Abstract
Background
Effective inpatient teaching requires intact patient memory, but studies suggest hospitalized adults may have memory deficits. Sleep loss among inpatients could contribute to memory impairment.
Objective
To assess memory in older hospitalized adults, and to test the association between sleep quantity, sleep quality and memory, in order to identify a possible contributor to memory deficits in these patients.
Design
Prospective cohort study
Setting
General medicine and hematology/oncology inpatient wards
Patients
59 hospitalized adults at least 50 years of age with no diagnosed sleep disorder.
Measurements
Immediate memory and memory after a 24-hour delay were assessed using a word recall and word recognition task from the University of Southern California Repeatable Episodic Memory Test (USC-REMT). A vignette-based memory task was piloted as an alternative test more closely resembling discharge instructions. Sleep duration and efficiency overnight in the hospital were measured using actigraphy.
Results
Mean immediate recall was 3.8 words out of 15 (SD=2.1). Forty-nine percent of subjects had poor memory, defined as immediate recall score of 3 or lower. Median immediate recognition was 11 words out of 15 (IQR=9, 13). Median delayed recall score was 1 word and median delayed recognition was 10 words (IQR= 8–12). In-hospital sleep duration and efficiency were not significantly associated with memory. The medical vignette score was correlated with immediate recall (r=0.49, p<0.01)
Conclusions
About half of inpatients studied had poor memory while in the hospital, signaling that hospitalization might not be an ideal teachable moment. In-hospital sleep was not associated with memory scores.
INTRODUCTION
Hospitalization is often utilized as a ‘teachable moment’, as patients are provided with education about treatment and disease management, particularly at discharge.1–3 However, memory impairment among hospitalized patients may undermine the utility of the teachable moment. In one study of community-dwelling seniors admitted to the hospital, one third had previously unrecognized poor memory at discharge.4
Sleep loss may be an underappreciated contributor to short-term memory deficits in inpatients, particularly in seniors, who have baseline higher rates of sleep disruptions and sleep disorders5. Patients often receive two hours less sleep than at home and experience poor quality sleep due to disruptions6,7. Robust studies of healthy subjects in laboratory settings demonstrate that sleep loss leads to decreased attention and worse recall, and that more sleep is associated with better memory performance8,9.
Very few studies have examined memory in hospitalized patients. While word-list tasks are often used to assess memory because they are quick and easy to administer, these tasks may not accurately reflect memory for a set of instructions provided at patient discharge. Finally, no studies have examined the association between inpatient sleep loss and memory. Thus, our primary aim in this study is to examine memory performance in older, hospitalized patients using a word list-based memory task and a more complex medical vignette task. Our second aim is to investigate the relationship between in-hospital sleep and memory.
METHODS
Study Design
We conducted a prospective cohort study with subjects enrolled in an ongoing sleep study at the University of Chicago Medical Center10. Eligible subjects were on the general medicine or hematology/oncology service, at least 50 years old, community-dwelling, ambulatory, and without detectable cognitive impairment on the Mini Mental State Exam11 or Short Portable Mental Status Questionnaire12,13. Patients were excluded if they had a documented sleep disorder (i.e. obstructive sleep apnea), were transferred from an ICU or were in droplet or airborne isolation, had a bedrest order, or had already spent over 72 hours in the hospital prior to enrollment. These criteria were used to select a population appropriate for wristwatch actigraphy and with low likelihood of baseline memory impairment. The University of Chicago Institutional Review Board approved this study, and participants provided written consent.
Data Collection
Memory testing
Memory was evaluated using the University of Southern California Repeatable Episodic Memory Test (USC-REMT), a validated verbal memory test in which subjects listen to a list of 15 words and then complete free-recall and recognition of the list14,15. Free-recall tests subjects’ ability to procure information without cues. In contrast, recognition requires subjects to pick out the words they just heard from distractors, an easier task. The USC-REMT contains multiple functionally equivalent different word lists, and may be administered more than once to the same subject without learning effects.15 Immediate and delayed memory were tested by asking the subject to complete the tasks immediately after listening to the word list and 24-hours after listening to the list, respectively.
