Abstract
Background
High body mass index (BMI) is consistently linked to increased risk of colorectal cancer (CRC) for men, whereas the association is less clear for women. As risk estimates from observational studies may be biased and/or confounded, we conducted a Mendelian randomization study to estimate the causal association between BMI and CRC.
Methods
We used data from 10,226 CRC cases and 10,286 controls of European ancestry. The Mendelian randomization analysis used a weighted genetic risk score, derived from 77 genome-wide association study identified variants associated with higher BMI, as an instrumental variable (IV). We compared the IV odds ratio (IV-OR) with the OR obtained using a conventional covariate-adjusted analysis.
Results
Individuals carrying greater numbers of BMI-increasing alleles had higher CRC risk (per weighted allele OR, 1.31; 95% confidence interval [CI], 1.10–1.57). Our IV estimation results support the hypothesis that genetically influenced BMI is directly associated with risk for CRC (IV-OR per 5 kg/m2, 1.50; 95% CI, 1.13–2.01). In the sex-specific IV analyses higher BMI was associated with higher risk of CRC among women (IV-OR per 5 kg/m2, 1.82; 95% CI, 1.26–2.61). For men, genetically influenced BMI was not associated with CRC (IV-OR per 5 kg/m2, 1.18; 95% CI, 0.73–1.92).
Conclusions
High BMI was associated with increased CRC risk for women. Whether abdominal obesity, rather than overall obesity, is a more important risk factor for men requires further investigation.
Impact
Overall, conventional epidemiologic and Mendelian randomization studies suggest a strong association between obesity and the risk of CRC.
Keywords: Colorectal cancer, Obesity, Epidemiology, Sex, Risk factors
Introduction
Observational studies consistently show that high body mass index (BMI) is associated with an increased risk of colorectal cancer (CRC) for men, whereas the magnitude of the association is less clear for women (1). Although these findings came from well designed and conducted epidemiologic studies, associations from observational studies could arise from bias and residual confounding and, therefore, may not necessarily reflect a causal relationship. First, the correlation between BMI and multiple other lifestyle and clinical factors suggests that adequate control for all potential confounding may be difficult. Conversely, over-adjustment in multivariable models can attenuate risk estimates towards the null and may explain the smaller associations reported for women (e.g., adjusting for menopausal hormone therapy) (2). Second, conventional epidemiologic analyses are often based on self-reports of participants’ weights and heights at one point in time and thus may be subject to misclassification from inaccurate reporting and insufficient follow-up to capture changes in measurements over time (e.g., men over-report height more so than women, and heavier women tend to under-report weight more so than heavier men (3, 4)). Finally, early stages of cancer may result in weight loss, and so measures of body weight reported within a few years of CRC diagnosis may introduce bias, a particular problem in case-control studies. As the latent period between high BMI and CRC risk is unknown, a measure that reflects typical lifetime BMI may counteract some of these limitations. Determining whether or not the association is causal is important as BMI could be a key target for primary prevention of CRC.
The use of genetic variants under the Mendelian randomization framework is one approach to exploring the possible causal nature of the observed associations between BMI and risk of CRC (5). Mendelian randomization uses instrumental variables (e.g., genetic variants that proxy for directly measured environmental risk factors) to make causal inferences about the relationship between a risk factor and an outcome and this approach can overcome issues of confounding, recall bias and reverse causality inherent in observational studies (5–7). First, because alleles are randomly allocated from parents to offspring during gamete formation, the association between the instrumental variable and the outcome is not confounded by environmental exposures. Second, genetic variants are measured reliably and are not affected by disease status. Furthermore, as those with the risk alleles have been essentially allocated randomly to higher levels of exposure across the lifecourse, genetic variation may more accurately reflect lifetime exposure compared with a single measurement. A potential limitation of Mendelian randomization arises however for highly complex traits whereby genetics may explain only a small fraction of the phenotypic variability. Many early Mendelian randomization studies used a single variant as an instrumental variable and, in the case described above, were unable to test the full spectrum of genetically influenced phenotype. By using multiple genetic variants as instrumental variables, we can increase statistical power and improve the precision of the instrumental variable estimate (8).
We therefore conducted a Mendelian randomization study using a weighted genetic risk score, derived from 77 genetic variants associated with higher BMI, as an instrumental variable to reassess the observational estimates of the associations between BMI and CRC risk.
Materials and Methods
Our analyses included individual participant data and genetic material from 10,226 CRC cases and 10,286 population-based controls of European ancestry in the Genetics and Epidemiology of Colorectal Cancer Consortium (GECCO) and Colon-Cancer Family Registry (C-CFR). The 11 studies (6 cohort and 5 case-control) used in our analyses (Supplementary Table S1) have been described in detail previously (9) and include the Health Professionals Follow-up Study (HPFS) (10); Nurses’ Health Study (NHS) (11); Physician’s Health Study (PHS) (12); Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial (PLCO) (13); VITamins and Lifestyle Study (VITAL) (14); Women’s Health Initiative (WHI) (15); the Colon-Cancer Family Registry (C-CFR) (16); Ontario Familial Colon Cancer Registries (OFCCR) (17); Diet, Activity and Lifestyle Survey (DALS) (18, 19); Postmenopausal Hormone Study (PMH-CCFR) (20); and Darmkrebs: Chancen der Verhütung durch Screening (DACHS) (21). To avoid confounding by population stratification, we used principal components analysis (HapMap II populations as reference) to restrict our analyses to individuals of European ancestry (22). Cases were men and women with primary invasive colorectal adenocarcinoma (International Classification of Diseases, 9th revision (ICD-9) codes 153.0–153.4, 153.6–153.9, and 154.0–154.1) and histologic confirmation (by medical records, pathologic reports, or death certificates) of CRC was performed for all studies. All participants provided written, informed consent and each study was approved by the relevant Institutional Review Boards.
