Abstract
The presence of human-leukocyte antigen (HLA)-antibodies and blood group incompatibility remain a large barrier to kidney transplantation leading to increased morbidity and mortality on the transplant waiting list. Over the last decade a number of new approaches were developed to overcome these barriers. Intravenous immunoglobulin (IVIG) remains the backbone of HLA desensitization therapy and has been shown in a prospective, randomized, placebo controlled trial to improve transplantation rates. Excellent outcomes with the addition of rituximab (anti-B cell) to IVIG based desensitization have been achieved. There is limited experience with bortezomib (anti-plasma cell) and eculizumab (complement inhibition) for desensitization. However, these agents may be good adjuncts for patients who are broadly sensitized with strong, complement-fixing HLA antibodies. Excellent short and long-term outcomes have been achieved in ABO incompatible transplantation with the combination of antibody removal, B cell depletion, and pre-transplant immunosuppression. Kidney paired donation has emerged as a reasonable alternative for programs who cannot provide desensitization or in conjunction with desensitization. Future therapies directed toward cytokines that alter B cell proliferation are under investigation.
Keywords: Desensitization, Antibodies, Intravenous immunoglobulin, Rituximab, ABO incompatible, Eculizumab, Bortezomib
Core tip: Intravenous immunoglobulin (IVIG) remains the backbone of human-leukocyte antigen (HLA) desensitization therapy and excellent outcomes with the addition of rituximab (anti-B cell) have been achieved. Bortezomib (anti-plasma cell) and eculizumab (complement inhibition) may be good adjuncts for patients who are broadly sensitized with strong, complement-fixing HLA antibodies. Excellent outcomes have been achieved in ABO incompatible transplantation with the combination of antibody removal, B cell depletion, and pre-transplant immunosuppression. Kidney paired donation has emerged as a reasonable alternative for programs who cannot provide desensitization or in conjunction with desensitization.
INTRODUCTION
Kidney transplantation is the gold standard for treating end-stage kidney disease and remarkable strides have been made over the last thirty years. However, there are now over 100000 people awaiting kidney transplantation in the United States according to the Organ Procurement and Transplantation Network. A significant proportion of these patients are broadly human-leukocyte antigen (HLA) sensitized and will have to wait longer to find an acceptable match; some may never. There are also those on the wait list with living donors who are blood type incompatible (ABOi), but would otherwise be an acceptable match. The long wait times incurred lead to increased mortality on the kidney transplant list[1]. The ability to provide a blood type or HLA incompatible transplant decreases mortality and gives hope to those languishing on the wait list.
Desensitization therapies started to emerge in the 1980’s. Donor specific blood transfusions were performed for HLA desensitization with limited success. There was more success with ABOi transplantation during this time period with techniques employing a combination of plasma exchange (PLEX) and splenectomy. HLA antibody desensitization with intravenous immunoglobulin (IVIG) was first reported in the mid-1990’s and ushered in a new era of transplantation. New immunomodulatory therapies have since emerged that successfully allow HLA and blood type incompatible transplant. In this review, we will discuss the current approaches and future directions of desensitization therapies.
IVIG AND RITUXIMAB (ANTI-B CELL)
IVIG is a complex preparation derived from the gamma globulin fraction of pooled human plasma used to treat primary hypogammaglobulinemia, acquired antibody deficiency, and various autoimmune disorders. It modulates the auto- and allo-immune response via broad-acting mechanisms. These mechanisms include neutralization of circulating antibodies, inhibition of B and T cell proliferation via interactions with Fc receptors, alteration of cytokine production, and down-regulation of complement. It therefore has powerful immunomodulatory effects and is now widely used for desensitization and treatment of antibody-mediated rejection (ABMR).
The efficacy of high-dose IVIG (1-2 g/kg per dose) was initially described separately by Glotz et al[2] and Tyan et al[3]. IVIG was administered on a monthly basis to those awaiting either a living or deceased donor kidney transplant. An improvement in panel reactive antibodies (PRA) and transplant rates was observed. These early successes lead to the first randomized, multicenter, placebo-controlled trial for desensitization. The National Institute of Health Ig02 trial included a total of 101 highly sensitized patients with a PRA greater than 50%. Subjects were randomized to receive dialysis with IVIG (2 g/kg) monthly for 4 mo or dialysis with equivalent volume of placebo[4] (Figure 1). Patients receiving high-dose IVIG had a statistically significant reduction in PRA and an improved rate of transplantation with a shorter wait time (4.8 years vs 10.3 years). There was a higher rate of acute rejection observed in the IVIG group (53%) compared with the placebo group (10%). However, the 2-year graft survival rates were not significantly different. This approach was effective for both living and deceased donor transplants.
Figure 1.
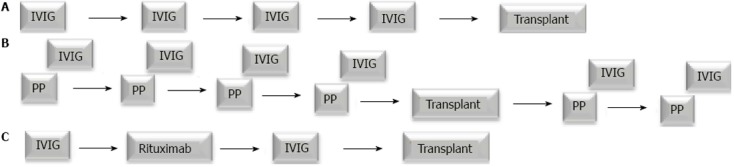
Desensitization protocols. A: The NIH Ig02 trial administered intravenous immunoglobulin (IVIG) in four monthly doses for patients awaiting a living or deceased donor transplant. This was followed by a living or deceased donor transplant once an acceptable crossmatch was achieved; B: Johns Hopkins University used a combination plasmapheresis (PP) with low-dose cytomegalovirus immune globulin following each PP session. The number and frequency of the PP sessions is dependent on the donor specific antibody titer. A living donor transplant occurs when an acceptable crossmatch is achieved. Additional sessions of PP/IVIG are administered after transplant; C: A modified protocol combining IVIG and rituximab was developed at Cedars-Sinai Medical Center. Two doses of IVIG are administered one month apart with one dose of rituximab given in between. A deceased or living donor transplant then takes place when an acceptable crossmatch is obtained.
