assembly in 2012.17 In its’ Global Action Plan for the Prevention and Control of Non-communicable Diseases 2013–2020,18 the WHO underlines the need for rehabilitation, including cardiac rehabilitation (CR). CR is forwarded as a central strategy to address CVD risk factors, such as obesity and physical inactivity, and to restore loss of function. It is also forwarded to reduce the consequences of CVD, slow or stop health deterioration, fasten hospital dismissal, and improve quality of life.18 To lessen the impact of CVDs on individuals and societies, a comprehensive approach such as that is offered in CR is needed.
Cardiac Rehabilitation
CR is a multidisciplinary approach designed to stabilize, slow, or even promote regression of CVD.19 The World Health Organization (WHO) defines CR as the “sum of activities required to influence favourably the underlying cause of the disease, as well as to provide the best possible physical, mental and social conditions, so that the patients may, by their own efforts, preserve or resume when lost, as normal a place as possible in the community”.20 As a means of secondary and even tertiary prevention, for the purposes of this review, we refer to CR delivered in the outpatient setting.
National and international associations, such as the American Association of Cardiovascular and Pulmonary Rehabilitation21 as well as the European Association of Cardiovascular Prevention and Rehabilitation,22 have established the core components of CR. These include baseline assessment of patients, physical activity training and counselling, nutritional counselling, management of risk factors (i.e., dyslipidemia, hypertension, obesity, diabetes mellitus, and smoking), as well as psychosocial interventions and counselling.21
The components delivered work to reduce cardiovascular risk, promote and maintain healthy behaviors and active lifestyles, improve quality of life, and reduce disability.21 Robust evidence demonstrates that CR participation reduces mortality by up to 25% over the subsequent several years when compared to usual care.23–28 The only risks to CR use are associated with exercise, and are low.
Population indicated for CR
According to clinical practice guidelines from reputed cardiovascular societies around the world, CR is recommended for patients with a primary diagnosis of one or a combination of the following: myocardial infarction, angina, heart failure; as well as following interventions, namely coronary artery bypass graft surgery, percutaneous coronary intervention, and heart or heart/lung transplant.29,30–32 Though we are unable to report prevalence of these CVD indications worldwide, several millions of patients, such as the 111.7 million with angina worldwide,10 are candidates for CR. These alarming figures demonstrate the scope of the need for CR services.
Given the current and expected future increase in CVD trends, CR capacity will need to be high to meet such demand. Consistent with the current international focus on CVD prevention and control, this review aims to describe the availability of CR in both high-income countries and LMICs, and to juxtapose this in the context of the accessibility of CR in these countries.
Availability of CR by country income classification
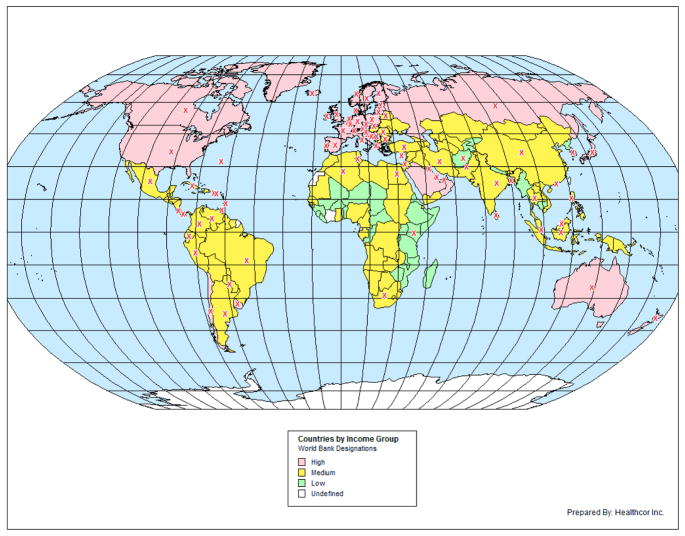
An extensive search (Box 2) of peer-reviewed and grey literature was undertaken to identify the presence of CR in all countries as recognized by the World Bank, and by their income classification (Box 1). Results are shown in Figure 1.
Box 2. Review criteria.
In October 2013, Medline, Excerpta Medica Database (EMBASE), and Google Scholar were searched for relevant articles. The authors started the search with cardiac rehabilitation surveys, meta-analyses, and reviews to report availability of CR and literature in high-, middle-, and low-income countries. The authors’ also used their personal collections of journal articles and references from key articles to write the review. Grey literature was used by searching CR by country, and searching services provided by hospitals within countries using the Google search engine to find CR Web sites.
Figure 1.
Availability of cardiac rehabilitation in high-, middle-, and low-income countries
Note. Countries coloured white do not exist in the current World Bank’s income-group list, as of January 2014.
CR availability in high-income countries
National and regional surveys, such as the CARINEX Survey,33 and the European CR Inventory Survey34 have described CR availability in many high-income countries. Of the 75 globally, results showed CR services are available in 51 (68.0%). These are Australia,35 Austria,33 Bahrain,36 Barbados,37 Belgium,34 Bermuda,38 Brunei Darussalam,39 Canada, 40 Channel Islands,41 Chile,42 Croatia,34 Cyprus,34 Czech Republic,43 Denmark,44 Estonia,43 Finland,34 France,45 Germany,46 Greece,47 Hong Kong,48 Iceland,34 Ireland,33 Isle of Man,49 Israel,50 Italy,51 Japan,52 Korea/Republic,53 Kuwait,54 Latvia,55 Lithuania,34 Luxembourg,34 Netherlands,34 New Zealand,56 Norway,57 Poland,34 Portugal,34 Puerto Rico,58 Qatar,59 Russian Federation,34 Singapore,60 Slovak Republic,34 Slovenia,61 Spain,33 Sweden,34 Switzerland,62 Trinidad and Tobago,63 United Arab Emirates,64 United Kingdom,65 United States,66 Uruguay,42 and the Virgin Islands (U.S.). 67
CR availability in middle-income countries
The most comprehensive data on the availability of CR in middle-income countries were published in two regional surveys: the Latin America and the Caribbean survey with 14 participating countries,68 and the South American survey with 9 participating countries.42 Moreover, a recent review69 explored CR services in LMICs and reported they were available in 22.1%. Of the 103 middle-income countries globally, this search revealed CR services exist in 29 (28.2%) countries (Figure 1). These were: Algeria,70 Argentina,42 Belarus,69 Bosnia And Herzegovina,69 Brazil,68 Bulgaria,69 China,71 Colombia,68 Costa Rica,69 Cuba,69 Ecuador,42 Egypt,72 India,73 Indonesia,74 Iran,75 Malaysia,69 Mexico,68 Pakistan,76 Panama,69 Paraguay,42 Peru,68 Philippines,43 Romania,77 South Africa,78 Sri Lanka,69 Thailand,69 Tunisia,79 Turkey,80 and Venzuela.42
CR availability in low-income countries
Of the 36 low-income countries globally, CR services were available in only 3 (8.3%). These were: Afghanistan,81 Bangladesh,82 and Kenya.83
Thus, overall, CR is available in 83 out of the 214 (38.8%) countries worldwide. CR services are available in only 23% of the LMICs, where 80% of CVD deaths occur84 underlining the insufficient supply of CR in countries with the greatest cardiovascular burden. There is an inverse relationship between the availability of CR and the number of patients indicated for CR therapy.
Density of CR
CR density, expressed as number of CR programs per inhabitant (population density), was used as a crude estimate of the number of indicated patients who may have a spot in a CR program by country. While it would be more informative to report the number of indicated patients per CR program (i.e., CR capacity),42,51 unfortunately as outlined above, country-level CVD prevalence data is not available for many countries. Moreover, this approach is limited by the variation in number of patients treated annually across CR programs (e.g., range of 75–232 patients/program in a US study).85 Finally, there is no accepted density threshold which could indicate sufficient CR capacity. There is a published position statement recommending a benchmark of 70% CR enrolment40; however, the translation of this recommendation into a density value has yet to be undertaken. Still, in line with previous research,42 the density of CR is presented and for the first time, compared across regions of the world (Table 3).
