Abstract
Context
With 25% of pre-school age children in the United States being overweight or obese, effective interventions for these children would have significant public health implications. Randomized trials targeting this age group have been done since the last systematic review.
Objective
To systematically review the literature on treatment interventions for overweight or obesity in pre-school age children.
Data Sources
Medline (1948–July 2014), the Cochrane Central Registry (1991–July 2014), CINAHL (1990–July2014) and PAS abstracts (2000–2014).
Study Selection
Inclusion criteria were children age 0–6 in the study and adiposity as an outcome. Exclusions were having normal weight children in the trial and not having a comparison group.
Data Extraction
Data were extracted independently by two authors using a template.
Results
The initial search yielded 1,981 results, narrowed to 289 abstracts after initial review. Further analysis and cross-referencing led to the selection of six randomized controlled trials representing 1222 children. Two studies used systems changes and motivational interviewing and showed no significant effect on adiposity. Two studies used an intensive, multi-disciplinary approach over six months and demonstrated significant decreases in adiposity. One study tested parental coaching and showed a significant reduction in adiposity at six months. One study used education on a dairy-rich diet and showed a possible effect on adiposity.
Limitations
The study designs were too heterogeneous for meta-analysis; few ethnic minority subjects were included.
Conclusions
Multi-disciplinary, intensive interventions have some evidence of efficacy in reducing adiposity in pre-school children.
Keywords: Obesity, Overweight, Body mass index, Child, Preschool, Health promotion, Health behavior
Introduction
Despite somewhat stabilized childhood obesity rates in the United States, 30% of children remain overweight or obese, with racial and ethnic minorities at higher risk.1 These trends are evident even in the youngest children with one out of ten children under the age of 6 being obese.1 Although the 2–5 year old age group experienced a slight decline in overweight prevalence (5.5%) from 2003–2004 and 2011–2012, all other age groups including 0–2 year olds have shown no significant decreases.
Data show that early childhood weight status tracks into adolescence and adulthood,2,3 suggesting that successful earlier intervention and prevention may potentially be more clinically effective and cost-effective. Positive health behaviors developed early in life can also track into adolescence and adulthood. Understanding what interventions are effective among overweight and obese children aged six and under is critical to preventing overweight in later years and the subsequent associated complications.
Synthesizing and assessing the research in childhood obesity interventions among children aged six and under would provide critical direction for future programs and policies. However, recent systematic reviews of interventions in childhood obesity have focused on school-age and adolescent children.4–6 Reviews of treatment interventions among younger children have included both normal and overweight children reducing the ability to identify effectiveness of treatment interventions exclusively as opposed to primary prevention7 or were completed prior to more recent clinical trials targeting this age group.8,9
In this systematic review, we attempted to address the question: In children age 0–6 years of age who are overweight or obese, what behavioral or clinical interventions have been shown to be effective in reducing adiposity using a clinical trial design? In asking this question, we aimed to characterize commonalities to success so as to best inform this rapidly developing area of research. Innovative aspects of this review include a focus on treatment interventions for overweight and obese children and an examination of intervention effectiveness among children six years and younger, a critical population for clinical and cost-effective interventions.
Methods
Review protocol
A detailed protocol was developed and is available by request from the corresponding author. A priori inclusion criteria were studies that enrolled children age 0–6, included a measure of adiposity as an outcome, and had a specific strategy for addressing children age 0–6 if other ages were included. Inclusion of normal weight children was an exclusion criteria as we chose to focus on intervention rather than primary prevention. We used three accepted definitions for overweight or obesity to evaluate this exclusion criterion: the Centers for Disease Control and Prevention10, the World Health Organization11, or the International Obesity Task Force.12 A search of Medline (1946–July 2014), the Cochrane Central Registry (1991–July 2014), CINAHL (1990–July2014) and PAS abstracts (2000–2014) was completed in July 2014. For the search of Medline, terms used in the search were ‘obesity,’ ‘overweight,’ combined with ‘OR,’ then the filters of children (age 0–18 years) and clinical trial applied to the results. Results from the initial search were cross-referenced and liberally screened by title and abstract to ensure the study focused on children and overweight or obesity. Any lack of clarity on the study’s inclusion criteria or outcomes at this point led to a full-text review. For the second round, abstracts and, as necessary, full articles were screened using the inclusion and exclusion criteria by two authors independently (BF, PP). A hand search of the reference lists of all selected full text articles was done by two authors independently (BF, PP). Only clinical trials, no observational studies, were included in this review.
Primary outcome
The primary outcome measure was a measure of adiposity in participants (children) using the longest available time point post intervention start; no minimum follow-up was a priori set. Acceptable outcome measures for adiposity a priori included body mass index (BMI), body mass index percentile (BMI%) or some iteration of percent overweight or obese using both height and weight, and waist circumference.
