Abstract
Background:
India leads the world with maximum number of diabetes patients being termed as the “diabetes capital of the world.” Certain risk factors including unsatisfactory diet, overweight, and a sedentary lifestyle are potentially reversible. Acharayas have widely described the role of diet and activities to control Madhumeha (type 2 diabetes mellitus [T2DM]) along with medications. Habitual consumption of roasted or dry Barley (Hordeum vulgare L.) flour, Mudga (Phaseolus aureus Roxb.) and Amalaki (Emblica officinalis Gaertn.) prevents the manifestation of Prameha.
Aim:
To assess the clinical effects of dietary interventions and life style modifications in Madhumeha patients.
Materials and Methods:
Present study was carried out on 56 patients of Madhumeha from S.S. Hospital, Banaras Hindu University, Varanasi. Dietary interventions and life style modifications schedule was prepared based on Ayurvedic principles and patients were advised to follow this regimen. Three consecutive follow-ups were done for 3 months at the interval of one month each.
Results:
Significant improvement was observed in clinical signs and symptoms along with plasma glucose and glycosylated hemoglobin (HbA1c) in Madhumeha patients after these interventions (P < 0.001).
Conclusion:
Dietary interventions and life style modifications are two important tools by which adequate glycemic control can be obtained, especially in newly diagnosed T2DM patients and in patients who are on antidiabetic medication, but not properly controlled.
Keywords: Amalaki, blood sugar, HbA1c, Madhumeha, Mudga, type 2 diabetes mellitus, Yava
Introduction
India leads the world with maximum number of diabetic patients being termed as the “diabetes capital of the world.” According to the Diabetes Atlas 2006 published by the International Diabetes Federation, the number of people with diabetes in India currently around 40.9 million is expected to rise to 69.9 million by 2025 unless urgent preventive steps are taken.[1] The so called “Asian Indian Phenotype” refers to certain unique clinical and biochemical abnormalities in Indians which include increased insulin resistance, greater abdominal adiposity that is, higher waist circumference despite lower body mass index (BMI), lower adiponectin and higher high sensitive C-reactive protein levels. This phenotype makes Asian Indians more prone to diabetes and premature coronary artery disease. At least a part of this is due to genetic factors.[2] However, the primary driver of the epidemic of diabetes is the rapid epidemiological transition associated with changes in dietary patterns and decreased physical activity as evident from the higher prevalence of diabetes in the urban population.
Treatment prevents some of its devastating complications, but does not usually restore normoglycemia or eliminate all the adverse consequences. The diagnosis is often delayed until complications are present. Since current methods of treating diabetes remain inadequate, prevention is preferable.[3] The hypothesis that type 2 diabetes is preventable is supported by observational studies and clinical trials of diet and exercise. Interventions that work in some societies may not work in others because social, economic, and cultural factors influence diet and exercise. This is of special concern in India, where there is great regional and ethnic diversity in dietary and lifestyle patterns.
Sahaja/Kulaja/Jataja and Apathyanimittaja[4] (diabetogenic diet and activity) are the two important etiological factors that explain the heterogenous nature of this disease. Incidence of this disease increases with age due to natural dominancy of Vata in the old age.[5] In Ayurveda treatment principle of Madhumeha includes bio-purification therapy, palliative care, rejuvenation therapy, dietary interventions and life style modifications. Acharayas have widely described the role of diet and activities to control Madhumeha along with medications. Habitual consumption of roasted or dry Yava (barley - Hordeum vulgare L.) flour, Mudga (Phaseolus aureus Roxb.) and Amalaki (Emblica officinalis Gaertn.) prevents the manifestation of Prameha.[6] In new cases of diabetes, adequate glycemic control can be obtained by diet and life style advice alone in approximately 50%, only 20–30% will need oral antidiabetic drugs and 20–30% will require insulin.[7] In a patient with suspected type 2 diabetes mellitus (T2DM), the first line of therapy involves advice about dietary and life style modifications. In this regard, present study had been under taken to assess the effect of dietary interventions and life style modifications in Madhumeha (T2DM) patients on clinical signs and symptoms with biochemical parameters.