Data on demographic and lifestyle factors were collected using in-person interviews or self-completed questionnaires, and data were centrally harmonized as previously described (23). BMI was calculated as weight in kilograms divided by height in meters squared (kg/m2). Although the studies obtained participants’ weight (either self-report or measured) at different time points with respect to CRC diagnosis (Supplementary Table S1), we used weight that most accurately reflected usual adult weight prior to any disease-related weight loss. For the Mendelian randomization analysis, we used a weighted genetic risk score as an instrumental variable (IV) for BMI. A recent genome-wide association study (GWAS) conducted by the Genetic Investigation of Anthropometric Traits (GIANT) consortium involving over 300,000 individuals of European-descent identified 77 single nucleotide polymorphisms (SNPs) associated with BMI at genome-wide significance (e.g., P<5×10−8) (24). Genotype information on these 77 SNPs was used to construct the weighted genetic risk score. The GIANT GWAS for BMI found no evidence of non-additive effects among SNPs, thus we fit additive SNP effects. For each SNP, participants received a score of 0, 1 or 2 for carrying zero (wild-type homozygous), one (heterozygous) or two (homozygous for the risk allele) alleles associated with higher BMI. For imputed SNPs, participants received scores that ranged from 0 to 2. SNPs were externally-weighted in the score by the per-allele change in BMI (the increase in BMI per 1 additional risk allele) reported for that SNP in the GIANT GWAS for BMI (24). Details on genotyping and quality assurance/quality control have been previously published (9). Call rates were ≥98% and all selected SNPs were in Hardy-Weinberg Equilibrium among controls (P≥1×10−4).
Statistical analysis
Associations between potential confounders and CRC risk were assessed using chi-square tests and Student t-tests. Associations among potential confounders, the IV, and BMI were assessed in controls using linear regression, Student t-tests and analysis of variance.
All participants were analyzed using a single-model (pooled) approach with adjustment for study. For the IV analysis, we used the two-stage control function IV approach, with the genetic risk score as an IV for BMI, and assumed an additive model (25). First, we fit a linear regression model within controls to predict BMI from the IV, adjusted for study and the top three principal components of genetic ancestry. Next, we fit a logistic regression model with BMI as a predictor and CRC case-control status as the outcome using robust standard errors and adjusted for the residuals from the first step (25). The coefficient for BMI from the second-stage model is the causal estimate for BMI. In Mendelian randomization studies, the IV for the exposure of interest is considered sufficiently strong if the first-stage F-statistic exceeds 10 (26). For the conventional covariate-adjusted analysis, BMI was the variable of interest and odds ratios (OR) and 95% confidence intervals (95%CI) were estimated using unconditional logistic regression models. We conducted minimally adjusted analyses (models were adjusted for age, sex, and study) and fully adjusted analyses (models were additionally adjusted for smoking status, family history of cancer, history of diabetes, use of aspirin or non-steroidal anti-inflammatory drugs [NSAIDs], consumption of fruit, vegetables, processed meat, and red meat, and [women only] use of menopause hormone therapy). Variables were retained in the fully adjusted analyses if they were statistically significantly associated with CRC risk after mutual adjustment for other risk factors. Participants with missing data on covariates were included in the analyses using an additional category for missing values. We assessed whether the estimates obtained using conventional epidemiologic and IV methods were different using the Durbin form of the Durbin-Wu-Hausman statistic (27). Rejection of the null hypothesis (i.e., risk estimates for BMI from both analyses are equal) indicates that the OR from the conventional covariate-adjusted analysis differs from the OR from the IV approach. We examined potential statistical interaction between BMI and sex by including a multiplicative term in the model, and conducted additional analyses for the BMI-CRC association stratified by sex and cancer sub-site. Furthermore, we performed a sensitivity analysis excluding studies with self-reported weight. In a supplementary analysis, we examined the association between a weighted genetic risk score for waist-to-hip ratio (WHR), derived using 47 variants associated with WHR adjusted for BMI (28), and CRC risk. Statistical significance was determined at α=0.05 and all tests for statistical significance were two-sided. Analyses were performed using Stata 12.0 (StataCorp, College Station, TX).
Results
The mean age of study participants was 63 years and 56% were women (Supplementary Table S1). Compared with controls, cases were more likely to smoke cigarettes, have a family history of cancer, and have diabetes and less likely to use aspirin or NSAIDs and (women only) menopausal hormones (Table 1). Cases consumed more red and processed meats on average than controls, but less fruit and vegetables. On average, cases (women: mean BMI, 27.0; standard deviation [SD], 5.4; men: mean BMI, 27.3; SD, 4.0) had statistically significantly higher BMI than controls (women: mean BMI, 26.2; SD, 5.0; men: mean, 26.5; SD, 3.7) (Supplementary Table S1). BMI was statistically significantly associated with age, sex, history of diabetes, use of aspirin/NSAIDs, consumption of fruit, processed meat, and red meat and, for women only, use of menopause hormone therapy (Supplementary Table S2).
Table 1.