Secondary outcomes
We collected secondary outcome data on any measure of behavioral change, measures of nutritional intake, activity or feeding patterns in order to help elucidate potential mechanisms.
Data collection
Data were collected using a standardized form that was piloted between two authors (BF, JF). The pilot process involved both authors extracting data from previously identified obesity intervention manuscripts and cross-comparing extracted data on intervention and outcomes; the only data process changed was including multiple measures of adiposity within a study. The data were extracted independently by two authors (BF, JF). Authors of primary studies were contacted as needed for clarification of results. For each study, we extracted data on the study date and duration; number, demographics and age of participants enrolled and completed in each group; intervention methods; setting; exclusion criteria; the primary and secondary outcomes defined by this review and when data were collected.
Heterogeneity and bias assessment
For methodological heterogeneity, we used a qualitative approach with two authors (BF, ES) examining the studies for similarities in intervention, comparison and population. We planned to use the I2 statistic to test for statistical heterogeneity if there was sufficient methodologic similarity to combine studies in a meta-analysis.
Using the criteria proposed by the Cochrane group, random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, and selective reporting were assessed.13 These were graded for each individual study as low, high or unclear risk of bias by two authors (BF, PP) independently. If an article had a high risk of bias, it was discussed for inclusion status. To assess bias across studies, we planned to use a funnel plot and assess for asymmetry.
Results
Search results
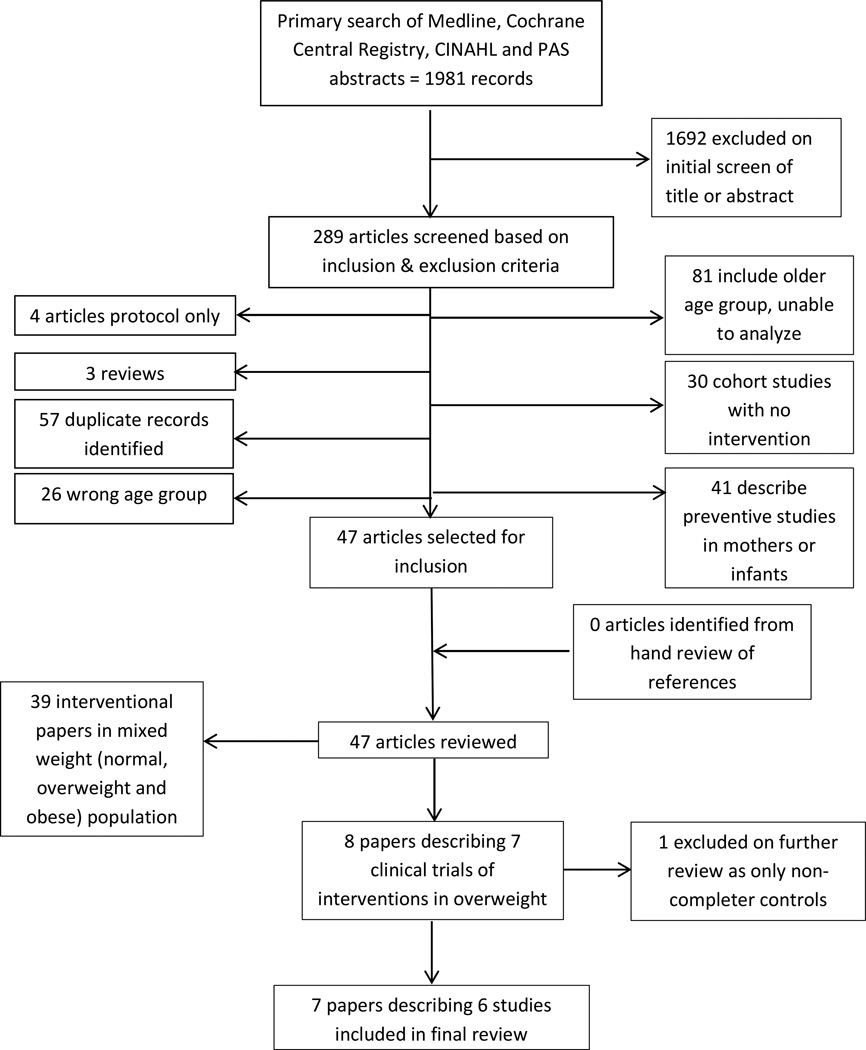
The initial search yielded 1,981 results which were narrowed down to 289 abstracts after initial review of title and abstract for inclusion criteria (done by BF, JF, PP) (Figure 1). Further analysis of full articles and cross-referencing led to the selection of the six studies included in this review (BF, JF); any conflicts were resolved via discussion. Of the 289, 81 were excluded due to inability to analyze the 0–6 year old age group independently of other age groups. For example, most studies only included five year olds on the lower age range with very few actually enrolled, e.g. 5–11 year olds. Additionally, 37 studies were excluded because they included normal weight children in the intervention and were thus deemed preventive in nature for this analysis. Recent systematic reviews and the included articles were analyzed and cross-referenced for additional studies. Our final analysis revealed seven papers representing six studies (Table 1) representing 1222 children enrolled in the studies.14–19 For the two papers reporting on one study, we used the initial publication15 as the main reference for analysis since the second publication reporting follow-up data did not present data by treatment group.20
Figure 1.
