Abstract
Medial patella subluxation is a disabling condition typically associated with previous patellofemoral instability surgery. Patients often describe achy pain with painful popping episodes. They often report that the patella shifts laterally, which occurs as the medial subluxed patella dramatically shifts into the trochlear groove during early knee flexion. Physical examination is diagnostic with a positive medial subluxation test. Nonoperative treatment, such as focused physical therapy and patellofemoral stabilizing brace, is often unsuccessful. Primary surgical options include lateral retinacular repair/imbrication or lateral reconstruction. Prevention is key to avoid medial patella subluxation. When considering patellofemoral surgery, important factors include appropriate lateral release indications, consideration of lateral retinacular lengthening vs release, correct MPFL graft placement and tension, and avoiding excessive medialization during tubercle transfer. This review article will analyze patient symptoms, diagnostic exam findings and appropriate treatment options, as well as pearls to avoid this painful clinical entity.
Introduction
Medial patella subluxation is denned as excessive medial patella translation that re-creates a sense of pain, popping or instability. This entity was first described by Hughston and Deese in patients with previous arthroscopic lateral retinacular release (and associated vastus lateralis release)1. The entity is typically iatrogenic, with common causes including a previous lateral release, detachment of the vastus lateralis from the patella, previous medial tibial tubercle transfer, or an overly tight and/or malpositioned medial patella femoral ligament (MPFL) graft. Underlying hyperlaxity, trochlear dysplasia, and deficient vastus lateralis musculature may also play a role in the development of medial patella subluxation. Often a difficult diagnosis, this article reviews cases, clinical evaluation, and treatment options. We will also provide tips and technical pearls to avoid medial patella subluxation in patients with patellofemoral symptoms.
Case Examples
Case 1
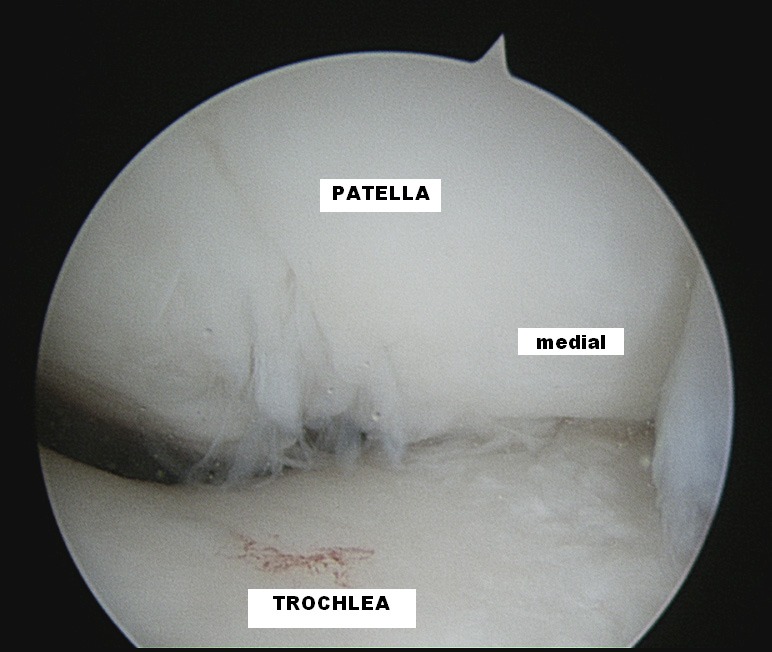
A 39 year old female underwent a lateral retinacular release, tibial tubercle transfer and vastus medialis advancement for patellofemoral instability 2 years prior to presenting to our office. One year prior, she had an MPFL reconstruction and hardware removal. She presented to our office with achy pain at rest and acute episodes of patella shifting and popping. On exam, she had a positive medial subluxation test, medial patella tilt and a tight MPFL graft. A lateral radiograph and MRI were obtained (Figures 1, 2) which showed an anterior and proximally positioned femoral tunnel. After a long discussion, we decided to proceed with revision surgery to address her medial patella subluxation. At the time of arthroscopy, she was found to have a tight medial retinaculum, medial patella tilt, and evidence of medial patellofemoral joint overload (Figure 3). She was treated with a medial retinaculum release, chondroplasty and lateral retinaculum imbrication, which alleviated her symptoms.
