Abstract
Background: A respiratory severity score (RSS) describing acute respiratory illness (ARI) severity would be useful for research and clinical purposes.
Methods: A total of 630 term infants presenting with ARI had their RSS measured.
Results: RSS was higher in those with lower respiratory tract infection (LRTI) compared with those with upper respiratory infection (URI; LRTI 6.5 [4–8.5]; URI 1 [0–2], p<0.001) and in hospitalized infants compared with outpatients (hospitalized 6.5 [4–9]; outpatient 1 [0–3], p<0.001).
Conclusions: RSS is higher in LRTI compared with URI and in hospitalized compared with nonhospitalized infants.
Introduction
Acute respiratory illness (ARI), comprising upper (URI) and lower respiratory tract infections (LRTI), is the most common infectious disease in infants that requires acute care visits and hospitalization.1 Infant respiratory syncytial virus (RSV) LRTI and rhinovirus (RV) LRTI are also strongly associated with asthma inception.2–8
Because of the impact of ARI on infant and child respiratory health, having an ordinal scale of disease severity across the spectrum of ARI would be highly useful for both research and clinical purposes. Several severity scores exist for bronchiolitis, among which a system proposed by Tal et al.9–11 has been the most widely used, and has been shown to be internally consistent and have good interrater reliability.11 However, the modified Tal score or other bronchiolitis severity scores (BSS) have not been applied across the entire spectrum of ARI (i.e., to describe both URI and LRTI severity), and have not been used to predict measures of ARI severity, such as need for inpatient care. The present study hypothesized that the modified Tal BSS associates infants by diagnosis (LRTI vs. URI) as well as by level of care (inpatient vs. outpatient). Because this severity scoring system is being applied to all ARIs, it is termed a “respiratory severity score” (RSS).
Materials and Methods
A total of 630 previously healthy, term infants were studied with ARI due to LRTI or URI who were enrolled during the 2004–2008 viral respiratory seasons in a prospective longitudinal cohort study, the Tennessee Children's Respiratory Initiative (TCRI).12
Eligible infants with ARI were approached for enrollment from the pediatric acute care clinic, the pediatric emergency department, or the inpatient ward of the Vanderbilt Children's Hospital. ARI was defined as at least one of three major symptoms (wheeze, retractions, and/or dyspnea) and at least two minor symptoms (fever, rhinorrhea, cough, otitis media, hoarse cry, vomiting after cough, and/or RSV testing ordered by the treating clinician). LRTI versus URI was based on the clinical diagnosis of the treating clinicians, or if a clear diagnosis was not available, this was assigned by a panel of pediatricians who reviewed the chart. Hospitalized infants were oversampled, and therefore account for a larger percentage of the cohort. The study was approved by the Vanderbilt Institutional Review Board, and parents provided written informed consent for study participation.
RSS was determined for each infant, and is a composite score ranging from 0 to 12, with a higher score indicating more severe disease, with 0–3 points each assigned to respiratory rate, flaring/retractions, room air oxygen saturation, and wheezing (Supplementary Table S1; Supplementary Data are available online at www.liebertpub.com/ped). RSS was determined by chart extraction; when there was more than one set of vitals (e.g., among inpatients), the most severe values from the first 24 h of care were used. For outpatient care, where oxygen saturation was not available, it was imputed to >95%. If wheezing severity could not be determined from the chart but was noted to be present, 1.5 points were assigned (this was the case for only 16% of infants).
Two nasal and throat swabs were obtained from infants at enrollment during the acute illness. These specimens were tested for RSV A and B, RV, adenovirus, human metapneumovirus, coronaviruses, influenza A and B, and parainfluenza types 1, 2, and 3, using quantitative reverse transcriptase polymerase chain reaction assays.
Statistical analysis
Demographic features of the cohort and viral etiology of ARI were presented as frequency and proportion, median and interquartile range (IQR), or mean and standard deviation (SD) as appropriate, and were compared by URI versus LRTI using Wilcoxon's rank sum test for continuous measures and the chi square test for proportions. The main independent variable was RSS. Dependent variables were URI versus LRTI, inpatient versus outpatient care, and among inpatients, maximum location of care (inpatient, intensive care unit (ICU), ICU and receiving positive pressure ventilation). To assess the adjusted association of RSS with ARI diagnosis (LRTI vs. URI) and level of care (inpatient vs. outpatient), separate multivariable logistic regression models were used, including a priori selected covariates (infant age, sex, weight, gestational age, maternal current smoking, mother's race, presence of siblings and insurance status). Infant age and RSS score were included as flexible nonlinear terms. Statistical analysis was performed using R v3.1.0 (www.R-project.org).
Results
The demographics of the 630 infants with ARI (LRTI or URI) are summarized in Supplementary Table S2. Of these, 72% were diagnosed with LRTI and 28% with URI. Median infant age at presentation was lower in the LRTI group compared with the URI group (11 [6–21] weeks vs. 23 [9.5–39] weeks; p<0.001). There was a higher percentage of males in both the LRTI (56%) and URI (57%) groups. Infants with LRTI were more likely to have an older sibling at home (82% in the LRTI group; 58% in the URI group). Self-reported maternal smoking was approximately the same in both groups.