Another approach utilizes low-dose IVIG (100 mg/kg) plus PLEX (Figure 1). Montgomery et al[5] demonstrated the efficacy of this combined therapy to rescue three living donor kidney transplant recipients who experienced ABMR and to preemptively eliminate donor specific antibody (DSA) in four recipients scheduled for a living donor kidney transplant. Recently, Montgomery et al[1] reported a significant survival benefit of desensitization with the low-dose IVIG/PLEX regimen in 211 HLA sensitized patients compared to patients who remained on the waiting list for eight years[1]. This low-dose IVIG/PLEX regimen is primarily limited to living donor kidney transplantation due to rebound of HLA-antibody that is often seen within days following therapy.
Rituximab, a chimeric anti-CD20 (anti-B cell) monoclonal antibody, has emerged as an important drug for modification of B cell and antibody responses. It is approved for treatment of lymphoma and rheumatoid arthritis and has demonstrated a significant benefit in a number of autoimmune disorders[6]. Clinical data suggest that the beneficial effects of rituximab are likely related to modification of dysfunctional cellular immunity rather than simply a reduction in antibody. Rituximab binds to CD20 and marks the cell for destruction by antibody-dependent cell mediated cytotoxicity, complement-dependent cytotoxicity and cell-mediated apoptosis via CD20 cross-linking[7,8]. Rituximab depletes CD20+ B-cells in the bone marrow, spleen and lymph nodes. It does not deplete plasma cells as they are CD20 negative. Rituximab may have some effect on plasmablasts that emerge primarily from the spleen. Data suggest that splenectomy is effective in treating ABMR because it removes DSA secreting plasmablasts that are the primary source of DSA production[9].
Over the past several years, rituximab has been studied and incorporated into desensitization protocols based on the synergistic effect with IVIG observed in patients with autoimmune diseases. Our group evaluated the effect of adding two weekly doses of rituximab to a high-dose IVIG regimen in 20 highly sensitized patients. This protocol reduced PRA from an average 77% to 44%. There was an 80% rate of transplantation with excellent patient and allograft survival. Acute rejection occurred in 50% of patients who received a transplant. Most rejection episodes were diagnosed within the first month after transplantation and were reversible with treatment[10].
We subsequently reported a larger experience evaluating the efficacy of IVIG plus rituximab. Seventy-six highly sensitized patients with a positive cross-match who were treated with a desensitization regimen (IVIG 2 g/kg on day 1 and 30 and rituximab 1 g on day 15), had significant reductions in the T cell flow cytometry crossmatch, and were successfully transplanted. Thirty-one patients received a living donor and 45 patients received a deceased donor kidney transplant. Those awaiting a deceased donor were transplanted, on average, four months following desensitization. This was after waiting an average of 95 mo. There was a 37% rate of ABMR in this cohort, occurring mostly within the first month after transplant. ABMR was treated with pulse steroids, IVIG, and rituximab. PLEX was additionally administered for severe ABMR. The rejection episodes were reversible and did not translate to inferior outcomes. Patient and graft survival were 95% and 84%, respectively, at 24 mo[11].
These studies indicate that IVIG and rituximab offer a significant benefit in reduction of anti-HLA antibodies allowing improved rates of transplantation for highly sensitized patients. However, Marfo et al[12] found IVIG and rituximab to lack efficacy in a prospective cohort study that included highly sensitized kidney transplant candidates with a calculated PRA (cPRA) greater than 50%. The cPRA estimates the percentage of deceased donor offers that will be crossmatch incompatible for a candidate taking into account both class I and class II PRA. After a mean follow-up of 334 d, only two patients received a kidney transplant compared with 14 patients in the non-desensitized group (18% vs 52%). Desensitization did not lead to any significant reduction in patients’ class I and II cPRA. There was also no change in the number of unacceptable antigens or their strength as measured by the mean fluorescence intensity (MFI). However, whole blood gene expression analyzed by microarrays demonstrated a down-regulation of immunoglobulin and B cell-associated transcripts after treatment[12].
More recently, our group conducted a double-blind randomized placebo-controlled trial comparing IVIG (2 g/kg, max 140 g administered at weeks 0 and 4) with rituximab (1 g administered at week 2) to IVIG (2 g/kg, max 140 g administered at weeks 0 and 4) with placebo (normal saline administered at week 2). Initially, 13 of 15 randomized patients received deceased donor transplants. The number of serious adverse events reported in the control group prohibited the completion of this trial and the study was un-blinded. There were six patients randomized to IVIG with rituximab and seven to IVIG with placebo. The data showed that all ABMR episodes occurred in the IVIG plus placebo group (N = 3, 43%) vs IVIG plus rituximab N = 0, 0%) (P = 0.06). The patients with ABMR episodes were treated with IVIG and rituximab with significantly improved renal function post-transplant at 6 and 12 mo. No transplant glomerulopathy was seen on protocol biopsies for the patients in IVIG plus rituximab group. It appeared that both protocols were effective in achieving an acceptable crossmatch allowing for transplantation. However, the combination of IVIG with rituximab was more effective at preventing DSA rebound, ABMR, and transplant glomerulopathy[13]. Desensitization using the combination of IVIG with rituximab was additionally shown to be cost-effective in a separate study[14].
BORTEZOMIB (ANTI-PLASMA CELL)
Bortezomib, a selective inhibitor of the 26S proteasome, was developed and approved by the United States Food and Drug Administration (FDA) for the treatment of multiple myeloma. Bortezomib inhibits antibody production from plasma cells, mediates apoptosis of this cell type and decreases the number of bone marrow-derived plasma cells. Therefore, it is expected to have strong suppressive effects on humoral immunity and may represent a promising desensitization strategy.