Materials and Methods
Randomly 56 patients of Madhumeha (T2DM) from OPD and IPD of S.S. Hospital Ayurveda wing and Endocrine O.P.D were selected for the present study from August 2011 to November 2012. The study was approved by the ethical committee of the Institute of Medical Sciences, Banaras Hindu University, Varanasi (vide letter no Dean/2010-11/346 dated 21-12-2010). Informed consent was obtained from selected patients. Selection of patients was based on subjective and objective criteria.
Inclusion criteria
Age of patients in between 25 and 75 years
Patients with diagnostic features of Madhumeha (T2DM) clinically such as Prabhuta Mutrata (polyuria), Bahuashee (polyphagia), Pipasa (polydipsia), Gal-Talu Shosha (throat dryness), Kara-Pada Suptata (numbness/tingling hand and foot), Daurbalya (weakness), Sayyasana-Swapna Sheela (always desire to occupy bed), Netra Upadeha (more Akshi Vit), Dantadinam Maladhyatvam (dirty teeth), Swedo-Anga Gandha (sweating with smell) and Asya Madhurya (sweet taste in mouth)
Fasting plasma glucose (FPG) level ≥120 mg/dl and/or 2-h (postprandial) plasma glucose level ≥200 mg/dl.[8]
Exclusion criteria
Patients with T1DM
Patients with T2DM who were insulin dependent and with severe diabetic complications like cardiovascular diseases, nephropathy and retinopathy
DM associated with systemic viral/bacterial infections like HIV, Hepatitis, Tuberculosis and Malignancy etc
Diabetes due to endocrinopathies, e.g., phaeochromocytoma, acromegaly, Cushing's syndrome, hyperthyroidism, etc
Patients with certain genetic syndromes, which are sometimes associated with DM, e.g. Down's syndrome, Klinefelter's syndrome, Turner's syndrome, etc.
Posology
Registered patients were advised to follow dietary interventions and life style modifications strictly as per our advice and informed them to come to next follow-up at 1 one month interval for three consecutive months along with ancillary investigations to report the changes in biochemical parameters after following the dietary interventions and life style modifications.
Instructions for dietary interventions and life–style modifications
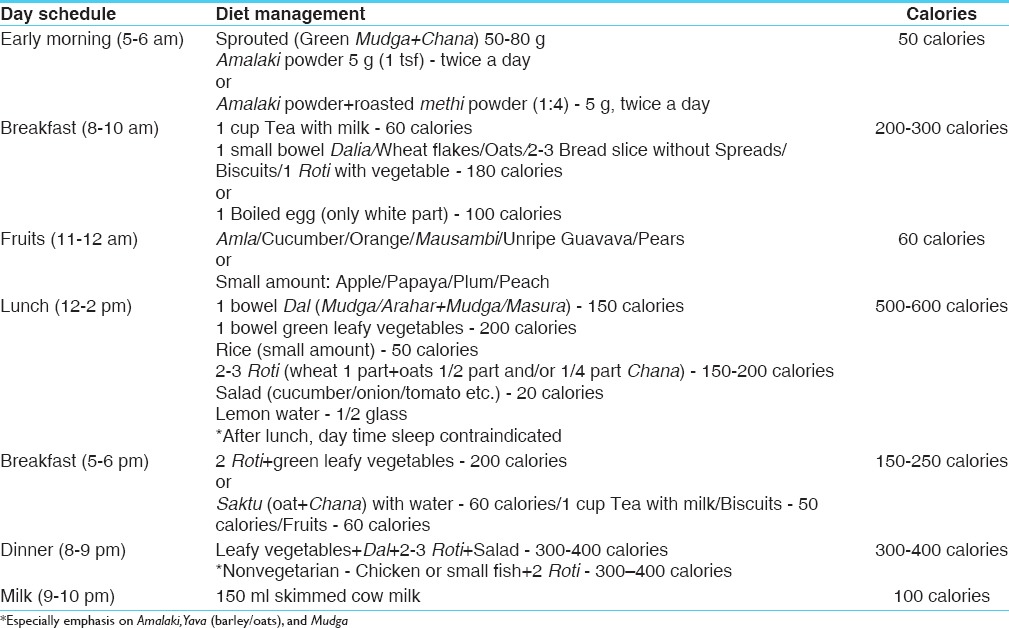
Diet and activities schedule was prepared, and the same was advised to the patients. Detail description of dietary interventions, which were advised to the patients [Table 1].