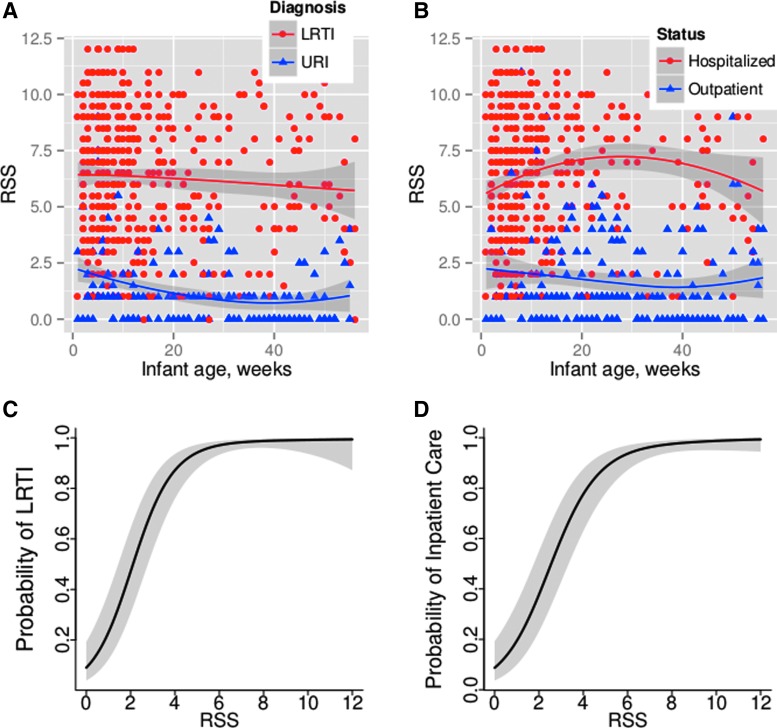
More infants diagnosed with LRTI were RSV positive (76% with LRTI vs. 14% with URI; p<0.001). Conversely, more infants with the diagnosis of URI were RV positive (18% with LRTI vs. 46% with URI; p<0.001). Of note, these values include co-infections. A majority of patients who received outpatient care only was diagnosed with URI, and a majority of those who received inpatient care was diagnosed with LRTI (82% outpatient only care and 18% inpatient care among those with URI vs. 14% outpatient only care and 86% inpatient care among those with LRTI; p<0.001). There were no patients diagnosed with URI who required treatment in the ICU. Infants with LRTI had a higher RSS than those with URI (LRTI 6.5 [4, 8.5] vs. URI 1 [0, 2], p<0.001; Fig. 1A). The results were similar when restricting the analysis to inpatients only who had all data elements available (data not shown). RSS was also higher in infants who were hospitalized than in infants who received outpatient care only (hospitalized 6.5 [4, 9] vs. outpatient 1 [0, 3], p<0.001; Fig. 1B). RSS was higher in the subset of inpatients that required ICU care (9 [7.5, 12], p<0.001). Predicted probability of LRTI diagnosis was positively associated with RSS (Fig. 1C), and similarly predicted probability of hospitalization increased with increasing RSS (Fig. 1D). In this cohort, having an RSS of ≥5 was associated with a 90% probability of having an LRTI versus a URI and of being managed inpatient versus outpatient (Fig. 1C and D).
FIG. 1.
Respiratory severity scale (RSS) separates individual infants with lower respiratory tract infection (LRTI; red dots) from those with upper respiratory tract infection (URI; blue dots) (A), and separates infants who required inpatient care (red dots) from those managed as outpatients (blue dots) (B). (C) and (D) Separate multivariable logistic regressions were used to assess the relationship of RSS with URI diagnosis (C) and RSS with inpatient care (D), adjusting for infant age at time of acute respiratory illness (ARI), sex, birth weight, gestational age, insurance status, presence of siblings, maternal tobacco current use, and race. The RSS was included as a flexible smooth parameter using splines. The predicted probability of LRTI versus URI diagnosis (C) or of inpatient versus outpatient care (D) increases as RSS increases.
Discussion
This study has shown that when the previously validated modified Tal severity score for bronchiolitis is applied across the spectrum of ARI (those with URI as well as those with LRTI), it can be a useful tool for distinguishing LRTI from URI and for measuring the severity of disease. Using RSS in this manner could be a helpful tool for investigations of early life ARI, to improve accuracy of diagnosis (LRTI vs. URI), and to provide an objective quantitative variable about disease severity for both research and clinical purposes.
In addition to being a major source of morbidity among infants, ARI is also important due to its impact on childhood asthma. Previous studies have shown that both RSV LRTI and RV LRTI are strongly associated with asthma risk,2–7 and that increasingly severe LRTI is associated with increased odds of childhood asthma.8 Using a score that captures the degree of severity would allow assessment of the heterogeneity of ARI's relationship with asthma risk and the assessment of a severity–response relationship.