Bortezomib has been used for the treatment of ABMR[15-18]. Nigos et al[19] performed a retrospective chart review of six kidney transplant patients with biopsy-proven ABMR. These six patients were treated with PLEX, IVIG (100 mg/kg after each PLEX and 300-400 mg/kg for 1-2 d after the last PLEX with a cumulative dose of 1 g/kg), steroids, and single-dose rituximab (375 mg/m2) along with bortezomib (1.3 mg/m2). Four out of the six patients had biopsy proven resolution of ABMR and stable allograft function over a median follow-up of 14 mo[19]. However, in a case series of four kidney transplant recipients with subacute ABMR and persistent DSA, Sberro-Soussan et al[16] found that bortezomib (1.3 mg/m2) did not significantly decrease DSA MFI over a 5 mo follow-up. In this study, bortezomib was used as the sole therapeutic agent and only one dose was administered.
The potential effect of bortezomib on HLA antibody makes it an intriguing choice for desensitization. However, experiences with bortezomib as an alternative desensitizing agent are currently limited. Idica et al[20] reported the effect of bortezomib in thirteen highly sensitized patients. They found elimination of DSA in 10 of the patients and reduced MFI in the remaining three. Trivedi et al[17] reported a decrease in anti-HLA antibodies, both DSA and non-DSA, to less than 1000 MFI in nine of eleven patients treated with a combination of bortezomib and PLEX. The two patients without successful desensitization had strong HLA-antibodies with a peak MFI greater than 10000. Four patients had reappearance of anti-HLA antibodies after the initial reduction. However, all patients had stable graft function at a mean follow-up of 4 mo post-transplant[17]. Wahrmann used two cycles of bortezomib for pre-transplant desensitization in two highly sensitized kidney recipients[21]. Dexamethasone was added to the second cycle to enhance treatment efficacy. PRA decreased slightly from 87% to 80% in one patient and 37% to 13% in the second patient. However, both patients showed a greater than 50% reduction in the degree of complement fixing anti-HLA antibodies. Reghavan et al[22] reported a kidney transplant recipient with a weak binding DSA who successfully received a deceased-donor kidney transplant after using bortezomib in combination with rituximab. The patients cPRA was reduced from 57% to 31% and the DSA, became undetectable after transplant. The reduction in complement fixing antibodies is significant since they are mostly responsible the acute presentation of c4d positive ABMR and are difficult to modify. However, non-complement binding antibodies acting via antibody-dependent cell-mediated cytotoxicity are equally deleterious leading to chronic ABMR and transplant glomerulopathy[23].
In most studies, bortezomib shows promising outcomes for HLA desensitization. There is evidence, albeit limited, suggesting that bortezomib may be effective for altering complement fixing HLA-antibodies. These antibodies are difficult to modify with current therapies and are more deleterious to allografts. Proteasome inhibition alone may not provide durable modulation of HLA antibodies since there is no effect on precursor B cells or cytokines that promote antibody production. The main adverse effect of bortezomib is peripheral neuropathy that may occur in about 30% of treated patients. Severe events noted with bortezomib therapy include thrombocytopenia (28%) and neutropenia (11%). Given the limited experience and lack of long-term follow-up, bortezomib may be best utilized as an adjunct to other established therapies. Well-designed placebo-controlled studies are needed to further elucidate the role of bortezomib for HLA antibody desensitization.
ECULIZUMAB (COMPLEMENT INHIBITION)
Eculizumab is a humanized monoclonal antibody that binds to the complement factor C5 with high affinity, inhibiting its cleavage to C5a and C5b. This ultimately prevents the formation of the membrane attack complex. It is approved for the treatment of paroxysmal nocturnal hemoglobinuria and atypical hemolytic uremic syndrome (aHUS). It has been used primarily in transplantation to treat refractory ABMR and thrombotic microangiopathy. The binding of DSA to the donor endothelium initiates the classical pathway of the complement cascade. This, in turn, leads to the formation of the membrane attack complex (C5b-C9) and ultimately cell destruction. Eculizumab is administered as an adjunctive agent in desensitization to prevent complement dependent cytotoxicity mediated by antibody. Complement directed therapies do not have any depletive effects on HLA antibodies. Locke et al[24] presented a single case in which eculizumab was used combined with PLEX and IVIG to salvage an ongoing severe ABMR. Kidney allograft biopsies after treatment with eculizumab showed a dramatic reduction of the membrane attack complex without a significant change in C4d deposition or DSA. This is expected since C5 is located downstream from C4d in the complement activation cascade. Although the C5 epitope bound by eculizumab is located far from the C5a portion of C5, eculizumab can block C5 cleavage effectively. Eculizumab prevents the entry of the substrate molecule C5 into the C5 convertase, which means that C5 cleavage and the formation of C5a and C5b-9 are inhibited, resulting in blockade of the pro-inflammatory, pro-thrombotic and lytic functions of complement. The inhibition of complement activation at the level of C5 creates a functional C5 deficiency[25]. In the context of multiple different interventions, it was difficult to determine the impact of the anti-C5 antibody on the outcome. Burbach et al[26] reported the unsuccessful use of eculizumab in ABMR. However, this rejection was characterized by the absence of both C4d deposition in peritubular capillaries and complement binding DSA.
The role of eculizumab for HLA desensitization is not well defined. There is some evidence that eculizumab is effective in preventing ABMR in highly sensitized recipients. Stegall et al[27] reported significantly decreased incidence of early ABMR in 26 highly sensitized recipients with a positive crossmatch against their living donor. The incidence of ABMR was 7.7% (2/26) in the eculizumab group compared to 41.2% (21/51) in the control group. The two cases of ABMR in the eculizumab group occurred on post-transplant day seven and 14 in the setting of increased DSA and a biopsy that showed both C4d deposition and glomerular microthrombi. PLEX was instituted resulting in the resolution of the histologic features of ABMR in one week. The percentage of patients who developed high levels of DSA (MFI > 10000) in the first three months after transplant was similar in both groups. As expected, eculizumab did not have an impact on the presence and strength of DSA after transplant[27]. Long-term follow-up of eculizumab treated patients showed a much higher incidence of transplant glomerulopathy. Thus, C5 inhibition, alone, does not provide long-term protection from other forms of antibody-mediated injury. This raises the question of the need for concomitant B cell and antibody reduction therapies to prevent the development of transplant glomerulopathy.
