Abstract
Objective
Vestibular rehabilitation therapy (VRT) can benefit patients with a variety of balance and vestibular disorders. This expanding field requires knowledgeable and experienced therapists; however, the practice and experience of those providing this care may vary greatly. The purpose of this study was to analyze variations in training and practice patterns among practicing vestibular rehabilitation therapists.
Study Design
Case-controlled cohort study
Setting
Investigation of outpatient physical therapy and audiology practices that offer vestibular rehabilitation conducted by a tertiary academic referral center.
Main Outcome Measure
Questionnaire-based investigation of level of training in vestibular disorders and therapy, practice patterns of vestibular rehabilitation, and referral sources for VRT patients.
Results
We identified 27 subjects within the state of Kentucky who practice vestibular rehabilitation and the questionnaire response rate was 63%. Responses indicated that 53% of respondents had no training in VRT during their professional degree program. Attendance of a course requiring demonstration of competence and techniques was 24% of participants. The development of VRT certification was significantly more favored by those who attended such courses compared with those who did not (p=0.01). 50% of therapists have direct access to patients without physician referrals.
Conclusions
There is a wide range of educational background and training among those practicing VRT. This variability in experience may affect care provided within some communities. Certification is not necessary for the practice of VRT but the development of certification is favored among some therapists to improve standardization of practice of this important specialty.
Introduction
Vestibular dysfunction is a common problem and an estimated 35.4% of adults over 40 report balance impairment.1 Additionally, an estimated 60 million doctor visits per year are attributed to the complaint of dizziness.2 Management of chronic vestibular dysfunction is complex and treatment options are limited. Patients with vestibular dysfunction not amenable to medical or surgical treatment may be candidates for vestibular rehabilitation therapy (VRT). This mode of treatment is an exercise-based treatment program targeted at reducing the symptoms of vestibular disease and improving daily functioning in patients with chronic disequilibrium through exercises that focus on adaptation of the vestibular system and the promotion of postural stability. VRT has been promoted by the American Academy of Otolaryngology-Head and Neck Surgery as “valid for the treatment of persistent dizziness due to incomplete compensation of the vestibular system, dizziness resulting from medical or surgical treatment, and acute peripheral vestibular dizziness.”3 Furthermore, VRT was stated to be of benefit in reducing the fall risk in the elderly population suffering multiple sensory and motor deficits.3
There are an ever-increasing number of disorders that are being treated with vestibular rehabilitation. VRT is now standard of care for diseases that cannot be adequately treated medically including benign paroxysmal positional vertigo (BPPV), vestibular hypofunction, and other related balance deficiencies. Rehabilitation techniques, such as the canal repositioning maneuver (CRM), have long been used to treat posterior canal BPPV with reported success rates over 80%.4 Newer techniques are being used effectively for symptom relief from horizontal canal BPPV.5 There is also clear support for the use of vestibular rehabilitation in treating in unilateral vestibular hypofunction.6 In addition, vestibular rehabilitation may be useful in reducing fall risk even in dizzy patients without documented vestibular deficits.7
Interestingly, this beneficial therapy lacks standardization within the field. Practice patterns in vestibular rehabilitation may vary widely and there is some evidence internationally that educational backgrounds are also diverse.8 Traditionally, this type of therapy has been conducted by Physical Therapists or Occupational Therapists; however, Audiologists and other allied health professionals are increasingly conducting VRT. Education regarding vestibular anatomy, physiology, pathology, and rehabilitation may come through many different routes but are not pre-requisite to the practice of VRT. The American Occupational Therapy Association has summarized recommended knowledge and practice for occupational therapists but no other published standards exist across disciplines.9 As vestibular rehabilitation practice expands both in scope and complexity, it is important for Otolaryngologists and other referring physicians to understand the practice patterns of VRT and gain insight into the therapists that are delivering this care. The purpose of this study is to assess the training background of practicing vestibular rehabilitation therapists and current practice and referral patterns.
