Abstract
Background
Subjective responses to alcohol (SR) have been implicated in alcoholism etiology, yet less is known about the latent factor structure of alcohol responses. The aim of this study is to examine the factor structure of SR using a battery of self-report measures during a controlled alcohol challenge.
Methods
Non-treatment seeking drinkers (N = 242) completed an intravenous alcohol challenge including the following SR measures: Biphasic Alcohol Effects Scale, Subjective High Assessment Scale, Profile of Mood States, Alcohol Urge Questionnaire, and single items assessing alcohol ‘Liking,’ and ‘Wanting.’ Ascending limb target Breath Alcohol Concentrations were 0.02, 0.04 and 0.06, and descending limb target was 0.04 g/dl. Exploratory factor analyses were conducted separately on estimates of mean and dose responses on the ascending limb and on descending limb data. To examine the generalizability of this factor structure these analyses were repeated in heavy drinkers (≥14 drinks/week for men, ≥7 for women; n = 132) and light drinkers (i.e. non-heavy drinkers; n = 110).
Results
In the full sample, a 4-factor solution was supported for ascending limb mean and dose responses and descending limb data representing the following SR domains: Stimulation/Hedonia, Craving/Motivation, Sedation/Motor Intoxication, and Negative Affect. This 4-factor solution was replicated in heavy drinkers. In light drinkers however, SR was better summarized by a 3-factor solution where ascending mean and descending limb responses consisted of Stimulation/Hedonia, Craving/Motivation and a general negative valence factor, and dose responses consisted of a general positive valence factor, Sedation/Motor Intoxication and Negative Affect.
Conclusions
These findings suggest that SR represents a multifaceted construct with consistent factor structure across both ascending and descending limbs. Further, as drinking levels escalate more defined Craving/Motivation and negative valence dimensions may emerge. Longitudinal studies examining these constructs are needed to further our understanding of SR as potentially sensitive to alcohol-induced neuroadaptation.
Keywords: Subjective Response, Factor Analysis, Stimulation, Craving, Sedation
Introduction
The acute subjective responses to alcohol (SR) are biphasic in nature (Earleywine, 1994; Earleywine and Martin, 1993; Martin et al., 1993), with individuals reporting stimulatory and hedonic subjective effects as breath alcohol content (BrAC) rises or is at a peak (King, de Wit, et al., 2011; Roche et al., 2014), and largely sedative and aversive effects as BrAC declines (Newlin and Thomson, 1990; Ray et al., 2009). While this pattern of SR has been characterized across numerous acute alcohol administration studies, individual SR has been shown to be highly variable and sensitive to a multitude of factors, including the alcohol dose that was administered and risk factors for development of an alcohol use disorder (AUD; King, de Wit, et al., 2011; Quinn and Fromme, 2011). In turn, the direction and magnitude of an individual’s SR may play a significant role in their future alcohol use and risk for the development of an AUD. For example, in the laboratory, greater stimulatory and hedonic SR is associated with increased alcohol preference and self-administration (Corbin et al., 2008; de Wit and Doty, 1994), whereas greater sedative and aversive SR, or reduced stimulatory and hedonic SR, are associated with decreased alcohol consumption and preference (Chutuape and de Wit, 1994; de Wit et al., 1989). Furthermore, sons of alcohol dependent individuals (versus controls) display a reduced sedative/aversive SR in the laboratory (Schuckit, 1984) and this SR is predictive of future AUD development, independent of the risk conveyed by family history of alcoholism (Schuckit et al., 2004; Schuckit and Smith, 1996). Further, heavy drinkers, compared to light drinkers, display greater stimulatory and hedonic SR during the rising BrAC limb and reduced sedative SR during the declining BrAC limb, a pattern which was predictive of future increases in binge drinking and the number of AUD symptoms (King, de Wit, et al., 2011; King et al., 2014; Roche et al., 2014). Given the variability in SR and its importance to understanding the development of AUD, clearly characterizing the nature and measurement of SR is a high research priority.
While SR has been well characterized and is relatively stable within individual samples of at-risk drinkers (Roche et al., 2014; Schuckit and Smith, 1996), there is little consilience on SR across studies or between different populations of at-risk drinkers. As a result, the role of independent dimensions of SR in the development in AUD remains under debate (King, Roche, et al., 2011; Newlin and Renton, 2010; Schuckit, 2011). Both heightened and attenuated responses to alcohol have been theorized to contribute to AUD development among young adults with family history of the disorder or who regularly binge drink (King, de Wit, et al., 2011; King et al., 2014; Newlin and Renton, 2010; Newlin and Thomson, 1990; Quinn and Fromme, 2011; Schuckit, 2011; Schuckit and Smith, 1996). These seemingly paradoxical theories on the relationship between SR and AUD development have been speculated to be due to several methodological inconsistencies, including the use of multiple and disparate SR measures across alcohol administration studies (King, Roche, et al., 2011; Ray et al., 2009, 2010). For example, a seminal series of studies by Schuckit and colleagues has indicated that reduced SR, as measured by the Subjective High Assessment Scale (SHAS), is highly predictive of future AUD development (Schuckit et al., 2004; Schuckit and Smith, 1996). However, the SHAS appears to best describe “maximum terrible feelings” in response to alcohol (Schuckit, 1985; Schuckit and Gold, 1988) or to be most strongly related to the sedative effects of alcohol (Ray et al., 2009, 2010). Thus, the aforementioned series of studies may have only characterized the role of the aversive or sedative SR in AUD development without considering the contribution of the hedonic and stimulatory dimensions of SR. This is relevant, as the degree of stimulatory and hedonic SR is predictive of AUD symptomatology in heavy drinkers (King, de Wit, et al., 2011; King et al., 2014) and the positively reinforcing effects of alcohol are prominent in theories of AUD development (Newlin and Thomson, 1990). Yet, while the King and colleagues experiments used multiple measures to ensure the assessment of stimulating, sedating, and hedonic components of the SR, they did not include the SHAS, rendering the comparison and synthesizing of findings with the Schuckit studies difficult.
While the concurrent use of multiple measures certainly provides a more comprehensive assessment of individual differences in SR, they also raise issues regarding how to best define the core constructs of SR and may even complicate the integration of findings in the alcohol administration literature because of the ambiguity of the relationship between the SR measures (Ray et al., 2009, 2010). A more parsimonious conceptual understanding of the multiple dimensions encompassing SR would help advance and integrate the seemingly paradoxical SR literature. To that end, a previous study by our group (Ray et al., 2009) assessed SR across the rising BrAC limb during an alcohol administration study in a sample of heavy drinkers and examined the latent factor structure of SR as indexed by three commonly used measures: the SHAS , the Biphasic Alcohol Effects Scale (BAES: Martin et al., 1993), and the Profile of Mood States (POMS: McNair et al., 1971). Results revealed a three-factor model which captured the following dimensions of subjective intoxication: (a) stimulation and other pleasant effects; (b) sedation and unpleasant effects; and (c) alleviation of tension and negative mood. Findings from this study support the notion that different measures of SR uniquely assess domains of individual differences in the phenomenology of the construct, and that SR is multifaceted and should not be simply defined as either positive or negative on a single dimension. Rather, SR at moderate levels of alcohol dosing appears to have concomitant dimensions of positive reinforcement, negative reinforcement, and punishment (Ray et al., 2009).