Flow Chart Showing the Results of the Search Process
Tble 1.
Summary of included studies’ design and context for all randomized controlled trials (n=6)
| Study ID | Age range |
Inclusion criteria |
Intervention condition (provider, n of sessions) |
Time intensity | Control condition (provider, n of sessions) |
Sample size |
|---|---|---|---|---|---|---|
| Bocca 2012, Netherlands14 | 3–5 years | Overweight or obese children with BMI-z score >1.1 | Diet advice (dietician, 6), physical activity sessions (physiotherapist, 12), group behavioral counseling sessions (psychologist, 6) | 27 hours over 4 months | Healthy eating behaviors, encouraged activity (pediatrician, 3) | 32 IC, 25 CC |
| Kelishadi 2009, Iran18 | 5.6 ± 0.5 years | BMI ≥ age or sex-specific 95th% | Healthy lifestyle education plus diet information (pediatrician, dietician, 6); DR group: >800mg Ca/day; ER group: restricted calories | 6 monthly sessions for IC and CC (unclear time/session) | Healthy lifestyle education (pediatrician, dietician); no specific diet advice | 36 DR, 31 ER, 32 CC |
| Quattrin 2012, USA19 | 2–5 years | BMI ≥85th% for age and gender AND 1 parent with BMI ≥27 | Diet, physical, and sedentary activities education with phone-based coaching between meetings (PEAs, 10) | 10 hours over 6 months in person, 8 phone calls | Same educational sessions without in-person coach after meetings | 46 IC, 50 CC |
| Stark 2011, USA15 | 2–5 years | ≥95th% BMI, not more than 100% above the mean BMI and a parent with a BMI ≥25 | Diet, physical activity, and behavioral management; mixed group and individual sessions (psychologist, 18). 12 week supply of vegetables provided | 27 hours over 6 months in clinic and in home | Healthy diet, physical activity, decrease screen time (pediatrician, 1); brochure given | 8 IC, 10 CC |
| Taveras 2011, USA16 | 2–6.9 years | BMI ≥95th% or >85th% and 1 parent overweight | Motivational interviewing and education focused on: TV, sugar sweetened beverages and fast food (PNP, 4); also enhanced EMR | 4 clinic visits (25 min each), 4 phone calls (15 min each) over 1 year | Standard of care in the practice (pediatrician) | 253 IC, 192 CC |
| van Grieken 2013, Netherlands17 | 5 years | Overweight but not obese children | Motivational interviewing on 1) playing outdoors 2) eating breakfast 3) reducing sweet drinks 4) watching TV, computer gaming (physician-nurse team, 4) | 4 visits in clinic over 1 year (unclear time per visit) | General information on a healthy lifestyle during the well-child visit (physician-nurse team) | 277 IC, 230 CC |
BMI = body mass index, DR = Dairy Rich, ER = Energy Restricted, IC = intervention condition, CC = control condition, PEA = practice enhancement assistant: person embedded in practice with a Master or Bachelor degree in psychology, nutrition, or exercise science, PNP = pediatric nurse practitioner, EMR = electronic medical record
Study designs and setting
The six studies all randomized participants to a control or intervention condition that ran simultaneously; basic design characteristics are presented in Table 1. All studies used exclusion criteria of having a chronic medical condition or not obtaining clearance from their pediatrician to participate. Of the three studies conducted in the United States, one enrolled a significant number of non-white participants (43.3% of the subjects);16 with the others targeting a largely white population (83% in both studies).15,19 Similarly, 8–11% of participants in the latter two studies15,19 were from “low income” families, defined as <$20,00019 or <$50,00015, while in the former study16 that figure was 29%, defined as <$50,000.16 Two non-U.S. studies did not provide demographics;14,18 one Dutch study enrolled mostly children of mid-high to highly educated mothers (66.7%) and primarily native Dutch (83.1%).17
Control conditions
All the studies randomized subjects to a control condition that ranged from usual care with their current provider16 up to 10 × 60-minute educational sessions with a separate provider with special training in providing education (Table 1).19
Interventions and outcomes
There was a wide range of content and intensity of the interventions across studies. The adiposity outcomes, the primary focus of this review, were measured at the end of the intervention period using the baseline assessment as comparison. Four of the six studies also included an additional post-intervention follow-up time point.14,15,17,18 Given the heterogeneity in both design and especially in the intervention, we did not conduct a meta-analysis of the outcome data. Instead, we provide a qualitative synthesis of the papers grouped by design similarities. As outlined in detail below, two studies attempted to leverage existing clinic resources and randomized by clinic or clinician, two studies had intensive, multi-disciplinary interventions, one study evaluated the effect of personalized coaching versus education, and one study evaluated different dietary education prescriptions.