There are some limitations to the use of eculizumab for desensitization. The duration of therapy after transplant has not been well established. Therefore, treatment may need to be continued indefinitely. Furthermore, it has no depletive effect on DSA and thus cannot alter the underlying immune disorder. Eculizumab only has effect against complement binding HLA antibodies. This can prevent acute ABMR but will likely be ineffective for the prevention of chronic ABMR and transplant glomerulopathy since this is mostly mediated by non-complement dependent pathways (antibody-dependent cell-mediated cytotoxicity). Finally, the cost of eculizumab is prohibitive in many settings and may ultimately limit its utility in kidney transplantation.
ABO INCOMPATIBLE TRANSPLANTATION
The development of protocols allowing for the transplantation of ABOi pairs has expanded the donor pool to recipients with a living donor who would otherwise be awaiting a deceased donor. ABOi transplantation has eased the pressure on the deceased donor waiting list and improved outcomes by transplanting recipients before they begin to experience the burden of chronic renal replacement therapy. Early experience in kidney transplantation showed that transplanting blood type incompatible donor/recipient pairs lead to hyperacute rejection and allograft thrombosis. Anti- A/B isoagglutinins bound to antigens on endothelial cells incite a cascade of events that leads to graft failure, often within minutes of graft reperfusion. Anti-A and B isoagglutinins are distinct from HLA antibodies in that they are natural antibodies that are likely produced in the bowel and peritoneum by precursor B1 cells in response to the presence of normal bacteria. Individuals are sensitized to non-self carbohydrate chains that exist on red blood cells and vascular endothelium. These chains are represented by the designation of blood types A, B, and AB. Those with blood type O do not express these chains and therefore develop antibodies to both A and B isoagglutinins.
There is now a wealth of experience with ABOi transplantation which dates back to the 1980s[28-30]. Early experience with ABOi transplantation occurred primarily in Japan where, at that time, there was limited availability of deceased donors. Through this early experience three essential components of successful ABOi transplantation were elucidated. They include antibody removal, B cell depletion, and pre-transplant immunosuppression. Many center specific protocols have been developed based on these principles[31] (Figure 2). PLEX was initially employed to remove anti-A/B antibodies prior to living donor transplantation, but this alone was not successful. It was the addition of B cell depletion by splenectomy that allowed early success[32]. However, the requirement of splenectomy for successful ABOi transplantation limited its wide spread acceptance given the added surgical risk and resultant life-long risk of infection. The development of rituximab eliminated the need for splenectomy allowing the process to be more palatable to both physicians and patients.
Figure 2.
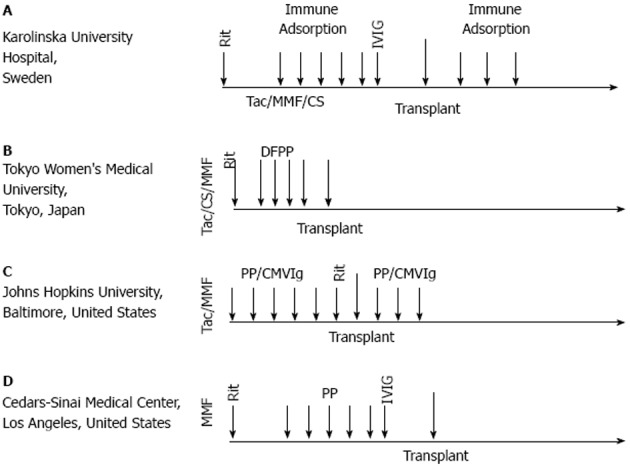
ABOi protocols. Successful ABOi transplantation has been achieved through various protocols around the world. These four protocols all contain the critical components of ABOi desensitization: antibody removal, pre-transplant immunosuppression and B cell depletion. Many protocols also use immune globulin. Rit: Rituximab; Tac: Tacrolimus; MMF: Mycophenolate mofetil; CS: Corticosteroid; DFPP: Double filtration plasmapheresis; PP: Plasmapheresis; CMVIg: Cytomegalovirus immune globulin.
Outcomes in ABOi transplantation have markedly improved over the years. In Japan, higher rates of rejection and graft loss were seen prior to the introduction of tacrolimus and mycophenolate mofetil. Toki et al[33] analyzed the impact of ABMR on ABOi transplantation. In this study, 58 consecutive ABOi transplants were divided into two groups: those that developed ABMR within months and those that did not. Graft survival was statistically less at 3, 5, and 8 years after transplant (95% vs 49%) in the ABMR group. Multivariable analysis revealed the presence of HLA DSA and an anti A/B titer ≥ 1:32 to be predictive of ABMR while pre-transplant immunosuppression with mycophenolate mofetil was protective. Successful ABOi programs incorporate these elements into their protocol starting immunosuppression with mycophenolate mofetil with or without tacrolimus and steroids one to four weeks prior to transplant, achieving an anti-A/B titer of < 1:32 at the time of transplant, and screening for anti-HLA antibodies (Figure 2).