Figure 1. Lateral radiograph of Case 1 patient with continued symptoms after MPFL reconstruction. Femoral tunnel placement is anterior and proximal.

Figure 2. Axial MRI of same patient showing anteriorly placed MPFL graft.

Figure 3. Arthroscopic view of Case 1 patient with evidence of medial patellofemoral overload.
Case 2
A 33-year-old woman underwent a tibial tubercle transfer with MPFL allograft reconstruction for patellofemoral instability at an outside institution. She presented to our office with continued pain and instability. She was found to have a positive medial subluxation test, medial patella tracking and tilt, and pain over the medial retinaculum. MRI revealed an anteriorly placed MPFL femoral tunnel (Figure 4). After failing non-operative treatment, she was taken to surgery to address her medial patella subluxation. At the time of arthroscopy, she had medial patella tilt and extensive medial facet cartilage loss. She was treated with medial release and chondroplasty, but eventually required a patellofemoral arthroplasty to achieve pain relief (Figure 5).
Figure 4. Axial MRI of Case 2 patient with anteriorly placed tunnel.
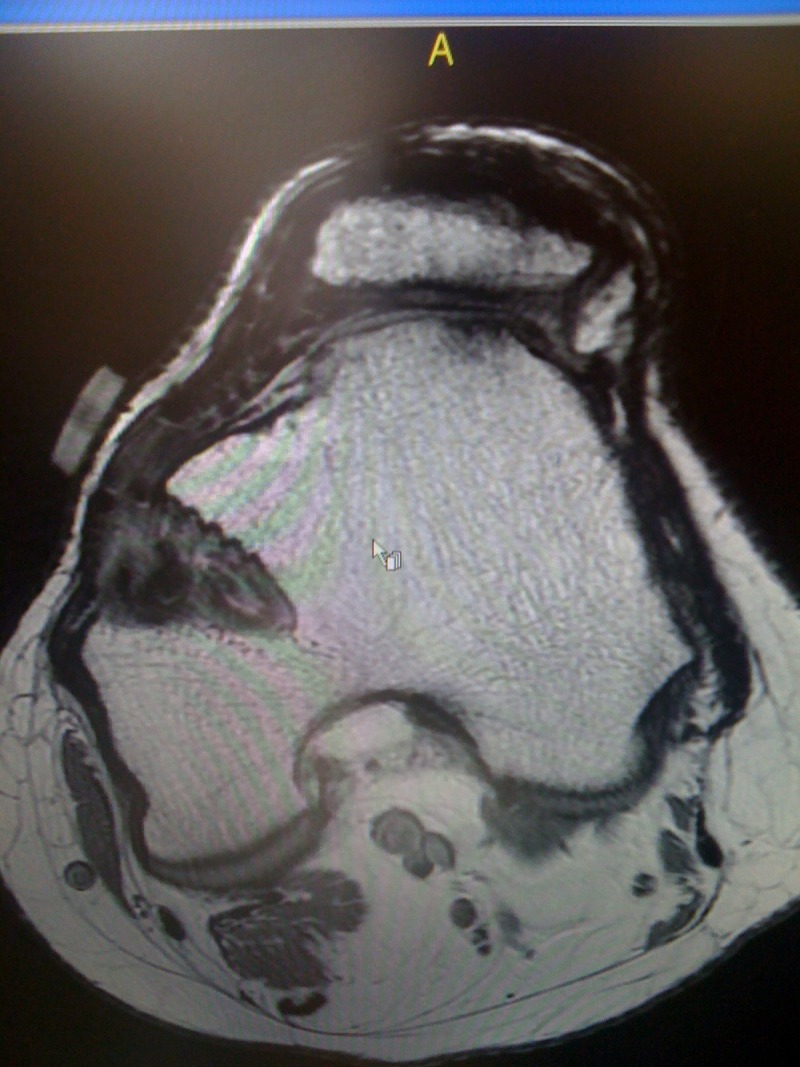
Figure 5. Case 2 patient lateral radiograph status post patellofemoral arthroplasty.