To further our understanding of SR, the goal of the present study is to characterize the psychological structure of SR using exploratory factor analysis on a battery of self-report measures during a controlled intravenous alcohol challenge. To extend the results of our prior factor analytic work (Ray et al., 2009) and to determine whether the factor structure of SR differs as a function of drinking pattern, the current study included two groups of drinkers (i.e., heavy and light drinkers). Furthermore, we seek to expand the conceptualization of SR measurement beyond the SHAS, BAES, and POMS via inclusion of a commonly used measure alcohol craving, the Alcohol Urge Questionnaire (Bohn et al., 1995; MacKillop, 2006) and measures of alcohol ‘Liking’ and ‘Wanting’ based on incentive sensitization theory (King, de Wit, et al., 2011; King et al., 2014; Robinson and Berridge, 2001). These additions are important for the promotion of consilience across alcohol challenge studies as no previous research has empirically established the structural relationship between craving, ‘Liking,’ ‘Wanting’ and SR domains. Further we will examine the factor structure of these SR domains on both the ascending and descending limb of alcohol intoxication. We hypothesized that we would replicate the 3-factor model previously observed in heavy drinkers (Ray et al., 2009) with the addition of a fourth craving dimension. Further, as dose-dependent increases in SR along the ascending limb have been reported (e.g. King, de Wit, et al., 2011; Ray et al., 2009) this study characterized the latent factor structure of ascending limb SR at both the level of mean response, and response to an escalating dose in addition to descending limb SR. In light of previous work validating the BAES across ascending and descending limbs (Rueger et al., 2009) we hypothesized that the factor structure of SR would be consistent across these three levels of analysis.
Methods
Participants
This study was approved by the Human Research Review Committee at the University of New Mexico. Non-treatment seeking drinkers (N = 242) were recruited from the community through fliers and advertisements targeting regular drinkers over the age of 21. In order to reduce the possibility of adverse events in the alcohol challenge, participants were required to be regular drinkers reporting at least 3 or more drinks (2 for women) twice per week. Participants with a history of depression with suicidal ideation or lifetime psychotic disorder were excluded. Based on their past 60-day drinking history, participants were split into two groups based on whether they were heavy drinkers (N = 132; i.e. ≥ 14 drinks per week for men, ≥ 7 for women; NIAAA, 1995) or light drinkers (N = 110; < 14 (7 for women) drinks per week).
Screening Procedure
Initial eligibility was conducted via telephone screening, and eligible participants were then invited to a laboratory session. Upon arriving to the laboratory, participants provided written informed consent, were breathalyzed (Alcosensor IV from Intoximeters, Inc.), provided urine for a drug screen, and completed a battery of self-report questionnaires and interviews. All participants were required to test negative on a urine drug screen (except marijuana) and to have a BrAC reading of zero, otherwise they were rescheduled. Female participants were required to test negative for pregnancy. This in-person assessment visit took approximately 2 hours after which time eligible participants traveled with the experimenter to a university-based hospital for the alcohol administration procedure.
Alcohol Administration Paradigm
Alcohol was administered intravenously in order to assess participants’ subjective response to alcohol as distinct from learned responses to alcohol cues, and to allow for precise experimental control over BrAC (Li et al., 2001). Each participant was tested individually following an established infusion protocol (Ray and Hutchison, 2004; Ray et al., 2013). Participants were seated in a recliner chair with an IV placed in their non-dominant arm. Alcohol was administered using a 5% alcohol solution. Participants were infused at a rate of 0.166 ml/min × body weight in kilograms (0.126 ml/min × body weight for females). The alcohol infusion started at half target rate, to ensure safety, and was then escalated to the full rate after 5 minutes of monitoring. BrAC was measured via breathalyzer every three to five minutes. Target ascending limb BrACs were 0.02, 0.04, and 0.06 g/dl. Upon reaching each target BrAC, infusion rates were reduced by half to maintain BrAC stable during testing (i.e. short-term clamping). Participants were told that they would receive alcohol but remained blinded to their BrAC throughout the experiment. The IV alcohol administration resulted in highly controlled BrAC levels at each assessment of the ascending limb: mean BrAC (SD): 0.020 (0.001), 0.040 (0.002), and 0.060 (0.002) g/dl. Participants took an average of 15.77 minutes to reach a BrAC of 0.02, 15.97 minutes (from assessment completion) to go from a BrAC of 0.02 to 0.04, and, 16.48 minutes to reach the last target BrAC of 0.06. Participants were maintained at each target BrACs for approximately 5-7 minutes while they completed self-reports of SR. After completion of the 0.06 assessments, the IV catheter was removed. Participants’ BrAC was monitored via breathalyzer approximately every 5 minutes and participants completed one descending limb self-report battery (target BrAC 0.04 g/dl).
Measures
Alcohol Use Measures
The Timeline Follow-Back (TLFB) was administered in interview format to capture daily alcohol use over the 60 days prior to the visit (Sobell et al., 1988). Several indicators of alcohol use quantity and frequency were computed from the TLFB included drinks per drinking day (DPDD) and number of drinking days (Drinking Days). TLFB data were used to group participants based on their drinking pattern over the past 60 days (i.e., light vs. heavy drinking groups).
Subjective Response Measures
The following self-report measures were selected based on their frequent use in alcohol challenge research and were collected at the following BrAC time points: ascending 0.02, 0.04 and 0.06 g/dl and descending 0.04 g/dl. The Biphasic Alcohol Effects Scale (BAES) was used to capture self-reported feelings of stimulation and sedation in response to alcohol and is a reliable and valid measure (Erblich and Earleywine, 1995; Martin et al., 1993; Roche et al., 2014). In this sample, both BAES subscales were found to have excellent reliability at each BrAC time point (α’s ≥ 0.83). The Subjective High Assessment Scale (SHAS) captured subjective feelings of alcohol intoxication. This measure was adapted from Schuckit (1984) and has been widely used in alcohol challenge studies (Ray et al., 2012, 2009). The SHAS was found to be highly reliable (α’s ≥ 0.88). The Profile of Mood States (POMS) is a popular affect scale with four dimensions: positive mood, negative mood, vigor, and tension. This version of the POMS has been validated in the context of alcohol administration at the doses examined in the present study (Ray et al., 2009). The vigor and positive mood subscales were found to have good reliability at every time point (α’s ≥ 0.85) and the tension and negative mood subscales had adequate internal-reliability (α’s ≥ 0.61). The Alcohol Urge Questionnaire (AUQ) assesses state alcohol craving and has demonstrated high reliability in experimental studies including alcohol administration (Bohn et al., 1995; MacKillop, 2006). The AUQ was highly reliable (α’s ≥ 0.84). Alcohol ‘Liking’ and ‘Wanting’ were assessed via single items from the Alcohol Rating Scale (Liking: ‘How much did you like the exposure to alcohol?’; Wanting: ‘Do you want to be infused with more alcohol?’; Hobbs et al., 2005). Both liking and wanting were rated on a 10-point Likert scale.