Isoagglutinin titers have a large impact on the incidence of rejection and graft outcomes after ABOi transplantation. However, recognition of titer rebound and post-transplant PLEX have improved outcomes dramatically. Won et al[34] explored the significance of isoagglutinin titers in a retrospective analysis of 95 patients receiving an ABOi allograft. The desensitization regimen consisted of pre-transplant immunosuppression with tacrolimus, mycophenolate mofetil, and steroids seven to ten days prior to transplant. Rituximab, fixed dose (200 mg or 500 mg), was administered two to 18 d prior to PLEX. The goal titer at the time of transplant was ≤ 1:4. Basiliximab was administered for induction at the time of transplant. Isoagglutinins rebounded and peaked two weeks after transplant. There were 34 patients (35.8%) that had a rebound in titer to ≥ 1:16. Titer rebound was associated with an initial pre-transplant titer ≥ 1:256, rituximab administration ≤ 7 d prior to initiation of PLEX, and blood type O. Titer rebound was treated with additional post-transplant PLEX. Only one episode of ABMR was reported with at titer of 1:32 at the time of rejection. The addition of immune globulin to the preconditioning regimen may also have the beneficial effect of limiting titer rebound and is used in many protocols around the world (Figure 2).
The use of rituximab facilitated the expansion of ABOi transplantation by obviating the need for splenectomy. Sonnenday et al[35] reported in 2004 an early case series of successful ABOi transplantation using a regimen consisting of PLEX, low-dose CMV immune globulin and rituximab. Many other groups have since reported good outcomes with rituximab making it a key ingredient in the current era of ABOi desensitization (Figure 2). More recently, there has been a trend toward minimizing the dose of rituximab in an effort to prevent infections and decrease costs. Some programs have successfully used doses as low as 200 mg[36]. Successful ABOi desensitization has also been described in the absence of both rituximab and splenectomy. Montgomery et al[37] reported a series of 24 patients who underwent ABOi transplantation without pre-transplant B cell depletion. Good short-term outcomes were achieved with 100% graft survival. There were three episodes of ABMR. Two were treated with additional PLEX and one with salvage splenectomy. B cell depletion, via splenectomy or rituximab, has long-term proven efficacy. A minimalist approach to ABOi transplantation should only be undertaken by experienced transplant centers.
Excellent short and long-term outcomes have been achieved following these principles. Genberg et al[38] reported no difference in rejection or allograft survival in ABOi recipients vs ABO compatible recipients at three years after transplantation using a protocol consisting of immunoadsorption (antibody removal), pre-transplant immunosuppression with mycophenolate mofetil, and B-cell depletion with rituximab (Figure 2). Analysis of variables associated with rejection revealed elevated anti-A/B titer prior to transplant, absence of pre-transplant immunosuppression, and presence of DSA.
KIDNEY PAIRED DONATION
The recent development of kidney paired donation programs has facilitated the transplant of hundreds of patients in the United States. These programs may be an option for kidney transplant recipients with an HLA or blood type incompatible living donor. Many paradigms exist and range from simple two way exchanges to long, so-called domino chains that have bridging donors (Figure 3). Programs are able to completely avoid unacceptable antigens and blood types removing the need for desensitization in patients with an easy to match phenotype. However, those who are very broadly sensitized with strong HLA antibodies remain a challenge.
Figure 3.
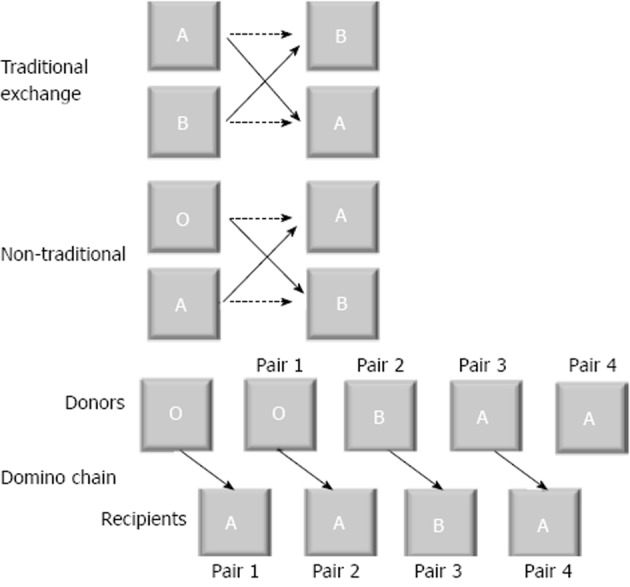
Paired kidney exchange paradigms. Traditional exchange: This exchange swaps two ABO incompatible pairs so that new donor recipient pairs are now ABO compatible. Non-traditional exchange: This exchange uses one human-leukocyte antigen (HLA) incompatible pair and one ABO incompatible pair and trades for two HLA compatible and ABO compatible transplants. Domino chain: This chain starts with a non-directed donor. The recipient of this kidney then has their donor available for another recipient. This occurs progressively until a donor cannot be matched. This donor can act as a bridge to a new chain or can donate to the deceased donor waiting list, thereby ending the chain.
A combination of desensitization therapies with kidney paired donation may result in donors with more favorable immunologic profiles. The group at Johns Hopkins recently reported on their experience combining desensitization with kidney paired donation[39]. Mathematical simulations have shown that this approach may improve the rates of transplantation with kidney paired donation programs. Yabu et al[40] recently reported the successful transplantation of five patients with a cPRA of 100% utilizing this approach. Desensitization consisted of IVIG and rituximab with the addition of bortezomib and PLEX in one case. Some centers have also adopted the approach of accepting an ABO incompatible donor in exchange for one that is HLA compatible.
Kidney paired donation provides a good alternative to desensitization in many circumstances; however it is not uniformly effective. A major limitation is that one must have a living donor available to present to the exchange. In addition, favorable donor characteristics including age and blood type must be taken into consideration and effect the likelihood of achieving a match. Patients who are very broadly sensitized with strong binding HLA antibody will be persistently difficult to match without the use of desensitization therapies.