Table 1.
Specific low caloric diet chart (1400-1800 calories)
Life-style modifications
Details of life style modifications advised to the patient are as follows:
Early morning awakening
Brisk walking/light exercises for 30 min
Massage/swimming
Yoga - Asana (as Padmasana, Pashcimottanasana, Suptavajrasana, Surya-Namaskar, Dhanurasana)
Pranayama (Bhastrika, Anuloma-Viloma)
After lunch walking for 15 min
After dinner slow walking for 15 min.
Patients were advised to sleep only 6–7 h during the night and avoid sleep during day time. Patients were totally prohibited to take sweet items, fried items, fast foods, Urad, meat, milk products, cold drinks, chocolates, alcohol substances, dry fruits, curd, pickles, potato, sweet-potato, bread, butter, fermented items, etc.
Assessment criteria
Subjective parameters
The assessment was done with cardinal symptoms of Madhumeha such as Prabhuta-Mutrata (polyuria), Bahuashee (polyphagia), Pipasa (polydipsia), Gal-Talu Shosha (polydipsia), Daurbalya (weakness), Sayyasana-Swapna (always desire to occupy bed), Danteshu-Malotpatti (teeth sensation/pyorrhoea), Swedaadhikya-Anga-Gandha (sweating with smell), Netra-Updeha (blurring vision) and Asya-Madhurya (sweet taste in mouth).
Objective parameters
Blood pressure, body weight, BMI, central obesity, plasma glucose (FPG); 2-h plasma glucose (2-hPG) and glycosylated haemoglobin (HbA1c).
Statistical analysis
Statistical analysis was performed using Statistical Package of Social Science (SPSS)-(IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.) Data was analyzed statistically in terms of mean score (M), standard deviation (S.D.). Paired t-test was carried out at the level of P values 0.05, 0.01 and 0.001.
Observations
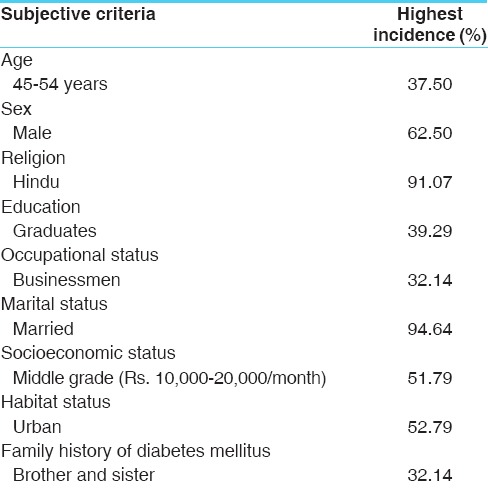
Patients selected for study were in the range of 25–74 years of age. The present clinical study reveals that the age predominance of 45–54 years that is, 37.00% and then 55–64 years, 35–44 years, 65–74 years, 25–34 years were 24.00%, 23.00%, 9.00%, and 7.00% respectively. Of 56 patients, 62.50% of the patients were males and 37.50% of patients were females. In this clinical study, 91.00% of patients were belonging to Hindu religion while 8.93% of patients belonging to Muslim religion. Present study reveals that the education-wise majority of the patients as graduates 39.29%, 23.21% had completed their primary education, 19.64% of the patients had completed intermediate education, and 17.86% were uneducated. Of 56 patients, maximum no of patients, that is, 32.14. % are belonging to business category, and 26.79% patients were indulged in house hold work. 16.07%, 10.71%, 8.93%, and 5.36% patients were belonging to labour, retired (Government employee), farmer and service in field work respectively. Data shows that 94.64% of patients were married and 5.36% were unmarried. The present study covered a cross-section of the society. It was found that majority of the patients were belonging to middle income group, that is, 51.79% and 39.29% patients were from lower income group and 08.92% patients were from high income group. It was found that the majority of the patients were from urban habitat (52.79%) when compared to those from rural habitat are (48.21%). The present study reveals that brothers and sisters were maximum sufferers, that is, 32.14% followed by father, mother and both 14.29%, 14.29%, and 8.93% respectively. No family history observed in 30.35% of cases [Table 2].