Case 3
A 19-year-old woman with Ehlers-Danlos disease had undergone bilateral lateral retinaculum releases for patellofemoral instability. Due to continued symptoms, she had a left MPFL reconstruction with autograft. A few months later, she presented to our office with medial retinaculum pain and acute episodes of dramatic popping. A lateral radiograph (Figure 6) showed an anteriorly placed MPFL femoral tunnel. She underwent an MPFL graft release, debridement of her medial patella chondral lesion and lateral patella stabilization, and achieved relief of her symptoms.
Figure 6. Case 3 patient lateral radiograph with anteriorly placed MPFL femoral tunnel.

Etiology
Medial patella subluxation is frequently related to previous patellofemoral surgery. Hughston and Deese first reported medial patella subluxation in 54 patients (60 knees) who had worsening symptoms or failure to improve after a lateral retinacular release. Of the 60 knees, 30 developed medial subluxation postoperatively1. 144 of 154 (94%) reported cases of medial patella subluxation were in patients who previously had a lateral reticular release, with or without a tibial tubercle transfer2. Nonweiler and DeLee reported on five cases of medial patellar subluxation after isolated lateral retinacular release3. Bollier, et al, reported five patients having disabling symptoms after malpositioned MPFL grafts, which led to medial subluxation and medial patellofemoral articular overload in three cases4. Less commonly, hyperlaxity, trochlear dysplasia and deficient musculature can lead to medial patella subluxation2,5. Spontaneous medial patellar subluxation is a very rare and limited to case reports5.
Patient History
Patients typically complain of a dramatic, painful patellofemoral popping sensation with certain knee movements. There often is a history of previous patellofemoral surgery. Often, they are worse after surgery and the timing, extent and description of symptoms need to be carefully sorted out. This condition can be quite disabling and can severely limit activities. Patients are apprehensive and avoid activities and knee positions that may reproduce their symptoms or instability. Often, they report that the patella shifts laterally and this condition can easily be mistaken for lateral patellofemoral instability. However, the patella is subluxed medially in full extension. As the knee flexes, the patella jumps laterally into the trochlear groove. Other reported symptoms are anterior knee pain, swelling, “giving away” episodes, and difficult navigating stairs.
Patients are substantially disabled by this condition. Hughston et al, found that 85% of patients were unable to perform light recreational activities, 69% reported severe or disable knee pain and only five of 65 patients could participate in competitive sports6.
Physical Exam
Static medial patella subluxation, notable vastus lateralis atrophy, or a visible and palpable lateral patella void may be observed1. Standard patellofemoral exam should be performed including assessment of patella glide, crepitus, lateral apprehension, tracking, and alignment. Medial patella translation greater than 2 quadrants indicates loss of lateral patellofemoral restraints or underlying hyperlaxity7. Although increased laxity suggests the diagnosis, the key is to reproduce the patient's symptoms or apprehension with the medial patella subluxation test8. With the knee in full extension, the examiner applies a medial translational force to the patella. The knee is then flexed. In the first 30 degrees of knee flexion, pain, instability or dramatic reproduction of the patient's symptoms occurs as the patella snaps laterally into the trochlear groove.
Nonweiler and DeLee described the gravity subluxation test3. The patient is placed in the lateral decubitus position, with the affected leg abducted in the air. Patients are then asked to contract their quadriceps. A positive test is shown by the inability to pull the subluxed patella laterally into the trochlear groove and indicates laxity of the lateral retinaculum and/or detachment of the vastus lateralis from the patella.
Imaging
Standard knee radiographs are obtained, including weight-bearing AP, lateral, notch and Merchant views. Merchant views, obtained to measure the congruence angle, can show static patellar subluxation at a specific knee flexion angle9. Trochlear dysplasia can be assessed on lateral radiographs looking for the “crossing sign10.” The lateral view can also assess for patella alta. Gravity AP radiographs, taken with the leg abducted, have been described as a dynamic picture of the patella during non-contracted and contracted states of the quadriceps3.
MRI has been used to assess the status of medial and lateral soft tissue restraints, the patella cartilage, and to measure tibial tubercle to trochlear groove, or TT-TG, distance. Dynamic MRI has been proposed to better assess patellar instability11-13. However confounding factors (patient position, motion, and muscle firing patterns) can change the position of the patella in various degrees of knee flexion.