Materials and Methods
We obtained institutional review board approval for this study (Protocol 12-0461-X1B). Practicing vestibular rehabilitation therapists within Kentucky were identified through internet search for VRT and these practitioners were self-advertised as offering VRT. Additional potential subjects were also identified through professional contacts. Additional subjects were identified based on membership to the Vestibular Disorders Association and located from that database.10 These methods resulted in the identification of 27 potential participants reported to be practicing vestibular rehabilitation therapists within the state. We contacted these therapists via phone and/or email to discuss the study. To assess practitioner's education and training as well as to assess practice patterns, we developed and administered this 37-question survey by mail or email, depending on the therapist's preference. The questionnaire was an expanded version of a validated questionnaire8 used by the Bárány Society to evaluate international VRT practice. Additional questions regarding training and practice within the United States were included. Questions pertaining to vestibular research as well as international concerns were removed to make the survey more applicable for the audience. A complete form of the modified questionnaire was piloted within a local group of vestibular therapists and optimized prior to circulation to the study subjects. We collected demographic data including therapist age, gender, practice location, and professional discipline (physical therapy, occupational therapy, or audiology), and clinical volume of patients. Education and training data was collected which included pre-degree VRT training, methods for learning VRT, attendance and completion of a competency-based course such as the Herdman Vestibular Certification course, membership in the Vestibular Disorders Association, and attitudes regarding the development of certification in the field of VRT. Open-ended questions about standardization in the education and practice of VRT were also included. Current practice patterns were assessed by collecting data on diagnostic equipment, exercise maneuvers used for treatment, type of and duration of therapies for various vestibular diseases, referral patterns and patient base, as well as what proportion of a practice is devoted to vestibular rehabilitation.
Participants were contacted by main office phone and asked to participate by completing the survey over the phone or electronically. All participants chose to complete the survey electronically. Following initial contact, follow-up telephone calls or emails were used to increase participation. The rurality of the practice setting was also recorded using USDA Beale Codes, which qualified the counties as urban, rural, or very rural according to their population density.11 A p-value<0.05 was considered statistically significant. Associations between measured variables were assessed using chi square tests for dichotomous variables and Mann Whitney U test for significant difference and association for continuous variables. Correlation analysis was performed with the Pearson's correlation test.
Results
We obtained completed surveys from 17 of the 27 practitioners with whom contact was made (63% response rate). Data pertaining to the therapist demographics is summarized in Table 1. Most of the therapists were located in urban counties. The educational background data of the therapists is summarized in Table 2. 82% of participants had a physical therapy advanced degree (masters, doctorate, or both). Only half of the participants had VRT training as a part of their formal training. Nearly 75% reported that they received their training through post-training courses and instruction; however, only 25% of participants obtained training through courses or programs that required demonstration of competence in VRT techniques. Only 25% were members of the Vestibular Disorders Association. Those participants who demonstrated competence during their training courses were more likely to report greater need/importance of certification in VRT (p=0.01). Furthermore, there was a strong correlation between membership in Vestibular Disorders Association and completion of a VRT course that required demonstration of competency (R=0.8345 p<0.001). The completion of a competency-based VRT course was moderately correlated to practice devoted to VRT (greater than 10% of practice devoted to vestibular patients) (R=0.5533 p=0.02).
Table 1. Demographics of Vestibular Rehabilitation Therapists.
| Age | Mean: 39.4 years (28-52) |
| Gender | Male: 7 Female:10 |
| County status | Urban: 12 Rural: 4 Very Rural: 1 |
Table 2. Educational Background of Participants.
| Degree obtained | DPT: 10 MPT: 14 AuD: 3 |
| VRT part of educational curriculum (at least as an elective course) | Yes: 9 (53%) No: 8 (47%) |
| Post-degree formal training (apprenticeships, national/regional conferences, continuing education) | Yes: 14 (78%) No: 3 (22%) |
| Attendance in training program requiring demonstration of techniques | Yes: 4 (24%) No: 13 (76%) |
| Membership in Vestibular Disorders Association | Yes: 4 (24%) No: 13 (76%) |
| Need and Importance of Certification in VRT | 1 (most important): 4(24%) 2: 1 (5%) 3: 6 (35%) 4: 2 (12%) 5 (not important): 4 (24%) |
Additionally we asked the practitioners the open-ended question, “What would be helpful in your mind to improve the standardization in training and/or certification in the field of vestibular rehab?” Responses are presented below:
“Board Certification under ABPTS” (American Board of Physical Therapy Specialists)
“Hands-on training for special tests associated with diagnosing condition; knowledge base of which tests would be important to determine appropriate treatment plan for condition; knowledge base of vestibular tests completed by ENTs for vestibular complications (i.e. caloric test, etc); knowledge of pharmacological effects/benefits of patient medication; knowledge of etiologies to dizziness, specific diagnoses and differences in those diagnoses and how they present clinically. Working through case studies was the best learning tool for me in the coursework for my DPT.”