Immediate Recall and Recognition
Recall and recognition following a night of sleep in the hospital was the primary outcome for this study. After one night of actigraphy recorded sleep, subjects listened as a 15-item word list (word list A) was read aloud. For the free-recall task, subjects were asked to repeat back all the words they could remember immediately after hearing the list. For the recognition task, subjects were read a new list of 15 words, including a mix of words from the previous list and new distractor words. They answered “yes” if they thought the word had previously been read to them and “no” if they thought the word was new.
Delayed Recall and Delayed Recognition
At the conclusion of study enrollment on day 1 prior to the night of actigraphy, subjects were shown a laminated paper with a printed word list (Word list B) from the USC-REMT. They were given two minutes to study the sheet and were informed they would be asked to remember the words the following day. One day later, after the night of actigraphy recorded sleep, subjects completed the free recall and “yes-no” recognition task based on what they remembered from word list B. This established delayed recall and recognition scores.
Medical Vignette
Since it is unclear how word recall and recognition tasks approximate remembering discharge instructions, we developed a 5-sentence vignette about an outpatient medical encounter, based on the logical memory component of the Wechsler Memory Scale IV, a commonly used, validated test of memory assessment.16,17 After the USC-REMT was administered following a night of sleep in the hospital, patients listened to a story and were immediately asked to repeat back in free form as much information as possible from the story. Responses were recorded by trained research assistants. The story is comprised of short sentences with simple ideas and vocabulary (Appendix 1).
Sleep: Wrist Actigraphy and Karolinska Sleep Log
Patient sleep was measured by actigraphy following the protocol described previously by our group.7 Patients wore a wrist actigraphy monitor to collect data on sleep duration and quality18. The monitor detects wrist movement by measuring acceleration.19 Actigraphy has been validated against polysomnography, demonstrating a correlation in sleep duration of 0.82 in insomniacs and 0.97 in healthy subjects20. Sleep duration and sleep efficiency overnight were calculated from the actigraphy data using Actiware 5 software.21 Sleep duration was defined by the software based on low levels of recorded movement. Sleep efficiency was calculated as the percentage of time asleep out of the subjects’ self-reported time in bed, which was obtained using the Karolinska Sleep Log22.
The Karolinska Sleep Log questionnaire also asks patients to rate their sleep quality, restlessness during sleep, ease of falling asleep and the ability to sleep through the night on a 5-point scale. The Karolinska Sleep Quality Index (KSQI) is calculated by averaging the latter 4 items23. A score of 3 or less classifies the subject in an “insomniac” range7,22.
Demographic information
Demographic information, including age, race and gender were obtained by chart audit.
Data Analysis
Data were entered into REDCap, a secure online tool for managing survey data24.
Memory scoring
For immediate and delayed recall scores, subjects received one point for every word they remembered correctly, with a maximum score of 15 words. We defined poor memory on the immediate recall test as a score of 3 or lower, based on a score utilized by Lindquist et al4 in a similar task. This score was less than half of the mean score of 6.63 obtained Parker et al for a sample of healthy 60–79 year olds in a sensitivity study of the USC-REMT14. For immediate and delayed recognition, subjects received one point for correctly identifying whether a word had been on the word list they heard or whether it was a distractor, with a maximum score of 15.
A key was created to standardize scoring of the medical vignette by assigning 1 point to specific correctly remembered items from the story (Appendix 2a). These points were added to obtain a total score for correctly remembered vignette items. It was also noted when a vignette item was remembered incorrectly; for example, when the patient remembered “left foot” instead of “right foot.” Each incorrectly remembered item received one point and these were summed to create total score for incorrectly remembered vignette items (see Appendix 2a for scoring guide.) Forgotten items were assigned zero points. Two independent raters scored each scored subject’s responses and their scores were averaged for each item. Inter-rater reliability was calculated as percentage of agreement across responses.
Statistical analysis
Descriptive statistics were performed on the memory task data. Tests for skew and curtosis were performed for recall and recognition task data. The mean and standard deviation were calculated for normally distributed data and the median and interquartile ranges were obtained for data that showed significant skew. Mean and standard deviation were also calculated for sleep duration and sleep efficiency measured by actigraphy.
