Abstract
Eyelid myoclonia with absences is classified as a unique type of generalized seizure. Its pathogenesis is proposed to involve the functional abnormalities in cortical–subcortical networks. Here, we describe the case of a 7-year-old boy who had eyelid myoclonia with absences, along with focal motor seizures. Video-EEG monitoring demonstrated eyelid myoclonia associated with 4- to 5-Hz generalized polyspike–waves preceded by focal frontal discharges. Interictal EEG showed focal epileptiform discharges over the frontal regions. Our case suggests an important role of the frontal lobe in the generation of eyelid myoclonia with absences.
Keywords: Eyelid myoclonia, Absences, Generalized seizures, Video-EEG, Frontal lobe
1. Introduction
Diffuse spike–wave activity is an electrographic hallmark of generalized epilepsy. However, focal abnormalities on electroencephalography (EEG) have also been observed in patients with generalized epilepsy. In such cases, it is supposed that the cortical focus drives widespread epileptic networks that results in generalized seizures. Eyelid myoclonia with absences is classified as a unique type of generalized seizure. Here, we describe a patient who had eyelid myoclonia with absences, along with focal motor seizures. Ictal video-EEG recording showed generalized spike–waves preceded by focal frontal discharges, suggesting that focal cortical abnormalities may induce eyelid myoclonia with absences.
2. Case report
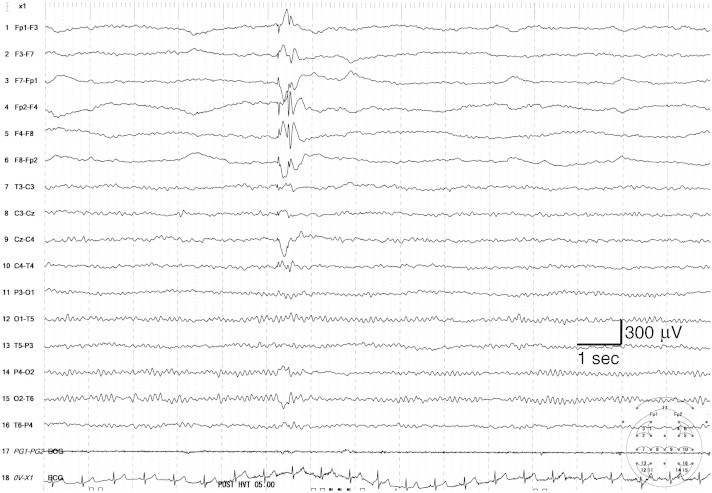
The patient is a 7-year-old boy who exhibited eyelid myoclonia with absence seizures. He was born to nonconsanguineous parents. The pregnancy and delivery were uneventful. His growth and developmental milestones were normal. Since the age of 5 years, he complained of involuntary movements of the eyelids, which occurred a few times per week. A physician diagnosed this as a tic disorder. However, his parents and brother noticed brief episodes of unresponsiveness, often associated with jerks of the eyelids, lasting 3–5 s. These episodes gradually increased in frequency, occurring many times a day. He was referred to our hospital at the age of 6. There was no family history of epilepsy. Neurological and physical examinations were normal. Magnetic resonance imaging (MRI) of the brain showed no abnormality. Eyelid movement appeared like rapid blinking and was often accompanied with upward deviation of the eyeballs and retropulsion of the head. Video-EEG recording revealed eyelid myoclonia and 4- to 5-Hz generalized polyspike–waves preceded by frontal discharges (Fig. 1). Further, EEG recording during the interictal period showed normal background activity and focal epileptiform discharges over the frontal regions (Fig. 2). Eyelid myoclonia was not triggered after eye closure. Intermittent photic stimulation evoked no photoparoxysmal response. A marked reduction in seizure frequency was achieved by sodium valproate treatment. However, he experienced a focal motor seizure with impairment of consciousness and a generalized tonic seizure during sleep in the next 2 years. The focal seizures consisted of clonic movements of the right upper limb and upward deviation of the eyeballs, lasting less than a minute. The onset of the generalized seizure was not detected. When the patient started to have focal seizures, he underwent MRI scanning of the brain, the result of which showed no abnormality.
Fig. 1.

Ictal EEG recording during eyelid myoclonia shows 4- to 5-Hz generalized polyspike–waves preceded by focal frontal discharges.
Fig. 2.
Interictal EEG recording shows focal epileptiform discharges over the frontal regions.
3. Discussion
We describe the case of a patient with eyelid myoclonia with absences who had been misdiagnosed with facial tic disorder. Video-EEG monitoring demonstrated eyelid myoclonia associated with 4- to 5-Hz generalized polyspike–waves preceded by focal frontal discharges. Interictal EEG showed focal epileptiform discharges over the frontal regions. The patient has developed focal motor seizures during follow-up. Our study suggests that frontal lobe abnormalities may induce eyelid myoclonia with absences.
Our patient had eyelid myoclonia that appeared like rapid blinking and was often associated with jerky upward deviation of the eyeballs and retropulsion of the head. The absences were brief, lasting 3–5 s. Ictal EEG revealed 4- to 5-Hz generalized polyspike–waves. These electroclinical features were in contrast to those of a typical absence seizure in childhood absence epilepsy wherein the eyes look straight ahead, and the absence seizures are associated with 3-Hz spike-and-wave discharges over a longer duration.
