Summary
Background
Gene therapy has the potential to reverse disease or prevent further deterioration of vision in patients with incurable inherited retinal degeneration. We therefore did a phase 1 trial to assess the effect of gene therapy on retinal and visual function in children and adults with Leber’s congenital amaurosis.
Methods
We assessed the retinal and visual function in 12 patients (aged 8–44 years) with RPE65-associated Leber’s congenital amaurosis given one subretinal injection of adeno-associated virus (AAV) containing a gene encoding a protein needed for the isomerohydrolase activity of the retinal pigment epithelium (AAV2-hRPE65v2) in the worst eye at low (1·5×1010 vector genomes), medium (4·8×1010 vector genomes), or high dose (1·5×1011 vector genomes) for up to 2 years.
Findings
AAV2-hRPE65v2 was well tolerated and all patients showed sustained improvement in subjective and objective measurements of vision (ie, dark adaptometry, pupillometry, electroretinography, nystagmus, and ambulatory behaviour). Patients had at least a 2 log unit increase in pupillary light responses, and an 8-year-old child had nearly the same level of light sensitivity as that in age-matched normal-sighted individuals. The greatest improvement was noted in children, all of whom gained ambulatory vision. The study is registered with ClinicalTrials.gov, number NCT00516477.
Interpretation
The safety, extent, and stability of improvement in vision in all patients support the use of AAV-mediated gene therapy for treatment of inherited retinal diseases, with early intervention resulting in the best potential gain.
Funding
Center for Cellular and Molecular Therapeutics at the Children’s Hospital of Philadelphia, Foundation Fighting Blindness, Telethon, Research to Prevent Blindness, F M Kirby Foundation, Mackall Foundation Trust, Regione Campania Convenzione, European Union, Associazione Italiana Amaurosi Congenita di Leber, Fund for Scientific Research, Fund for Research in Ophthalmology, and National Center for Research Resources.
Introduction
One of the most severe forms of inherited retinal degeneration is Leber’s congenital amaurosis, which is a group of diseases that are caused by mutations in any of 13 genes. Patients with Leber’s congenital amaurosis have severe loss of vision and abnormal eye movements (nystagmus) in early infancy and childhood. Diminished pupillary light reflexes and flat or nearly undetectable responses during electroretinography confirm the clinical diagnosis.1–4 Type 2 Leber’s congenital amaurosis, caused by mutations in a gene that encodes a protein needed for the isomerohydrolase activity of the retinal pigment epithelium (RPE65), accounts for about 6% of cases.5 There is no treatment for Leber’s congenital amaurosis and severe visual impairment during childhood usually progresses to total blindness by the third or fourth decade of life.4 Clues for how to treat type 2 disease came from studies in which mutations in RPE65 resulted in substantially diminished amounts of 11-cis retinal.6–9
Replication-deficient adeno-associated virus (AAV)-mediated delivery of the wildtype RPE65 cDNA to the RPE in animal models of Leber’s congenital amaurosis resulted in rapid development of retinal and visual function through the enzyme-mediated generation of 11-cis retinal.10 Furthermore, the success rate for recovery and magnitude of improvement was related to the age at treatment, with best results obtained in young animals before widespread cellular degene ration.11,12 This result and additional findings for safety and efficacy13 provided the basis for a phase 1 trial of gene augmentation therapy in individuals with RPE65-associated Leber’s congenital amaurosis, and for the inclusion of children who might get the most benefit from the intervention.14 AAV-mediated RPE65 therapy in young adults15–20 resulted in most individuals reporting a perception of increased brightness in the injected eye after treatment, as judged with various methods, including dark adaptometry, perimetry, and pupillary light reflexes.15–18 Two individuals in two studies15,16 showed improvements in ambulation. Significant improvements in visual acuity in all three individuals were reported in one study.15
Here we present the results from the complete phase 1 dose-escalation study done at the Children’s Hospital of Philadelphia (CHOP, PA, USA) with the aim to assess the safety and efficacy of AAV2-hRPE65v2.15 We also assessed the role of an individual’s age (or stage of disease progression) on the extent of reversal of blindness.