Table 3.
Density of cardiac rehabilitation programs by country and income classification
| Country | CR Density (million inhabitants/program) |
|---|---|
| High-income | |
| Chile*42 | 1.7 |
| Italy51 | 0.3 |
| United States86 | 0.1 |
| Uruguay*42 | 0.3 |
| Middle-income | |
| Brazil42 | 4.9 |
| Colombia42 | 0.9 |
| Ecuador42 | 2.9 |
| Paraguay42 | 6.4 |
| Peru42 | 3.1 |
| Venezuela42 | 3.3 |
| Low-income ** | |
| Afghanistan81 | 29.1 |
| Bangladesh82 | 164.4 |
| Kenya83 | 40.9 |
Recently classified as high-income countries.3
Extrapolated estimate.
High-income countries
Based on national and regional surveys in high-income countries, CR density ranges from one program per 100 thousand to 300 thousand inhabitants,42,51,86 except in the case of Chile which has recently been classified as high-income.3 In the United States specifically, which has the highest CR density worldwide, there was one CR program per 102 thousand inhabitants in 2003, with a range of one program per 23 to 261 thousand inhabitants by state.86
CR density in LMICs
In middle-income countries, CR density is smaller than that of high-income countries.42 It ranged from 0.9–6.4 (Table 3). CR density in the United States was almost 23-fold greater than that reported in South America, where CR density was estimated at one program per 2.3 million inhabitants.42 Further, while CR density was 1 program per less than half a million inhabitants in high-income countries,42,51,86 CR density was almost 1 program per 1 to 6 million inhabitants in middle-income countries.
CR density in low-income countries has not been reported. Our extensive search identified only one program per country in the 3 low-income countries where CR was found to exist, namely Afghanistan,81,87 Bangladesh,82,87 and Kenya.83,87
Availability of CR to Patients
Physician Referral
Patient referral to a CR program by a physician is a prerequisite step for participation in most countries. In high-income countries, physician referral to CR has been highlighted as a key barrier in several studies.88,40,42,89–92 Findings of these studies reported 33%–71% of eligible patients were not referred, and hence were unable to access to CR (Table 4), despite the scientific statements and evidence-based guidelines on referral to CR. 93 Recently, data from the EUROASPIRE III Survey, conducted in 22 European countries (19 of which were high-income countries), showed that 44.8% of the 8,845 patients eligible for CR were advised by physicians or other healthcare professionals to attend a CR program.55 Whether this advice was a formal referral to CR or a verbal recommendation was not stated in the study; hence, this referral rate could be over-reported.
Table 4.
Proportion of patients referred to CR by country
| Country | No. Patients | % Referred | Diagnosis |
|---|---|---|---|
| High-income | |||
| Australia96 | 15, 186 | 29% | Cardiac event |
| Australia, Canada, USA 97 | 30,333 | 34% | Coronary artery disease |
| Canada91 | 3,739 | 52% | CABG, PCI |
| UK98 (England, Wales, Northern Ireland) | 146,000 | 45–67% | MI, unstable angina or following revascularization |
| USA89 | 72,817 | 56% | MI, PCI, CABG |
| USA90 | 145,661 | 60% | PCI |
| LMICs | |||
| Hungary55 | 452 | 57%* | CABG, PCI, MI, acute myocardial ischemia without infarction |
| Iran95 | NA | 15%** | NS |
| Romania55 | 516 | 26.4%* | CABG, PCI, MI, acute myocardial ischemia without infarction |
| Turkey55 | 329 | 7.3%* | CABG, PCI, MI, acute myocardial ischemia without infarction |
Patients were advised by physicians or health professionals to attend CR.
Based on 122 physicians’ perception. Abbreviations: CABG, coronary artery bypass graft surgery; MI, myocardial infarction; percutaneous coronary intervention; NS, not specified; NA, not applicable; UK, United Kingdom; USA, United States of America.
In LMICs, very few studies have investigated physician referral to CR, and where reported CR referral rates are even lower than those reported in high-income countries. In a study undertaken in Brazil94 for example, low CR referral was reported as a barrier to enrolment. Similarly, in a survey in Iran, low physician CR referral was also reported as a barrier to participation; Iranian cardiologists perceived < 15% of patients are referred.95 In European middle-income countries, the EUROASPIRE III survey demonstrated low CR “advice” rates, from 7.3% in Turkey to 26.4% in Romania.55 (Table 4)
Disparities in patient access to CR
Inappropriate variability in CR use has been documented in high-income countries.19,90,91 Certain vulnerable groups are less likely to be referred, and hence participate in CR.19,90,91 This includes women, the elderly, ethnocultural minorities, patients of low socioeconomic status, and with comorbidities.90,91,99 Paradoxically, these patients often have greater need for CR due to greater disease management complexity or evidence of poorer outcomes. In middle-income countries, women are similarly less represented than men (<30%) in CR.73,75,100,101 Indeed in one CR study in Brazil, there were no women represented.102 Given there is no evidence that these vulnerable groups derive less clinical benefit from CR, these disparities suggest that some vulnerable groups have even less access to CR than does the average patient.
CR Availability in Comparison to other Evidence-based Interventions
While the WHO states “cardiac rehabilitation should be an integral component of the long-term, comprehensive care of cardiac patients”,103 governments allocate more resources to acute treatment of CVD than to less expensive, long-term disease management, such as CR68,52 (Table 5). In a national CR survey, only 6.5% of 1,059 hospitals in Japan were “approved” to offering CR services.52 This is compared to 61.8% and 58.8% of these hospitals implementing coronary angiography and percutaneous coronary intervention, respectively, following myocardial infarction.52
Table 5.
Cost of treatment for cardiovascular diseases in 2 high-income countries
| Intervention | Cost |
|---|---|
| UK109 | |
| Cardiac rehabilitation | £427 |
| CABG for chronic angina (elective) | £4,956 |
| Angioplasty for chronic angina (elective) | £2,369 |
| USA | |
| Cardiac rehabilitation110 | $US1,728 |
| CABG16 | $US133, 247 |
| PCI16 | $US67, 086 |
| Cardiac catheterization16 | $US39,264 |
Abbreviations: CABG, coronary artery bypass graft surgery; MI, myocardial infarction; PCI, percutaneous coronary intervention; UK, United Kingdom; USA, United States of America.