Characteristics of controls and cases with colorectal cancer (CRC), stratified by sex
| Women | Men | |||||
|---|---|---|---|---|---|---|
| Variable | Controls n=5747 |
CRC n=5644 |
P a | Controls n=4539 |
CRC n=4582 |
P a |
| Smoking status | <0.001 | <0.001 | ||||
| Never | 3029 (52.9) | 2819 (50.2) | 1706 (37.9) | 1525 (33.6) | ||
| Former | 2145 (37.4) | 2126 (37.9) | 2365 (52.6) | 2422 (53.3) | ||
| Current | 554 (9.7) | 669 (11.9) | 428 (9.5) | 594 (13.1) | ||
| Missing | 19 | 30 | 40 | 41 | ||
| Body mass index (kg/m2) | <0.001 | <0.001 | ||||
| <25 | 2699 (47.0) | 2347 (41.6) | 1637 (36.1) | 1324 (28.9) | ||
| 25–29.99 | 1935 (33.7) | 1964 (34.8) | 2223 (49.0) | 2344 (51.2) | ||
| ≥30 | 1113 (19.4) | 1333 (23.6) | 679 (15.0) | 914 (19.9) | ||
| Family history | <0.001 | <0.001 | ||||
| No | 4806 (86.0) | 4483 (82.0) | 3685 (89.9) | 3430 (82.1) | ||
| Yes | 782 (14.0) | 986 (18.0) | 414 (10.1) | 749 (17.9) | ||
| Missing | 159 | 175 | 440 | 403 | ||
| Diabetes | <0.001 | 0.01 | ||||
| No | 4742 (95.0) | 4362 (91.1) | 3262 (91.0) | 3289 (89.2) | ||
| Yes | 249 (5.0) | 428 (8.9) | 323 (9.0) | 400 (10.8) | ||
| Missing | 756 | 854 | 954 | 893 | ||
| Aspirin/NSAID use | <0.001 | <0.001 | ||||
| No | 3553 (62.0) | 3895 (69.3) | 2519 (55.7) | 2928 (64.3) | ||
| Yes | 2176 (38.0) | 1727 (30.7) | 2004 (44.3) | 1626 (35.7) | ||
| Missing | 18 | 22 | 16 | 28 | ||
| Fruit (servings/day) | <0.001 | 0.01 | ||||
| Q1 | 1052 (19.1) | 1072 (20.3) | 780 (18.0) | 824 (19.6) | ||
| Q2 | 2101 (38.2) | 2226 (42.1) | 1905 (43.9) | 1917 (45.7) | ||
| Q3 | 1397 (25.4) | 1204 (22.7) | 982 (22.6) | 888 (21.2) | ||
| Q4 | 952 (17.3) | 790 (14.9) | 673 (15.5) | 566 (13.5) | ||
| Missing | 245 | 352 | 199 | 387 | ||
| Vegetables (servings/day) | <0.001 | <0.001 | ||||
| Q1 | 1222 (22.2) | 1328 (24.9) | 805 (18.5) | 863 (20.5) | ||
| Q2 | 1825 (33.1) | 1824 (34.3) | 1791 (41.1) | 1832 (43.5) | ||
| Q3 | 1394 (25.3) | 1209 (22.7) | 1086 (24.9) | 893 (21.2) | ||
| Q4 | 1071 (19.4) | 962 (18.1) | 673 (15.5) | 623 (14.8) | ||
| Missing | 235 | 321 | 184 | 371 | ||
| Processed meat (servings/day) | <0.001 | <0.001 | ||||
| Q1 | 893 (19.1) | 787 (19.0) | 837 (23.4) | 634 (18.6) | ||
| Q2 | 1914 (41.0) | 1514 (36.4) | 1413 (39.5) | 1281 (37.6) | ||
| Q3 | 1117 (23.9) | 1108 (26.7) | 698 (19.5) | 780 (22.9) | ||
| Q4 | 742 (15.9) | 745 (17.9) | 630 (17.6) | 714 (20.9) | ||
| Missing | 1081 | 1490 | 961 | 1173 | ||
| Red meat (servings/day) | 0.001 | <0.001 | ||||
| Q1 | 1489 (26.8) | 1235 (23.7) | 1228 (28.2) | 949 (22.9) | ||
| Q2 | 1439 (25.9) | 1378 (26.4) | 1325 (30.4) | 1177 (28.4) | ||
| Q3 | 1421 (25.6) | 1371 (26.3) | 1009 (23.1) | 1077 (26.0) | ||
| Q4 | 1207 (21.7) | 1232 (23.6) | 798 (18.3) | 940 (22.7) | ||
| Missing | 191 | 428 | 179 | 439 | ||
| Menopause hormone therapy | <0.001 | - | ||||
| No | 3062 (58.9) | 3334 (67.6) | - | - | ||
| Yes | 2139 (41.1) | 1599 (32.4) | - | - | ||
| Missing | 546 | 711 | - | - | ||
NSAID, non-steroidal anti-inflammatory drug.
P-value from Chi-square tests for categorical variables. Missing categories were excluded from comparison tests.
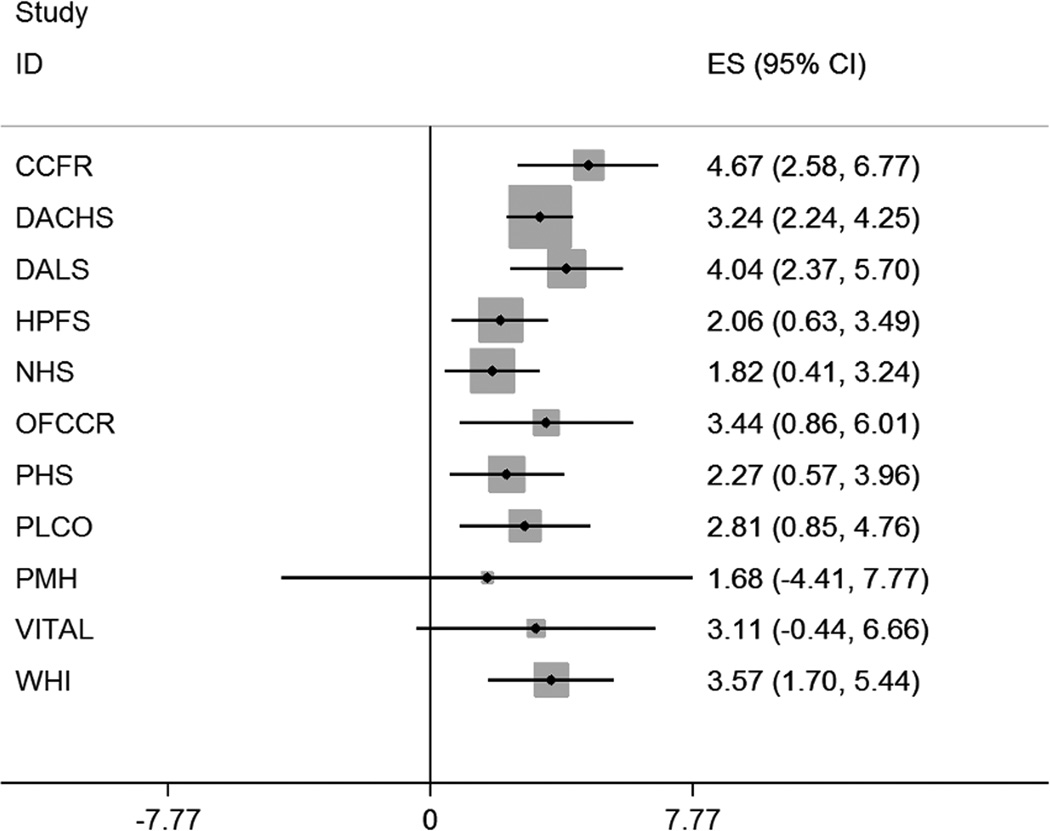
The allele frequencies for each of the 77 SNPs were consistent across the 11 studies (data not shown). The IV was normally distributed (mean, 1.97; median, 1.97; SD, 0.2; minimum, 1.37; maximum, 2.66) and the association between the IV and BMI was homogeneous across studies (test for heterogeneity, I2 = 0%; P = 0.45; Figure 1). From the pooled analysis, a one-unit increase in the IV was associated with a 3.23 kg/m2 (95% CI, 2.66–3.79) increase in BMI. The IV explained only 1.2% of the variance in BMI, but was a sufficiently strong instrument for BMI (F-statistic, 126). There were no associations of the IV with age, sex, smoking status, family history of cancer, consumption of fruit, vegetables, processed meat, and red meat or use of menopause hormone therapy (Supplementary Table S2). However, the IV was associated with history of diabetes, and we found a modest positive association between the IV and use of aspirin/NSAIDs (Supplementary Table S2).