Methods
Patients
Inclusion and exclusion criteria for patients are reported by Maguire and colleagues.15 12 patients (aged 8–44 years) with RPE65-associated Leber’s congenital amaurosis were enrolled and consecutively treated, with an interval of at least 6 weeks between individuals (table). All surgery was done at CHOP and follow-up tests were done at CHOP or Seconda Università degli Studi di Napoli (Naples, Italy) for the Italian patients (webappendix pp 1–2 and 6–8). 20 age-matched normal-sighted male and female individuals were assessed for pupillary light reflexes.
Table.
Summary of patient demographics and nystagmus
| Low dose | Medium dose | High dose | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NP01 | NP02 | NP03 | NP04 | CH06* | CH08 | CH09 | CH10 | CH11 | CH12 | CH13 | NP15 | |
| Date at administration | Oct 11, 2007 |
Dec 13, 2007 |
Jan 24, 2008 |
April 10, 2008 |
May 22, 2008 |
July 10, 2008 | Sept 25, 2008 | Nov 18, 2008 | Dec 30, 2008 |
March 5, 2009 |
April 16, 2009 |
June 2, 2009 |
| Age (years) | 26 | 26 | 19 | 17 | 20 | 9 | 8 | 10 | 24 | 44 | 35 | 11 |
| Sex | Female | Male | Female | Male | Female | Male | Male | Male | Female | Female | Male | Male |
| RPE65 mutations | E102K/ E102K |
E102K/ E102K |
R234X/ R234X |
R91W/ T149N |
IVS1+5g>a/ L341S |
F530fs/F530fs | R124X/ Lys297del1aggA |
IVS1+5g>a/ Phe530del1ttc |
V473D/ V473D |
K303X/ W431C |
IVS1+5g>a/ IVS1+5g>a |
D167W/ H313R |
| Injected eye† | Right | Right | Right | Left | Right | Right | Left | Right | Right | Right | Right | Right |
| Nystagmus frequency before and 90 days after gene therapy (Hz) |
3·8/2·0 | 2·3/2·1 | 4·2/3·0 | 1·0/0 | 1·1/1·3 | 3·7/2·0 | 2·5/2·0 | 4·0/2·0 | 0·5/0·5 | 1·0/0·25 | 0·3/0·4 | 0·4/0·4 |
Also heterozygous for RDH12 S203R.
Eye with worst sight selected for surgery.
This study was approved by a national ethics committee in Italy. Patients from Italy provided written informed consent (if ≥18 years) or written assent and parental permission (if <18 years) at two study sites—the Referral Centre of Hereditary Retinopathies, Department of Ophthalmology, Seconda Università degli Studi di Napoli, and Foundation Fighting Blindness CHOP-University of Pennsylvania (CHOP-PENN) Pediatric Center for Retinal Degenerations (Philadelphia, PA, USA). The other patients provided written informed consent (or assent) only at the Foundation Fighting Blindness CHOP-PENN Pediatric Center for Retinal Degenerations. All patients appearing in webvideos provided written media consents or assents.
Vector and surgical delivery
The transgene cassette in the AAV2-hRPE65v2 vector had a chicken β-actin promoter for expression of the human RPE65 cDNA with an optimised Kozak sequence.21 The Center for Cellular and Molecular Therapeutics at CHOP manufactured the vector using good manufacturing practices (webappendix p 2).13,15
For each patient, we selected the eye with the worst function for treatment with AAV2-hRPE65v2.13,15 We did a standard three-port pars plana vitrectomy, with removal of the posterior cortical vitreous, as described by Maguire and colleagues.15 Patients in the low-dose cohort were injected with 1·5×1010 vector genomes (1·0×108 per µL) and those in the medium-dose with 4·8×1010 vector genomes (3·2×108 per µL) of AAV2-hRPE65v2 in a volume of 150 µL into the subretinal space (table). Patients in the high-dose cohort were injected with 1·5×1011 vector genomes (5·0×108 per µL) in 300 µL (table) after the focal area was buttressed from hydrodynamic stress during injection with perfluorooctane liquid (Perfluoron, Alcon, Fort Worth, TX, USA), which is heavier than water. The liquid was aspirated after the AAV2-hRPE65v2 had been delivered.