While acute revascularization strategies such as coronary artery bypass graft surgery and percutaneous coronary interventions confer benefit for patients, CR is also considered as a Class I, Level A indication in clinical practice guidelines (i.e. useful and effective).104,32 For example, research demonstrates coronary artery bypass graft surgery conferred significant reductions in mortality of 39% (odds ratio [OR], 0.61; 95% CI, 0.48–0.77) at 5 years of follow-up,105 percutaneous coronary interventions conferred significant reductions of 20% (OR, 0.80; 0.64 to 0.99),106 and CR conferred significant reductions of 26% (OR, 0.74; 0.58–0.95).107 Moreover, a study from the United States showed that after revascularization, provision of CR would prevent or postpone the greatest number of deaths following myocardial infarction; while CR was the intervention which would prevent or postpone the greatest number of deaths in patients with unstable angina and heart failure.108
Middle-income countries are now starting to provide these expensive cardiac procedures. While this is appropriate given the epidemic of CVD in these contexts, resources are highly limited.68 While the cost of CR provision in LMICs is not known, consistent with high-income countries (Table 5), it is expected to cost much less than acute revascularization. Thus, CR should be developed prior to building of operating theatres and cardiac catheterization facilities, or at a minimum in concert with it. However, a survey of centres offering cardiac catheterization in 13 Latin American countries revealed only 56% had CR programs.68
CR utilization is also less than other guideline-recommended secondary prevention therapies, namely medications.111 For example, in a study on implementation of the American Heart Association’s Get with the Guidelines program,112 in multiple hospitals they were able to achieve rates of 94% aspirin use, 92.5% beta-blockade, and 84.8% angiotensin-converting enzyme inhibitor use. This is in stark contrast to the rates of CR use reported herein. With regard to outpatient care, data from the American College of Cardiology’s Practice Innovation and Clinical Excellence (PINNACLE) program similarly reveal greater, although more moderate, provision of evidence-based therapies than CR.113 In a sample of 8,132 coronary artery disease patients, CR referral was only 18.1%, eclipsed only by diabetes screening at 13.3%. Other practice recommendations such as blood pressure measurement (94.0%), smoking assessment (83.8%), and annual lipid assessment (74.3%) were much higher.113
A similar situation of greater provision of non-CR secondary prevention recommendations is observed in LMICs. For instance, the proportion of CHD patients receiving aspirin was 81.2%; beta-blockers was 48.1%; angiotensin-converting enzyme inhibitors was 39.8%; and for statins was 29.8% in 10 countries.114
Reasons for Under-utilization of CR
Much research has been done in high-income countries to identify reasons for under-utilization of CR despite its benefits. For example, in a systematic review, Murray et al.115 found 253 factors associated with uptake of cardiovascular lifestyle behavior change programs including CR. These barriers have been described at three inter-related levels: patient, provider, and system levels.
The most commonly-reported patient-related CR barriers included older age, low socioeconomic status, role obligations and subsequent time conflicts (i.e., work), patient disinterest, and comorbidities.19, 76, 88,90,91,97,115–117 Despite the scarcity of studies on CR barriers from middle-income countries, the barriers reported were consistent with those in high-income countries. 76,94,95,102 With regard to low-income countries, no studies on CR barriers were identified.
Physicians, in both high and middle-income settings, are demonstrated to play an important role in CR utilization.19,95,117,118 Inadequate physician knowledge about CR benefits, lack of incentives to refer and low physician endorsement of CR to their patients have been often described.95,117 Low physician referral may be compounded by their subjective assessment of a patient’s (in)ability to participate, and lack of implementation of systematic CR referral strategies at patient discharge.40,119, 118 Moreover, compensation for physicians to provide CR is considered much less than that for interventional cardiologists, which likely plays a role in physician choice of specialty and area of practice. This would lead to the system-level barrier of lack of health human resource capacity to deliver CR.
At the health-system level there are also many barriers to CR provision. Limited availability of CR programs, financial constraints, distance, transportation problems, and lack of insurance coverage are some of the most frequently-reported system-level barriers in high- and middle-income countries.19,95,102,115,117
CR barriers have only been investigated in the middle-income countries of Brazil, Iran, and Pakistan.76, 94,95, 102 Physicians perceived low patient referral in Iran due to limited general knowledge about CR program and its benefits, limited knowledge about methods of reimbursement, and lack of insurance coverage.95 In Brazil, distance, cost, lack of patient knowledge about CR benefits, and work and family responsibilities were barriers to CR participation.94,102 Similarly, employment conflicts and distance were the main barriers to CR participation in Pakistan.76 Barriers to CR provision in low-income settings have not been investigated, however barriers to healthcare provision more broadly have been well-described.
Strategies to Increase CR Provision
There are loud calls to increase CR provision in high-income countries,120 and clearly these calls need to be broadcast in LMICs. Implementation of evidence-based care is highly dependent upon the behaviors of policy-makers, healthcare professionals and patients.121,122 The Theoretical Domains Framework122 integrates theories of behavior change to address complex implementation problems such as with CR. It may be useful in developing complex interventions to overcome the gap in CR implementation, through its consideration of theory, as well as evidence and practical barriers, as reviewed herein.
Strategies to improve rehabilitation service delivery worldwide have been described by the WHO.123 They include reforming policies, expanding research, developing funding mechanisms to address barriers, increasing health human resources, expanding and decentralizing service delivery, and increasing the use and affordability of technology. Below, strategies to increase CR supply and demand, with particular relevance to LMICs, are forwarded.
Health policies to increase CR capacity
To address the inadequate availability of CR globally, coordinated effort at national and international levels are required.124 With regard to reforming CR policies specifically, surveys of program directors in high- and middle-income countries alike confirmed the need for national policies to support CR provision and comprehensive reimbursement.125,68 While sufficient evidence exists to support the provision of CR in high-income contexts, there have been few randomized controlled trials of CR undertaken in LMICs71,126,127 (however it is expected that greater gains would be observed given the low rates of risk factor screening and control).128 With expanded, context-specific research evidence, Ministries of Health could then implement public health policies that acknowledge, promote, and prioritize resources to support CR.68
With respect to low resources for CR delivery in LMICs, we have highlighted the discrepancy between the dissemination of expensive coronary interventions for treatment of CHD versus the poor implementation of CR (despite being less expensive, requiring less infrastructure and its’ efficacy).68 This underscores the need for re-allocation of resources and development of novel funding models to support cost-effective129 strategies such as CR. For instance, in the recent edition of the British Association for Cardiovascular Prevention and Rehabilitation Standards, they suggest that CR should be part of the “integrated cardiology service”.130 As cardiology services are being developed in LMICs, CR should be a required service provided post-event or procedure. This could reduce the need for repeat revascularization and other downstream medical care utilization.
While alternative models of CR delivery will be considered below, expanding health human resources and service delivery as recommended by WHO would likely also have substantive impact in increasing CR supply. CR rotations should be incorporated into training and education of healthcare providers, from community health workers to physicians. “Task-shifting” of provision of some of the core elements of CR, such as self-management education for instance, could be allocated to nurses rather than physicians, for example. Other approaches such as increasing the hours of operation of existing programs, and development of satellite sites of well-established programs could also greatly “scale up” CR capacity.
Health system approaches to increase CR demand
Arguably, if we increase patient demand for CR, then there will be pressure to increase provision (i.e., bottom-up approach). In a Cochrane review by Davies et al, 3 RCTs of interventions to increase patient uptake were identified. 131 These studies were conducted in high-income countries, and all were successful. One of these was low-cost,132 however the other 2 were complex and human resource-intensive.133,134 The former intervention comprised provision of a motivational letter to patients. A recent study135 also revealed that the use of theory-based invitation letters improved attendance at CR. Such a low-cost, simple method should be adapted and tested in middle-income contexts.
Systematic CR referral is a policy that has been demonstrated to increase CR use.136 Several associations have endorsed CR referral,40 including as an indicator of care quality, namely the American Association of Cardiovascular and Pulmonary Rehabilitation,137 the European Association for Cardiovascular Prevention and Rehabilitation,29 and the Canadian Association of Cardiac Rehabilitation (http://ddqi.ccs.ca/). Further, the latter association is close to achieving “pay for performance” for CR referral.138 This funding reform could represent a “disruptive innovation” in increasing CR participation rates.
Alternative models of CR delivery to increase reach
Due to the challenges confronting the delivery of traditional hospital-based CR including cost and accessibility, alternative models have been developed. Some of these models are seen in both high- and middle-income countries, such as home-127,139 and community-based programs.100,139,140 These programs are found to be as effective as hospital-based CR in reduction of CVD risk factors and mortality in recent systematic reviews.41,142 Moreover, home-based programs are shown to be as beneficial as supervised programs in middle-income countries, and may be lower cost.73 Unfortunately, due to lack of comprehensive reimbursement approaches for these models (with the United Kingdom being a notable exception) their implementation has not been wide.
Another alternative model for CR implementation is provision within the primary healthcare setting,143,144 which is much more broadly available globally than specialty care. Integration of chronic care into primary healthcare in low-resource settings has been successful, such as for diabetes and hypertension.145 Though such findings are promising, primary care providers are often over-stretched with limited capacity to engage in preventive care. Use of “physician extenders” trained in the core elements of CR may support CR provision in this context.