Two-tailed t-tests were used to examine the association between memory and gender and African American race. Cuzick’s nonparametric test of trend was used to test the association between age quartile and recall and recognition scores.25 Mean and standard deviation for the correct total score and incorrect total score for the medical vignette were calculated. Pearson’s correlation coefficient was used to examine the association between USC-REMT memory measures and medical vignette score.
Pearson’s correlation coefficient was calculated to test the associations between sleep duration and memory scores (immediate and delayed recall, immediate and delayed recognition, medical vignette task). This test was repeated to examine the relationship between sleep efficiency and the above memory scores. Linear regression models were used to characterize relationship between inpatient sleep duration and efficiency and memory task performance. Two-tailed t-tests were used to compare sleep metrics (duration and efficiency) between high- and low-memory groups, with low memory defined as immediate recall of ≤3 words.
All statistical tests were conducted using Stata 12.0 software (College Station, TX). Statistical significance was defined as p<0.05.
RESULTS
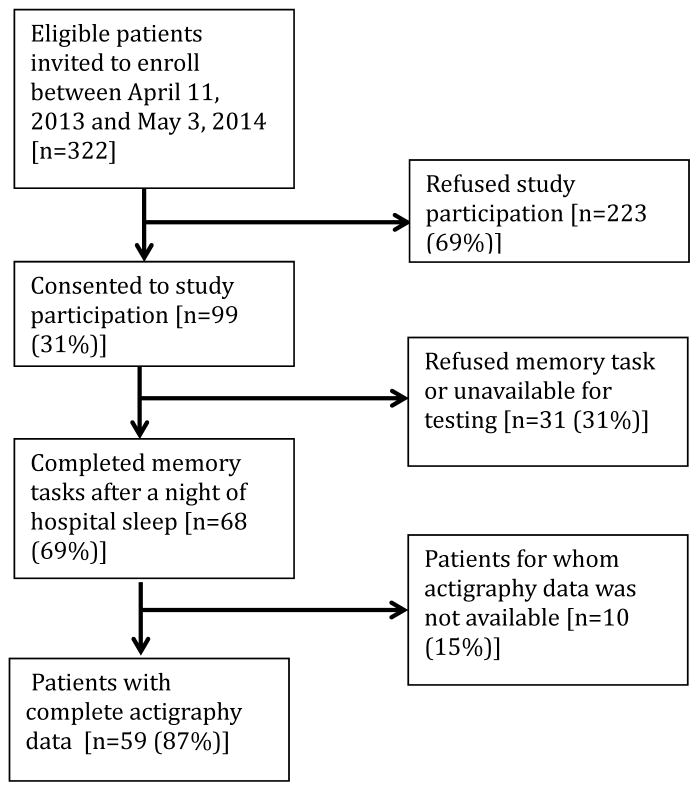
From April 11, 2013 to May 3, 2014, 322 patients were eligible for our study. Of these, 99 patients were enrolled in the study. We were able to collect sleep actigraphy data and immediate memory scores from 59 on Day 2 of the study (Figure 1).
Figure 1. Eligible and consented subjects.
322 patients were eligible for our study, of which 59 completed both memory testing and sleep testing.
The study population had a mean age of 61.6 years (SD=9.3 years). Demographic information is presented in Table 1. Average nightly sleep in the hospital was 5.44 hours (326.4 minutes, SD=134.5 minutes), while mean sleep efficiency was 70.9 (SD = 17.1), which is below the normal threshold of 85%.26,27. Forty-four percent had a KSQI score of 3 or less, representing in-hospital sleep quality in the insomniac range.
Table 1.