FUTURE APPROACHES
The ongoing development of biologic agents particularly for the treatment of rheumatologic diseases may provide new avenues of exploration for desensitization. All of these agents modulate B cell activity. Epratuzumab targets CD22 on B cells and effectively modulates their activity. It has shown promise in patients with systemic lupus erythematosus (SLE)[41]. Belimumab, an antibody directed against B lymphocyte stimulator (BLyS) was recently approved for SLE and also has B cell modulator effects via inhibition of B cell proliferation[42]. Atacicept is currently under study in SLE and acts as a soluble receptor for the B cell proliferation cytokines BLyS and a proliferation-inducing ligand (APRIL) thereby neutralizing their activity. A decrease in total IgG levels has been demonstrated in early phase studies. Tocilizumab is a monoclonal antibody directed against the receptor for interleukin-6, a potent inflammatory cytokine. It is currently approved for rheumatoid arthritis and leads to reductions in IgG and inflammatory responses. It was shown in to modulate the development of DSA in a mouse model of allosensitization[43].
In summary, desensitization therapies with IVIG, rituximab and PLEX have greatly improved the access to and success of incompatible transplantation, both for HLA sensitized and ABOi patients. However, it is important to continue to pursue newer, potentially less toxic approaches that focus on B cells, plasma cells and inhibition of complement-activating antibodies. These basic therapies have also gained acceptance in treatment of ABMR and will likely become more important in transplant medicine as the impact of de novo DSA generation post-transplant is better understood.
Footnotes
P- Reviewer: Trimarchi H S- Editor: Song XX L- Editor: A E- Editor: Yan JL
Conflict-of-interest statement: The authors do not have any competing interests in relation to the submitted work.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: October 21, 2014
First decision: November 27, 2014
Article in press: April 7, 2015
References
- 1.Montgomery RA, Lonze BE, King KE, Kraus ES, Kucirka LM, Locke JE, Warren DS, Simpkins CE, Dagher NN, Singer AL, et al. Desensitization in HLA-incompatible kidney recipients and survival. N Engl J Med. 2011;365:318–326. doi: 10.1056/NEJMoa1012376. [DOI] [PubMed] [Google Scholar]
- 2.Glotz D, Haymann JP, Sansonetti N, Francois A, Menoyo-Calonge V, Bariety J, Druet P. Suppression of HLA-specific alloantibodies by high-dose intravenous immunoglobulins (IVIg). A potential tool for transplantation of immunized patients. Transplantation. 1993;56:335–337. doi: 10.1097/00007890-199308000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Tyan DB, Li VA, Czer L, Trento A, Jordan SC. Intravenous immunoglobulin suppression of HLA alloantibody in highly sensitized transplant candidates and transplantation with a histoincompatible organ. Transplantation. 1994;57:553–562. [PubMed] [Google Scholar]
- 4.Jordan SC, Tyan D, Stablein D, McIntosh M, Rose S, Vo A, Toyoda M, Davis C, Shapiro R, Adey D, et al. Evaluation of intravenous immunoglobulin as an agent to lower allosensitization and improve transplantation in highly sensitized adult patients with end-stage renal disease: report of the NIH IG02 trial. J Am Soc Nephrol. 2004;15:3256–3262. doi: 10.1097/01.ASN.0000145878.92906.9F. [DOI] [PubMed] [Google Scholar]
- 5.Montgomery RA, Zachary AA, Racusen LC, Leffell MS, King KE, Burdick J, Maley WR, Ratner LE. Plasmapheresis and intravenous immune globulin provides effective rescue therapy for refractory humoral rejection and allows kidneys to be successfully transplanted into cross-match-positive recipients. Transplantation. 2000;70:887–895. doi: 10.1097/00007890-200009270-00006. [DOI] [PubMed] [Google Scholar]
- 6.Kahwaji J, Tong C, Jordan SC, Vo AA. Rituximab: An emerging therapeutic agent for kidney transplantation. Transpl Res Risk Manag. 2009;1:15–29. [Google Scholar]
- 7.Jordan SC, Pescovitz MD. Presensitization: the problem and its management. Clin J Am Soc Nephrol. 2006;1:421–432. doi: 10.2215/CJN.01651105. [DOI] [PubMed] [Google Scholar]
- 8.Markasz L, Vanherberghen B, Flaberg E, Otvös R, Stuber G, Gustafsson Jernberg A, Olah E, Skribek H, Szekely L. NK cell-mediated lysis is essential to kill Epstein-Barr virus transformed lymphoblastoid B cells when using rituximab. Biomed Pharmacother. 2009;63:413–420. doi: 10.1016/j.biopha.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 9.Orandi BJ, Zachary AA, Dagher NN, Bagnasco SM, Garonzik-Wang JM, Van Arendonk KJ, Gupta N, Lonze BE, Alachkar N, Kraus ES, et al. Eculizumab and splenectomy as salvage therapy for severe antibody-mediated rejection after HLA-incompatible kidney transplantation. Transplantation. 2014;98:857–863. doi: 10.1097/TP.0000000000000298. [DOI] [PubMed] [Google Scholar]