Imaging studies are often nonspecific for the diagnosis of medial patella dislocation. This is usually a diagnosis made by history and physical exam.
Nonoperative Management
Physical therapy, specifically vastus lateralis strengthening, or the use of a patellofemoral brace during activities can be tried. Unfortunately, nonoperative management is often unsuccessful. Patients with continued symptoms after 3–6 months of non-operative treatment can be indicated for surgical intervention.
Operative Management
Most techniques involve repairing or reconstructing the lateral patellar stabilizers.
Open Lateral Repair
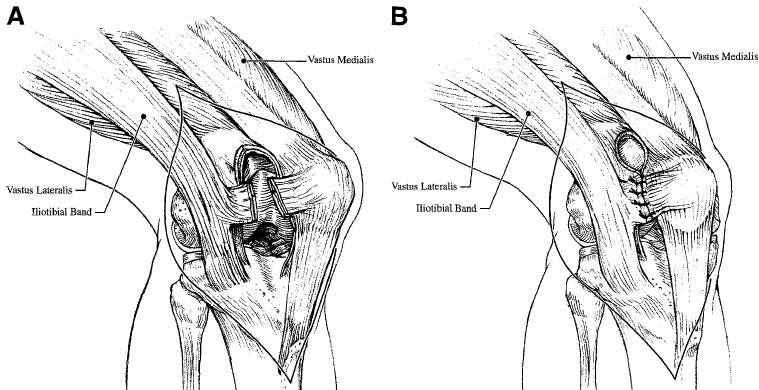
Direct repair of the lateral retinaculum fascia was described by Hughston6 and Brinker14. When good tissue is present, a side-to-side anastomosis technique can be used to reapproximate the tissues (Figure 7). If the vastus lateralis has been released or retracted, it should be mobilized and repaired14. Nonweiler and DeLee reported on 5 patients who had imbrication and vastus lateralis advancement. At an average followup of 3.3 years, four of the five patients had no instability symptoms with negative gravity subluxation tests. Three patients had excellent and two had good results. Heyworth, et al, reported results in 22 patients with previous lateral retinacular releases who underwent open lateral retinacular closure15. Each patient had symptoms of anterolateral pain, a palpable lateral defect and positive medial apprehension test. Average follow up was 3.2 years, with 82% of patients rating their outcome as good or excellent and 14% as fair. Preoperatively, 86% of patients rated themselves as poor. Good tissue is necessary to perform repair or imbrication
Figure 7. Lateral retinaculum direct repair via side to side suture technique. (Reproduced with permission from Brinker M, O'Connor D.P, Flandry F, Hughston J.C. Diagnosis and surgical correction of medial patellar subluxation. Oper Tech Sports; 2001; 9(3): 184–189.).
Open Lateral Reconstruction
When tissue quality is poor or insufficient, reconstruction should be considered. Various techniques have been described, utilizing iliotibial (IT) band, tensor fascia lata or patellar tendon for the reconstruction. Hughston described using an anterior strip of iliotibial band6. With this technique, the surgeon dissects a one centimeter strip of tissue 3–4 cm in length. The distal aspect of the IT band is left attached to the lateral aspect of Gerdy's tubercle. The strip is then used to close the lateral deficit by attachment to the lateral patella (Figure 8). The IT band can be either sewed to the soft tissues or placed through a patellar tunnel.
Figure 8. Depiction of lateral retinaculum reconstruction with iliotibial band graft sutured to lateral patella. (Reproduced with permission from Brinker M, O'Connor D.P, Flandry F, Hughston J.C. Diagnosis and surgical correction of medial patellar subluxation. OperTech Sports; 2001; 9(3): 184–189.).