Patient Demographics and Baseline Sleep Characteristics, Total N=59
| Patient Characteristics | Value [n (%)] | |
|---|---|---|
| Age (in years), mean (SD) | 61.6 (9.3) | |
| Female | 36 (61.0%) | |
| BMI | ||
| Underweight (<18.5) | 3 (5.1%) | |
| Normal weight (18.5–24.9) | 16 (27.1%) | |
| Overweight (25.0–29.9) | 14 (23.7%) | |
| Obese (≥30.0) | 26 (44.1%) | |
| African American | 43 (72.9%) | |
| Non-Hispanic | 57 (96.6%) | |
| Education | ||
| Did not finish high school | 13 (23.2%) | |
| High school graduate | 13 (23.2%) | |
| Some college or junior college | 16 (28.6%) | |
| College graduate or post-graduate degree | 13 (23.2%) | |
| Discharge diagnosis (ICD-9-CM classification) | ||
| Circulatory system disease | 5 (8.5%) | |
| Digestive system disease | 9 (15.3%) | |
| Genitourinary system disease | 4 (6.8%) | |
| Musculoskeletal system disease | 3 (5.1%) | |
| Respiratory system disease | 5 (8.5%) | |
| Sensory organ disease | 1 (1.7%) | |
| Skin and subcutaneous tissue disease | 3 (5.1%) | |
| Endocrine, nutritional and metabolic disease | 7 (11.9%) | |
| Infection and parasitic disease | 6 (10.2%) | |
| Injury and poisoning | 4 (6.8%) | |
| Mental disorders | 2 (3.4%) | |
| Neoplasm | 5 (8.5%) | |
| Symptoms, signs and ill-defined conditions | 5 (8.5%) | |
| Comorbidities by self-report (n=57) | ||
| Cancer | 6 (10.5%) | |
| Depression | 15 (26.3%) | |
| Diabetes | 15 (26.3%) | |
| Heart trouble | 16 (28.1%) | |
| HIV/AIDS | 2 (3.5%) | |
| Kidney disease | 10 (17.5%) | |
| Liver disease | 9 (15.8%) | |
| Stroke | 4 (7.0%) | |
| Subject on the Hematology and Oncology service | 6 (10.2%) | |
|
| ||
| Sleep Characteristics | ||
|
| ||
| Nights in hospital prior to enrollment | ||
| 0 nights | 12 (20.3%) | |
| 1 night | 24 (40.7%) | |
| 2 nights | 17 (28.8%) | |
| 3 nights | 6 (10.1%) | |
| Received pharmacologic sleep aids | 10 (17.0%) | |
| Karolinska Sleep Quality Index scores (score ≤3) | 26 (44.1%) | |
| Sleep duration (in minutes)b, mean (SD) | 326.4 (134.5) | |
| Sleep efficiency (percent), mean (SD) | 70.9 (17.1) | |
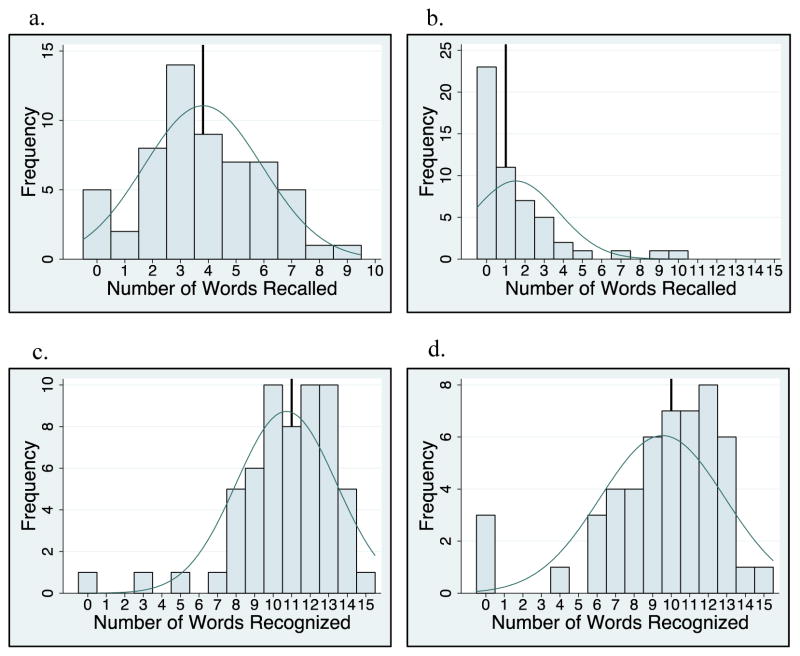
Memory test scores are presented in Figure 2. Nearly half (49%) of patients had poor memory, defined by a score of ≤3 words (Figure 2). Immediate recall scores varied significantly with age quartile, with older subjects recalling fewer words (Q1 (age 50.4–53.6) =4.9 words; Q2 (age 54.0–59.2) mean=4.1 words; Q3 (age 59.4–66.9) mean=3.7 words; Q4 (age 68.2–85.0) mean=2.5 words; p=0.001). Immediate recognition scores did not vary significantly by age quartile (Q1 (age 50.4–53.6) =10.3 words; Q2 (age 54.0–59.2) =10.3 words; Q3 (age 59.4–66.9) =11.8 words; Q4 (age 68.2–85.0) =10.4 words; p=0.992). Fifty-two subjects completed the delayed memory tasks. The median delayed recall score was low, at 1 word (IQR= 0–2), with 44% of subjects remembering 0 items. Delayed memory scores were not associated with age quartile. There was no association between any memory scores and gender or African American race.