Data Analytic Strategy
In order to capture ascending limb subjective response to alcohol both at the level of mean response and across alcohol-dose, a series of linear multi-level random coefficient growth models were conducted on each SR variable. In these models, BrAC was centered at the 0.04 g/dl time point, and both intercepts and linear slopes along rising BrAC were estimated as random effects at the subject level. This analytic scheme is comparable to conducting an OLS regression in each subject with a mean centered predictor variable (BrAC), which produces an intercept value equal to the mean of the outcome, and a slope representing the linear effect of BrAC. This methodology thus allows for the estimation of individual participants’ mean response (predicted value at the mean BrAC time point) and dose response (linear effect of an escalating alcohol dose) parameters, via empirical Bayesian estimation. This approach has been shown to be superior to conducting a series of ordinary linear regression in each subject independently, as it allows for parameter estimation with missing data, and utilizes data from all participants in parameter estimation, thus reducing the influence of random measurement error (Raudenbush and Bryk, 2001). These analytic procedures were selected for the following reasons: 1) To limit the number and redundancy of statistical tests. 2) Mean and dose-response variables represent more mathematically dissociable aspects of alcohol response (mean r = 0.39, versus 0.82 for individual time points), thus providing a stronger test of the true psychological structure of SR, particularly if a consistent factor structure is observed, and 3) To reduce the influence of random measurement error (Raudenbush & Bryk, 2001). Of note, the dose-response examined in this study is referring to the effect of a single escalating dose from a single alcohol administration. This is opposed to more traditional pharmacological dose studies where different doses are administered at separate sessions. All multilevel modeling was conducted using the lme function in the multilevel package (Bliese, 2008) in R version 2.13.1.
After these empirical Bayesian parameter estimates were computed for each subject, a series of exploratory factor analyses were conducted on the full sample to examine the latent factor structure of SR. Exploratory factor analysis was conducted using the fa function in the psych package (Revelle, 2014). A minimum residual extraction technique was used to minimize the risk of Heywood cases while still producing reliable indices of latent factor structure (Revelle, 2014) and the Scree test was used to determine the number factors to extract (Velicer and Jackson, 1990). Oblique factor rotation via direct oblimin was used which allows factors to be correlated (Costello and Osborne, 2005). A factor loading threshold of 0.32 was used to determine item inclusion in a factor (Tabachnick and Fidell, 2001). While specific recommendations for adequate sample size in exploratory factor analysis have been contested in the statistics literature (e.g. Costello and Osborne, 2005), factor analyses performed in this study exceeded the canonical recommendation of ≥ 10 subjects per variable (Everitt, 1975).
Analytic procedures for descending limb data were nearly identical with a few exceptions. First, since descending limb data was only collected at a single time point, factor analytic techniques were applied to the SR raw data. Furthermore, owing to the lack of a clamping procedure on the descending limb, observed BrAC’s at this time point were substantially more variable (SD = 0.007). Thus, only data from subjects with a measured BrAC ≥ 0.030 and ≤ 0.050 were included in the analyses (N = 200; 111 heavy drinkers and 89 light drinkers).
Results
Sample Characteristics
Sample characteristics are reported in Table 1. No differences were observed between drinking groups (i.e., light vs. heavy drinkers) in terms of demographic variables including cigarette smoking (p’s ≥ 0.31). As expected, heavy drinkers reported greater drinking frequency and quantity and more alcohol related problems (p’s < 0.001).
Table 1.
Sample characteristics and tests of drinking group differences.
| Light Drinkers (N = 110) |
Heavy Drinkers (N = 132) |
Statistical Test | |
|---|---|---|---|
| Age | 25.75 (4.04) | 25.53 (4.32) | t = 0.41, p = 0.68 |
| Sex (% Male) | 65% | 62% | Χ2 (1) = 0.22, p = 0.64 |
| Ethnicity (% White) | 45% | 52% | Fisher Exact p = 0.31 |
| Education (years) | 14.76 (2.49) | 14.61 (2.21) | t = 0.48, p = 0.63 |
| Cigarette Smoking Days (past 60) | 20.03 (96.58) | 21.53 (26.20) | t = 0.17, p = 0.86 |
| DPDD | 3.53 ( 1.61) | 6.12 ( 2.80) | t = 8.60, p < 0.001 |
| Drinking Days | 16.27 (9.64) | 32.89 (11.90) | t = 11.80, p< 0.001 |
| Heavy Drinking Days | 3.95 (4.47) | 20.36 (11.90) | t = 13.68, p < 0.001 |
| AUDIT | 9.10 (4.33) | 14.22 (5.04) | t = 8.41, p < 0.001 |
Note: Ethnicity differences between groups were tested as a 5 level categorical variable and overall distribution of ethnicity was not found to differ between groups; however, for simplicity of presentation, only percent Caucasian is reported.
Ascending Limb Mean Response Factor Structure
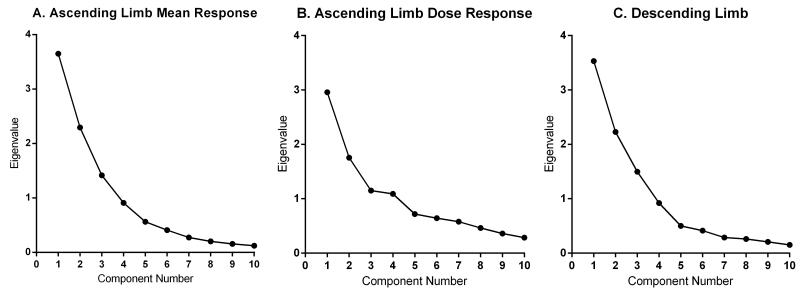
For mean response over the ascending limb, examination of the Scree plot (Figure 1A) suggested a 4-factor solution for the full sample. These four factors cumulatively explained 73% of the variance in SR variables with each factor contributing a substantial amount of variance (21%, 18%, 18% and 15%). All items loaded ≥ 0.56 on their primary factor, and only one item, POMS Positive Mood, cross-loaded with both Factors 1 and 4 (loadings = 0.61 and −0.44 respectively).
Figure 1.
Scree plots of subjective responses to alcohol in the full sample in terms of (A) ascending limb mean response across the alcohol challenge, (B) change in response along an ascending limb alcohol dose, and (C) descending limb of the alcohol challenge.