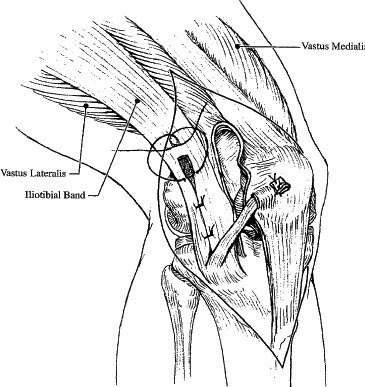
Hughston also described using the patellar tendon to reconstruct the lateral restraints6. The lateral 1/4th of the patella tendon is detached distally from the tibial tubercle and left intact proximally, either with or without a bone block attachment (Figure 9). The patellar tendon can be secured to the tibia through bone tunnels, suture anchors, or with direct suturing to the soft tissues.
Figure 9. Patellar tendon graft used to reconstruct lateral retinaculum, sutured to the tibia at Gerdy's tubercle. (Reproduced with permission from Brinker M, O'Connor D.P, Flandry F, Hughston J.C. Diagnosis and surgical correction of medial patellar subluxation. OperTech Sports; 2001; 9(3): 184–189.).
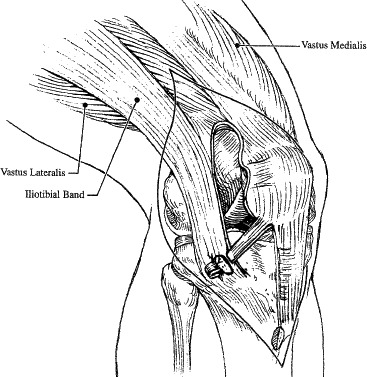
Reconstruction using both IT band and patellar tendon can also be performed6. The IT band graft is rotated toward the patella and patellar tendon rotated toward Gerdy's tubercle. The patella tendon is secured at Gerdy's tubercle and the IT band is fixed to the patella.
Regardless of surgical intervention chosen, the retracted vastus lateralis should be mobilized for transfer, and attached to the patella or quadriceps mechanism6.
Hughston et al evaluated outcomes after lateral reconstruction with the patella tendon6. They reported on 65 knees. At an average follow up of 53.7 months, 44 patients (68%) reported improvement in their functional levels and 49 patients (75%) were subjectively improved. Fifty patients (80%) rated their outcome as good or excellent. A second surgical reconstruction was required in six knees secondary to index surgical failure, re-injury or failure to improve.
Postoperative recommendations for either repair or reconstruction consist of full weight-bearing with a knee immobilizer for 6 weeks14. Quadriceps sets and straight leg raises are allowed the day after surgery. Immediate full knee ROM is allowed when seated.
Arthroscopic Medial Retinacular Release
Arthroscopic medal release has also been described to address medial subluxation of the patella. Shannon et al reported seven patients (nine knees) with history and exam consistent with medial subluxation and all of whom failed an extensive rehabilitation course and a trial of bracing2. A diagnostic arthroscopy was performed on each patient, followed by the medial release using an acromioplasty electrode. The medial retinaculum was divided, beginning at the superior pole of the patella and traverses distally to the anteromedial portal. Once this was done, the authors grasped and tilted the patella laterally 50 to 70 degrees on its lateral edge to ensure any remaining retinacular tissue was divided. Final palpation over the medial undersurface of the patella was done to confirm a complete release. At an average follow up of 2.7 years, all seven patients had alleviation of their symptoms, with 6 excellent and 3 good results. There were no complications or need for further surgical intervention.
Avoidance of Medial Patella Subluxation
The key to avoiding medial patella subluxation is careful attention to initial surgical indications and technique. Lateral release should not be performed as the sole procedure to treat patellofemoral instability. Indications for isolated lateral release include a tight lateral retinaculum and/or lateral facet overload. Lateral release is often performed in conjunction with MPFL reconstruction or tibia tubercle transfer in the setting of patellofemoral instability surgery. In this setting, a lateral release may be indicated when the patella has lateral patella tilt less than neutral.