Figure 1.
The association between the weighted genetic risk score (the instrumental variable) and body mass index (BMI) across the 11 participating studies in GECCO and C-CFR.
Individuals with greater numbers of (weighted) BMI-increasing alleles (i.e., those with a higher weighted genetic risk score) were at increased risk for CRC (per weighted allele OR, 1.31; 95%CI, 1.10–1.57; Supplementary Table S3). The IV analysis showed evidence that higher BMI was causally associated with increased risk of CRC (IV-OR per 5 kg/m2, 1.50; 95% CI, 1.13–2.01). The IV point estimate was greater in magnitude than the point estimate from conventional covariate-adjusted analysis (minimally adjusted OR per 5 kg/m2, 1.18; 95% CI, 1.15–1.22); however the 95% CIs overlapped and they were not statistically significantly different from one another (P-difference = 0.10). The findings were similar when we examined the BMI-CRC association by cancer sub-site in the colorectum (Table 2). Additional adjustment for confounding did not change the estimates in the conventional analysis (Table 2) and, likewise, adjustment of the IV analysis for age, sex, history of diabetes, and use of aspirin/NSAIDs did not change the IV risk estimate for BMI (IV-OR per 5 kg/m2, 1.51; 95%CI, 1.13–2.02).
Table 2.
Estimates of the effect of body mass index on risk of colorectal cancer (CRC), colon cancer and rectal cancer obtained using conventional covariate-adjusted and instrumental variable (IV) analysis (Odds ratios per 5 kg/m2)
| Conventional covariate-adjusted analysis |
Instrumental variable analysis |
||||
|---|---|---|---|---|---|
| Controls / Cases |
Minimally adjusted ORa (95% CI) |
Fully adjusted ORb (95% CI) |
IV-ORc (95% CI) |
Pd | |
| All | |||||
| CRC | 10286/10226 | 1.18 (1.15–1.22) | 1.17 (1.14–1.21) | 1.50 (1.13–2.01) | 0.10 |
| Colon cancer | 10286/6864 | 1.19 (1.15–1.23) | 1.18 (1.14–1.22) | 1.50 (1.08–2.07) | 0.17 |
| Rectal cancer | 10286/2365 | 1.15 (1.09–1.21) | 1.14 (1.08–1.20) | 1.26 (0.77–2.04) | 0.73 |
| Men | |||||
| CRC | 4539/4582 | 1.30 (1.23–1.38) | 1.29 (1.22–1.37) | 1.18 (0.73–1.92) | 0.70 |
| Colon cancer | 4539/2942 | 1.31 (1.23–1.39) | 1.29 (1.21–1.37) | 1.03 (0.60–1.78) | 0.39 |
| Rectal cancer | 4539/1253 | 1.25 (1.14–1.36) | 1.25 (1.13–1.37) | 1.33 (0.62–2.85) | 0.87 |
| Women | |||||
| CRC | 5747/5644 | 1.14 (1.10–1.18) | 1.12 (1.08–1.17) | 1.82 (1.26–2.61) | 0.01 |
| Colon cancer | 5747/3922 | 1.15 (1.10–1.20) | 1.13 (1.08–1.18) | 1.94 (1.30–2.91) | 0.01 |
| Rectal cancer | 5747/1112 | 1.11 (1.04–1.18) | 1.08 (1.01–1.16) | 1.24 (0.64–2.37) | 0.74 |
CI, confidence interval; OR, odds ratio.
Adjusted for age, sex, and study.
Adjusted for age, sex, study, smoking status, family history of cancer, aspirin/NSAID use, diabetes, fruit, vegetable, processed meat, red meat, and (women only) menopause hormone therapy.
Using weighted genetic risk score derived from 77 SNPs as an instrumental variable for BMI (Mendelian randomization), adjusted for study and the top three principal components of ancestry.
For comparison of IV-OR with minimally adjusted OR (P<0.05 rejects the null hypothesis that they are equal).