As shown in Table 2, Factor 1 comprised the scales BAES Stimulation, POMS Positive Mood and POMS Vigor, suggesting that this factor represents a stimulatory and hedonic rewarding component of SR. Factor 2 was indexed by the AUQ as well as the ‘Liking’ and ‘Wanting’ items, suggesting that it represents a craving or motivational component of subjective response to alcohol. Factor 3 was indexed by the BAES Sedation and the SHAS scales indicating that it represents the sedative and motor intoxication responses. Finally, Factor 4 was indicated by the POMS Tension and Negative Mood subscales as well as a negative loading of the POMS Positive Mood subscale suggesting that this factor represents a negative affect dimension. Factors were also found to correlate with one another (r-range −0.22 – 0.42, Table 2).
Table 2.
Factor loadings and inter-factor correlations from the full sample. Significant factor loadings are bolded. In the full sample, a 4-factor solution was supported both for mean and dose responses representing the following SR domains: Stimulation/Hedonia, Craving/Motivation, Sedation/Motor Intoxication, and Negative Affect.
|
Ascending Limb Mean Response
|
Ascending Limb Dose Response
|
|||||||
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 1 | Factor 2 | Factor 3 | Factor 4 | |
|
|
|
|||||||
| BAES Stimulation | 0.75 | 0.11 | 0.14 | 0.11 | 0.48 | 0.24 | 0.10 | 0.06 |
| POMS Pos. Mood | 0.61 | 0.02 | 0.18 | − 0.44 | 0.63 | 0.10 | 0.10 | −0.17 |
| POMS Vigor | 0.99 | −0.02 | −0.08 | 0.04 | 0.85 | −0.09 | −0.06 | 0.04 |
| AUQ | 0.04 | 0.56 | −0.04 | 0.09 | 0.18 | 0.12 | 0.43 | −0.01 |
| Liking | −0.02 | 0.89 | 0.09 | −0.03 | 0.29 | 0.27 | 0.38 | 0.08 |
| Wanting | 0.02 | 0.81 | −0.09 | 0.00 | −0.06 | −0.06 | 0.85 | −0.01 |
| BAES Sedation | 0.01 | −0.05 | 0.94 | −0.01 | −0.15 | 0.74 | −0.07 | −0.03 |
| SHAS | 0.00 | 0.10 | 0.88 | 0.07 | 0.05 | 0.91 | 0.01 | 0.02 |
| POMS Tension | 0.09 | 0.00 | 0.01 | 0.90 | 0.00 | 0.00 | 0.00 | 0.87 |
| POMS Neg. Mood | −0.11 | −0.06 | 0.20 | 0.66 | −0.30 | 0.09 | −0.02 | 0.33 |
| Inter-factor Correlations |
Inter-factor Correlations |
|||||||
| Factor 1 | Factor 2 | Factor 3 | Factor 1 | Factor 2 | Factor 3 | |||
| Factor 2 | 0.33 | Factor 2 | 0.14 | |||||
| Factor 3 | 0.29 | 0.42 | Factor 3 | 0.31 | 0.22 | |||
| Factor 4 | −0.22 | −0.11 | 0.21 | Factor 4 | −0.10 | 0.06 | −0. 10 | |
Ascending Limb Dose-Response Factor Structure
As with ascending limb mean response, examination of the Scree plot suggested a 4-factor solution for alcohol dose responses (Figure 1B). These 4 factors cumulatively explained 54% of the overall variance and each factor contributed a substantial amount of variance (17%, 16%, 12%, and 9%). All items loaded ≥ 0.33 on their respective factors. Each item loaded on one and only one factor.
The factor structure of ascending limb dose-responses was nearly identical to that observed for mean response (Table 2). Factor 1 comprised the BAES Stimulation and POMS Positive Mood and Vigor subscales. Factor 2 was indicated by the BAES Sedation subscale as well as the SHAS. Factor 3 was comprised by the AUQ, ‘Liking’ and ‘Wanting.’ Lastly, Factor 4 was comprised of the POMS Tension and Negative Mood subscales. Factors were also found to correlate with one another (r-range −0.10 – 0.31). These results revealed that, in the full sample, the factor structure of the ascending mean responses and the dose-responses were consistent, representing the four domains of: Stimulation/Hedonia, Craving/Motivation, Sedation/Motor Intoxication, and Negative Affect.
Descending Limb Factor Structure
Four factors were also suggested for descending limb SR (Figure 1C). These factors cumulatively explained 71% of the overall variance and each factor contributed a significant amount of variance (20%, 19%, 17%, and 14%). Each item loaded ≥ 0.55 on their primary factor, though two items exhibited cross-loading. Specifically, POMS Positive Mood and POMS Negative Mood both loaded onto Factors 2 and 4 (Table 3).
Table 3.
Descending limb factor loadings and inter-factor correlations from the full sample. Significant factor loadings are bolded. In the full sample, a 4-factor solution was supported descending limb alcohol responses representing the following SR domains: Stimulation/Hedonia, Craving/Motivation, Sedation/Motor Intoxication, and Negative Affect.
| Descending Limb | ||||
|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | |
|
|
||||
| BAES Stimulation | 0.81 | 0.10 | 0.07 | 0.08 |
| POMS Pos. Mood | 0.56 | 0.23 | 0.02 | − 0.42 |
| POMS Vigor | 0.96 | −0.08 | −0.01 | 0.02 |
| AUQ | 0.10 | −0.03 | 0.65 | 0.23 |
| Liking | 0.06 | 0.18 | 0.64 | −0.10 |
| Wanting | −0.04 | −0.04 | 0.91 | −0.06 |
| BAES Sedation | −0.04 | 0.88 | 0.00 | 0.00 |
| SHAS | 0.07 | 0.90 | 0.03 | 0.05 |
| POMS Tension | 0.07 | 0.03 | −0.05 | 0.88 |
| POMS Neg. Mood | −0.16 | 0.34 | 0.01 | 0.55 |
|
|
||||
| Inter-factor Correlations |
||||
| Factor 1 | Factor 2 | Factor 3 | ||
| Factor 2 | 0.32 | |||
| Factor 3 | 0.27 | 0.31 | ||
| Factor 4 | −0.21 | 0.19 | −0. 17 | |
The factor structure of descending limb alcohol responses was fully analogous to the results obtained for both mean and dose responses on the ascending limb (Table 3). Factor 1 comprised the BAES Stimulation and POMS Positive Mood and Vigor subscales. Factor 2 was indicated by the SHAS, the BAES Sedation, and the POMS Negative Mood subscales. Factor 3 was comprised of the AUQ, ‘Liking’ and ‘Wanting.’ Lastly, Factor 4 was comprised of the POMS Tension and Negative Mood subscales and negatively loading POMS Positive Mood. Factors were also found to correlate with one another (r-range −0.21 – 0.32). In sum, the factor structure of SR was found to be consistent across ascending and descending limbs representing the four domains of: Stimulation/Hedonia, Craving/Motivation, Sedation/Motor Intoxication, and Negative Affect.