“Perhaps there could be levels of competency ranging from Level 1 basic clinical testing and rehab, Level 2 Technology use and assessment - video goggles/Posturography etc. Level 3 Written/Video and Practical exam.”
“The understanding from the medical community (ie. physicians, therapists, insurance companies) that specialized training is needed to successfully treat this patient population”
“I think that physical therapy school programs should require a course and not just an elective course.”
“Increase awareness of vestibular rehab and success of PT interventions for both BPPV and vestibulopathy.”
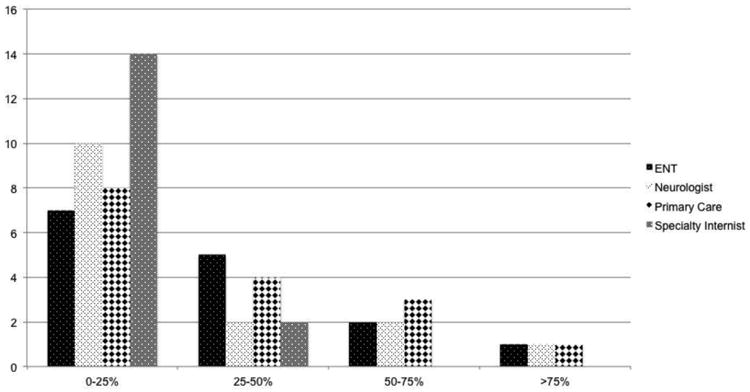
The summary of the practice patterns of the participants and referral patterns is summarized in Table 3. The number of patients seen per year with vestibular symptoms varied widely. The mean number of patients seen per year with vestibular symptoms was 66.6, range 10-400. We asked about the types of diagnostic and therapeutic equipment that were available to therapists for VRT. Of the respondents, 52% (9/17) utilized posturography to asses balance function in their patients.Two of the respondents had access to a SMART Balance Master® (NeuroCom; Clackamus, OR) for assessment and retraining of vestibular disorders. Three respondents utilized videonystagmography (VNG) and two utilized electronystagmography (ENG). Additional equipment reported included infrared goggles (3), balance foam (2) and an optokinetic drum (1). There were 3 respondents who reported no available equipment. Of these 3, all reported that less than 10% of their practice consisted of VRT, and 2 of the practitioners reported that they only treated BPPV. The duration of clinical visits were approximately 1 hour, on average, and the number of visits needed to treat varied widely, based on the therapist and the disease type (Figure 1). A diagnosis of chronic disequilibrium typically required the greatest number of visits and BPPV required the fewest. Referral patterns from physicians varied widely. 50% of therapist were able to evaluate/treat patients without a physician referral. Many patients travel extensive distances to obtain VRT. The majority of referrals came Otolaryngologists overall; however, there is significant variability in referral source and the percentage of patients obtaining VRT (Figure 2).
Table 3. Practice Patterns of Participants and Patient Demographics.
| Years in practice | Mean: 13.2 (2-29) |
| Percent or practice devoted to vestibular rehabilitation | Less than 10%: 11 (65%) Greater than 10%: 6 (35%) |
| Dynamic gait testing | Yes: 14 (78%) No: 3 (22%) |
| Functional gait testing | Yes: 15 (88%) No: 2 (12%) |
| Clinical test of sensory organization and balance (CTSIB) | Yes: 13 (72%) No: 4 (28%) |
| Length of typical evaluation session and/or treatment | Mean: 64 minutes (45-120) |
| Number of follow-up visits per disease type | BPPV: 2.1 (1-8) Unilateral hypofunction: 6.6 (1-12) Bilateral hypofunction: 8.2 (1-14) Menieres: 7.3 (0-15) Chronic disequilibrium: 9.1 (1-15) |
| Physician referral required | Yes: 8 (50%) No: 8 (50%) Unanswered: 1 |
| Farthest patient travel per visit | 73.5 minutes (15-300) |
| Percent of patients within 25 miles | <10%: 0 10-25%: 0 25-50%: 2 (12.5%) 50-75%: 7 (44%) 75-90%: 2 (12.5%) >90%: 5 (31%) No response: 1 |
Figure 1. The number of visits reported by participants that were needed to treat various vestibular disorders based on disease type.