Eyelid myoclonia has been well recognized as the clinical feature of seizures in individuals with generalized epilepsy. Jeavons syndrome, a form of generalized epilepsy, is clinically characterized by the triad of eyelid myoclonia with or without absences, eye closure-induced seizures or EEG paroxysms, and photosensitivity. Electroencephalographic manifestations have been described as focal frontal or occipital predominant epileptiform discharges followed by generalized epileptiform discharges in both interictal and ictal recordings [1]. Thus, it has been suggested that either the frontal or the occipital lobe initiates eyelid myoclonia. The pathogenesis of eyelid myoclonia is proposed to involve the functional abnormalities in cortical–subcortical networks but not in specific brain lesions [2].
A recent cortical stimulation study has demonstrated that vertical upward eye movements can be induced by electrical stimulation of the frontal eye field (FEF), which is located in the frontal cortex [3]. Furthermore, sustained stimulation induces retropulsion of the head. Upward deviation of the eyeballs occured with frontal epileptiform activity in a patient with epilepsy [4]. Further, absence seizures are also present in patients with frontal lobe epilepsy. A subgroup of children with absence epilepsy showed an EEG epileptic abnormality with frontal onset of the typical generalized 3-Hz spike-and-wave discharges [5]. Dense-array EEG, a technique that improves the spatial resolution of scalp EEG, has demonstrated that selective cortical networks in the frontal lobe are involved in the propagation of ictal discharges in absence seizures [6]. Further, microarchitectural abnormalities in the frontal lobe have also been reported as potential facilitators of seizures in juvenile myoclonic epilepsy, another generalized epilepsy [7]. In generalized epilepsy, many brain regions have a tendency to reach an epileptogenicity level that exceeds the seizure threshold [8]. Thus, generalized seizures may start from focal brain regions and tend to generalize very fast. Eyelid myoclonia with absences may represent a type of secondarily generalized seizure originating in the frontal lobe.
In conclusion, our case suggests an important role of the frontal lobe in the generation of eyelid myoclonia with absences. Eyelid myoclonia with absences is a unique type of absence seizure associated with a variety of epilepsy syndromes [9]. Our case supports the concept that there is no absolute distinction between generalized and focal epilepsy but rather a continuum [8].
Conflict of interest
None of the authors has any conflict of interest to disclose.
Acknowledgments
We thank the patient and his parents for their willingness to be included in this report.
References
- 1.Wang X.L., Bao J.X., Liang-Shi, Tie-Ma, Deng Y.C., Zhao G. Jeavons syndrome in China. Epilepsy Behav. 2014;32:64–71. doi: 10.1016/j.yebeh.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 2.Vaudano A.E., Ruggieri A., Tondelli M., Avanzini P., Benuzzi F., Gessaroli G. The visual system in eyelid myoclonia with absences. Ann Neurol. 2014;76:412–427. doi: 10.1002/ana.24236. [DOI] [PubMed] [Google Scholar]
- 3.Kaiboriboon K., Lüders H.O., Miller J.P., Leigh R.J. Upward gaze and head deviation with frontal eye field stimulation. Epileptic Disord. 2012;14:64–68. doi: 10.1684/epd.2012.0494. [DOI] [PubMed] [Google Scholar]
- 4.Kaplan P.W., Lesser R.P. Vertical and horizontal epileptic gaze deviation and nystagmus. Neurology. 1989;39:1391–1393. doi: 10.1212/wnl.39.10.1391. [DOI] [PubMed] [Google Scholar]
- 5.Jocić-Jakubi B., Jovanović M., Janković D.S., Lagae L. Frontal-onset absences in children: associated with worse outcome? A replication study. Seizure. 2009;18:275–278. doi: 10.1016/j.seizure.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 6.Holmes M.D., Brown M., Tucker D.M. Are “generalized” seizures truly generalized? Evidence of localized mesial frontal and frontopolar discharges in absence. Epilepsia. 2004;45:1568–1579. doi: 10.1111/j.0013-9580.2004.23204.x. [DOI] [PubMed] [Google Scholar]
- 7.Woermann F.G., Free S.L., Koepp M.J., Ashburner J., Duncan J.S. Voxel-by-voxel comparison of automatically segmented cerebral gray matter—a rater-independent comparison of structural MRI in patients with epilepsy. Neuroimage. 1999;10:373–384. doi: 10.1006/nimg.1999.0481. [DOI] [PubMed] [Google Scholar]
- 8.Lüders H.O., Turnbull J., Kaffashi F. Are the dichotomies generalized versus focal epilepsies and idiopathic versus symptomatic epilepsies still valid in modern epileptology? Epilepsia. 2009;50:1336–1343. doi: 10.1111/j.1528-1167.2009.02074.x. [DOI] [PubMed] [Google Scholar]
- 9.Ferrie C.D., Agathonikou A., Parker A., Robinson R.O., Panayiotopoulos C.P. The spectrum of childhood epilepsies with eyelid myoclonia. In: Panayiotopoulos C.P., Duncan J.S., editors. Eyelid myoclonia with absences. John Libbey &Company Ltd; London: 1996. pp. 39–48. [Google Scholar]