Figure 2. Memory Scores.
Histogram of memory score distribution with superimposed normal distribution curve and solid vertical line representing the mean or median. a. Immediate recall scores were normally distributed. Mean = 3.81 word. b. Delayed recall scores showed right skew. Median = 1 word. c. Immediate recognition scores showed left skew. Median = 11 words. d. Delayed recognition scores also showed right skew. Median = 10 words.
For 35 subjects in this study, we piloted the use of the medical vignette memory task. Two raters scored subject responses. Of the 525 total items, there 98.1% agreement between the 2 raters and only 7 out of 35 subjects’ total scores differed between the two raters (detailed results in Appendix 2b). Median number of items remembered correctly was 4 out of 15 (IQR 2–6). Median number of incorrectly remembered items was 0.5 (IQR 0–1). Up to 57% (20 subjects) incorrectly remembered at least one item. The medical vignette memory score was significantly correlated with immediate recall score (r=0.49, p<0.01) but not immediate recognition score (r=0.24, p=0.16), delayed recall (r=0.13, p=0.47), or delayed recognition (r=−0.01, p=0.96). There was a negative relationship between the number of items correctly recalled by a subject and the number of incorrectly recalled items on the medical vignette memory task that did not reach statistical significance (r=−0.32, p=0.06).
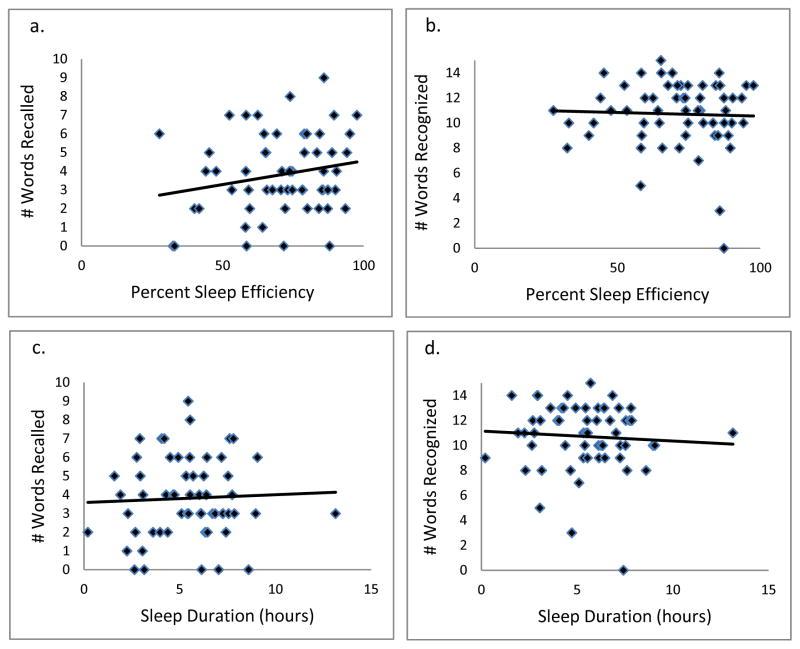
There was no association between sleep duration, sleep efficiency and KSQI with memory scores (immediate and delayed recall, immediate and delayed recognition, medical vignette task) (Table 2.) The relationship between objective sleep measures and immediate memory are plotted in Figure 3. Finally, there was no significant difference in sleep duration or efficiency between groups with high memory (immediate recall of >3 words) and low memory (immediate recall of ≤ 3 words).