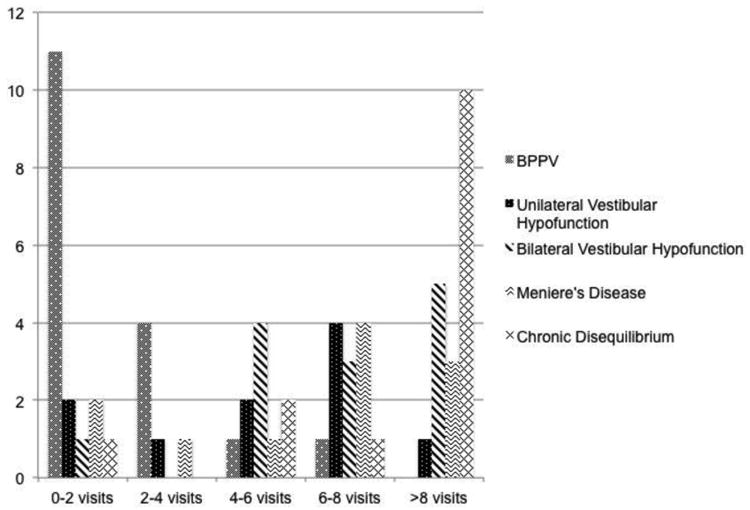
Figure 2. The percentage of participants' VRT patients referred from different types of physicians.
Discussion
This study provides insight into the training background and experiences of vestibular rehabilitation therapists. There is significant variability and overall, a lack of certification and standardization. Of our respondents, about half had exposure to VRT while obtaining their degree and most spent time and resources to seek additional training. Those that underwent competency-based VRT training devote more of their practice to VRT, are often members of the Vestibular Disorders Association, and were, in general, more supportive of a certification process. The study also complements previous efforts to evaluate the process of education and certification for VRT.8 The participants in this study provided some meaningful comments regarding methods to develop standardized training and certification for therapists practicing VRT by recommending practical competency training.
This study evaluated practice patterns and referral sources for VRT and further identified significant variability. Although many clinicians care for patients who may benefit from VRT, many clinicians are unaware of the methods and practice of vestibular rehabilitation.12 A systematic review of VRT for unilateral vestibulopathy found that VRT was a safe and effective treatment for short- and long-term management of symptoms; however, evidence is lacking to assess the efficacy on various forms of VRT.6 Some therapists offer VRT but reported that they lacked experience and equipment necessary to treat balance and vestibular disorders other than BPPV. Others devoted nearly their entire practice to treating balance disorders. In order to deliver the best care to patients with vestibular disorders, it is important for a referring physician to be cognizant of the key components of VRT and those that can provide comprehensive VRT in their region as well as the qualifications and experience of therapists offering VRT. Specialists are often involved in the referral for VRT; however, we identified that PCP referrals do make up a significant proportion of VRT patients for the participants of this study. Interestingly, many therapists reported having direct access to patients. From the standpoint of a referring physician, it is important to establish relationships with experienced therapists throughout the state. Access to healthcare continues to be an important topic nationally, especially in largely rural states, such as Kentucky where 25% of the population resides in a rural area.11 The significant travel distances and the requirement for multiple follow-up visits may result in poor compliance in VRT. Relatively few practitioners offer this type of therapy, most of whom are located in urban areas. Of our 17 participants, 12 practiced in urban counties, 4 in rural counties, and 1 in a very rural county. Therapists who spent greater than 10% of their time treating vertiginous and balance-related disorders are heavily concentrated in more urban areas (5 are in urban counties, 1 in a rural county, and none were in very rural counties). Travel distance is a significant barrier to rural populations seeking healthcare.13 Furthermore, limited numbers of VRT therapists and frequency of visits, rural patients referred for vestibular rehabilitation in Kentucky may face significant barriers to completing their therapy.
A questionnaire study such as this is limited by a small number of participants even thought the response rate was 63%. Efforts were taken to increase the through follow-up phone calls and emails to potential participants. The key providers of VRT within the state at large did participate in the study. It is quite possible that these results may underestimate the variability of training or practice patterns. Considering the limited circulation of this questionnaire, the results cannot be generalized widely; however, it is the first of its kind to specifically investigate therapist training and practices within the US. A larger-scale investigation of the topic may better assess current training and practices of vestibular rehabilitation therapists and may identify methods to provide better access to care from qualified experienced therapists.