Table 2.
Demographic profile of Madhumeha patients (n=56)
Results
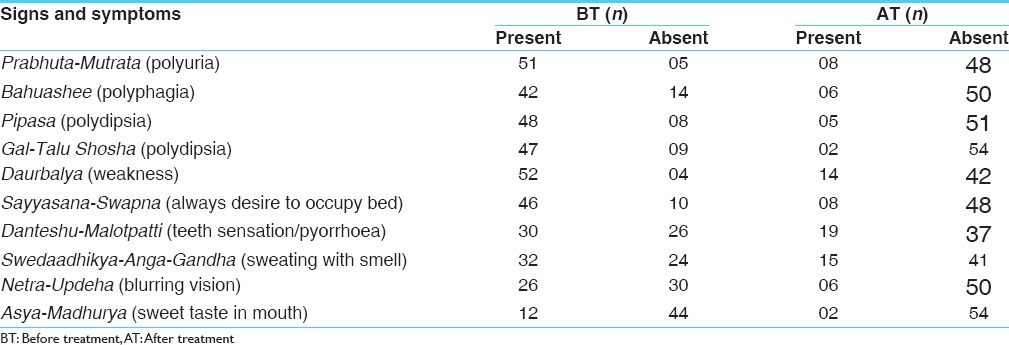
Effect of therapy on subjective parameters
Clinical improvement in signs and symptoms after dietary interventions and lifestyle modifications observed in the present clinical study indicated its utility in Madhumeha management [Table 3].
Table 3.
Effect of dietary interventions and life-style modifications in Madhumeha patients
Effect of therapy on objective parameters
In present clinical study significant improvement was observed in blood pressure control, Weight reduction and BMI of Madhumeha patients after three consecutive follow-ups of dietary interventions and life style modifications.
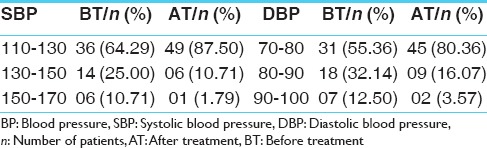
Effect of therapy on blood pressure
The present study revealed that before dietary interventions and life style modifications, 64.29% patients were having normal systolic blood pressure, 25.00% patients were having raised systolic blood pressure in the range of 130–150 mm/Hg, while 10.71% patients belonged to hypertensive group in the range of 150–170 mm/Hg. None of the patient in this study has reported systolic blood pressure above 170 mm/Hg. After dietary interventions and life style modifications, above data was changed up to 87.50%, 10.71%, and 1.79% respectively. The data of the present clinical study indicated that before dietary interventions and life style modifications, 55.36% patients were having normal diastolic blood pressure, 32.14% patients were having had raised diastolic blood pressure in the range of 80–90 mm/Hg. 12.50% patients had raised to hypertensive group in the range of 90–100 mm/Hg. None of the patients in this study have reported diastolic blood pressure above 100 mm/Hg. After dietary interventions and life style modifications, above data were changed up to 80.36%, 16.07%, and 3.57% respectively [Table 4].
Table 4.