Finally, internet-based, telehealth, and mobile device delivery modalities represent a burgeoning and active area of CR research. These program models have advantages in terms of cost, time (i.e., no conflict with work schedules, no transportation required, less interference with family obligations), privacy (i.e., no group embarrassment), and in overcoming logistical barriers such as infrastructure and health human resource constraints. Based on our literature review, internet- or web-based models141,146 have only been tested in high-income countries to date. Because of the variations in the internet-based interventions, it was not possible to compare effectiveness of internet-based with hospital-based CR program146; still, the internet-based interventions had positive effects on health behavior compliance, physical activity, as well as psychosocial and clinical outcomes (i.e., blood pressure, cholesterol, hospital visits.146 Mobile CR models are emerging in high-income countries with promising results.141,147 While there are yet no data from LMICs, one study is under way in Jordan.147,148 Given the penetrance of mobile technology in many LMICs, these models have significant potential to increase delivery of CR.
Conclusions
While the global trends of CVD burden and death are increasing, the global availability of CR is very low. Only 38.8% of countries have CR programs, with densities in middle-income contexts as low as one program per 6 million inhabitants. The problem is worse in LMICs where only 23% of countries have CR, yet they have the greatest burden of CVD. While the multi-factorial reasons for this paradox are known, so are strategies to increase provision. Moreover, novel delivery modalities hold incredible promise of reach, given the penetrance of mobile phones in LMICs in particular. We have effectively increased CR use in the United States and much of Western Europe, countries which have a plethora health care system delivery models. It is time to focus our efforts on tailoring these approaches to LMICs. The burden of evidence for CR is equivalent to other therapies, and thus as cardiology services are developed in LMICs, CR should be at the forefront of care.
Key points.
CR services are poorly implemented worldwide, with 38.8% of countries having CR services globally
CR services are available in only 23% of LMICs, countries which have the greatest cardiovascular disease burden and highest rates of mortality.
The density of CR is greatest in the United States where there is one program per 102,000 inhabitants; this contrasts starkly with middle-income countries with a density of one program per 1–6 million inhabitants
Less than 50% of eligible patients are referred to CR programs
CR services are less often implemented than are other evidence-based secondary prevention therapies, though its’ cost is much less
More research is required to evaluate effectiveness of affordable and feasible CR models in both high and LMICs, while taking advantage of new technologies
Acknowledgments
The authors gratefully acknowledge the assistance of the University Health Network information specialist Ms. Maureen Pakosh in conducting the electronic database searches. Dr. Sarrafzadegan also acknowledges the University of British Columbia School of Population and Public Health where she was undertaking sabbatical while writing this manuscript.
Footnotes
Conflicts to disclose: none
Contributor Information
Karam Turk-Adawi, Cardiovascular Rehabilitation & Prevention, University Health Network, 399 Bathurst Street, Toronto, Ontario, M5T 2S8, Canada.
Nizal Sarrafzadegan, Isfahan Cardiovascular Research Center, Cardiovascular Research Institute, Isfahan University of Medical Sciences, Seddigheh Tahereh Research and Treatment Hospital, Khorram Ave, PO Box: 81465-1148 Isfahan, Iran.
Sherry L. Grace, School of Kinesiology and Health Science, York University, 4700 Keele Street, Toronto, Ontario, M3J 1P3, Canada, and Cardiovascular Rehabilitation & Prevention, University Health Network, 399 Bathurst Street, Toronto, Ontario, M5T 2S8, Canada
References
- 1.Mendis S, Alwan A, editors. Prioritized research agenda for prevention and control of noncommunicable diseases. World Health Organization; Geneva: 2011. [Google Scholar]
- 2.Gaziano TA, Pagidipati N. Scaling up chronic disease prevention interventions in lower-and middle-income countries. Annu Rev Public Health. 2013;34:317–335. doi: 10.1146/annurev-publhealth-031912-114402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Bank. How we classify countries? 2013 http://data.worldbank.org/about/country-classifications.
- 4.Bloom DE, et al. The Global Economic Burden of Non-communicable Diseases. World Economic Forum; Geneva: 2011. [Google Scholar]
- 5.Balady G, et al. Cardiac rehabilitation programs. A statement for healthcare professionals from the American Heart Association. Circulation. 1994;90:1602–1610. doi: 10.1161/01.cir.90.3.1602. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. The Global Burden of Disease: 2004 Update. World Health Organization; Geneva: 2008. [Google Scholar]
- 7.World Health Organization. Mental Health: DALYs/YLD definition. 2013 http://www.who.int/mental_health/management/depression/daly/en/
- 8.Mackay J, Mensah GA, Mendis S, Greenlund K. The atlas of heart disease and stroke. World Health Organization; Geneva: 2004. [Google Scholar]
- 9.Murray CJL, Lopez AD. Global Health Statistics. Harvard School of Public Health; Boston: 1996. [Google Scholar]
- 10.Vos T, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2012;380:2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heart Foundation. Data and statistics. 2013 http://www.heartfoundation.org.au/information-for-professionals/data-and-statistics/Pages/default.aspx.
- 12.Neto GB, Silva ENd. The costs of cardiovascular disease in Brazil: A brief economic comment. Arquivos Brasileiros de Cardiologia. 2008;91:217–218. doi: 10.1590/s0066-782x2008001600002. [DOI] [PubMed] [Google Scholar]
- 13.Heart and Stroke Foundation. Statistics. 2013 http://www.heartandstroke.com/site/c.ikIQLcMWJtE/b.3483991/k.34A8/Statistics.htm#heartdisease.