Using conventional methods, we found a statistically significant interaction between BMI and sex (CRC, Pinteraction<0.001; Colon, Pinteraction <0.001, Rectal, Pinteraction =0.02). The IV was a sufficiently strong instrument for BMI in stratified analyses for men (F-statistic, 74.2; R2, 1.6%) and women (F-statistic, 60.5; R2, 1.0%). For men, there was no evidence that carriers of greater numbers of (weighted) BMI-increasing alleles were at increased risk for CRC and the risk estimate for CRC obtained from the IV analysis (IV-OR per 5 kg/m2, 1.18; 95% CI, 0.73–1.92) contained 95% CIs that included the null; however, the IV results were in the same direction as the estimate from conventional covariate-adjusted analysis (minimally adjusted OR per 5 kg/m2, 1.30; 95% CI, 1.23–1.38) and the two estimates were not statistically significantly different (P-difference = 0.70). In contrast, for women, carriers of greater numbers of (weighted) BMI-increasing alleles were at increased risk for CRC and the IV estimate for CRC risk (IV-OR per 5 kg/m2, 1.82; 95% CI, 1.26–2.61) was statistically significantly different from the estimate obtained from conventional covariate-adjusted analysis (minimally adjusted OR per 5 kg/m2, 1.14; 95% CI, 1.10–1.18; P-difference = 0.01).
For men, the OR for BMI associated with CRC was greater in magnitude when the conventional covariate-adjusted analysis was restricted to those studies with measured height and weight (minimally adjusted OR per 5 kg/m2, 1.53; 95% CI, 1.33–1.76); there was no difference to the overall analysis for women (minimally adjusted OR per 5 kg/m2, 1.13; 95% CI, 1.06–1.19).
In supplementary analyses, individuals with greater numbers of (weighted) WHR-increasing alleles were at increased risk for CRC (per weighted allele OR, 1.36; 95%CI, 1.08–1.73). In contrast to that seen for BMI, men with greater numbers of (weighted) WHR-increasing alleles were at increased risk for CRC, while there was no evidence that women carriers of greater numbers of (weighted) WHR-increasing alleles were at increased risk for CRC (Supplementary Table S3).
Discussion
Observational studies have consistently reported that high BMI is associated with increased risk of CRC; however, the magnitude of the BMI-CRC association may differ between men and women (1). The limitations of observational studies, such as residual confounding (e.g., by socio-economic status, smoking, alcohol, and other lifestyle and behavioral factors), reverse causation, and reporting bias, may contribute to the heterogeneity reported in previous studies. Using Mendelian randomization methods, we re-examined the association between BMI and CRC risk without the inherent limitations in observational studies and compared the IV and conventional estimates. Overall, we found that BMI was associated with CRC risk; however, the sex-specific associations in our study are in conflict with expectations based on the existing literature of the BMI-CRC association. For women, genetically influenced BMI was statistically significantly associated with risk of CRC and our findings suggest that BMI may confer greater risk of CRC than previously reported (1). On the other hand, for men, while the IV and conventional estimates of CRC risk associated with high BMI were not statistically significantly different, the IV for BMI was not associated with CRC risk for men.
Results from large meta-analyses indicate that the risk of CRC for men increases by 20–30% per 5 kg/m2 increase in BMI. For women, the magnitude of the association was lower in all studies (~10% increased risk per 5 kg/m2) and did not always reach statistical significance (1). Consistent with these results, in our conventional covariate-adjusted analysis, the magnitude of the BMI-CRC association was substantially higher for men (32% increased risk per 5 kg/m2) than for women (15% increased per 5 kg/m2).
Using the Mendelian randomization approach, for women, we found evidence that genetically raised BMI was associated with increased risk of CRC. Importantly, the instrumental variable estimation for the BMI-CRC association for women was higher in magnitude than the risk estimate for BMI obtained from the conventional covariate-adjusted analysis. This suggests that the conventional risk estimate for women in our study, as well as those previously reported, may underestimate the true causal association between BMI and CRC risk for women. It is possible that previous estimates may have been biased toward the null if heavier women were more likely to under-report their weight than women with normal weight (3). This appears unlikely in our study as the results for women were similar between self-reported and measured BMI. There may also be sex-specific behavioral factors associated with BMI and CRC that may not be adequately measured and/or controlled for in a conventional epidemiologic analysis. This may explain why the risk estimates for BMI were different between self-reported and measured BMI for men, but not for women. It is also possible that the stronger effect in the IV analysis for women may be due to the IV for BMI reflecting genetic factors that express themselves early in life (e.g., BMI in childhood) and influence CRC risk more so than adult weight gain. An early effect of BMI on CRC risk for women may be plausible based on possible interactions between the different hormonal milieu associated with pre- and post-menopause. Mendelian randomization methods may better capture an early BMI effect on CRC risk for women than conventional epidemiologic methods. However, while our findings suggest that higher genetically influenced BMI is directly associated with increased CRC risk for women, the instrumental variable estimate is a valid test of the direction of the effect, and given the low variance explained, the exact magnitude of the effect could be in the range between the conventional estimates and our IV estimate.
For men, the conventional and IV estimates were not statistically significantly different from one another. However, the instrumental variable estimation gave evidence that genetically influenced BMI was not associated with CRC risk for men. It is unclear why the IV estimate for men was not statistically significant; however, it is unlikely that this was due to weak instrument bias as the IV was a strong instrument for BMI (F-statistic = 74.2). A possible explanation could be that the distribution of body fat, rather than total body fatness, may be an important predictor of CRC risk for men. In the supplementary analysis, we found that an IV for WHR was associated with CRC risk for men but not for women. Given that the IV was derived using SNPs associated with WHR adjusted for BMI, the two IVs in this study are largely distinct and these findings suggest that fat distribution may be important for CRC risk for men, while overall obesity may be more important for CRC risk for women.