Table 2.
Pearson’s correlation (r) and regression beta coefficient for memory scores and sleep measurements
| Independent variables | ||||
|---|---|---|---|---|
|
| ||||
| Sleep Duration (hours) | Sleep Efficiency (percent) | Karolinska Sleep Quality Index | ||
| Immediate Recall (n=59) | Pearson’s r | 0.044 | 0.2 | −0.18 |
| β coefficient | 0.042 | 0.025 | −0.27 | |
| p-value | 0.74 | 0.12 | 0.16 | |
| Immediate Recognition (n=59) | Pearson’s r | −0.066 | −0.037 | −0.13 |
| β coefficient | −0.080 | −0.0058 | −0.25 | |
| p-value | 0.62 | 0.78 | 0.31 | |
| Delayed Recall (n=52) | Pearson’s r | 0.028 | −0.0020 | −0.0081 |
| β coefficient | 0.027 | 0.00025 | −0.012 | |
| p-value | 0.85 | 0.99 | 0.96 | |
| Delayed Recognition (n=52) | Pearson’s r | 0.21 | 0.12 | 0.15 |
| β coefficient | 0.31 | 0.024 | −0.35 | |
| p-value | 0.13 | 0.39 | 0.29 | |
Figure 3. Scatterplot of immediate memory scores and sleep measures with regression line (N=59).
a. Immediate recall v. sleep efficiency (y = 0.0254x + 2.0148). b. Immediate recognition v. sleep efficiency (y = −0.0058x + 11.12). c. Immediate recall v. sleep duration (y = 0.0416x + 3.5872). d. Immediate recognition v. sleep duration (y = −0.0794x + 11.144). Delayed memory scores are not portrayed but similarly showed no significant associations.
CONCLUSIONS/DISCUSSION
This study demonstrated that roughly half of hospitalized older adults without diagnosed memory or cognitive impairment had poor memory using an immediate word recall task. While performance on an immediate word recall task may not be considered a good approximation for remembering discharge instructions, immediate recall did correlate with performance on a more complex medical-vignette memory task. Though our subjects had low sleep efficiency and duration while in the hospital, memory performance was not significantly associated with inpatient sleep.
Perhaps the most concerning finding in this study was the substantial number of subjects who had poor memory. In addition to scoring approximately one standard deviation lower than the community sample of healthy older adults tested in the sensitivity study of USC-REMT,14 our subjects also scored lower on immediate recall when compared to another hospitalized patient study.4 In the study by Lindquist et al. that utilized a similar 15-item word recall task in hospitalized patients, 29% of subjects were found to have poor memory (recall score of ≤3 words), compared to 49% in our study. In our 24-hour delayed recall task we found that 44% of our patients could not recall a single word, with 65% remembering one word or fewer. In their study, Lindquist et al. similarly found that greater than 50% of subjects qualified as poor memory by recalling 1 or fewer words after merely an 8-minute delay. Given these findings, hospitalization may not be the optimal ‘teachable’ moment that is often suggested to be. Use of transition coaches, memory aids like written instructions and reminders, and involvement of caregivers are likely critical to ensuring inpatients retain instructions and knowledge. More focus also needs to be given to older patients, who often have the worst memory. Technology tools, such as the Vocera Good To Go app, could allow medical professionals to make audio recordings of discharge instructions that patients may access at any time on a mobile device.