Conclusion
This research assessed the training and practice patterns of VRT and demonstrated significant variability in practicing VRT therapists. The field of VRT lacks a certification process currently and the practice of VRT is not standardized. Development of standards within the field may improve the delivery of VRT for patients in need of this beneficial treatment.
Acknowledgments
Source of Funding: This publication was supported by the National Institutes of Health (8 KL2 TR000116-02), the National Institute of Deafness and Other Communication Disorders (1U24-DC012079-01).
Footnotes
Conflicts of Interest: The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Bibliography
- 1.Agrawal Y, Carey JP, Minor LB. Disorders of Balance and Vestibular Function in US Adults Data From the National Health and Nutrition Examination Survey, 2001-2004. Arch Intern Med. 2009;169(10):938–944. doi: 10.1001/archinternmed.2009.66. [DOI] [PubMed] [Google Scholar]
- 2.National Institute on Deafness and Other Communication Disorders, US Department of Health and Human Services, National Institutes of Health. The National Strategic Research Plan. 1995;97–3217:77–110. [Google Scholar]
- 3.Guidelines and Policies Policy Statement: Vestibular Rehabilitation. American Academy of Otolaryngology – Head and Neck Surgery. 2007 http://www.entnet.org/Practice/policyVestibularRehab.cfm.
- 4.Hunt WT, Zimmerman EF, Hilton MP. Modifications of the Epley (canalith repositioning) manoeuvre for posterior canal benign paroxysmal positional vertigo (BPPV) Cochrane Database Syst Rev. 2012 Apr 18;4:1–42. doi: 10.1002/14651858.CD008675.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Testa D, Castaldo G, De Santis C. Treatment of Horizontal Canal Benign Paroxysmal Positional Vertigo: A New Rehabilitation Technique. Scientific World Journal. 2012;2012:1–4. doi: 10.1100/2012/160475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hillier SL, McDonnell M. Vestibular rehabilitation for unilateral peripheral vestibular dysfunction. Cochrane Database Syst Rev. 2011 Feb;16(2):2–75. doi: 10.1002/14651858.CD005397.pub3. [DOI] [PubMed] [Google Scholar]
- 7.Hall CD, Heusel-Gillig L, Tusa RJ, Herdman SJ. Efficacy of gaze stability exercises in older adults with dizziness. J Neurol PhysTher. 2010;34:64–69. doi: 10.1097/NPT.0b013e3181dde6d8. [DOI] [PubMed] [Google Scholar]
- 8.Cohen HS, Gottshall KR, Graziano M, et al. International survey of vestibular rehabilitation therapists by the Barany Society Ad Hoc Committee on Vestibular Rehabilitation Therapy. Journal of Vestibular Research. 2009;19:15–20. doi: 10.3233/VES-2009-0339. [DOI] [PubMed] [Google Scholar]
- 9.Cohen HS, Burkardt A, Cronin MJ, et al. Specialized knowledge and skills in adult vestibular rehabilitation for occupational therapy practice. Amer J Occup Ther. 2006;55:661–665. doi: 10.5014/ajot.55.6.661. [DOI] [PubMed] [Google Scholar]
- 10.Vestibular Disorders Association. [Accessed 8/25/2014]; http://vestibular.org/
- 11.Davis AF. Kentucky's Urban/Rural Landscape: What is driving the differences in wealth across Kentucky? [Accessed 8/26/2014];Kentucky Annual Economic Report 2009. http://cber.uky.edu/Downloads/annrpt09.html.
- 12.Polensek SH, Tusa RJ, Sterk CE. The challenges of managing vestibular disorders: a qualitative study of clinicians' experiences associated with low referral rates for vestibular rehabilitation. Int J Clin Pract. 2009;63:1604–1612. doi: 10.1111/j.1742-1241.2009.02104.x. [DOI] [PubMed] [Google Scholar]
- 13.Buzza C, Ono SS, Turvey C, et al. Distance is Relative: Unpacking a Principal Barrier in Rural Healthcare. J Gen Intern Med. 2011 Nov;26:648–654. doi: 10.1007/s11606-011-1762-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