- 10.Vo AA, Lukovsky M, Toyoda M, Wang J, Reinsmoen NL, Lai CH, Peng A, Villicana R, Jordan SC. Rituximab and intravenous immune globulin for desensitization during renal transplantation. N Engl J Med. 2008;359:242–251. doi: 10.1056/NEJMoa0707894. [DOI] [PubMed] [Google Scholar]
- 11.Vo AA, Peng A, Toyoda M, Kahwaji J, Cao K, Lai CH, Reinsmoen NL, Villicana R, Jordan SC. Use of intravenous immune globulin and rituximab for desensitization of highly HLA-sensitized patients awaiting kidney transplantation. Transplantation. 2010;89:1095–1102. doi: 10.1097/TP.0b013e3181d21e7f. [DOI] [PubMed] [Google Scholar]
- 12.Marfo K, Ling M, Bao Y, Calder B, Ye B, Hayde N, Greenstein S, Chapochnick-Friedman J, Glicklich D, de Boccardo G, et al. Lack of effect in desensitization with intravenous immunoglobulin and rituximab in highly sensitized patients. Transplantation. 2012;94:345–351. doi: 10.1097/TP.0b013e3182590d2e. [DOI] [PubMed] [Google Scholar]
- 13.Vo AA, Choi J, Cisneros K, Reinsmoen N, Haas M, Ge S, Toyoda M, Kahwaji J, Peng A, Villicana R, et al. Benefits of rituximab combined with intravenous immunoglobulin for desensitization in kidney transplant recipients. Transplantation. 2014;98:312–319. doi: 10.1097/TP.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 14.Vo AA, Petrozzino J, Yeung K, Sinha A, Kahwaji J, Peng A, Villicana R, Mackowiak J, Jordan SC. Efficacy, outcomes, and cost-effectiveness of desensitization using IVIG and rituximab. Transplantation. 2013;95:852–858. doi: 10.1097/TP.0b013e3182802f88. [DOI] [PubMed] [Google Scholar]
- 15.Everly MJ, Everly JJ, Susskind B, Brailey P, Arend LJ, Alloway RR, Roy-Chaudhury P, Govil A, Mogilishetty G, Rike AH, et al. Bortezomib provides effective therapy for antibody- and cell-mediated acute rejection. Transplantation. 2008;86:1754–1761. doi: 10.1097/TP.0b013e318190af83. [DOI] [PubMed] [Google Scholar]
- 16.Sberro-Soussan R, Zuber J, Suberbielle-Boissel C, Candon S, Martinez F, Snanoudj R, Rabant M, Pallet N, Nochy D, Anglicheau D, et al. Bortezomib as the sole post-renal transplantation desensitization agent does not decrease donor-specific anti-HLA antibodies. Am J Transplant. 2010;10:681–686. doi: 10.1111/j.1600-6143.2009.02968.x. [DOI] [PubMed] [Google Scholar]
- 17.Trivedi HL, Terasaki PI, Feroz A, Everly MJ, Vanikar AV, Shankar V, Trivedi VB, Kaneku H, Idica AK, Modi PR, et al. Abrogation of anti-HLA antibodies via proteasome inhibition. Transplantation. 2009;87:1555–1561. doi: 10.1097/TP.0b013e3181a4b91b. [DOI] [PubMed] [Google Scholar]
- 18.Walsh RC, Everly JJ, Brailey P, Rike AH, Arend LJ, Mogilishetty G, Govil A, Roy-Chaudhury P, Alloway RR, Woodle ES. Proteasome inhibitor-based primary therapy for antibody-mediated renal allograft rejection. Transplantation. 2010;89:277–284. doi: 10.1097/TP.0b013e3181c6ff8d. [DOI] [PubMed] [Google Scholar]
- 19.Nigos JG, Arora S, Nath P, Hussain SM, Marcus RJ, Ko TY, Sureshkumar KK. Treatment of antibody-mediated rejection in kidney transplant recipients: a single-center experience with a bortezomib-based regimen. Exp Clin Transplant. 2012;10:609–613. doi: 10.6002/ect.2012.0131. [DOI] [PubMed] [Google Scholar]
- 20.Idica A, Kaneku H, Everly MJ, Trivedi HL, Feroz A, Vanikar AV, Shankar V, Trivedi VB, Modi PR, Khemchandani SI, et al. Elimination of post-transplant donor-specific HLA antibodies with bortezomib. Clin Transpl. 2008:229–239. [PubMed] [Google Scholar]
- 21.Wahrmann M, Haidinger M, Körmöczi GF, Weichhart T, Säemann MD, Geyeregger R, Kikić Z, Prikoszovich T, Drach J, Böhmig GA. Effect of the proteasome inhibitor bortezomib on humoral immunity in two presensitized renal transplant candidates. Transplantation. 2010;89:1385–1390. doi: 10.1097/TP.0b013e3181d9e1c0. [DOI] [PubMed] [Google Scholar]
- 22.Raghavan R, Jeroudi A, Achkar K, Suki W, Gaber AO, Knight R, Land G, Dilioglou S, Patel S, Abdellatif A. Bortezomib in kidney transplant desensitization: a case report. Clin Transpl. 2009:339–342. [PubMed] [Google Scholar]
- 23.Loupy A, Hill GS, Jordan SC. The impact of donor-specific anti-HLA antibodies on late kidney allograft failure. Nat Rev Nephrol. 2012;8:348–357. doi: 10.1038/nrneph.2012.81. [DOI] [PubMed] [Google Scholar]
- 24.Locke JE, Magro CM, Singer AL, Segev DL, Haas M, Hillel AT, King KE, Kraus E, Lees LM, Melancon JK, et al. The use of antibody to complement protein C5 for salvage treatment of severe antibody-mediated rejection. Am J Transplant. 2009;9:231–235. doi: 10.1111/j.1600-6143.2008.02451.x. [DOI] [PubMed] [Google Scholar]
- 25.Zuber J, Fakhouri F, Roumenina LT, Loirat C, Frémeaux-Bacchi V. Use of eculizumab for atypical haemolytic uraemic syndrome and C3 glomerulopathies. Nat Rev Nephrol. 2012;8:643–657. doi: 10.1038/nrneph.2012.214. [DOI] [PubMed] [Google Scholar]
- 26.Burbach M, Suberbielle C, Brochériou I, Ridel C, Mesnard L, Dahan K, Rondeau E, Hertig A. Report of the inefficacy of eculizumab in two cases of severe antibody-mediated rejection of renal grafts. Transplantation. 2014;98:1056–1059. doi: 10.1097/TP.0000000000000184. [DOI] [PubMed] [Google Scholar]