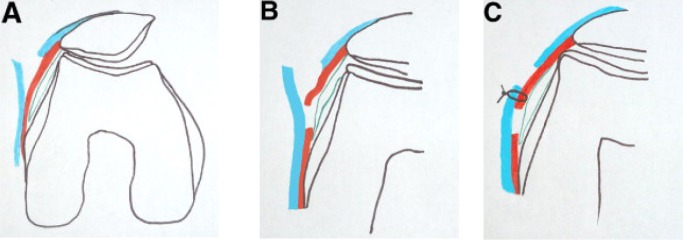
In lieu of a release, surgeons can consider a lateral retinacular lengthening16. In a recent prospective study, 28 patients were randomized to lateral release (14) or lengthening (14)16. The lateral lengthening group was found to have less quadriceps atrophy, less medial instability and improved outcomes at two years compared to the lateral release group. To perform, the superficial and deep retinacular layers are split sequentially and patellar tilt performed. The superficial layer is then sutured to the deep layer under no tension (Figure 10).
Figure 10. Depiction of lateral retinacular lengthening. (Reproduced with permission from Pagenstert G, Wolf N, Bachmann M, Gravius S, Barg A, Hintermann B, Wirtz DC, Valderrabano V, Leumann AG. Arthroscopy. 2012;28(6): 788–797.
MPFL reconstruction is a common procedure to address patellofemoral symptoms. When performing MPFL reconstruction, it is important to have appropriate graft length/ tension, and an anatomic femoral tunnel position. The native MPFL acts as a checkrein during the first 30 degrees of knee flexion, guiding the patella into the trochlear groove. The trochlea then becomes the primary restraint at deeper flexion angles. The MPFL remains isometric from extension to 60 degrees of flexion17. With further flexion, tension declines, with no measureable tension in deep knee flexion18. Appropriate graft placement and tension are keys to avoid medial patella subluxation4. An incision large enough to allow palpation of the MPFL insertion between the medial epicondyle and adductor tubercle is recommended (Figure 11)19. Palpating the adductor magnus tendon can assist in defining surgical anatomy (Figure 12). A suture can be used to connect the proposed femoral insertion site to the patella and isometry can be determined. If the suture tightens in flexion, the proposed femoral attachment site is too anterior or proximal. Finally, lateral fluoroscopic landmarks should be used to confirm accurate guidewire placement (Figure 13). The guidewire should be placed 1 millimeter anterior to the posterior cortical line of the femur, just proximal to Blumensaat's line20 (Figure 14).
Figure 11. Medial knee bony anatomy, shows MPFL attachment on femur. (Reproduced with permission from LaPrade R, Engebretsen A, Ly T, Johansen S, Wentorf F, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am 2007;89:2000–2010).
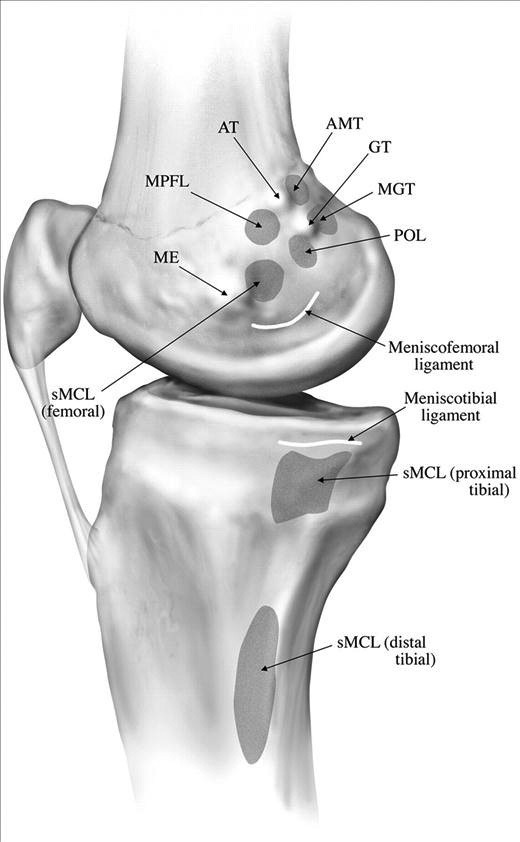
Figure 12. Medial knee soft tissue anatomy, shows MPFL course from patella to femoral attachment. (Reproduced with permission from LaPrade R, Engebretsen A, Ly T, Johansen S, Wentorf F, Enge-bretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am 2007;89:2000–2010).