- 14.Hu SS, et al. Outline of the Report on Cardiovascular Disease in China, 2010. Biomedical and Environmental Sciences. 2012;25:251–256. doi: 10.3967/0895-3988.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 15.Health India. Getting straight to the heart of the attack. 2013 http://health.india.com/diseases-conditions/getting-straight-to-the-heart-of-the-attack/
- 16.Go AS, et al. Heart disease and stroke statistics—2013 update: A report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Heart Federation. Global health agenda. Targets and indicators. 2013 http://www.world-heart-federation.org/what-we-do/advocacy/global-health-agenda/un-summit-on-ncds/targets-and-indicators/
- 18.World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013–2020. World Health Organization; Geneva: 2013. [Google Scholar]
- 19.Balady GJ, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: A presidential advisory from the American Heart Association. Circulation. 2011;124:2951–2960. doi: 10.1161/CIR.0b013e31823b21e2. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization. Needs and action priorities in cardiac rehabilitation and secondary prevention in patients with CHD. World Health Organization; Geneva: 1993. [Google Scholar]
- 21.Balady GJ, et al. Core Components of Cardiac Rehabilitation/Secondary Prevention Programs: 2007 Update: A Scientific Statement From the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2007;115:2675–2682. doi: 10.1161/CIRCULATIONAHA.106.180945. [DOI] [PubMed] [Google Scholar]
- 22.Piepoli MF, et al. Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery. European Journal of Preventive Cardiology. 2012;0:1–18. doi: 10.1177/2047487312449597. [DOI] [PubMed] [Google Scholar]
- 23.Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: Secondary prevention programs for patients with coronary artery disease. Annals of Internal Medicine. 2005;143:659–672. doi: 10.7326/0003-4819-143-9-200511010-00010. [DOI] [PubMed] [Google Scholar]
- 24.Jolliffe JA, et al. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2001:CD001800. doi: 10.1002/14651858.CD001800. [DOI] [PubMed] [Google Scholar]
- 25.Taylor R, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116:682–692. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 26.McAlister FA, Lawson FM, Teo KK, Armstrong PW. Randomised trials of secondary prevention programmes in coronary heart disease: Systematic review. British Medical Journal. 2001;323:957–962. doi: 10.1136/bmj.323.7319.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oldridge NB, Guyatt GH, Fischer ME, Rimm AA. Cardiac rehabilitation after myocardial infarction. Combined experience of randomized clinical trials. Journal of the American Medical Association. 1988;260:945–950. [PubMed] [Google Scholar]
- 28.O’Connor GT, et al. An overview of randomized trials of rehabilitation with exercise after myocardial infarction. Circulation. 1989;80:234–244. doi: 10.1161/01.cir.80.2.234. [DOI] [PubMed] [Google Scholar]
- 29.Piepoli MF, et al. Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery. European Journal of Preventive Cardiology. 2012;0:1–18. doi: 10.1177/2047487312449597. [DOI] [PubMed] [Google Scholar]
- 30.Hillis LD, et al. ACCF/AHA Guideline for coronary artery bypass graft surgery: executive summary: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124:2610–2642. doi: 10.1161/CIR.0b013e31823b5fee. [DOI] [PubMed] [Google Scholar]
- 31.Levine G, et al. ACCF/AHA/SCAI Guideline for percutaneous coronary intervention: executive summary: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011;124:2574–2609. doi: 10.1161/CIR.0b013e31823a5596. [DOI] [PubMed] [Google Scholar]
- 32.Smith S, et al. AHA/ACCF Secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: A guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124:2458–2473. doi: 10.1161/CIR.0b013e318235eb4d. [DOI] [PubMed] [Google Scholar]
- 33.Vanhees L, McGee HM, Dugmore LD, Schepers D, van Daele P. A representative study of cardiac rehabilitation activities in European Union Member States: The CARINEX SURVEY. Journal of Cardiopulmonary Rehabilitation and Prevention. 2002;22:264–272. doi: 10.1097/00008483-200207000-00009. [DOI] [PubMed] [Google Scholar]
- 34.Bjarnason-Wehrens B, et al. Cardiac rehabilitation in Europe: Results from the European Cardiac Rehabilitation Inventory Survey. European Journal of Cardiovascular Prevention and Rehabilitation. 2010;17:410–418. doi: 10.1097/HJR.0b013e328334f42d. [DOI] [PubMed] [Google Scholar]
- 35.Fletcher SM, Burley MB, Thomas KE, Mitchell EKL. Feeling supported and abandoned: mixed messages from attendance at a rural community cardiac rehabilitation program in australia. Journal of Cardiopulmonary Rehabilitation and Prevention. 2013 doi: 10.1097/HCR.1090b1013e3182a52734. Publish Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 36.Nooruddin T, Matooq A, Mansoor F, Alaswamy Z, Khalil SH. Effectiveness of cardiac rehabilitation program in reducing cardiovascular risk factor and improving functional capacity among cardiac patients in Kingdom of Bahrain. 23 Australian Annual Cardiovascular Health and Rehabilitation Conference; Mellborn, Australia. 2013. [Google Scholar]
- 37.Heart and Stroke Foundation of Barbados. Cardiac Disease Prevention & Rehabilitation Programme - CDP&R. 2013 http://www.hsfbarbados.org/%28S%28fknmqa454jp2nranjahcb4fk%29%29/GymCDPR.aspx.
- 38.Bermuda Hospitals Board. Cardiac rehabilitation services. 2013 http://www.bermudahospitals.bm/cardiac-care/cardiac_rehabilitation_services.asp.
- 39.The Brunei Times. Ripas designs exercise regimen for patients in cardiac rehabilitation. 2013 http://www.bt.com.bn/classification/news/home_news/2007/05/16/ripas_designs_exercise_regimen_for_patients_in_cardiac_rehabilitation.
- 40.Grace SL, et al. Systematizing inpatient referral to cardiac rehabilitation 2010: Canadian Association of Cardiac Rehabilitation and Canadian Cardiovascular Society joint position paper. Journal of Cardiopulmonary Rehabilitation and Prevention. 2011;31:E1–E8. doi: 10.1097/HCR.0b013e318219721f. [DOI] [PubMed] [Google Scholar]
- 41.State of Jersey-Channel Islands. Specialist help for cardiac patients. http://www.gov.je/News/2011/Pages/HelpForCardiacPatients.aspx.
- 42.Cortes-Bergoderi M, et al. Availability and characteristics of cardiovascular rehabilitation programs in South America. Journal of Cardiopulmonary Rehabilitation and Prevention. 2013;33:33–41. doi: 10.1097/HCR.0b013e318272153e. [DOI] [PubMed] [Google Scholar]
- 43.Stewart R, et al. Physical activity in patients with stable coronary heart disease: An international perspective. European Heart Journal. 2013;34:3286–3293. doi: 10.1093/eurheartj/eht258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zwisler ADO, Traeden U, Videbaek J, Madsend M. Cardiac rehabilitation services in Denmark: Still room for expansion. Scandinavian Journal of Public Health. 2005;33:376–383. doi: 10.1080/14034940510005824. [DOI] [PubMed] [Google Scholar]
- 45.Cottin Y, et al. Specific profile and referral bias of rehabilitated patients after an acute coronary syndrome. Journal of Cardiopulmonary Rehabilitation. 2004;24:38–44. doi: 10.1097/00008483-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 46.Karoff M, Held K, Bjarnason-Wehrens B. Cardiac rehabilitation in Germany. European Journal of Cardiovascular Prevention & Rehabilitation. 2007;14:18–27. doi: 10.1097/HJR.0b013e3280128bde. [DOI] [PubMed] [Google Scholar]
- 47.Antonakoudis H, et al. Cardiac rehabilitation effects on quality of life in patients after acute myocardial infarction. Hippokratia. 2006;10:176–181. [PMC free article] [PubMed] [Google Scholar]
- 48.Chan DSK, Chau JPC, Chang AM. Acute coronary syndromes: Cardiac rehabilitation programmes and quality of life. Journal of Advanced Nursing. 2005;49:591–599. doi: 10.1111/j.1365-2648.2004.03334.x. [DOI] [PubMed] [Google Scholar]
- 49.Isle of Man Government. Cardiac services. 2013 https://www.gov.im/categories/health-and-wellbeing/hospitals-and-emergency-treatment/noble%27s-hospital/cardiac-services/
- 50.Gendler Y, et al. A multicenter intervention study on referral to cardiac rehabilitation after coronary artery bypass graft surgery: A 1-year follow-up of rehabilitation rates among USSR-born and veteran Israeli patients. Harefuah. 2012;151:511–517. [PubMed] [Google Scholar]
- 51.Tramarin R, et al. The Italian Survey on Cardiac Rehabilitation-2008 (ISYDE-2008). Part 3. National availability and organization of cardiac rehabilitation facilities. Official report of the Italian Association for Cardiovascular Prevention, Rehabilitation and Epidemiology (IACPR-GICR) Monaldi Arch Chest Dis. 2008;70:175–205. doi: 10.4081/monaldi.2008.413. [DOI] [PubMed] [Google Scholar]
- 52.Goto Y, et al. Poor implementation of cardiac rehabilitation despite broad dissemination of coronary interventions for acute myocardial infarction in Japan. A nationwide survey. Circulation Journal. 2007;71:173–179. doi: 10.1253/circj.71.173. [DOI] [PubMed] [Google Scholar]
- 53.Kim YJ, et al. Beneficial effects of cardiac rehabilitation and exercise after percutaneous coronary intervention on hsCRP and inflammatory cytokines in CAD patients. Pflugers Arch. 2008:1081–1088. doi: 10.1007/s00424-007-0356-6. [DOI] [PubMed] [Google Scholar]
- 54.Four Square. Cardiac Rehabilitation Center - CDH Medical Center Alsabah, Kuwait. 2013 https://foursquare.com/v/cardiac-rehabilitation-center--cdh/51b40915498e614915ba6b01.