- 27.Stegall MD, Diwan T, Raghavaiah S, Cornell LD, Burns J, Dean PG, Cosio FG, Gandhi MJ, Kremers W, Gloor JM. Terminal complement inhibition decreases antibody-mediated rejection in sensitized renal transplant recipients. Am J Transplant. 2011;11:2405–2413. doi: 10.1111/j.1600-6143.2011.03757.x. [DOI] [PubMed] [Google Scholar]
- 28.Tanabe K. Japanese experience of ABO-incompatible living kidney transplantation. Transplantation. 2007;84:S4–S7. doi: 10.1097/01.tp.0000296008.08452.4c. [DOI] [PubMed] [Google Scholar]
- 29.Genberg H, Kumlien G, Wennberg L, Berg U, Tydén G. ABO-incompatible kidney transplantation using antigen-specific immunoadsorption and rituximab: a 3-year follow-up. Transplantation. 2008;85:1745–1754. doi: 10.1097/TP.0b013e3181726849. [DOI] [PubMed] [Google Scholar]
- 30.Montgomery RA, Locke JE, King KE, Segev DL, Warren DS, Kraus ES, Cooper M, Simpkins CE, Singer AL, Stewart ZA, et al. ABO incompatible renal transplantation: a paradigm ready for broad implementation. Transplantation. 2009;87:1246–1255. doi: 10.1097/TP.0b013e31819f2024. [DOI] [PubMed] [Google Scholar]
- 31.Kahwaji J, Vo AA, Jordan SC. ABO blood group incompatibility: a diminishing barrier to successful kidney transplantation? Expert Rev Clin Immunol. 2010;6:893–900. doi: 10.1586/eci.10.78. [DOI] [PubMed] [Google Scholar]
- 32.Alexandre GP, Squifflet JP, De Bruyère M, Latinne D, Reding R, Gianello P, Carlier M, Pirson Y. Present experiences in a series of 26 ABO-incompatible living donor renal allografts. Transplant Proc. 1987;19:4538–4542. [PubMed] [Google Scholar]
- 33.Toki D, Ishida H, Setoguchi K, Shimizu T, Omoto K, Shirakawa H, Iida S, Horita S, Furusawa M, Ishizuka T, et al. Acute antibody-mediated rejection in living ABO-incompatible kidney transplantation: long-term impact and risk factors. Am J Transplant. 2009;9:567–577. doi: 10.1111/j.1600-6143.2008.02538.x. [DOI] [PubMed] [Google Scholar]
- 34.Won D, Choe W, Kim HJ, Kwon SW, Han DJ, Park SK. Significance of isoagglutinin titer in ABO-incompatible kidney transplantation. J Clin Apher. 2014;29:243–250. doi: 10.1002/jca.21312. [DOI] [PubMed] [Google Scholar]
- 35.Sonnenday CJ, Warren DS, Cooper M, Samaniego M, Haas M, King KE, Shirey RS, Simpkins CE, Montgomery RA. Plasmapheresis, CMV hyperimmune globulin, and anti-CD20 allow ABO-incompatible renal transplantation without splenectomy. Am J Transplant. 2004;4:1315–1322. doi: 10.1111/j.1600-6143.2004.00507.x. [DOI] [PubMed] [Google Scholar]
- 36.Hatakeyama S, Fujita T, Murakami R, Suzuki Y, Sugiyama N, Yamamoto H, Okamoto A, Imai A, Tobisawa Y, Yoneyama T, et al. Outcome comparison of ABO-incompatible kidney transplantation with low-dose rituximab and ABO-compatible kidney transplantation: a single-center experience. Transplant Proc. 2014;46:445–448. doi: 10.1016/j.transproceed.2013.09.036. [DOI] [PubMed] [Google Scholar]
- 37.Montgomery RA, Locke JE. ABO-incompatible transplantation: less may be more. Transplantation. 2007;84:S8–S9. doi: 10.1097/01.tp.0000296032.12974.bb. [DOI] [PubMed] [Google Scholar]
- 38.Genberg H, Kumlien G, Wennberg L, Tydén G. Long-term results of ABO-incompatible kidney transplantation with antigen-specific immunoadsorption and rituximab. Transplantation. 2007;84:S44–S47. doi: 10.1097/01.tp.0000296031.41424.f8. [DOI] [PubMed] [Google Scholar]
- 39.Montgomery RA, Lonze BE, Jackson AM. Using donor exchange paradigms with desensitization to enhance transplant rates among highly sensitized patients. Curr Opin Organ Transplant. 2011;16:439–443. doi: 10.1097/MOT.0b013e32834897c1. [DOI] [PubMed] [Google Scholar]
- 40.Yabu JM, Pando MJ, Busque S, Melcher ML. Desensitization combined with paired exchange leads to successful transplantation in highly sensitized kidney transplant recipients: strategy and report of five cases. Transplant Proc. 2013;45:82–87. doi: 10.1016/j.transproceed.2012.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Strand V, Petri M, Kalunian K, Gordon C, Wallace DJ, Hobbs K, Kelley L, Kilgallen B, Wegener WA, Goldenberg DM. Epratuzumab for patients with moderate to severe flaring SLE: health-related quality of life outcomes and corticosteroid use in the randomized controlled ALLEVIATE trials and extension study SL0006. Rheumatology (Oxford) 2014;53:502–511. doi: 10.1093/rheumatology/ket378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Webber A, Hirose R, Vincenti F. Novel strategies in immunosuppression: issues in perspective. Transplantation. 2011;91:1057–1064. doi: 10.1097/TP.0b013e3182145306. [DOI] [PubMed] [Google Scholar]
- 43.Wu G, Chai N, Kim I, Klein AS, Jordan SC. Monoclonal anti-interleukin-6 receptor antibody attenuates donor-specific antibody responses in a mouse model of allosensitization. Transpl Immunol. 2013;28:138–143. doi: 10.1016/j.trim.2013.03.003. [DOI] [PubMed] [Google Scholar]