Two studies used an approach building on current capacity using the current clinical context and providers to implement most of the intervention.16,17 Taveras et al16 was a cluster-randomized trial with individual practices assigned to intervention or control. Intervention practices received updates to their electronic medical record, staff training, health promotion in waiting rooms, educational handouts and resource lists for patients. Motivational interviewing around obesity related health behaviors was delivered by trained pediatric nurse practitioners, with four in-person visits designed to occur over the first year; notably only about half (56%) of the participants had two or more interactions (including phone calls). They did not find a significant difference in change in BMI at one year between intervention and control participants (Table 2); a post-hoc analysis showed significant effects on BMI in females (p=0.03), and those in households with incomes less than $50,000 (p=0.01). van Grieken et al17 randomized by clinical team (n=44 physician-nurse teams, 72% pediatricians) within clinic sites (n=9). All clinical sites and therefore teams received some systems-based intervention to improve identification and tracking of weight status. Intervention teams received motivational interviewing training and could provide up to four total visits over the first year of the program; 76.7% of participants received two visits, and 30.6% received all four visits. They did not show significant decreases in overall BMI between groups (Table 2); they did demonstrate a difference for only mildly overweight individuals in their sub-analysis (p=0.05).
Table 2.
Summary of outcomes across included studies using the longest time point for each study
| Study ID | Primary outcomes |
Time point |
Outcome at end of study | Secondary outcomes (diet and activity assessments) |
||
|---|---|---|---|---|---|---|
| Intervention condition |
Control condition | Difference between conditions |
||||
| Bocca 2012, Netherlands14 | BMI | 12 months | −1.0 kg/m2 95% CI: −1.52, −0.47 | 0.0 kg/m2 95% CI: −0.67, 0.62 | p=0.03 | No difference in activity (steps per day) at 12 months, p=0.39; no difference in energy intake (calories) at 12 months, p=0.87 |
| WC z-score | 12 months | −0.4 95% CI: −0.57, −0.14 | −0.3 95% CI: −0.61, −0.01 | p=0.01 | ||
| BMI z-score | 12 months | −0.6 95% CI: 0.82, −0.44 | −0.3 95% CI: −0.49, −0.05 | p=0.02 | ||
| Kelishadi 2009, Iran18 | BMI z-score | 36 months | Change from baseline, mean (SD): DR −0.1 (0.004) | ER: 0.7 (0.01); control: 0.6 (0.02) | p=0.001 | Mean energy intake lower in ER group at 6 months, no difference at 36 months; energy expenditure reported as NS difference at all time points |
| WC | Change from baseline, mean (SD): DR 4.1 (0.3) | ER: 4.8 (0.2); control: 5.2 (0.4) | p=0.04 | |||
| Quattrin 2012, USA19 | Percent over median BMI | 6 months | From 30.6% ± 9.7, to 24.2% ± 10.1 | From 30.5% ± 9.3 to 28.3% ± 9.5 | p<0.0021 | None reported |
| Stark 2011, USA15 | BMI z-score | 12 months | Change from baseline, mean (SD): −0.37 (0.41) | Change from baseline, mean (SD): 0.40 (0.49) | −0.77, 95% CI: −1.26, −0.27 | Difference at 12 months for calorie intake (kcal): −525, 95% CI: −811, −240. Average of 20min vigorous activity, 59–75min moderate activity/day across time points, NS between groups. |
| Taveras 2011, USA16 | BMI | 12 months | From baseline, mean (SE): 0.31 (0.09) | From baseline, mean (SE): 0.49 (0.10) | −0.21kg/m2 95% CI: −0.50, 0.07 | NS difference at 12 months for activity (hours/day); soda (servings/day); fruit/vegetable intake (servings/day) or fast food (servings/week). TV (hours/day): −0.36 95% CI: −0.64, −0.09, p=0.01 |
| BMI z-score | 12 months | n/a | n/a | −0.05 95% CI: −0.14, 0.04 | ||
| van Grieken 2013, Netherlands17 | BMI | 2 years | Change from baseline, mean (SD): 1.37 (1.53) | Change from baseline, mean (SD): 1.44 (1.71) | −0.16kg/m2 95% CI: −0.6, 0.27 | None reported |
| WC | 2 years | Change from baseline, mean (SD): 7.20 (5.49) | Change from baseline, mean (SD): 7.33 (5.30) | −0.16cm 95% CI: −1.10, 0.78 | ||
BMI = body mass index, WC = Waist Circumference, DR = Dairy Rich, ER = Energy Restricted, NS = non-significant