This study also has implications for how to measure memory in inpatients. For example, a vignette-based memory test may be appropriate for assessing inpatient memory for discharge instructions. Our task was easy to administer and correlated with immediate recall scores. Furthermore, the story-based task helps us to establish a sense of how much information from a paragraph is truly remembered. Our data show that only 4 items of 15 were remembered, and the majority of subjects actually misremembered one item. This latter measure sheds light on the rate of inaccuracy of patient recall. It is worth noting also that word recognition showed a ceiling effect in our sample, suggesting the task was too easy. In contrast, delayed recall was too difficult, as scores showed a floor effect with over half of our sample unable to recall a single word after 24-hour delay.
This is the first study to assess the relationship between sleep loss and memory in hospitalized patients. We found that memory scores were not significantly associated with sleep duration, sleep efficiency or with the self-reported KSQI. Memory during hospitalization may be affected by factors other than sleep, like cognition, obscuring the relationship between sleep and memory. It is also possible that we were unable to see a significant association between sleep and memory because of universally low sleep duration and efficiency scores in the hospital.
Our study has several limitations. Most importantly, this study includes a small number of subjects who were hospitalized on a general medicine service at a single institution, limiting generalizability. Also importantly, our data captures only one night of sleep and this may limit our study’s ability to detect an association between hospital sleep and memory. More longitudinal data measuring sleep and memory across a longer period of time may reveal the distinct contribution of in-hospital sleep. We also excluded patients with known cognitive impairment from enrollment, limiting our patient population to those with only high cognitive reserve. We hypothesize that patients with dementia experience both increased sleep disturbance and greater decline in memory during hospitalization. In addition, we are unable to test causal associations in this observational study. Furthermore, we applied a standardized memory test, the USC-REMT, in a hospital setting, where noise and other disruptions at the time of test administration cannot be completely controlled. This makes it difficult to compare our results with those of community-dwelling members taking the test under optimal conditions. Finally, because we created our own medical vignette task, future testing to validate this method against other memory testing is warranted.
In conclusion, our results show that memory in older hospitalized inpatients is often impaired, despite patients’ appearing cognitively intact. These deficits in memory are revealed by a word recall task and also by a medical vignette task that more closely approximates memory for complex discharge instructions.
Supplementary Material
Acknowledgments
Funding: National Institute on Aging Short-Term Aging-Related Research Program (5T35AG029795), the National Institute on Aging Career Development Award (K23AG033763) and the National Heart Lung and Blood Institute (R25 HL116372)
Footnotes
Conflicts of Interest: None
References
- 1.Fonarow GC. Importance of In-Hospital Initiation of Evidence-Based Medical Therapies for Heart Failure: Taking Advantage of the Teachable Moment. Congest Heart Fail. 2005;11(3):153–154. doi: 10.1111/j.1527-5299.2005.04293.x. [DOI] [PubMed] [Google Scholar]
- 2.Miller NH, Smith PM, DeBusk RF, Sobel DS, Taylor CB. Smoking Cessation in Hospitalized Patients: Results of a Randomized Trial. Arch Intern Med. 1997;157(4):409–415. [PubMed] [Google Scholar]