Factor Structure by Drinking Group
In order to examine whether the latent factor structure of alcohol responses was reliable across levels of drinking, the sample was split by weekly heavy drinking, followed by identical EFA procedures conducted in these groups separately.
The identified latent factor structure of alcohol response in heavy drinkers was fully analogous to that identified in the full sample (Table 4). Specifically, a 4 factor solution was suggested for ascending limb mean response with the 4 factors explaining 72% of the total variance with identical item clustering as with the full sample. A 4 factor solution was also suggested in terms of ascending limb dose-response and descending limb with identical item clustering as with the full sample (54% and 71% variance explained respectively). Thus, as with the full sample, in the heavy drinking subsample, alcohol responses at all levels of analysis were clustered into the 4 domains of Stimulation/Hedonia, Craving/Motivation, Sedation/Motor Intoxication, and Negative Affect.
Table 4.
Factor loadings and inter-factor correlations in light and heavy drinkers. Significant loadings are bolded. In heavy drinkers, the factor structure was analogous to the full sample. In light drinkers SR was better summarized by a 3-factor solution where mean responses consisted of Stimulation/Hedonia, Craving/Motivation and a general negative valence factor, and dose responses consisted of a general positive valence factor, Sedation/Motor Intoxication and Negative Affect.
| Ascending Limb Mean Response | |||||||
|
| |||||||
|
Light Drinkers
|
Heavy Drinkers
|
||||||
| Factor 1 | Factor 2 | Factor 3 | Factor 1 | Factor 2 | Factor 3 | Factor 4 | |
| BAES Stimulation | 0.70 | 0.27 | 0.09 | 0.83 | 0.09 | 0.05 | 0.11 |
| POMS Pos. Mood | 0.84 | −0.11 | 0.09 | 0.56 | 0.22 | 0.02 | − 0.52 |
| POMS Vigor | 0.93 | 0.03 | −0.13 | 0.95 | −0.08 | 0.02 | 0.02 |
| AUQ | −0.02 | 0.16 | 0.53 | 0.04 | −0.09 | 0.55 | 0.08 |
| Liking | 0.00 | 0.04 | 0.87 | −0.01 | 0.14 | 0.84 | 0.02 |
| Wanting | −0.05 | 0.02 | 0.82 | 0.02 | −0.10 | 0.79 | −0.07 |
| BAES Sedation | 0.14 | 0.83 | 0.09 | 0.02 | 0.93 | −0.03 | −0.04 |
| SHAS | −0.22 | 0.60 | −0.28 | −0.01 | 0.87 | 0.11 | 0.10 |
| POMS Tension | −0.30 | 0.58 | −0.20 | 0.12 | 0.02 | −0.01 | 0.93 |
| POMS Neg. Mood | 0.10 | 0.81 | 0.22 | −0.14 | 0.26 | −0.08 | 0.63 |
| Inter-factor Correlations |
Inter-factor Correlations |
||||||
| Factor 1 | Factor 2 | Factor 1 | Factor 2 | Factor 3 | |||
| Factor 2 | 0.15 | Factor 2 | 0.26 | ||||
| Factor 3 | 0.38 | 0.31 | Factor 3 | 0.39 | 0.36 | ||
| Factor 4 | −0.23 | 0.15 | −0.15 | ||||
| Ascending Limb Dose Re sponse | |||||||
|
| |||||||
|
Light Drinkers
|
Heavy Drinkers
|
||||||
| Factor 1 | Factor 2 | Factor 3 | Factor 1 | Factor 2 | Factor 3 | Factor 4 | |
| BAES Stimulation | 0.68 | 0.03 | 0.11 | 0.29 | 0.48 | 0.10 | 0.13 |
| POMS Pos. Mood | 0.55 | 0.07 | − 0.51 | 0.10 | 0.60 | 0.10 | 0.03 |
| POMS Vigor | 0.71 | −0.16 | −0.11 | −0.10 | 0.85 | −0.06 | −0.05 |
| AUQ | 0.56 | 0.10 | 0.14 | 0.03 | 0.02 | 0.70 | −0.08 |
| Liking | 0.63 | 0.22 | −0.04 | 0.29 | 0.17 | 0.42 | −0.03 |
| Wanting | 0.43 | 0.06 | −0.14 | −0.08 | −0.05 | 0.78 | 0.05 |
| BAES Sedation | −0.15 | 0.90 | −0.07 | 0.68 | −0.15 | −0.05 | −0.02 |
| SHAS | 0.28 | 0.79 | 0.10 | 0.89 | 0.03 | 0.01 | 0.00 |
| POMS Tension | 0.19 | −0.06 | 0.60 | 0.10 | −0.02 | −0.15 | 0.33 |
| POMS Neg. Mood | −0.27 | 0.20 | 0.48 | −0.01 | 0.00 | 0.00 | 1.00 |
| Inter-factor Correlations |
Inter-factor Correlations |
||||||
| Factor 1 | Factor 2 | Factor 1 | Factor 2 | Factor 3 | |||
| Factor 2 | 0.21 | Factor 2 | 0.09 | ||||
| Factor 3 | −0.30 | 0.07 | Factor 3 | 0.21 | 0.25 | ||
| Factor 4 | 0.03 | −0.12 | 0.0 0 | ||||
For light drinkers, a 3-factor solution was identified as the best solution for ascending limb mean response to alcohol (Table 4). These 3 factors explained 65% of the variance and each factor explained individually a substantial amount of variance (23%, 22%, and 20% respectively). In terms of mean response, Factors 1 and 3 were identical to the Stimulation/Hedonia and Craving/Motivation factors identified in the full sample. The second factor however, was indexed by the BAES Sedation, SHAS, POMS Tension and POMS Negative Mood, suggesting a general negative valence dimension.
Three factors were also suggested for ascending limb dose response in light drinkers (51% variance explained; Table 4). In terms of alcohol dose response, the second and third factors were analogous to the Sedation/Intoxication and Negative Affect dimensions identified in the full sample. However, the first factor was comprised of the BAES stimulation, POMS Positive Mood, POMS Vigor, AUQ, ‘Liking,’ and ‘Wanting’ suggesting a general positive valence response dimension.
Among light drinkers, descending limb factor structure was nearly identical to that observed for ascending limb mean response. Specifically, three factors were observed (63% of variance explained) with a general negative valence Factor 1 indexed by the BAES Sedation, SHAS, and the POMS Tension and Negative Mood subscales. Factor 2 was indicated by the BAES Stimulation, POMS Positive Mood and Vigor subscales, and negative loading of the POMS Negative Mood subscale. Lastly, the third factor was comprised of the AUQ, ‘Liking’ and ‘Wanting’ and negative loading of the POMS Tension subscale.