Two studies had designs similar in using intensive interventions and fairly low levels of interaction with controls.14,15 Stark et al15 randomized parent-child dyads to intervention or control. They provided intervention participants with dietary education, physical activity education and coaching on physical activity and general behavioral management in both a group setting and via an in-home intervention in a two-stage process with initially 12 weeks of weekly interactions and then 12 weeks of every other week interactions. Professionals also used in-home assessments to help families identify play areas and reducing high-calorie, low-nutrient foods from their specific home environment. They demonstrated a sustained effect on BMI at 12 months with a between group difference of −0.77 kg/m2, 95% CI: −1.26, −0.27. In a similar design, parent-child dyads randomized to the intervention condition in Bocca et al14 received education on diet, physical activity and behavioral counseling. Diet education was provided in six, 30 minute sessions with a dietician; a physiotherapist conducted twelve, 60 minute sessions of group physical activity; and a psychologist conducted six, 120 minute group behavioral therapy sessions focusing on role modeling and behavior change appropriate for the age group. Bocca et al14 showed significant changes in BMI at both four months with a decrease of −1.2kg/m2 95%CI: −1.50, −0.81 in the intervention compared to−0.6kg/m2 95% CI: −1.04, −0.19 in controls, and at 12 months in the intervention compared to controls, p=0.03 (Table 2).
Quattrin et al19 differed as it provided education to both intervention and control while testing the effect of personalized coaching around behavior. All parent-child dyads received ten, 60-minute educational sessions on diet, physical activity and sedentary activities. All parents were contacted eight times over the phone to follow-up on the educational sessions. Only participants randomized to the intervention received teaching on behavioral techniques in a group setting and then a 1:1 coach to discuss specific objectives and review progress after these sessions. They showed significant reductions in percent over median BMI from 30.6% ± 9.7 at baseline to 24.2% ± 10.1 at six months compared with the control group of 30.5% ± 9.3 to 28.3% ± 9.5, p <0.0021.
Kelishadi et al18 provided all participants with six monthly educational sessions led by a pediatrician and dietician with randomization of children into one of three dietary recommendations: restricted caloric intake, dairy rich diet or usual care of non-specific healthy diet education. A specific diet was not provided by the study and no other visits were prescribed. They found significant reductions in mean BMI z-score across all groups compared with baseline after the end of the intervention at six months (dairy-rich: −0.6, p=0.01; energy-restricted: −0.6, p=0.01; control: −0.5, p=0.01) with no significant difference between groups; they reported a significant mean change from baseline to six months in waist circumference: dairy-rich (DR): −2.0cm; energy-restricted (ER): −2.5cm; control: −1.7, with a significant difference across all groups, p=0.01. At 36 months, researchers reported an increase in BMI z-score between baseline and follow-up in the energy-restricted (mean change 0.7, SD=0.01) and control groups (mean change 0.6, SD=0.02) with a smaller increase in the dairy-rich group (mean change −0.1, SD=0.004, p=0.001); similar data of a smaller increase in the dairy-rich group were presented for the waist circumference outcome (Table 2).
Secondary outcomes
While all of the study designs targeted diet and activity behaviors, two did not report on the secondary outcomes.17,19 Of the two intensive interventions, Bocca et al found no difference in activity as measured by a pedometer and energy intake measured by a food diary,14 and Stark et al found no difference in activity as measured by an actigraph but did find decreased caloric intake as assessed via serial 24-hour dietary recalls.15 Kelishadi et al found no difference in energy expenditure measured via a questionnaire reportedly validated against an accelerometer and no difference in mean energy intake at 36 months as assessed via a three day food diary.18
Risk of bias
All of the studies used either a form of computerized randomization or a random numbers table and method of allocation concealment that we considered to be low risk (Table 3). Three studies were determined to be high or unclear risk for blinding of personnel.14,16,19 Only two of the studies documented blinding to treatment status when obtaining outcome measures.15,17 For the unblinded studies, given the fact that the primary measures were adiposity indices, there is a low threat to validity given the objective nature of the measurement. While there were certain components of the individual studies that contained a high or unclear risk of bias, given the objective outcome, low selective reporting, suitable random sequence generation and allocation concealment, the threat to validity from these potential biases was judged to be low. Given the heterogeneity in reported outcomes (BMI versus BMI z-score versus % over median) and the small number of studies reporting the same outcome, we were not able to utilize a funnel plot to assess for potential publication bias.
Table 3.