The strengths of our study include the large sample size, centrally harmonized data, and the robust IV for the Mendelian randomization analysis. However, the findings from our Mendelian randomization study rely on three key assumptions, some of which are untestable: First, that the IV is associated with BMI. We constructed a weighted genetic risk score from 77 SNPs associated with higher BMI in an externally conducted genome-wide association study in order to maximize power (8) and provided evidence that the weighted genetic risk score (the IV) is associated with BMI in our study (a sufficiently strong instrument with F-statistics >> 10). However, our IV analyses may have been underpowered as the IV explained less than 2% of total phenotypic variation for BMI, certainly a limitation for this study but one that is common when constructing IVs for highly complex traits – and seen in the original Locke paper (24) that established the relationship between the SNPs and BMI. The second assumption with Mendelian randomization is that the IV is associated with CRC only through its association with BMI. Although the biological effects of all the variants used in constructing the IV are not well known and this assumption cannot be tested directly, we feel that it is highly unlikely that a large subset of the 77 SNPs in the score would have pleiotropic associations with BMI and CRC. If the IV is associated with CRC risk through the same metabolic pathways (e.g., inflammation, oxidative stress, glucose/insulin dysregulation) that are suspected to connect BMI to carcinogenesis, then this second assumption would still hold, since both the IV and BMI would be considered markers of altered metabolic (or related) risk factors. The final assumption is that the IV is not associated with factors that confound conventional observational associations. We found that the weighted genetic risk score was not associated with age, sex, smoking status, family history of cancer, diet, and other factors that may confound the BMI-CRC association in conventional covariate-adjusted analyses. The IV was associated with diabetes and use of aspirin/NSAIDs. The correlation with diabetes was expected since high BMI is such a strong risk factor for diabetes, and indeed, this is probably further evidence that the IV is an indicator of obesity-associated altered metabolism. The association with aspirin/NSAID-use was not expected a priori but might relate to prophylactic or treatment related use of aspirin regimens among heavier weight persons, or it might be due to chance. Nonetheless, inclusion of diabetes and aspirin/NSAID use in the IV analyses did not change the IV risk estimates for BMI. The majority of studies included in our analyses used self-reported weight and height and we showed that this may bias conventional estimates. Imprecision on genotypes from imputed SNPs is a limitation and may have resulted in loss of power in the instrumental variable analysis. A final limitation in this study is the lack of data on tumor molecular phenotype (29–31) and further research is warranted to answer this question.
Unlike estimates obtained from conventional covariate-adjusted analysis of observational data, the estimates from our IV analysis are not limited by confounding and/or bias. Therefore, they may be interpretable as a measure of the causal effect of BMI on CRC risk. Several mechanisms have been proposed to explain the association between high BMI and CRC risk, including insulin and the insulin-like growth factor system, adipokines (e.g., leptin, adiponectin), inflammation (e.g., C-reactive protein), oxidative stress, altered immunity, and steroid hormones, as discussed in recent comprehensive reviews (1, 32, 33).
Overweight and obesity are good targets for primary prevention of CRC, and men and women should be encouraged to maintain a normal BMI (18.5–25 kg/m2). Given the contrasting findings in this study for men and women, future studies are still needed to better understand the role of obesity (overall versus abdominal) in CRC carcinogenesis.
Supplementary Material
Acknowledgements
DACHS: We thank all participants and cooperating clinicians, and Ute Handte-Daub, Renate Hettler-Jensen, Utz Benscheid, Muhabbet Celik and Ursula Eilber for excellent technical assistance.
GECCO: The authors would like to thank all those at the GECCO Coordinating Center for helping bring together the data and people that made this project possible. The authors also acknowledge COMPASS (Comprehensive Center for the Advancement of Scientific Strategies) at the Fred Hutchinson Cancer Research Center for their work harmonizing the GECCO epidemiological data set. The authors acknowledge Dave Duggan and team members at TGEN (Translational Genomics Research Institute), the Broad Institute, and the Génome Québec Innovation Center for genotyping DNA samples of cases and controls, and for scientific input for GECCO.
HPFS, NHS and PHS: We would like to acknowledge Patrice Soule and Hardeep Ranu of the Dana Farber Harvard Cancer Center High-Throughput Polymorphism Core who assisted in the genotyping for NHS, HPFS, and PHS under the supervision of Dr. Immaculata Devivo and Dr. David Hunter, Qin (Carolyn) Guo and Lixue Zhu who assisted in programming for NHS and HPFS, and Haiyan Zhang who assisted in programming for the PHS. We would like to thank the participants and staff of the Nurses' Health Study and the Health Professionals Follow-Up Study, for their valuable contributions as well as the following state cancer registries for their help: AL, AZ, AR, CA, CO, CT, DE, FL, GA, ID, IL, IN, IA, KY, LA, ME, MD, MA, MI, NE, NH, NJ, NY, NC, ND, OH, OK, OR, PA, RI, SC, TN, TX, VA, WA, WY. In addition, this study was approved by the Connecticut Department of Public Health (DPH) Human Investigations Committee. Certain data used in this publication were obtained from the DPH. The authors assume full responsibility for analyses and interpretation of these data.
PLCO: The authors thank Drs. Christine Berg and Philip Prorok, Division of Cancer Prevention, National Cancer Institute, the Screening Center investigators and staff or the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial, Mr. Tom Riley and staff, Information Management Services, Inc., Ms. Barbara O’Brien and staff, Westat, Inc., and Drs. Bill Kopp, Wen Shao, and staff, SAIC-Frederick. Most importantly, we acknowledge the study participants for their contributions to making this study possible. The statements contained herein are solely those of the authors and do not represent or imply concurrence or endorsement by NCI.
PMH: The authors would like to thank the study participants and staff of the Hormones and Colon Cancer study.
WHI: The authors thank the WHI investigators and staff for their dedication, and the study participants for making the program possible. A full listing of WHI investigators can be found at: http://www.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Short%20List.pdf
Funding of Constituent Studies
GECCO: National Cancer Institute, National Institutes of Health, U.S. Department of Health and Human Services (U01 CA137088; R01 CA059045).
CCFR: National Institutes of Health (UM1 CA167551) and through cooperative agreements with members of the Colon Cancer Family Registry and P.I.s. This genome wide scan was supported by the National Cancer Institute, National Institutes of Health by U01 CA122839 and R01 CA143237 to Graham Casey. The content of this manuscript does not necessarily reflect the views or policies of the National Cancer Institute or any of the collaborating centers in the Colon Cancer Family Registry (CCFR), nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government or the CCFR. The following CCFR centers contributed data to this manuscript and were supported by National Institutes of Health: Australasian Colorectal Cancer Family Registry (U01 CA074778 and U01/U24 CA097735) Ontario Registry for Studies of Familial Colorectal Cancer (U01/U24 CA074783) Seattle Colorectal Cancer Family Registry (U01/U24 CA074794)
DACHS: German Research Council (Deutsche Forschungsgemeinschaft, BR 1704/6-1, BR 1704/6-3, BR 1704/6-4 and CH 117/1-1), and the German Federal Ministry of Education and Research (01KH0404 and 01ER0814).