- 55.Kotseva K, Wood D, Backer GD, Bacquer DD. Use and effects of cardiac rehabilitation in patients with coronary heart disease: Results from the EUROASPIRE III survey. European Journal of Preventive Cardiology. 2013;20:817–826. doi: 10.1177/2047487312449591. [DOI] [PubMed] [Google Scholar]
- 56.Briffa T, et al. Exposure to evidence-based secondary prevention after acute coronary syndrome (ACS) in Australia and New Zealand. Circulation. 2013;128:A11996. [Google Scholar]
- 57.Otterstad JE. Influence on lifestyle measures and five-year coronary risk by a comprehensive lifestyle intervention programme in patients with coronary heart disease. European Journal of Cardiovascular Prevention & Rehabilitation. 2003;10:429–437. doi: 10.1097/01.hjr.0000107024.38316.6a. [DOI] [PubMed] [Google Scholar]
- 58.Padró C, Correa-Pérez M. A clinical study of a cardiac rehabilitation program (phase II) PR Health Sci J. 1997;16:245–50. [PubMed] [Google Scholar]
- 59.Cardiac rehab in Qatar. 2013 https://twitter.com/QatarCRehab.
- 60.Blair J, Corrigall H, Angus N, Thompson D, Leslie S. Home versus hospital-based cardiac rehabilitation: A systematic review. Rural and Remote Health. 2011;11:1532. [PubMed] [Google Scholar]
- 61.G- movement. Life-enhancing movement for health. 2013 http://www.g-movement.org/programmes.html.
- 62.Stauber S, et al. Psychosocial outcome in cardiovascular rehabilitation of peripheral artery disease and coronary artery disease patients. Vascular Medicine. 2013;18:257–262. doi: 10.1177/1358863X13505861. [DOI] [PubMed] [Google Scholar]
- 63.Total rehab Centre. Holistic Health. 2013 http://www.ttwellnessconnect.com/total-rehab-centre-holistic-health/
- 64.Sheikh Khalifa Medical City. Cardiac sciences. 2013 http://www.skmc.ae/en-us/medicalservices/SpecialistCare/CardiacSciences/Pages/default.aspx.
- 65.Bethell H, et al. Outpatient cardiac rehabilitation attendance in England: Variability by region and clinical characteristics. Journal of Cardiopulmonary Rehabilitation and Prevention. 2008;28:386–391. doi: 10.1097/HCR.0b013e31818c3b44. [DOI] [PubMed] [Google Scholar]
- 66.Suaya J, et al. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116:1653–1662. doi: 10.1161/CIRCULATIONAHA.107.701466. [DOI] [PubMed] [Google Scholar]
- 67.Virgin Islands Cardiac Center at Juan F. Luis Hospital. 2013 http://www.jflusvi.org/cardiac_center.php.
- 68.Korenfeld Y, et al. Current status of cardiac rehabilitation in Latin America and the Caribbean. American Heart Journal. 2009;158:480–487. doi: 10.1016/j.ahj.2009.06.020. [DOI] [PubMed] [Google Scholar]
- 69.Shanmugasegaram S, Perez-Terzic C, Jiang X, Grace SL. Cardiac rehabilitation services in low- and middle-income countries: A scoping review. Journal of Cardiovascular Nursing. 2013 doi: 10.1097/JCN.1090b1013e31829c31414. Publish Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 70.Adghar D, Bougherbal R, Hanifi R, Khellaf N. Cardiac rehabilitation: First experience in Algeria. Ann Cardiol Angeiol (Paris) 2008;57:44–47. doi: 10.1016/j.ancard.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 71.Jiang X, Sit JW, Wong TK. A nurse-led cardiac rehabilitation programme improves health behaviours and cardiac physiological risk parameters: evidence from Chengdu, China. Journal of Clinical Nursing. 2007;16:1886–1897. doi: 10.1111/j.1365-2702.2007.01838.x. [DOI] [PubMed] [Google Scholar]
- 72.Tantaewy NM, Shebl AM, Shereif WI, Weheda SM. Effect of cardiac rehabilitation program on lifestyle pattern of patients with myocardial infraction. Journal of Biology, Agriculture and Healthcare. 2013;3 [Google Scholar]
- 73.Chakraborty K, et al. A comparative study on the effects of comprehensive rehabilitation in uncomplicated coronary artery bypass grafting patients from rural and urban India. Indian Journal of Physical Medicine and Rehabilitation. 2007;18:34–40. [Google Scholar]
- 74.Karapolat B. S36–3 Cardiac rehabilitation in Indonesia. CVD Prevention and Control. 2009;4:S49. [Google Scholar]
- 75.Sarrafzadegan N, et al. Gender differences in risk factors and outcomes after cardiac rehabilitation. Acta Cardiol. 2008;63:763–770. doi: 10.2143/AC.63.6.2033395. [DOI] [PubMed] [Google Scholar]
- 76.Ali M, et al. Factors affecting outpatient cardiac rehabilitation attendance after acute myocardial infarction and coronary revascularization_ a local experience. Journal of Pakistan Medical Association. 2012;62:347. [PubMed] [Google Scholar]
- 77.Avram A, et al. EUROASPIRE III Romania - the need to reinforce cardiac rehabilitation in patients with coronary artery disease. TMJ. 2010;60:299–304. [Google Scholar]
- 78.Digenio AG, et al. The Johannesburg Cardiac Rehabilitation Programme: A 5 year evaluation. Journal of Cardiopulmonary Rehabilitation and Prevention. 1997;17:340. [Google Scholar]
- 79.Nahali RM, et al. Place of cardiac rehabilitation in coronary patients. 26th Congress of SOFMER: Physical and Rehabilitation Medicine; Nantes, France. October 13–15, 2011. [Google Scholar]
- 80.Ciftçi C, Duman B, Cağatay P, Demiroğlu C, Aytekin V. The effects of phase II cardiac rehabilitation programme on patients undergone coronary bypass surgery. Anadolu Kardiyol Derg. 2005;5:116–121. [PubMed] [Google Scholar]
- 81.Kabul Medical University Cardiac Research Centre. Rehabilitation services. 2013 http://www.kcrc-af.ca/rehabilitation-services/
- 82.Zahan R. The Institute of Sport Science and Spor. Friedrich-Alexander University Erlangen-Nuremberg; Erlangen: 2013. Exercise-based cardiac rehabilitation program: Status in Bangladesh. [Google Scholar]
- 83.Coastweek Com Kenya. Aga Khan University Hospital Opens Cardiac Rehabilitation Unit. 2013 http://sjpaderborn.wordpress.com/2011/08/19/aga-khan-university-hospital-opens-cardiac-rehabilitation-unit-coastweek-com-kenya/
- 84.Laslett LJ, et al. The worldwide environment of cardiovascular disease: Prevalence, diagnosis, therapy, and policy issues. A report from the American College of Cardiology. Journal of the American College of Cardiology. 2012;60:S1–S49. doi: 10.1016/j.jacc.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 85.Pack QR, et al. What is the potential capacity for increasing cardiac rehabilitation utilization in the United States? (Abstract) Circ Cardiovasc Qual Outcomes. 2013;6:A180. 92. [Google Scholar]
- 86.Curnier DY, Savage PD, Ades PA. Geographic distribution of cardiac rehabilitation programs in the United States. J Cardiopulm Rehabil. 2005;25:80–84. doi: 10.1097/00008483-200503000-00006. [DOI] [PubMed] [Google Scholar]
- 87.World Atlas. Countries of the World. 2013 http://www.worldatlas.com/aatlas/populations/ctypopls.htm#.Uqyqv-IuehI.