Assessment of bias for included studies
| Study ID | Random Sequence Generation |
Allocation Concealment |
Blinding of participants and personnel |
Blinding of outcomes |
Incomplete outcome data |
Selective Reporting |
|---|---|---|---|---|---|---|
| Taveras 201116 | Low | Low | High | Unclear | Low | Low |
| Boca 201214 | Low | Low | Unclear | Unclear | Low | Low |
| Kelishadi 200918 | Low | Low | Low | Unclear | Low | Low |
| Quattrin 201219 | Low | Low | High | Unclear | Low | Low |
| van Grieken 201317 | Low | Low | Low | Low | Low | Low |
| Stark 201115 | Low | Low | Low | Low | Low | Low |
Discussion
In this systematic review of treatment interventions for obesity in early childhood, the more intensive, multi-disciplinary studies14,15 demonstrated significant reductions in adiposity measures compared to usual care, while negative results were seen in two large studies done using systems-based interventions along with motivational interviewing.16,17 The other study that demonstrated a significant change in adiposity measure19 differed from the more intensive studies in two ways. First, they primarily only tested one variable, the role of a parent coach. Second, they had a much more similar control group in terms of intensity, in contrast to the other two studies whose usual care conditions were very low intensity.14,15
The significant effects seen in the two intensive, multi-disciplinary interventions14,15 highlight the need for intense interventions but raises the issue of feasibility. Intensive studies may work to reduce adiposity, at least in the short term, but they would be challenging for most communities to implement. More scalable interventions like Taveras et al16 and van Grieken et al17 demonstrate that for interventional purposes, that degree of intensity may not be enough. The study by Quattrin et al19 is arguably somewhere in between the others in intensity of the intervention and places additional evidence behind the idea of using some form of coaching or mentoring as suggested by other studies.21–23 Indeed, the primary difference between Quattrin et al19 and the two motivational interviewing studies after taking into account the difference in control conditions can be viewed as frequency of contact as Quattrin had eight coaching interactions over six months versus the 4–7 interactions over a year in the others, with many having only two interactions as described above.16,17 Notably, data from Quattrin et al on longer-term follow-up outcomes published after this review was completed demonstrate a sustained effect of the intervention at 12 months post-intervention.24 An exploration of the frequency of contact needed to create and sustain behavioral change around diet and activity in this age group would assist future study and program designs.
The lack of an effect on the intermediate outcome of physical activity in three studies that showed some effect on adiposity14,15,18 seems to argue against focusing on that aspect in this age group. Outcomes from trials in older children have also failed to demonstrate a consistent or sustained effect of interventions focused on activity alone.25 The intermediate outcome of energy intake had mixed results with one study showing a significant difference in the intervention group and two failing to show a difference; the heterogeneity in assessments and known challenges to those methods and lack of direct comparisons in this age group limits any conclusions.
Prior systematic reviews examining obesity interventions in older children have highlighted that combined interventions that have a behavioral component are most effective.25,26 These were completed prior to the publication of the studies included in this review, but the general finding is consistent regarding what works – i.e. focusing on both diet and physical activity with a behavioral component. Also consistent with the findings here is that more intense interventions in older children tend to demonstrate greater efficacy in reducing adiposity though the exact level of intensity is not established.27,28 Motivational interviewing has been found to be effective in promoting weight loss in adults29, and this approach has been explored recently in older children with results thus far showing mixed results.30–32
We also examined how the U.S. expert committee recommendations33 align with the evidence from this review in order to inform current practice. The expert recommendations put forth a staged approach: stage 1 or prevention plus which constitutes engaging in healthy lifestyle eating and activity habits; stage 2 or structured weight management which includes a structured approach to diet, structured activity and increased monitoring (monthly visits); stage 3 or comprehensive multidisciplinary intervention which has similar goals but with more monitoring (weekly visits initially) and includes structured behavioral intervention (with a behavioral counselor), a dietician, and an activity specialist; and finally, stage 4 or tertiary care intervention which entails a program addressing the above as well as consideration of medications, severe dietary restrictions, or surgical intervention.33 Four studies approximated a stage 1 intervention for controls;14–17 only Bocca et al14 demonstrated any impact on BMI and that effect was seen at the four month follow-up and not the 12 month post-intervention time point. The other three studies showed an increase in the adiposity measure. None of the arms truly approximated step 2 of the recommendations; the control arm of Quattrin et al19 and both arms of Kelishadi et al18 approximate at least the monthly interaction component, and all three arms showed some reduction in adiposity measure at 6 months. The intervention arms of Stark et al15 and Bocca et al14 approximate step 3 of the recommendations and both arms showed a significant reduction in their adiposity measures. Therefore the evidence to date has the strongest support for step 3 interventions. There is no evidence to support step 1 interventions having a significant in this age group at this time, and there is an absence of evidence around step 2 for this age group.