DALS: National Institutes of Health (R01 CA48998 to M.L. Slattery);
HPFS is supported by the National Institutes of Health (P01 CA 055075, UM1 CA167552, R01 137178, R01 CA 151993 and P50 CA 127003), NHS by the National Institutes of Health (R01 CA137178, P01 CA 087969, R01 CA151993 and P50 CA 127003,) and PHS by the National Institutes of Health (R01 CA042182).
OFCCR: National Institutes of Health, through funding allocated to the Ontario Registry for Studies of Familial Colorectal Cancer (U01 CA074783); see CCFR section above. Additional funding toward genetic analyses of OFCCR includes the Ontario Research Fund, the Canadian Institutes of Health Research, and the Ontario Institute for Cancer Research, through generous support from the Ontario Ministry of Research and Innovation.
PLCO: Intramural Research Program of the Division of Cancer Epidemiology and Genetics and supported by contracts from the Division of Cancer Prevention, National Cancer Institute, NIH, DHHS. Additionally, a subset of control samples were genotyped as part of the Cancer Genetic Markers of Susceptibility (CGEMS) Prostate Cancer GWAS (Yeager, M et al. Genome-wide association study of prostate cancer identifies a second risk locus at 8q24. Nat Genet 2007 May;39(5):645-9), Colon CGEMS pancreatic cancer scan (PanScan) (Amundadottir, L et al. Genome-wide association study identifies variants in the ABO locus associated with susceptibility to pancreatic cancer. Nat Genet. 2009 Sep;41(9):986-90, and Petersen, GM et al. A genome-wide association study identifies pancreatic cancer susceptibility loci on chromosomes 13q22.1, 1q32.1 and 5p15.33. Nat Genet. 2010 Mar;42(3):224-8), and the Lung Cancer and Smoking study (Landi MT, et al. A genome-wide association study of lung cancer identifies a region of chromosome 5p15 associated with risk for adenocarcinoma. Am J Hum Genet. 2009 Nov;85(5):679-91). The prostate and PanScan study datasets were accessed with appropriate approval through the dbGaP online resource (http://cgems.cancer.gov/data/) accession numbers phs000207.v1.p1 and phs000206.v3.p2, respectively, and the lung datasets were accessed from the dbGaP website (http://www.ncbi.nlm.nih.gov/gap) through accession number phs000093.v2.p2. Funding for the Lung Cancer and Smoking study was provided by National Institutes of Health (NIH), Genes, Environment and Health Initiative (GEI) Z01 CP 010200, NIH U01 HG004446, and NIH GEI U01 HG 004438. For the lung study, the GENEVA Coordinating Center provided assistance with genotype cleaning and general study coordination, and the Johns Hopkins University Center for Inherited Disease Research conducted genotyping.
PMH: National Institutes of Health (R01 CA076366 to P.A. Newcomb).
VITAL: National Institutes of Health (K05 CA154337).
WHI: The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C.
The funders of the study had no role in the design, analysis, or interpretation of the data, or in writing or publication decisions related to this article.
Footnotes
Disclosure of potential conflicts of interest: No potential conflicts of interest to disclose.
References
- 1.Bardou M, Barkun AN, Martel M. Obesity and colorectal cancer. Gut. 2013;62:933–947. doi: 10.1136/gutjnl-2013-304701. [DOI] [PubMed] [Google Scholar]
- 2.Schisterman EF, Cole SR, Platt RW. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20:488–495. doi: 10.1097/EDE.0b013e3181a819a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shields M, Connor Gorber S, Tremblay MS. Estimates of obesity based on self-report versus direct measures. Health Rep. 2008;19:61–76. [PubMed] [Google Scholar]
- 4.Connor Gorber S, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev. 2007;8:307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 5.Davey Smith G, Ebrahim S. 'Mendelian randomization': can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol. 2003;32:1–22. doi: 10.1093/ije/dyg070. [DOI] [PubMed] [Google Scholar]
- 6.Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey Smith G. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med. 2008;27:1133–1163. doi: 10.1002/sim.3034. [DOI] [PubMed] [Google Scholar]
- 7.Greenland S. An introduction to instrumental variables for epidemiologists. Int J Epidemiol. 2000;29:722–729. doi: 10.1093/ije/29.4.722. [DOI] [PubMed] [Google Scholar]
- 8.Palmer TM, Lawlor DA, Harbord RM, Sheehan NA, Tobias JH, Timpson NJ, et al. Using multiple genetic variants as instrumental variables for modifiable risk factors. Stat Methods Med Res. 2012;21:223–242. doi: 10.1177/0962280210394459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peters U, Jiao S, Schumacher FR, Hutter CM, Aragaki AK, Baron JA, et al. Identification of genetic susceptibility loci for colorectal tumors in a genome-wide meta-analysis. Gastroenterology. 2013;144:799–807. doi: 10.1053/j.gastro.2012.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giovannucci E, Rimm EB, Stampfer MJ, Colditz GA, Ascherio A, Kearney J, et al. A prospective study of cigarette smoking and risk of colorectal adenoma and colorectal cancer in U.S. men. J Natl Cancer Inst. 1994;86:183–191. doi: 10.1093/jnci/86.3.183. [DOI] [PubMed] [Google Scholar]
- 11.Giovannucci E, Colditz GA, Stampfer MJ, Hunter D, Rosner BA, Willett WC, et al. A prospective study of cigarette smoking and risk of colorectal adenoma and colorectal cancer in U.S. women. J Natl Cancer Inst. 1994;86:192–199. doi: 10.1093/jnci/86.3.192. [DOI] [PubMed] [Google Scholar]