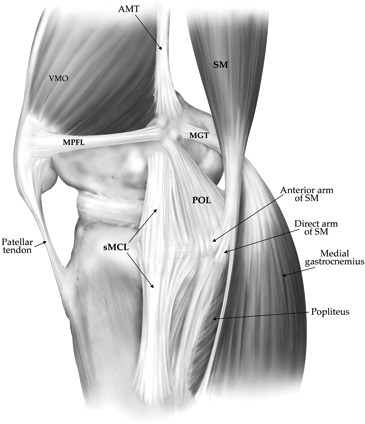
Figure 13. Lateral radiograph showing anterior and proximal MPFL graft Blue dot signifies correct radiographic location for guidewire placement.
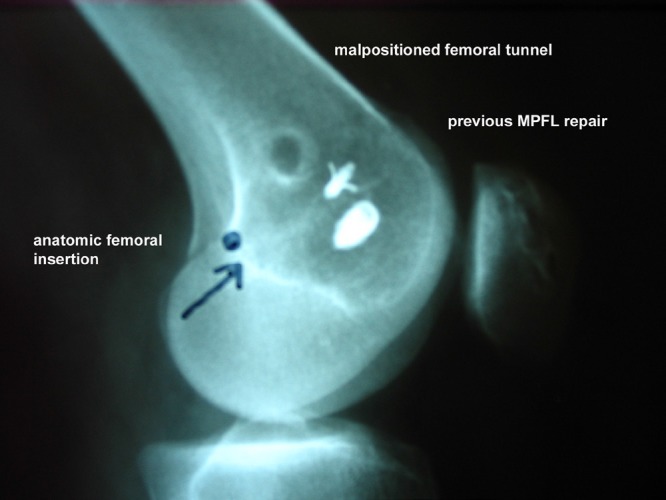
Figure 14. Lateral fluoroscopic view depicting correct guidewire placement in preparation for MPFL femoral tunnel.

When tensioning the graft, the surgeon can flex the knee 45–60 degrees so that the patella is centered in the trochlea. Another option is to hold the patella flush with the lateral trochlea with the knee flexed to 30 degrees during final graft fixation. Either way, the end result should have some lateral patella translation with the knee extended and solid endpoint. The patella should pull into the groove when the knee is flexed.
Tibial tubercle transfer is another common operative treatment for patellofemoral symptoms. However, in patients with lateral malalignment and medial patella chondral lesions, caution should be taken to avoid over-medialization of the patella. Normal TT-TG is 10 mm21. If the measured pre-operative TT-TG distance is 20 mm, then tubercle transfer should be limited to 10 mm22. This will help avoid over medialization and the potential for develop of medial patella subluxation.
Conclusion
Medial patella subluxation should be considered in any patient with patellofemoral pain, popping, or instability who has had previous patellofemoral surgery or lateral retinacular release. The diagnosis is clinical and, while a constellation of signs and symptoms are typical, the medial patella subluxation test is diagnostic. Unfortunately, non-operative treatment is usually unsuccessful. Operative options include lateral retinacular repair or imbrication and lateral reconstruction. Operative intervention can yield good outcomes in most patients. Awareness of this relatively rare entity can lead to not only earlier intervention but also decrease the incidence through careful surgical indications, procedures and techniques employed.