Effect of therapy on BP in Madhumeha patients
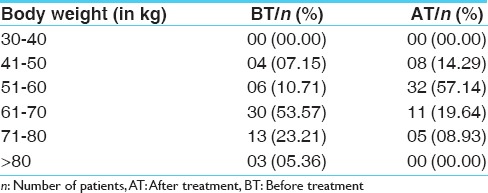
Effect of therapy on body weight
The present clinical study reveals that before dietary interventions and life style modifications, the incidence of patients in the weight group of 41–50 kg, 51–60 kg, 61–70 kg, 71–80 kg, and >80 kg was 7.15%, 10.71%, 53.57%, 23.21%, and 5.36% respectively. After dietary interventions and life style modifications, the incidence of patients in the weight group was 14.29%, 57.14%, 19.64%, 08.93%, and 00%, respectively [Table 5].
Table 5.
Effect of therapy on body weight in Madhumeha patients
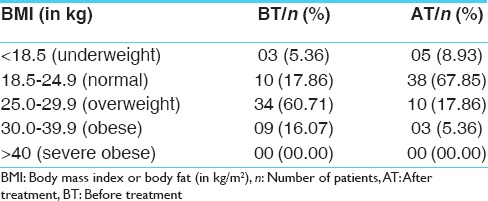
Effect of therapy on body mass index
The present study reveals that before dietary interventions and life style modifications, the incidence of patients in the overweight group of 25.0–29.9 kg/m2 (60.71%) was the highest, followed by normal group of 18.5–24.9 kg/m2 (17.86%), Obese group of 30.0–39.9 kg/m2 (16.07%), and underweight group of <18.5 kg/m2 (5.36%), respectively. After dietary interventions and life style modifications, the incidence of patient in the normal group of 18.5–24.9 kg/m2 (67.85%) was the highest, followed by overweight group of 25.0–29.9 kg/m2 (17.86%), underweight group of <18.5 kg/m2 (8.93%), and obese group of 30.0–39.9 kg/m2 (5.36%), respectively [Table 6].
Table 6.
Effect of therapy on BMI in Madhumeha patients
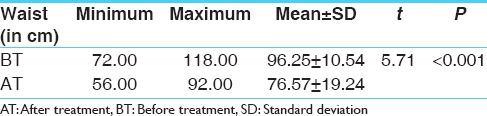
Effect of therapy on central obesity
Data showed that the presence of central obesity mean range before treatment was 96.25 ± 10.54 and after dietary interventions and life style modifications it reduced to 76.57 ± 19.24 [Table 7].
Table 7.
Effect of therapy on central obesity in Madhumeha patients (n=56)
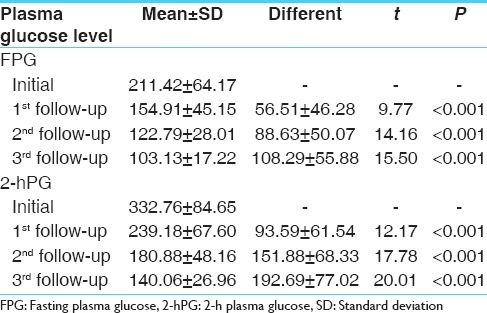
Effect of therapy on plasma glucose
The present clinical study reveals that mean initial score for FPG was 211.42, which reduced to 103.13, after three consecutive follow-up was done for 3 months at the interval of 1-month. Mean score for 2-hPG was 332.76, which reduced to 140.06, after three consecutive follow-up was done for 3 months at the interval of 1-month [Table 8].
Table 8.
Effect of therapy on plasma glucose level in Madhumeha patients (n=56)
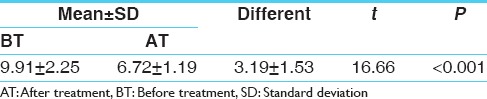
Effect of therapy on glycosylated hemoglobin
The present clinical data reveals that before dietary interventions and life style modifications HbA1c mean range was 9.91, which reduced to 6.72 after the 3 months regimen [Table 9].
Table 9.