- 88.Clark AM, et al. Factors influencing referral to cardiac rehabilitation and secondary prevention programs: A systematic review. European Journal of Preventive Cardiology. 2013;20:692–700. doi: 10.1177/2047487312447846. [DOI] [PubMed] [Google Scholar]
- 89.Brown TM, et al. Predictors of cardiac rehabilitation referral in coronary artery disease patients: Findings from the American Heart Association’s Get With The Guidelines program. Journal of the American College of Cardiology. 2009;54:515–521. doi: 10.1016/j.jacc.2009.02.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Aragam KG, et al. Trends and disparities in referral to cardiac rehabilitation after percutaneous coronary intervention. American Heart Journal. 2011;161:544–551. doi: 10.1016/j.ahj.2010.11.016. [DOI] [PubMed] [Google Scholar]
- 91.Brady S, Purdham D, Oh P, Grace S. Clinical and sociodemographic correlates of referral for cardiac rehabilitation following cardiac revascularization in Ontario. Heart & lung : The Journal of Critical Care. 2013;42:320–325. doi: 10.1016/j.hrtlng.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 92.Beckstead JW, et al. Physicians’ tacit and stated policies for determining patient benefit and referral to cardiac rehabilitation. Medical Decision Making. 2013 doi: 10.1177/0272989X13492017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Thomas RJ. Cardiac rehabilitation/secondary prevention programs: A raft for the rapids: Why have we missed the boat? Circulation. 2007;116:1644–1646. doi: 10.1161/CIRCULATIONAHA.107.728402. [DOI] [PubMed] [Google Scholar]
- 94.Mair V, Breda AP, Nunes MEB, Matos LDNJd. Evaluating compliance to a cardiac rehabilitation program in a private general hospital. Einstein (São Paulo) 2013;11:278–284. doi: 10.1590/S1679-45082013000300004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Moradi B, Maleki M, Maryam Esmaeilzadeh, Abkenar HB. Physician-related factors affecting cardiac rehabilitation referral. J Teh Univ Heart Ctr. 2011;6:187–192. [PMC free article] [PubMed] [Google Scholar]
- 96.Scott IA, Lindsay A, Harden HE. Utilisation of outpatient cardiac rehabilitation in Queensland. The Medical Journal of Australia. 2003;179:341–345. doi: 10.5694/j.1326-5377.2003.tb05588.x. [DOI] [PubMed] [Google Scholar]
- 97.Cortés O, Arthur HM. Determinants of referral to cardiac rehabilitation programs in patients with coronary artery disease: A systematic review. American Heart Journal. 2006;151:249–256. doi: 10.1016/j.ahj.2005.03.034. [DOI] [PubMed] [Google Scholar]
- 98.Beswick AD, et al. Provision, uptake and cost of cardiac rehabilitation programmes: Improving services to under-represented groups. Health Technology Assessment. 2004;8:iii–iv. ix–x, 1–152. doi: 10.3310/hta8410. [DOI] [PubMed] [Google Scholar]
- 99.Leung YW, Brual J, Macpherson A, Grace LS. Geographic issues in cardiac rehabilitation utilization: A narrative review. Health & Place. 2010;16:1196–1205. doi: 10.1016/j.healthplace.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rajendran A, Manoj S, Karthikeyan D, Davis S. Cardiac rehabilitation for CABG patients in south Indian setup : A prospective study. IJPMR. 2004;15:23–33. [Google Scholar]
- 101.Moradi B, Esmaeilzadeh M, Maleki M, Sari L. factors associated with failure to complete phase ii cardiac rehabilitation: survey registry in Rajaie Cardiovascular Medical and Research Center. Int Cardiovasc Res J. 2011;5:139–142. [Google Scholar]
- 102.Ghisi GLdM, et al. Perceptions of barriers to cardiac rehabilitation use in Brazil. Vasc Health Risk Manag. 2013;9:485–491. doi: 10.2147/VHRM.S48213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Goble AJ, Worcester M. Best practice guidelines for cardiac rehabilitation and secondary prevention. Department of Human Services Victoria; Carlton, Australia: 1999. [Google Scholar]
- 104.Oldridge N. Exercise-based cardiac rehabilitation in patients with coronary heart disease: Meta-analysis outcomes revisited. Future cardiology. 2012;8:729–751. doi: 10.2217/fca.12.34. [DOI] [PubMed] [Google Scholar]
- 105.Yusuf S, et al. Effect of coronary artery bypass graft surgery on survival: Overview of 10-year results from randomised trials by the coronary artery Bypass Graft Surgery Trialists Collaboration. Lancet. 1994;344:563–70. doi: 10.1016/s0140-6736(94)91963-1. [DOI] [PubMed] [Google Scholar]
- 106.Wijeysundera HC, Ko DT. Does percutaneous coronary intervention reduce mortality in patients with stable chronic angina: Are we talking about apples and oranges? Circulation: Cardiovascular Quality and Outcomes. 2009;2:123–126. doi: 10.1161/CIRCOUTCOMES.108.834853. [DOI] [PubMed] [Google Scholar]
- 107.Lawler P, Filion K, Eisenberg M. Efficacy of exercise-based cardiac rehabilitation post-myocardial infarction: A systematic review and meta-analysis of randomized controlled trials. The American Heart Journal. 2011;162:571–584.e572. doi: 10.1016/j.ahj.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 108.Kottke TE, et al. The Comparative Effectiveness of Heart Disease Prevention and Treatment Strategies. American journal of preventive medicine. 2009;36:82–88.e5. doi: 10.1016/j.amepre.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 109.Fidan D, Unal B, Critchley J, Capewell S. Economic analysis of treatments reducing coronary heart disease mortality in England and Wales, 2000–2010. QJM. 2007;100:277–289. doi: 10.1093/qjmed/hcm020. [DOI] [PubMed] [Google Scholar]
- 110.Carlson JJ, Johnson JA, Franklin BA, VanderLaan RL. Program participation, exercise adherence, cardiovascular outcomes, and program cost of traditional versus modified cardiac rehabilitation. The American Journal of Cardiology. 2000;86:17–23. doi: 10.1016/s0002-9149(00)00822-5. [DOI] [PubMed] [Google Scholar]
- 111.Mendis S, et al. The availability and affordability of selected essential medicines for chronic diseases in six low- and middle-income countries. Bull World Health Organ. 2007;85:279–288. doi: 10.2471/BLT.06.033647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Eagle KA, Koelling TM, Montoye CK. Primer: Implementation of guideline-based programs for coronary care. Nature Reviews Cardiology. 2006;3:163–171. doi: 10.1038/ncpcardio0499. [DOI] [PubMed] [Google Scholar]
- 113.Chan PS, et al. Cardiac performance measure compliance in outpatients: The American College of Cardiology and National Cardiovascular Data Registry’s PINNACLE (Practice Innovation And Clinical Excellence) Program. Journal of the American College of Cardiology. 2010;56:8–14. doi: 10.1016/j.jacc.2010.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Mendis S, et al. WHO study on prevention of recurrences of myocardial infarction and stroke (WHO-PREMISE) Bulletin of the World Health Organization. 2005;83:820–829. [PMC free article] [PubMed] [Google Scholar]
- 115.Murray J, Craigs C, Hill K, Honey S, House A. A systematic review of patient reported factors associated with uptake and completion of cardiovascular lifestyle behaviour change. BMC Cardiovascular Disorders. 2012;12:120. doi: 10.1186/1471-2261-12-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sarrafzadegan N, et al. Drop-out predictors in cardiac rehabilitation programmes and the impact of sex differences among coronary heart disease patients in an Iranian sample: A cohort study. Clinical Rehabilitation. 2007;21:362–372. doi: 10.1177/0269215507072193. [DOI] [PubMed] [Google Scholar]
- 117.Neubeck L, et al. Participating in cardiac rehabilitation: A systematic review and meta-synthesis of qualitative data. European Journal of Preventive Cardiology. 2012;19:494–503. doi: 10.1177/1741826711409326. [DOI] [PubMed] [Google Scholar]