References
- 1.Hughston JC, Deese M. Medial subluxation of the patella as a complication of lateral retinacular release. Am J Sports Med. 1988;16(4):383–8. doi: 10.1177/036354658801600413. [DOI] [PubMed] [Google Scholar]
- 2.Shannon BD, Keene JS. Results of arthroscopic medial retinacular release for treatment of medial subluxation of the patella. Am J Sports Med. 2007;35(7):1180–7. doi: 10.1177/0363546507299445. [DOI] [PubMed] [Google Scholar]
- 3.Nonweiler DE, DeLee JC. The diagnosis and treatment of medial subluxation of the patella after lateral retinacular release. Am J Sports Med. 1994;22(5):680–6. doi: 10.1177/036354659402200517. [DOI] [PubMed] [Google Scholar]
- 4.Bollier M, Fulkerson J, Cosgarea A, Tanaka M. Technical failure of medial patellofemoral ligament reconstruction. Arthroscopy. 2011;27(8):1153–9. doi: 10.1016/j.arthro.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 5.Aksahin E, Yumrukcal F, Yuksel HY, Dogruyol D, Celebi L. Role of pathophysiology of patellofemoral instability in the treatment of spontaneous medial patellofemoral subluxation: a case report. J Med Case Rep. 2010;4:148. doi: 10.1186/1752-1947-4-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hughston JC, Flandry F, Brinker MR, Terry GC, Mills JC., 3rd Surgical correction of medial subluxation of the patella. Am J Sports Med. 1996;24(4):486–91. doi: 10.1177/036354659602400413. [DOI] [PubMed] [Google Scholar]
- 7.Dye SF. The knee as a biologic transmission with an envelope of function: A theroy. Clin Orthop. 1996;325:10–18. doi: 10.1097/00003086-199604000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Fulkerson JP. A clinical test for medial patella tracking. Tech Orthop. 1997;12:144. [Google Scholar]
- 9.Beaconsfield T, Pintore E, Maffulli N, Petri GJ. Radiological measurements in patellofemoral disorders. A review. Clin Orthop RelatRes. 1994.;(308):18–28. [PubMed] [Google Scholar]
- 10.Dejour H, Walch G, Nove-Josserand L, et al. Factor of patellar instability: An anatomic radiographic study. Knee Surg Traumatol Arthrosc. 1994;2:19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 11.Shellock FG, Mink JH, Deutsch AL, Fox JM. Patellar tracking abnormalities: clinical experience with kinematic MR imaging in 130 patients. Radiology. 1989;172(3):799–804. doi: 10.1148/radiology.172.3.2772191. [DOI] [PubMed] [Google Scholar]
- 12.Shellock FG, Mink JH, Deutsch A, Fox JM, Ferkel RD. Evaluation of patients with persistent symptoms after lateral retinacular release by kinematic magnetic resonance imaging of the patellofemoral joint. Arthroscopy. 1990;6(3):226–34. doi: 10.1016/0749-8063(90)90079-s. [DOI] [PubMed] [Google Scholar]
- 13.Duchman K, Mellecker C, Thedens DR, Albright JP. Quantifying the effects of exensor mechanism medialization procedures using MRI: a cadaver-based study. [PMC free article] [PubMed] [Google Scholar]
- 14.Brinker MR, O'Connor DP, Flandry F, Hughston JC. Diagnosis and Surgical Correction of Medial patellar subluxation. 2001 [Google Scholar]
- 15.Heyworth BE, Carroll KM, Dawson CK, Gill TJ. Open lateral retinacular closure surgery for treatment of anterolateral knee pain and disability after arthroscopic lateral retinacular release. Am J Sports Med. 2012;40(2):376–82. doi: 10.1177/0363546511428600. [DOI] [PubMed] [Google Scholar]
- 16.Pagenstert G, Wolf N, Bachmann M, Gravius S, Barg A, Hintermann B, Wirtz DC, Valderrabano V, Leumann AG. Open lateral patellar retinacular lengthening versus open retinacular release in lateral patellar hypercompression syndrome: a prospective double-blinded comparative study on complications and outcome. Arthroscopy. 2012;28(6):788–97. doi: 10.1016/j.arthro.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Smirk C, Morris H. The anatomy and reconstruction of the medial patellofemoral ligament. Knee. 2003;10(3):221–7. doi: 10.1016/s0968-0160(03)00038-3. [DOI] [PubMed] [Google Scholar]
- 18.Elias JJ, Cosgarea AJ. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med. 2006;34(9):1478–85. doi: 10.1177/0363546506287486. [DOI] [PubMed] [Google Scholar]
- 19.LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. JBone Joint Surg Am. 2000–10, 2007;89(9) doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 20.Schottle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–4. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 21.Saranathan A, Kirkpatrick MS, Mani S, Smith LG, Cosgarea AJ, Tan JS, Elias JJ. The effect of tibial tuberosity realignment procedures on the patellofemoral pressure distribution. Knee Surg Sports Traumatol Arthrosc. 2012;20(10):2054–61. doi: 10.1007/s00167-011-1802-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fulkerson JP. Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop. 1983;177:176–181. [PubMed] [Google Scholar]