Discussion
The goal of this study was to promote consilience in alcohol challenge research through examination of the latent factor structure of SR as assessed using a battery of commonly used self-report measures and during a highly controlled intravenous alcohol challenge. In these analyses we were able to replicate a 3-factor structure of SR reported previously using the BAES, SHAS, and POMS measures (Ray et al., 2009) along the ascending limb at the level of both mean and dose response. This study also aimed to extend this multidimensional model by incorporating assessments of alcohol craving, ‘Liking’ and ‘Wanting’ in the conceptual framework of subjective response. Our results reveled that these three measures comprised a fourth Craving/Motivation factor. The inclusion of these additional items provides valuable insight into the structure of SR through incorporating craving and motivational salience, which are key constructs in alcoholism and addiction etiology (Addolorato et al., 2005; de Wit, 2000; Drummond et al., 2000; Robinson and Berridge, 1993, 2001). It should be noted that this study assessed alcohol-induced craving as opposed to unprovoked or cue-induced craving. Together these results suggest that SR is a multidimensional construct with four distinct domains representing Stimulation/Hedonia, Craving/Motivation, Sedation/Motor Intoxication, and Negative Affect. Furthermore, we were able to validate this four-factor structure on the descending limb of alcohol intoxication, thus providing much needed insight regarding the parallelism of SR structure on ascending versus descending limb. These results suggest that future alcohol challenge studies should assess these four domains of SR to ensure full coverage of alcohol’s subjective effects while reducing the number of redundant comparisons and perhaps increasing power to detect meaningful effects.
As a secondary aim, this study assessed the generalizability of this factor structure to different drinking groups. To achieve this goal, participants were dichotomized into light drinkers or heavy drinkers based on a threshold of 14 drinks (7 for women) per week (NIAAA, 1995). The 4-factor structure identified in the full sample was fully maintained in the subsample of heavy drinkers. In light drinkers however, a three-factor structure was observed. Specifically, in terms of ascending limb mean response and descending limb, sedation and negative affect loaded on a single negative valence factor, and in terms of dose-response stimulation and craving loaded on a single positive valence factor. Together these results suggest that heavy drinkers may experience greater dissociation in terms of subjective response, whereas light drinkers are more inclined to report global positive or negative responses to alcohol. Alternatively, tolerance and sensitization to the effects of alcohol may influence specific domains of alcohol response that would result in greater dissociation of SR constructs in heavy drinkers as compared to lighter drinkers. Further research is needed to validate and disentangle these potential effects.
While some of the results were direct replications of previous research by our group (Ray et al., 2009), alcohol ‘Liking’ was expected to load with stimulation and hedonic domains (Bice and Kiefer, 1990; Hobbs et al., 2005; Robinson and Berridge, 1993, 2001). In these data however, ‘Liking’ was found to load with the AUQ and ‘Wanting’ to a greater extent than stimulation and positive affect scales. In fact, alcohol ‘Liking’ was most highly correlated with ‘Wanting’ (mean response: r = 0.71; dose-response: r = 0.39, descending: r = 0.65). These results stand in opposition to the predictions of incentive sensitization theory which proposes that hedonic reward and motivational salience are both phenotypically and neurobiologically dissociable constructs, particularly in dependence (Robinson and Berridge, 1993, 2001). The high correlation between ‘Liking’ and ‘Wanting’ in these data may be influenced by the assessment procedure. This and many other similar alcohol challenge studies have assessed these two constructs with single items within a common measure, and thus proximal in time. As a result, it is possible that responses on the ‘Liking’ item may contaminate the assessment of ‘Wanting’ as subjects may recall their answer to their enjoyment of the alcohol dose when responding whether they would want more alcohol (Podsakoff and Organ, 1986; Salancik and Pfeffer, 1977). Studies that have utilized different assessment techniques for ‘Liking’ and ‘Wanting’ have demonstrated greater dissociation between these constructs (Hobbs et al., 2005).
Alternatively, the high correlation between ‘Liking’ and ‘Wanting’ in this sample may reflect the possibility that liking and wanting are still closely linked in many drinkers. ‘Liking’ is a fairly vague measure as it may reference both hedonic reward or alleviation of negative affect, and thus may simply be a global assessment of whether the subject had a net positive experience with the alcohol and thus would like to continue that experience, which would be expressed via wanting more alcohol. Conversely, the detailed assessment of Stimulation/Hedonia may capture in a more refined phenotype uniquely measuring a subset of positive and invigorating responses to alcohol. Recent work by our group has lent support to this idea that stimulation and hedonic assessments are sensitive to alcoholism-related differences in the association between hedonic reward and motivational salience as proposed by the incentive sensitization model of addiction (Bujarski and Ray, 2014).
Recent scale construction work has argued that the BAES and the SHAS, do not adequately assess all four affective quadrants affected by alcohol consumption (i.e. high/low arousal × positive/negative valence; Morean et al., 2012, 2013). Thus, Morean et al (2013) have developed the four-factor Subjective Effects of Alcohol Scale (SEAS), which expands SR measures by assessing high arousal negative (e.g. “demanding,” “rude,” and “aggressive”) and low arousal positive (e.g. “mellow,” “relaxed,” and “calm”) domains. While the SEAS measure was not included in this study, our inclusion of the POMS invites comparison to the SEAS. Specifically, while the direction is reversed, the tension subscale of the POMS contains identical items as the SEAS low arousal positive subscale (e.g. “calm,” and “relaxed”). Thus the tension subscale may be capturing a similar psychological construct as this SEAS subscale, though this proposition should be subjected to direct empirical investigation in future studies. However, while our data may have captured low arousal positive SR, no items in our data substantively overlapped with high arousal negative items.
This study and its findings should be interpreted in light of design strengths and limitations. Study strengths include the large sample size comprised of both light and heavy drinkers, the controlled alcohol administration methods, the reliance on multiple valid measures of subjective response to alcohol, and the analytic approach accounting for alcohol dosing, BrAC limb, and drinking pattern. Limitations include the moderate dose of alcohol, the lack of a saline or placebo control, and the lack of representation of more severe and chronic drinkers. As with all IV alcohol studies, this study sacrifices external validity for greater experimental control, and thus future research should validate the observed factor structure using more naturalistic designs (e.g. oral alcohol dosing). Lastly, while the timeframe of the alcohol administration was brief (~1.5hr) it is possible that acute sensitization and/or acute tolerance effects may have influenced the data and results.
In sum, this study extends alcohol challenge research by suggesting that SR is indeed a multifaceted construct, consistent with recent longitudinal work ascertaining its etiological contribution (King, de Wit, et al., 2011; King et al., 2014). Further, the observed distinction between light and heavy drinkers is consistent with the notion that alcohol exposure may alter the course of subjective response and this study suggest that heavy drinkers experience greater dissociation of SR dimensions as compared to light drinkers for whom alcohol’s effects may be more globally experienced as positive or negative. An important implication of this finding is that studies of SR in light drinkers may not translate effectively for heavy drinkers (and beyond) given that the structure of the core constructs differ. Future studies including more chronic alcohol users may reveal further structural differences in the SR constructs associated with level of alcohol use. Ultimately, longitudinal studies examining these constructs over the course of drinking trajectories at the individual level are needed to further our understanding of SR as a dynamic construct that may be sensitive to neuroadaptation resulting from chronic alcohol intake.