In addition to utility as a research tool, RSS would benefit from further study regarding possible clinical utility for providers treating infants with ARI. It was found that RSS differentiates LRTI from URI and the level of care required (outpatient, inpatient, ICU). Among other topics, future investigations could look at ability of low RSS to predict successful outpatient management, and ability of high RSS to predict infants in need of early aggressive inpatient care.
There are several limitations to this study. First, as noted, unavailable data elements were imputed; this was primarily an issue with O2 saturation among outpatients. However, a sensitivity analysis limiting to inpatients only yielded similar results, and because there were relatively few infants with URI among inpatients, the full cohort was included in the analysis. Second, this study was performed at a single academic medical center that represented the only children's hospital in its city, and so RSS ranges predictive of inpatient versus outpatient care and level of care among inpatients are likely higher than they would be at hospitals with less experience managing infant ARI. RSS ranges (e.g., level above which nearly all infants receive inpatient care) are likely to be institution specific and reflective of the comfort level of treating clinicians with ARI management. Additionally, such a scoring tool should not be the exclusive decision maker regarding need for inpatient care, which may be impacted by other factors such as availability of appropriate follow-up care, among other sociodemographic factors.
However, this study has shown that adapting a previously validated BSS into a RSS applicable to the spectrum of infants with ARI separates infants with URI versus LRTI, and separates both the need for inpatient versus outpatient care, and level of care for those managed as inpatients. RSS appears to be a useful research tool for moving from a dichotomized categorization of disease severity and clinical features of ARI to a continuous ordinal scale, which allows for more meaningful assessment of disease severity over a continuum, assessment of a severity-dependent relationship, and may have application to clinical decision making for infant ARI.
Supplementary Material
Acknowledgments
T.V.H. received support from Thrasher Research Fund; NIH K24 AI 077930; NIH UL1 RR024975; NIH AI 095227.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Yorita KL, Holman RC, Sejvar JJ, Steiner CA, Schonberger LB. Infectious disease hospitalizations among infants in the United States. Pediatrics 2008;121:244–252 [DOI] [PubMed] [Google Scholar]
- 2.Sigurs N, Bjarnason R, Sigurbergsson F, Kjellman B. Respiratory syncytial virus bronchiolitis in infancy is an important risk factor for asthma and allergy at age 7. Am J Respir Crit Care Med 2000;161:1501–1507 [DOI] [PubMed] [Google Scholar]
- 3.Jackson DJ, Evans MD, Gangnon RE, et al. . Evidence for a causal relationship between allergic sensitization and rhinovirus wheezing in early life. Am J Respir Crit Care Med 2012;185:281–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kotaniemi-Syrjanen A, Vainionpaa R, Reijonen TM, Waris M, Korhonen K, Korppi M. Rhinovirus-induced wheezing in infancy—the first sign of childhood asthma? J Allergy Clin Immunol 2003;111:66–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kusel MM, de Klerk NH, Kebadze T, et al. . Early-life respiratory viral infections, atopic sensitization, and risk of subsequent development of persistent asthma. J Allergy Clin Immunol 2007;119:1105–1110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee WM, Lemanske RF, Jr, Evans MD, et al. . Human rhinovirus species and season of infection determine illness severity. Am J Respir Crit Care Med 2012;186:886–891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lemanske RF, Jr, Jackson DJ, Gangnon RE, et al. . Rhinovirus illnesses during infancy predict subsequent childhood wheezing. J Allergy Clin Immunol 2005;116:571–577 [DOI] [PubMed] [Google Scholar]
- 8.Carroll KN, Wu P, Gebretsadik T, et al. . The severity-dependent relationship of infant bronchiolitis on the risk and morbidity of early childhood asthma. J Allergy Clin Immunol 2009;123:1055–1061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tal A, Bavilski C, Yohai D, Bearman JE, Gorodischer R, Moses SW. Dexamethasone and salbutamol in the treatment of acute wheezing in infants. Pediatrics 1983;71:13–18 [PubMed] [Google Scholar]
- 10.Goebel J, Estrada B, Quinonez J, Nagji N, Sanford D, Boerth RC. Prednisolone plus albuterol versus albuterol alone in mild to moderate bronchiolitis. Clin Pediatr (Phila) 2000;39:213–220 [DOI] [PubMed] [Google Scholar]
- 11.McCallum GB, Morris PS, Wilson CC, et al. . Severity scoring systems: are they internally valid, reliable and predictive of oxygen use in children with acute bronchiolitis? Pediatr Pulmonol 2013;48:797–803 [DOI] [PubMed] [Google Scholar]
- 12.Hartert TV, Carroll K, Gebretsadik T, Woodward K, Minton P. The Tennessee Children's Respiratory Initiative: objectives, design and recruitment results of a prospective cohort study investigating infant viral respiratory illness and the development of asthma and allergic diseases. Respirology 2010;15:691–699 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.