- 3.Rigotti NA, Munafo MR, Stead LF. Smoking cessation interventions for hospitalized smokers: a systematic review. Arch Intern Med. 2008;168(18):1950. doi: 10.1001/archinte.168.18.1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lindquist LA, Go L, Fleisher J, Jain N, Baker D. Improvements in Cognition Following Hospital Discharge of Community Dwelling Seniors. J Gen Intern Med. 2011;26(7):765–770. doi: 10.1007/s11606-011-1681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wolkove N, Elkholy O, Baltzan M, Palayew M. Sleep and aging: 1. Sleep disorders commonly found in older people. Can Med Assoc J. 2007;176(9):1299–1304. doi: 10.1503/cmaj.060792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yoder JC. Noise and Sleep Among Adult Medical Inpatients: Far From a Quiet Night. Arch Intern Med. 2012;172(1):68. doi: 10.1001/archinternmed.2011.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adachi M, Staisiunas PG, Knutson KL, Beveridge C, Meltzer DO, Arora VM. Perceived control and sleep in hospitalized older adults: A sound hypothesis? J Hosp Med. 2013;8(4):184–190. doi: 10.1002/jhm.2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lim J, Dinges DF. A meta-analysis of the impact of short-term sleep deprivation on cognitive variables. Psychol Bull. 2010;136(3):375–389. doi: 10.1037/a0018883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alhola P, Polo-Kantola P. Sleep deprivation: Impact on cognitive performance. Neuropsychiatr Dis Treat. 2007;3(5):553. [PMC free article] [PubMed] [Google Scholar]
- 10.Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(11):866–874. doi: 10.7326/0003-4819-137-11-200212030-00007. [DOI] [PubMed] [Google Scholar]
- 11.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 12.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;10:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 13.Roccaforte W, Burke W, Bayer B, Wengel S. Reliability and validity of the Short Portable Mental Status Questionnaire administered by telephone. J Geriatr Psychiatry Neurol. 1994;7(1):33–38. [PubMed] [Google Scholar]
- 14.Parker ES, Landau SM, Whipple SC, Schwartz BL. Aging, Recall and Recognition: A Study on the Sensitivity of the University of Southern California Repeatable Episodic Memory Test (USC-REMT) J Clin Exp Neuropsychol. 2004;26(3):428–440. doi: 10.1080/13803390490510130. [DOI] [PubMed] [Google Scholar]
- 15.Parker ES, Eaton EM, Whipple SC, Heseltine PNR, Bridge TP. University of southern california repeatable episodic memory test. J Clin Exp Neuropsychol. 1995;17(6):926–936. doi: 10.1080/01688639508402441. [DOI] [PubMed] [Google Scholar]
- 16.Morris J, Kunka JM, Rossini ED. Development of alternate paragraphs for the logical memory subtest of the Wechsler Memory Scale-Revised. Clin Neuropsychol. 1997;11(4):370–374. [Google Scholar]
- 17.Strauss Esther, Sherman Elisabeth M, Spreen Otfried. A Compendium of Neuropsychological Tests: Administration, Norms, and Commentary. 3. New York, NY: Oxford University Press; 2009. [Google Scholar]
- 18.Actiwatch2. Respironics, Inc; Murrysville, Pennsylvania: 2014. [Google Scholar]
- 19.Murphy SL. Review of physical activity measurement using accelerometers in older adults: Considerations for research design and conduct. Prev Med. 2009;48(2):108–114. doi: 10.1016/j.ypmed.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jean-Louis G, Gizycki HV, Zizi F, Spielman A, Hauri P, Taub H. The actigraph data analysis software: I. A novel approach to scoring and interpreting sleep-wake activity. Percept Mot Skills. 1997;85(1):207–216. doi: 10.2466/pms.1997.85.1.207. [DOI] [PubMed] [Google Scholar]
- 21.Chae KY, Kripke DF, Poceta JS, et al. Evaluation of immobility time for sleep latency in actigraphy. Sleep Med. 2009;10(6):621–625. doi: 10.1016/j.sleep.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 22.Harvey AG, Stinson K, Whitaker KL, Moskovitz D, Virk H. The subjective meaning of sleep quality: a comparison of individuals with and without insomnia. Sleep. 2008;31(3):383. doi: 10.1093/sleep/31.3.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Keklund G, Aakerstedt T. Objective components of individual differences in subjective sleep quality. J Sleep Res. 1997;6(4):217–220. doi: 10.1111/j.1365-2869.1997.00217.x. [DOI] [PubMed] [Google Scholar]
- 24.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cuzick J. A Wilcoxon-type test for trend. Stat Med. 1985;4(1) doi: 10.1002/sim.4780040112. [DOI] [PubMed] [Google Scholar]
- 26.Edinger JD, Bonnet MH, Bootzin RR, et al. Derivation of research diagnostic criteria for insomnia: report of an American Academy of Sleep Medicine Work Group. Sleep. 2004;27(8):1567–1596. doi: 10.1093/sleep/27.8.1567. [DOI] [PubMed] [Google Scholar]
- 27.Lichstein KL, Durrence HH, Taylor DJ, Bush AJ, Riedel BW. Quantitative criteria for insomnia. Behav Res Ther. 2003;41(4):427–445. doi: 10.1016/s0005-7967(02)00023-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.