We did not include studies that included normal weight children in their intervention to separate primary prevention from treatment. It should be noted that there were a number of quality studies excluded by taking this step, and this is a limitation in applicability. This review also highlights the paucity of studies conducted in primarily minority or poor populations, where the biggest obesity burden lies.1,33 Given the cultural contexts in which coaching, behavioral change and motivational interviewing take place, testing whether these methods work in diverse populations is needed.
It has becoming increasingly recognized that weight status in early childhood is a significant predictor for weight status and its associated comorbidities later in life. From the studies included in this systematic review, more intensive, multi-disciplinary treatment interventions provide the strongest evidence of effectiveness. For individual providers, the evidence synthesized in this review can be used to target individual therapy where indicated, understanding that the data that suggest a relatively intense intervention is likely needed. For policy makers, scalability and sustainability will need to be considered as these approaches are applied to addressing the public health scope of early childhood obesity.
“What this Systematic Review Adds”.
This is the first systematic review of treatment interventions for obese 2–5 year olds
Multi-disciplinary, intensive approaches to treatment have the most evidence of efficacy
Evidence testing treatment interventions in minority populations is limited
“How to Use this Systematic Review”.
Investigation into the degree of intensity required for effective treatment is warranted
Treatment programs need evaluation in high risk groups, particularly racial and ethnic minority groups
There is evidence supporting stage 3 interventions of obesity treatment; there is little evidence supporting the other stages
Acknowledgments
Funding: Dr. Foster is supported by a grant from the NIH/NCATS: KL2 TL001118. The sponsor had no role in the study design, collection, analysis or interpretation of data; nor in the writing of the report or the decision to submit the article for publication.
Abbreviations
- BMI
body mass index
- DR
dairy-rich
- ER
energy restricted
- NS
non-significant
- WC
waist circumference
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Potential Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cunningham SA, Kramer MR, Narayan KMV. Incidence of Childhood Obesity in the United States. N Engl J Med. 2014;370:403–411. doi: 10.1056/NEJMoa1309753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh AS, Mulder C, Twisk JWR, Van Mechelen W, Chinapaw MJM. Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes Rev. 2008;9:474–488. doi: 10.1111/j.1467-789X.2008.00475.x. [DOI] [PubMed] [Google Scholar]
- 4.Waters E, Bj H, Brown T, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011:CD001871. doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- 5.Showell NN, Fawole O, Segal J, et al. A systematic review of home-based childhood obesity prevention studies. Pediatrics. 2013;132:e193–e200. doi: 10.1542/peds.2013-0786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bleich SN, Segal J, Wu Y, Wilson R, Wang Y. Systematic review of community-based childhood obesity prevention studies. Pediatrics. 2013;132:e201–e210. doi: 10.1542/peds.2013-0886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Monasta L, Batty GD, Macaluso A, et al. Interventions for the prevention of overweight and obesity in preschool children: a systematic review of randomized controlled trials. Obes Rev. 2011;12(5):e107–e118. doi: 10.1111/j.1467-789X.2010.00774.x. [DOI] [PubMed] [Google Scholar]
- 8.Hesketh KD, Campbell KJ. Interventions to prevent obesity in 0–5 year olds: an updated systematic review of the literature. Obesity. 2010;18(Suppl 1):S27–S35. doi: 10.1038/oby.2009.429. [DOI] [PubMed] [Google Scholar]
- 9.Bond M, Wyatt K, Lloyd J, Taylor R. Systematic review of the effectiveness of weight management schemes for the under fives. Obes Rev. 2011;12:242–253. doi: 10.1111/j.1467-789X.2010.00713.x. [DOI] [PubMed] [Google Scholar]
- 10.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002;(246):1–190. [PubMed] [Google Scholar]
- 11.WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 2006;450:76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x. [DOI] [PubMed] [Google Scholar]
- 12.Cole TJ. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–1240. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higgins J, Green S, editors. Cochrane Collab. 2011. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. [Google Scholar]