Effect of therapy on glycosylated hemoglobin in Madhumeha patients (n=56)
Discussion
It is elaborately described since ages erratic lifestyle and diet lead to obesity, followed by Madhumeha (T2DM) along with its complications. Acharaya Sushurta[9] and Vagbhata[10] have similar opinion regarding the etiological factors that Apathya-Nimittaja Prameha may be due to intake of more foods, which aggravates Kapha, Meda and Mutra, lack of exercise and other sedentary life styles and it may be compared to T2DM. Excessive sleep during day and night, lack of exercise, laziness and frequent and excessive use of new grains, use of new peas, black gram and other pulses along with Ghrita, Tila, Tilapista etc., and the use of sugar cane juice, milk and its products, fresh wine, Dadhivikara, meat soups of different animals, residing in water or near water and all other materials vitiating Kapha, results into Prameha in susceptible individuals. Consuming foods that are low in fiber and high in glycemic loads is associated with increased risk of DM. The overall metabolic deregulation associated with Madhumeha (DM) causes secondary patho-physiologic changes in multiple organ system that imposes a tremendous burden on the individual with DM and on the health care system. All the above etiological factors of Prameha are similar to the modern concept of DM, which is a major health hazard affecting millions of people all over the world. So Prameha patients must take diet, which nourish the body elements, but will not contribute to the pathogenesis by generating excessive Kapha, Meda, Kleda and Mutra.[11] It must be planned according to agni of patient. According to Charaka, habitual consumption of roasted or/and dry barley (Yava) flour, Mudga and Amalaki prevents the manifestation of Prameha. Yava must constitute the major diet portion of Prameha patient. Yava causes Santarpana without vitiating Doshas. Yava possesses mutual properties, Pittaghna and Kaphaghna and bestowing stability. Earlier studies have shown that Yava has property of antihypertensive effect, gastrointestinal effects, sympathomimetic effects, glycemic/insulinemic effect, metabolic effects and lowers the serum cholesterol level.[12,13,14] Amalaki is highly nutritious and is an important dietary source of Vitamin C, minerals and amino acids. Several studies have shown their antioxidant and antidiabetic properties and also useful in heart and eye disorders.[15,16] Mudga contains 64.04% protein and fair source of calcium, iron, Vitamins A and B. Sprouts are a good source of Vitamin B which is important for proper functioning of nerve conduction and these increases Kleda. Several studies have also proved their hypolipidemic, hypotensive and chronotropic effects.[17,18] Apatarpana, that is, weight reduction with the help of Vihara in the treatment of Prameha as described by all Acharyas. All these manoeuver help to reduce Meda and Kapha, which are the culprits in Prameha. Sushruta has described different types of exercises helpful for Prameha patients.[19]
Outcome measure of the present study
Dietary interventions and life style modifications improved glycemic control, insulin sensitivity and cardiovascular fitness. Hence, reduction of plasma glucose level, hyperlipidemia and hypertensions were observed in the present study. Reduction of the signs and symptoms, weight and BMI also indicates that dietary interventions and life style modifications are important tools for the management of Madhumeha (T2DM).
Conclusion
It can be concluded that dietary interventions and life style modifications are two important tools by which adequate glycemic control can be obtained especially in newly diagnosed type-2 DM patients. These tools are also useful in patients, who are on antidiabetic medication, without porper control on glycemic index.
Acknowledgment
Authors are thankful to Dr. Girish Singh, Department of Community Medicine, IMS, BHU for statistical analysis.
Footnotes
Source of Support: Faculty of Ayurveda, IMS, BHU, Varanasi
Conflict of Interest: None declared.