- 118.Ghisi GLM, Polyzotis P, Oh P, Pakosh M, Grace SL. Physician factors affecting cardiac rehabilitation referral and patient enrollment: A systematic Review. Clinical Cardiology. 2013;36:323–335. doi: 10.1002/clc.22126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Boyden T, Rubenfire M, Franklin B. Will Increasing Referral to Cardiac Rehabilitation Improve Participation? Preventive Cardiology. 2010;13:198–202. doi: 10.1111/j.1751-7141.2010.00086.x. [DOI] [PubMed] [Google Scholar]
- 120.Arena R, et al. Increasing Referral and Participation Rates to Outpatient Cardiac Rehabilitation: The Valuable Role of Healthcare Professionals in the Inpatient and Home Health Settings: A Science Advisory From the American Heart Association. Circulation. 2012;125:1321–1329. doi: 10.1161/CIR.0b013e318246b1e5. [DOI] [PubMed] [Google Scholar]
- 121.Michie S, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Quality and Safety in Health Care. 2005;14:26–33. doi: 10.1136/qshc.2004.011155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7:37. doi: 10.1186/1748-5908-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.World Health Organization. World Report: Disabilities. Chapter 4. Geneva: World Health Organization; 2011. [Google Scholar]
- 124.Smith SC, et al. Our Time: A Call to Save Preventable Death From Cardiovascular Disease (Heart Disease and Stroke) Circulation. 2012;126:2769–2775. doi: 10.1161/CIR.0b013e318267e99f. [DOI] [PubMed] [Google Scholar]
- 125.Zwisler ADO, Schou L. Cardiac rehabilitation: Basic principles. Chapter 2. H:S Bispebjerg Hospital and National Institute of Public Health; Copenhagen: 2003. [Google Scholar]
- 126.Charoenkul P, Khuangsirikul W, Jalayondeja W, Krittayaphong R. Improvement in quality of life with phase II cardiac rehabilitation home program after coronary artery bypass surgery at Siriraj Hospital. Thai Heart J. 2007;20:165–170. [Google Scholar]
- 127.Karapolat H, et al. Effects of cardiac rehabilitation program on exercise capacity and chronotropic variables in patients with orthotopic heart transplant. Clinical Research in Cardiology. 2008;97:449–456. doi: 10.1007/s00392-008-0648-7. [DOI] [PubMed] [Google Scholar]
- 128.Salim Y, et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): A prospective epidemiological survey. The Lancet. 2011;378:1231–1243. doi: 10.1016/S0140-6736(11)61215-4. [DOI] [PubMed] [Google Scholar]
- 129.Brown A, Taylor R, Noorani H, Stone J, Skidmore B. Technology report # 34. Canadian Coordinating Office for Health Technology Assessment; Ottawa: 2003. Exercise-based cardiac rehabilitation programs for coronary artery disease: A systematic clinical and economic review. [Google Scholar]
- 130.Buckley JP, et al. BACPR scientific statement: British standards and core components for cardiovascular disease prevention and rehabilitation. Heart. 2013;99:1069–1071. doi: 10.1136/heartjnl-2012-303460. [DOI] [PubMed] [Google Scholar]
- 131.Davies P, et al. Promoting patient uptake and adherence in cardiac rehabilitation. Cochrane Database of Systematic Reviews. 2010 doi: 10.1002/14651858.CD007131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Wyer S, Earl J. Predicting attendance at cardiac rehabilitation: A review and recommendations. Coronary Health Care. 2001;5:171–177. [Google Scholar]
- 133.Jolly K, et al. Randomised controlled trial of follow up care in general practice of patients with myocardial infarction and angina: final results of the Southampton heart integrated care project (SHIP). The SHIP Collaborative Group. Br Med J. 1999;318:706–711. doi: 10.1136/bmj.318.7185.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Hillebrand T, Frodermann H, Lehr D, Wirth A. Vermehrte Teilnahme an ambulaten Herzgruppen durch poststationare Nachsorge [Increased participation in coronary groups by means of an outpatient care program] Herz Kreislauf. 1995;27:346–9. [Google Scholar]
- 135.Mosleh SM, Bond CM, Lee AJ, Kiger A, Campbell NC. Effectiveness of theory-based invitations to improve attendance at cardiac rehabilitation: A randomized controlled trial. European journal of cardiovascular nursing. 2013 doi: 10.1177/1474515113491348. [DOI] [PubMed] [Google Scholar]
- 136.Gravely-Witte S, et al. Effects of cardiac rehabilitation referral strategies on referral and enrollment rates. Nature reviews cardiology. 2010;7:87–96. doi: 10.1038/nrcardio.2009.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Thomas R, et al. AACVPR/ACCF/AHA 2010 update: Performance measures on cardiac rehabilitation for referral to cardiac rehabilitation/secondary prevention services: A report of the American Association of Cardiovascular and Pulmonary Rehabilitation and the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Clinical Performance Measures for Cardiac Rehabilitation) Circulation. 2010;122:1342–1350. doi: 10.1161/CIR.0b013e3181f5185b. [DOI] [PubMed] [Google Scholar]; King M. Euro 2007Prevent. Madrid, Spain: 2007. [Google Scholar]
- 138.Mead H, Grantham S, Siegel B. Improving Cardiovascular Care Through Outpatient Cardiac Rehabilitation: An Analysis of Payment Models That Would Improve Quality and Promote Use. Journal of cardiovascular nursing. 2014;29:158–164. doi: 10.1097/JCN.0b013e31828568f7. [DOI] [PubMed] [Google Scholar]
- 139.Radi B. Cardiac Rehabilitation in Indonesia. CVD Prevention and Control. 2009;4:S49. [Google Scholar]
- 140.Mandic S, et al. Effects of community-based cardiac rehabilitation on body composition and physical function in individuals with stable coronary artery disease: 1.6-year follow up. BioMed Research International 2013. 2013:7. doi: 10.1155/2013/903604. article ID 903604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Clark RA, et al. Alternative models of cardiac rehabilitation: A systematic review. European Journal of Preventive Cardiology. 2013 doi: 10.1177/2047487313501093. [DOI] [PubMed] [Google Scholar]
- 142.Dalal HM, Zawada A, Jolly K, Moxham T, Taylor RS. Home based versus centre based cardiac rehabilitation: Cochrane systematic review and meta-analysis. BMJ. 2010;340 doi: 10.1136/bmj.b5631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Márquez-Calderóna S, et al. Incorporation of cardiac rehabilitation programs and their characteristics in the Spanish National Health Service. Revista Española de Cardiologia (English Version) 2003;56:775–782. doi: 10.1016/s0300-8932(03)76956-5. [DOI] [PubMed] [Google Scholar]
- 144.Cupples ME, Reader C, Tully MA. Cardiac rehabilitation uptake following myocardial infarction: Cross-sectional study in primary care. Br J Gen Pract. 2010;60:431–435. doi: 10.3399/bjgp10X502155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Esterson YB, Carey M, Piette JD, Thomas N, Hawkins M. A systematic review of innovative diabetes care models in low-and middle-income countries (LMICs) Journal of Health Care for the Poor and Underserved. 2014;25:72–93. doi: 10.1353/hpu.2014.0037. [DOI] [PubMed] [Google Scholar]
- 146.Munro J, Angus N, Leslie SJ. Patient focused Internet-based approaches to cardiovascular rehabilitation - a systematic review. Journal of Telemedicine and Telecare. 2013;19:347–353. doi: 10.1177/1357633X13501763. [DOI] [PubMed] [Google Scholar]
- 147.Beatty AL, Fukuoka Y, Whooley MA. Using mobile technology for cardiac rehabilitation: A review and framework for development and evaluation. Journal of the American Heart Association. 2013;2 doi: 10.1161/jaha.113.000568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Alsaleh E, Blake H, Windle R. Behavioural intervention to increase physical activity among patients with coronary heart disease: Protocol for a randomised controlled trial. International Journal of Nursing Studies. 2012;49:1489–1493. doi: 10.1016/j.ijnurstu.2012.07.004. [DOI] [PubMed] [Google Scholar]