- 12.Christen WG, Gaziano JM, Hennekens CH. Design of Physicians' Health Study II--a randomized trial of beta-carotene, vitamins E and C, and multivitamins, in prevention of cancer, cardiovascular disease, and eye disease, and review of results of completed trials. Ann Epidemiol. 2000;10:125–134. doi: 10.1016/s1047-2797(99)00042-3. [DOI] [PubMed] [Google Scholar]
- 13.Prorok PC, Andriole GL, Bresalier RS, Buys SS, Chia D, Crawford ED, et al. Design of the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial. Control Clin Trials. 2000;21(6 Suppl):273S–309S. doi: 10.1016/s0197-2456(00)00098-2. [DOI] [PubMed] [Google Scholar]
- 14.White E, Patterson RE, Kristal AR, Thornquist M, King I, Shattuck AL, et al. VITamins And Lifestyle cohort study: study design and characteristics of supplement users. Am J Epidemiol. 2004;159:83–93. doi: 10.1093/aje/kwh010. [DOI] [PubMed] [Google Scholar]
- 15.Design of the Women's Health Initiative clinical trial and observational study. The Women's Health Initiative Study Group. Control Clin Trials. 1998;19:61–109. doi: 10.1016/s0197-2456(97)00078-0. [DOI] [PubMed] [Google Scholar]
- 16.Newcomb PA, Baron J, Cotterchio M, Gallinger S, Grove J, Haile R, et al. Colon Cancer Family Registry: an international resource for studies of the genetic epidemiology of colon cancer. Cancer Epidemiol Biomarkers Prev. 2007;16:2331–2343. doi: 10.1158/1055-9965.EPI-07-0648. [DOI] [PubMed] [Google Scholar]
- 17.Zanke BW, Greenwood CM, Rangrej J, Kustra R, Tenesa A, Farrington SM, et al. Genome-wide association scan identifies a colorectal cancer susceptibility locus on chromosome 8q24. Nat Genet. 2007;39:989–994. doi: 10.1038/ng2089. [DOI] [PubMed] [Google Scholar]
- 18.Slattery ML, Friedman GD, Potter JD, Edwards S, Caan BJ, Samowitz W. A description of age, sex, and site distributions of colon carcinoma in three geographic areas. Cancer. 1996;78:1666–1670. doi: 10.1002/(sici)1097-0142(19961015)78:8<1666::aid-cncr5>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 19.Slattery ML, Potter J, Caan B, Edwards S, Coates A, Ma KN, et al. Energy balance and colon cancer--beyond physical activity. Cancer Res. 1997;57:75–80. [PubMed] [Google Scholar]
- 20.Newcomb PA, Zheng Y, Chia VM, Morimoto LM, Doria-Rose VP, Templeton A, et al. Estrogen plus progestin use, microsatellite instability, and the risk of colorectal cancer in women. Cancer Res. 2007;67:7534–7539. doi: 10.1158/0008-5472.CAN-06-4275. [DOI] [PubMed] [Google Scholar]
- 21.Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister M. Protection from colorectal cancer after colonoscopy: a population-based, case-control study. Ann Intern Med. 2011;154:22–30. doi: 10.7326/0003-4819-154-1-201101040-00004. [DOI] [PubMed] [Google Scholar]
- 22.Price AL, Patterson NJ, Plenge RM, Weinblatt ME, Shadick NA, Reich D. Principal components analysis corrects for stratification in genome-wide association studies. Nat Genet. 2006;38:904–909. doi: 10.1038/ng1847. [DOI] [PubMed] [Google Scholar]
- 23.Hutter CM, Chang-Claude J, Slattery ML, Pflugeisen BM, Lin Y, Duggan D, et al. Characterization of gene-environment interactions for colorectal cancer susceptibility loci. Cancer Res. 2012;72:2036–2044. doi: 10.1158/0008-5472.CAN-11-4067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518:197–206. doi: 10.1038/nature14177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palmer TM, Sterne JA, Harbord RM, Lawlor DA, Sheehan NA, Meng S, et al. Instrumental variable estimation of causal risk ratios and causal odds ratios in Mendelian randomization analyses. Am J Epidemiol. 2011;173:1392–1403. doi: 10.1093/aje/kwr026. [DOI] [PubMed] [Google Scholar]
- 26.Staiger D, Stock JH. Instrumental variables regression with weak instruments. Econometrica. 1997;65:557–586. [Google Scholar]
- 27.Baum CF, Schaffer ME, Stillman S. Instrumental variables and GMM: estimation and testing. Stata Journal. 2003;3:1–32. [Google Scholar]
- 28.Shungin D, Winkler TW, Croteau-Chonka DC, Ferreira T, Locke AE, Magi R, et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature. 2015;518:187–196. doi: 10.1038/nature14132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Campbell PT, Jacobs ET, Ulrich CM, Figueiredo JC, Poynter JN, McLaughlin JR, et al. Case-control study of overweight, obesity, and colorectal cancer risk, overall and by tumor microsatellite instability status. J Natl Cancer Inst. 2010;102:391–400. doi: 10.1093/jnci/djq011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morikawa T, Kuchiba A, Lochhead P, Nishihara R, Yamauchi M, Imamura Y, et al. Prospective analysis of body mass index, physical activity, and colorectal cancer risk associated with beta-catenin (CTNNB1) status. Cancer Res. 2013;73:1600–1610. doi: 10.1158/0008-5472.CAN-12-2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuchiba A, Morikawa T, Yamauchi M, Imamura Y, Liao X, Chan AT, et al. Body mass index and risk of colorectal cancer according to fatty acid synthase expression in the nurses' health study. J Natl Cancer Inst. 2012;104:415–420. doi: 10.1093/jnci/djr542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aleman JO, Eusebi LH, Ricciardiello L, Patidar K, Sanyal AJ, Holt PR. Mechanisms of obesity-induced gastrointestinal neoplasia. Gastroenterology. 2014;146:357–373. doi: 10.1053/j.gastro.2013.11.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kant P, Hull MA. Excess body weight and obesity--the link with gastrointestinal and hepatobiliary cancer. Nat Rev Gastroenterol Hepatol. 2011;8:224–238. doi: 10.1038/nrgastro.2011.23. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.