Acknowledgments
This work was supported by the National Institutes of Health (R01 AA015968) to KEH. SB was supported as a predoctoral trainee from the National Institutes of Alcohol Abuse and Alcoholism (F31 AA022569). LAR is a consultant for GSK. No other authors have any conflict of interest.
References
- Addolorato G, et al. Neurobiochemical and clinical aspects of craving in alcohol addiction: a review. Addictive behaviors. 2005;30(6):1209–1224. doi: 10.1016/j.addbeh.2004.12.011. [DOI] [PubMed] [Google Scholar]
- Bice PJ, Kiefer SW. Taste reactivity in alcohol preferring and nonpreferring rats. Alcoholism: Clinical and Experimental Research. 1990;14(5):721–727. doi: 10.1111/j.1530-0277.1990.tb01234.x. [DOI] [PubMed] [Google Scholar]
- Bliese P. multilevel: Multilevel Functions. R Package; 2008. [Google Scholar]
- Bohn MJ, et al. Development and Initial Validation of a Measure of Drinking Urges in Abstinent Alcoholics. Alcoholism: Clinical and Experimental Research. 1995;19(3):600–606. doi: 10.1111/j.1530-0277.1995.tb01554.x. [Online] [DOI] [PubMed] [Google Scholar]
- Bujarski S, Ray LA. [Accessed 19 May 2014];Subjective response to alcohol and associated craving in heavy drinkers vs. alcohol dependents: An examination of Koob’s allostatic model in humans. Drug and Alcohol Dependence. 2014 doi: 10.1016/j.drugalcdep.2014.04.015. [Online] [online]. Available from: http://www.sciencedirect.com/science/article/pii/S0376871614008412. [DOI] [PMC free article] [PubMed]
- Chutuape MAD, de Wit H. Relationship between subjective effects and drug preferences: ethanol and diazepam. Drug and Alcohol Dependence. 1994;34(3):243–251. doi: 10.1016/0376-8716(94)90163-5. [Online] [DOI] [PubMed] [Google Scholar]
- Corbin WR, et al. Stimulant alcohol effects prime within session drinking behavior. Psychopharmacology. 2008;197(2):327–337. doi: 10.1007/s00213-007-1039-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello AB, Osborne JW. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval 2005; 10. pareonline. net/getvn. asp. 2005;107 [Google Scholar]
- Drummond DC, et al. Craving research: future directions. Addiction. 2000;95(8s2):247–255. doi: 10.1080/09652140050111816. [Online] [DOI] [PubMed] [Google Scholar]
- Earleywine M. Confirming the factor structure of the anticipated biphasic alcohol effects scale. Alcoholism: Clinical and Experimental Research. 1994;18(4):861–866. doi: 10.1111/j.1530-0277.1994.tb00051.x. [DOI] [PubMed] [Google Scholar]
- Earleywine M, Martin CS. Anticipated stimulant and sedative effects of alcohol vary with dosage and limb of the blood alcohol curve. Alcoholism: Clinical and Experimental Research. 1993;17(1):135–139. doi: 10.1111/j.1530-0277.1993.tb00738.x. [DOI] [PubMed] [Google Scholar]
- Erblich J, Earleywine M. Distraction Does Not Impair Memory during Intoxication: Support for the Attention-Allocation Model. Journal of Studies on Alcohol and Drugs. 1995;56(4):444. doi: 10.15288/jsa.1995.56.444. [DOI] [PubMed] [Google Scholar]
- Everitt BS. Multivariate analysis: The need for data, and other problems. The British Journal of Psychiatry. 1975;126(3):237–240. doi: 10.1192/bjp.126.3.237. [DOI] [PubMed] [Google Scholar]
- Hobbs M, et al. Dissociation of wanting and liking for alcohol in humans: a test of the incentive-sensitisation theory. Psychopharmacology. 2005;178(4):493–499. doi: 10.1007/s00213-004-2026-0. [Online] [DOI] [PubMed] [Google Scholar]
- King AC, et al. Alcohol Challenge Responses Predict Future Alcohol Use Disorder Symptoms: A 6-Year Prospective Study. Biological Psychiatry. 2014;75(10):798–806. doi: 10.1016/j.biopsych.2013.08.001. [Online] [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AC, de Wit H, et al. Rewarding, Stimulant, and Sedative Alcohol Responses and Relationship to Future Binge Drinking. Arch Gen Psychiatry. 2011;68(4):389–399. doi: 10.1001/archgenpsychiatry.2011.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AC, Roche DJO, et al. Subjective Responses to Alcohol: A Paradigm Shift May Be Brewing. Alcoholism: Clinical and Experimental Research. 2011;35(10):1726–1728. doi: 10.1111/j.1530-0277.2011.01629.x. [Online] [DOI] [PubMed] [Google Scholar]
- Li T-K, et al. Genetic and Environmental Influences on Alcohol Metabolism in Humans. Alcoholism: Clinical and Experimental Research. 2001;25(1):136–144. [Online] [PubMed] [Google Scholar]
- MacKillop J. Factor Structure of the Alcohol Urge Questionnaire Under Neutral Conditions and During a Cue-elicited Urge State. Alcoholism: Clinical and Experimental Research. 2006;30(8):1315–1321. doi: 10.1111/j.1530-0277.2006.00159.x. [Online] [DOI] [PubMed] [Google Scholar]
- Martin CS, et al. Development and Validation of the Biphasic Alcohol Effects Scale. Alcoholism: Clinical and Experimental Research. 1993;17(1):140–146. doi: 10.1111/j.1530-0277.1993.tb00739.x. [Online] [DOI] [PubMed] [Google Scholar]
- McNair D, et al. [Accessed 13 December 2013];Two EITS Manual for the Profile of Mood States (1971 & 1992) 1971 [online]. Available from: http://ubir.buffalo.edu/xmlui/handle/10477/1893.