References
- 1.Sicree R, Shaw J, Zimmet P. Diabetes and impaired glucose tolerance. In: Gan D, editor. Diabetes Atlas. International Diabetes Federation. 3rd ed. Belgium: International Diabetes Federation; 2006. pp. 15–103. [Google Scholar]
- 2.Mohan V, Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of type 2 diabetes: Indian scenario. Indian J Med Res. 2007;125:217–30. [PubMed] [Google Scholar]
- 3.Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with life-style intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sushruta, Sushruta Samhita, Chikitsa Sthana, Prameha Chikitsa Adhyaya. In: 11/3. 12th ed. Ambikadutta Shastri., editor. Varanasi: Chowkhamba Prakahsan; 2001. p. 59. [Google Scholar]
- 5.Byadgi PS. 1st ed. Vol. 1. Varanasi: Chowkhamba Prakasan; 2009. Ayurvediya Vikriti-Vijnan and Roga Vijanan; p. 474. [Google Scholar]
- 6.Agnivesha, Charaka, Dridhabala, Charaka Samhita, Chikitsa Sthana, Prameha Chikitsa Adhyaya. In: 6/46-48. 2nd edition. Jadavaji T, editor. Varanasi: Chaukhamba Sanskrit Sansthan; 2007. p. 242. [Google Scholar]
- 7.Frier BM, Fisher M. Diabetes mellitus. In: Colledge NR, Walker BR, Ralston SH, editors. Davidson's Principles and Practice of Medicine. 21st ed. Edinburg: Churchil Livingstone Elsevier; 2010. p. 818. International edition. [Google Scholar]
- 8.Powers AC. Diabetes mellitus. In: Longo DL, Fauci SA, Kasper DL, Hauser SL, Jameson SL, Loscalzo J, editors. Harrison's Principles of Internal Medicine. 18th ed. II. USA: McGraw Hill Companies; 2012. p. 2970. [Google Scholar]
- 9.Sushruta, Sushruta Samhita, Nidana Sthana, Prameha Nidanam Adhyaya. In: 6/3. 12th ed. Ambikadutta Shastri., editor. Varanasi: Chowkhamba Prakahsan; 2001. p. 251. [Google Scholar]
- 10.Vagbhatta, Astanga Hridayam, Nidana Sthana, Prameha Nidanam Adhyaya. In: 10/1-3/ 13th ed. Yadunandana Upadhyaya., editor. Varanasi: Chowkhamba Prakahsan; 2009. p. 253. [Google Scholar]
- 11.Ibidem. Astanga Hridayam, Chikitsa Sthana, Prameha ChikitsumAdhyaya, 12/37; 374 [Google Scholar]
- 12.Behall KM, Scholfield DJ, Hallfrisch J. Whole-grain diets reduce blood pressure in mildly hypercholesterolemic men and women. J Am Diet Assoc. 2006;106:1445–9. doi: 10.1016/j.jada.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 13.Qureshi AA, Burger WC, Peterson DM, Elson CE. The structure of an inhibitor of cholesterol biosynthesis isolated from barley. J Biol Chem. 1986;261:10544–50. [PubMed] [Google Scholar]
- 14.Casiraghi MC, Garsetti M, Testolin G, Brighenti F. Post-prandial responses to cereal products enriched with barley beta-glucan. J Am Coll Nutr. 2006;25:313–20. doi: 10.1080/07315724.2006.10719541. [DOI] [PubMed] [Google Scholar]
- 15.Anthony C, Dweck FLS, Dweck D, Mitchell D. Emblica officinalis [Syn: Phyllanthus Emblica] or Amla: The Ayurvedic wonder. Available form: http://www.dweckdata.com/published_papers/emblica_officinalis.pdf .
- 16.Khan KH. Roles of Emblica officinalis in medicine – A review. Bot Res Int. 2009;2:218–28. [Google Scholar]
- 17.Srivastava A, Joshi LD, Singh SP. Changes in serum lipids in normal and diabetic guinea pigs on feeding Phaseolus aureus (Green gram) Indian J Clin Biochem. 1989;4:50–7. [Google Scholar]
- 18.Chiu KW, Fung AY. The cardiovascular effects of green beans (Phaseolus aureus), common rue (Ruta graveolens), and kelp (Laminaria japonica) in rats. Gen Pharmacol. 1997;29:859–62. doi: 10.1016/s0306-3623(97)00001-3. [DOI] [PubMed] [Google Scholar]
- 19.Sushruta, Sushruta Samhita, Chikitsa Sthana, Prameha Chikitsa Adhyaya. In: 11/12. Twelth edition. Ambikadutta Shastri., editor. Varanasi: Chowkhamba Prakahsan; 2001. p. 62. [Google Scholar]