- 14.Bocca G, Corpeleijn E, Stolk RP, Sauer PJJ. Results of a multidisciplinary treatment program in 3-year-old to 5-year-old overweight or obese children: a randomized controlled clinical trial. Arch Pediatr Adolesc Med. 2012;166(12):1109–1115. doi: 10.1001/archpediatrics.2012.1638. [DOI] [PubMed] [Google Scholar]
- 15.Stark LJ, Spear S, Boles R, et al. A pilot randomized controlled trial of a clinic and home-based behavioral intervention to decrease obesity in preschoolers. Obesity. 2011;19(1):134–141. doi: 10.1038/oby.2010.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taveras EM, Gortmaker SL, Hohman KH, et al. Randomized controlled trial to improve primary care to prevent and manage childhood obesity: the High Five for Kids study. Arch Pediatr Adolesc Med. 2011;165:714–722. doi: 10.1001/archpediatrics.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van Grieken A, Veldhuis L, Renders CM, et al. Population-based childhood overweight prevention: outcomes of the “Be active, eat right” study. PLoS One. 2013;8(5):e65376. doi: 10.1371/journal.pone.0065376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kelishadi R, Zemel MB, Hashemipour M, Hosseini M, Mohammadifard N, Poursafa P. Can a dairy-rich diet be effective in long-term weight control of young children? J Am Coll Nutr. 2009;28(5):601–610. doi: 10.1080/07315724.2009.10719792. [DOI] [PubMed] [Google Scholar]
- 19.Quattrin T, Roemmich JN, Paluch R, Yu J, Epstein LH, Ecker Ma. Efficacy of family-based weight control program for preschool children in primary care. Pediatrics. 2012;130(4):660–666. doi: 10.1542/peds.2012-0701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuhl ES, Clifford LM, Bandstra NF, et al. Examination of the association between lifestyle behavior changes and weight outcomes in preschoolers receiving treatment for obesity. Health Psychol. 2014;33(1):95–98. doi: 10.1037/a0032741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schwartz RP, Hamre R, Dietz WH, et al. Office-Based Motivational Interviewing to Prevent Childhood Obesity: A Feasibility Study. Arch Pediatr Adolesc Med. 2007;161(5):495–501. doi: 10.1001/archpedi.161.5.495. [DOI] [PubMed] [Google Scholar]
- 22.Woo Baidal JA, Price SN, Gonzalez-Suarez E, et al. Parental perceptions of a motivational interviewing-based pediatric obesity prevention intervention. Clin Pediatr. 2013;52:540–548. doi: 10.1177/0009922813483170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Resnicow K, Davis R, Rollnick S. Motivational interviewing for pediatric obesity: Conceptual issues and evidence review. J Am Diet Assoc. 2006;106:2024–2033. doi: 10.1016/j.jada.2006.09.015. [DOI] [PubMed] [Google Scholar]
- 24.Quattrin T, Roemmich JN, Paluch R, Yu J, Epstein LH, Ecker MA. Treatment outcomes of overweight children and parents in the medical home. Pediatrics. 2014;134(2):290–297. doi: 10.1542/peds.2013-4084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oude Luttikhuis H, Baur L, Jansen H, et al. Interventions for treating obesity in children. Cochrane database Syst Rev. 2009;(1):CD001872. doi: 10.1002/14651858.CD001872.pub2. [DOI] [PubMed] [Google Scholar]
- 26.McGovern L, Johnson JN, Paulo R, et al. Clinical review: treatment of pediatric obesity: a systematic review and meta-analysis of randomized trials. J Clin Endocrinol Metab. 2008;93(12):4600–4605. doi: 10.1210/jc.2006-2409. [DOI] [PubMed] [Google Scholar]
- 27.Savoye M, Shaw M, Dziura J, et al. Effects of a weight management program on body composition and metabolic parameters in overweight children: a randomized controlled trial. JAMA. 2007;297(24):2697–2704. doi: 10.1001/jama.297.24.2697. [DOI] [PubMed] [Google Scholar]
- 28.Hughes AR, Stewart L, Chapple J, et al. Randomized, controlled trial of a best-practice individualized behavioral program for treatment of childhood overweight: Scottish Childhood Overweight Treatment Trial (SCOTT) Pediatrics. 2008;121(3):e539–e546. doi: 10.1542/peds.2007-1786. [DOI] [PubMed] [Google Scholar]
- 29.Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgarn BR. Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2011;12(9) doi: 10.1111/j.1467-789X.2011.00892.x. [DOI] [PubMed] [Google Scholar]
- 30.Davoli AM, Broccoli S, Bonvicini L, et al. Pediatrician-led motivational interviewing to treat overweight children: an RCT. Pediatrics. 2013;132(5):e1236–e1246. doi: 10.1542/peds.2013-1738. [DOI] [PubMed] [Google Scholar]
- 31.Wong EMY, Cheng MMH. Effects of motivational interviewing to promote weight loss in obese children. J Clin Nurs. 2013;22(17–18):2519–2530. doi: 10.1111/jocn.12098. [DOI] [PubMed] [Google Scholar]
- 32.Walpole B, Dettmer E, Morrongiello BA, McCrindle BW, Hamilton J. Motivational interviewing to enhance self-efficacy and promote weight loss in overweight and obese adolescents: a randomized controlled trial. J Pediatr Psychol. 2013;38(9):944–953. doi: 10.1093/jpepsy/jst023. [DOI] [PubMed] [Google Scholar]
- 33.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]