- Morean ME, et al. The Anticipated Effects of Alcohol Scale: Development and psychometric evaluation of a novel assessment tool for measuring alcohol expectancies. Psychological assessment. 2012;24(4):1008. doi: 10.1037/a0028982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morean ME, et al. [Accessed 3 September 2013];The Subjective Effects of Alcohol Scale: Development and Psychometric Evaluation of a Novel Assessment Tool for Measuring Subjective Response to Alcohol. Psychological Assessment. 2013 doi: 10.1037/a0032542. [Online] [online]. Available from: http://search.proquest.com/docview/1349393719?accountid=14512. [DOI] [PMC free article] [PubMed]
- Newlin DB, Renton RM. High risk groups often have higher levels of alcohol response than low risk: the other side of the coin. Alcoholism: Clinical and Experimental Research. 2010;34(2):199–202. doi: 10.1111/j.1530-0277.2009.01081.x. [DOI] [PubMed] [Google Scholar]
- Newlin DB, Thomson JB. Alcohol challenge with sons of alcoholics: A critical review and analysis. Psychological Bulletin. 1990;108(3):383–402. doi: 10.1037/0033-2909.108.3.383. [Online] [DOI] [PubMed] [Google Scholar]
- NIAAA . The physicians’ guide to helping patients with alcohol problems. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism; 1995. (US) [Google Scholar]
- Podsakoff PM, Organ DW. Self-Reports in Organizational Research: Problems and Prospects. Journal of Management. 1986;12(4):531–544. [Online] [Google Scholar]
- Quinn PD, Fromme K. Subjective Response to Alcohol Challenge: A Quantitative Review. Alcoholism: Clinical and Experimental Research. 2011;35(10):1759–1770. doi: 10.1111/j.1530-0277.2011.01521.x. [Online] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd edition SAGE Publications, Inc.; Thousand Oaks: 2001. [Google Scholar]
- Ray LA, et al. Catching the Alcohol Buzz: An Examination of the Latent Factor Structure of Subjective Intoxication. Alcoholism: Clinical and Experimental Research. 2009;33(12):2154–2161. doi: 10.1111/j.1530-0277.2009.01053.x. [Online] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray LA, et al. Pharmacogenetics of Naltrexone in Asian Americans: A Randomized Placebo-Controlled Laboratory Study. Neuropsychopharmacology. 2012;37(2):445–455. doi: 10.1038/npp.2011.192. [Online] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray LA, et al. Subjective Responses to Alcohol Consumption as Endophenotypes: Advancing Behavioral Genetics in Etiological and Treatment Models of Alcoholism. Substance Use & Misuse. 2010;45(11):1742–1765. doi: 10.3109/10826084.2010.482427. [Online] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray LA, et al. Subjective Response to Alcohol Among Alcohol-Dependent Individuals: Effects of the Mu-Opioid Receptor (OPRM1) Gene and Alcoholism Severity. Alcoholism: Clinical and Experimental Research. 2013:37E116–E124. doi: 10.1111/j.1530-0277.2012.01916.x. [Online] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray LA, Hutchison KE. A Polymorphism of the μ-Opioid Receptor Gene (OPRM1) and Sensitivity to the Effects of Alcohol in Humans. Alcoholism: Clinical and Experimental Research. 2004;28(12):1789–1795. doi: 10.1097/01.alc.0000148114.34000.b9. [Online] [DOI] [PubMed] [Google Scholar]
- Revelle W. [Accessed 21 August 2014];psych: Procedures for Psychological, Psychometric, and Personality Research. 2014 [online]. Available from: http://cran.r-project.org/web/packages/psych/index.html.
- Robinson TE, Berridge KC. Incentive-sensitization and addiction. Addiction. 2001;96(1):103–114. doi: 10.1046/j.1360-0443.2001.9611038.x. [Online] [DOI] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain research reviews. 1993;18(3):247–291. doi: 10.1016/0165-0173(93)90013-p. [DOI] [PubMed] [Google Scholar]
- Roche DJ, et al. Acute alcohol response phenotype in heavy social drinkers is robust and reproducible. Alcoholism: Clinical and Experimental Research. 2014;38(3):844–852. doi: 10.1111/acer.12280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rueger SY, et al. Expanding the Utility of the Biphasic Alcohol Effects Scale (BAES) and Initial Psychometric Support for the Brief-BAES (B-BAES) Alcoholism: Clinical and Experimental Research. 2009;33(5):916–924. doi: 10.1111/j.1530-0277.2009.00914.x. [Online] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salancik GR, Pfeffer J. An examination of need-satisfaction models of job attitudes. Administrative Science Quarterly. 1977:427–456. [PubMed] [Google Scholar]
- Schuckit MA. Comment on the paper by Quinn and Fromme entitled subjective response to alcohol challenge: a quantitative review. Alcoholism: Clinical and Experimental Research. 2011;35(10):1723–1725. doi: 10.1111/j.1530-0277.2011.01561.x. [DOI] [PubMed] [Google Scholar]
- Schuckit MA. EThanol-induced changes in body sway in men at high alcoholism risk. Archives of General Psychiatry. 1985;42(4):375–379. doi: 10.1001/archpsyc.1985.01790270065007. [Online] [DOI] [PubMed] [Google Scholar]
- Schuckit MA. Subjective responses to alcohol in sons of alcoholics and control subjects. Archives of general psychiatry. 1984;41(9):879–884. doi: 10.1001/archpsyc.1984.01790200061008. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, et al. The search for genes contributing to the low level of response to alcohol: patterns of findings across studies. Alcoholism: Clinical and experimental research. 2004;28(10):1449–1458. doi: 10.1097/01.alc.0000141637.01925.f6. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Gold EO. A simultaneous evaluation of multiple markers of ethanol/placebo challenges in sons of alcoholics and controls. Archives of General Psychiatry. 1988;45(3):211–216. doi: 10.1001/archpsyc.1988.01800270019002. [Online] [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Smith TL. An 8-year follow-up of 450 sons of alcoholic and control subjects. Archives of general psychiatry. 1996;53(3):202–210. doi: 10.1001/archpsyc.1996.01830030020005. [DOI] [PubMed] [Google Scholar]
- Sobell LC, et al. Reliability of a timeline method: assessing normal drinkers’ reports of recent drinking and a comparative evaluation across several populations. British journal of addiction. 1988;83(4):393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. [Accessed 21 August 2014];Using multivariate statistics. 2001 [online]. Available from: http://www.ulb.tu-darmstadt.de/tocs/135813948.pdf.
- Velicer WF, Jackson DN. Component analysis versus common factor analysis: Some issues in selecting an appropriate procedure. Multivariate behavioral research. 1990;25(1):1–28. doi: 10.1207/s15327906mbr2501_1. [DOI] [PubMed] [Google Scholar]
- De Wit H, et al. Assessing individual differences in ethanol preference using a cumulative dosing procedure. Psychopharmacology. 1989;98(1):113–119. doi: 10.1007/BF00442016. [DOI] [PubMed] [Google Scholar]
- De Wit H. Laboratory-based assessment of alcohol craving in social drinkers. Addiction. 2000;95(8s2):165–169. doi: 10.1080/09652140050111735. [Online] [DOI] [PubMed] [Google Scholar]
- De Wit H, Doty P. Preference for ethanol and diazepam in light and moderate social drinkers: a within-subjects study. Psychopharmacology. 1994;115(4):529–538. doi: 10.1007/BF02245577. [Online] [DOI] [PubMed] [Google Scholar]