Assessment of safety and efficacy
Patients were assessed before and at designated timepoints after surgery as described (webappendix p 6–8).13,15 For each individual, efficacy was monitored with objective and subjective measurements of the changes in vision.15 The response duration was measured from 3 months to 2 years. Additional details are provided in the webappendix (pp 1–8).
The study is registered with ClinicalTrials.gov, number NCT00516477.
Role of the funding source
The main sponsor of the study and personnel working for the sponsor were involved in study design, data gathering, analysis, and interpretations, and writing of the report. None of the other funding sources had any direct role with respect to the design or execution of the study, data gathering, analysis, interpretation, or writing of the report. The corresponding author had full access to all data throughout the study and had final responsibility for submission for publication.
Results
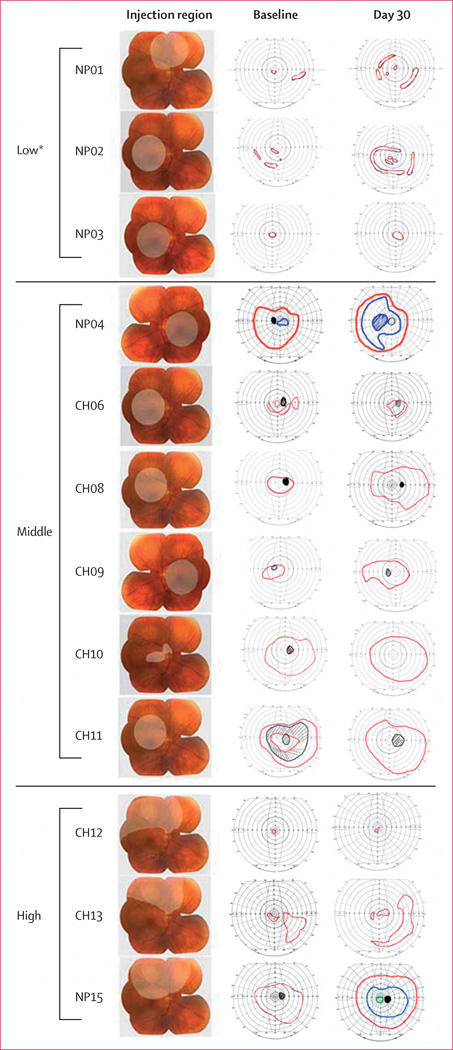
Maguire and colleagues15 have described the short-term results from the first three patients (NP01, NP02, and NP03 in the low-dose cohort). The vector was injected into the macula in nine patients, but not in three patients (NP01,15 CH12, CH13) with substantial atrophy in this region. About half the macula was exposed in patient NP15 (figure 1). An epiretinal membrane that was noted during baseline studies in the injected eye of patient CH10 was removed before injection. A foveal dehiscence was noted at the time of injection in this individual as some of the vector escaped from the foveal defect, reducing the total volume in the subretinal space by about 70% and resulting in the exposure of a third of the macula (figure 1).
Figure 1. Area of retina exposed to adeno-associated virus-mediated delivery of wild-type retinal pigment epithelium (AAV2-hRPE65v2).
Column 1 was drawn over composite photographs of a normal retina, and columns 2 and 3 over the baseline and follow-up Goldmann visual fields, respectively, in the injected eyes. All follow-up visual fields are shown at day 30, except for patients NP01 (4·75 months) and NP02 (2·75 months). Stimuli used to measure Goldmann visual fields were V4e (red) and II4e (blue). Scotomas and the natural blind spot are shown in black. *Visual field data from these patients were reported previously1 but are presented here for completeness.
All of the retinal detachments had resolved by the next assessment (within 14 h after surgery); and foveal abnormalities were noted in only one patient (NP02), as noted previously,15 with optical coherence tomography. The foveal dehiscence in patient CH10 had completely resolved with no evidence of a macular hole after surgery at the first assessment with optical coherence tomography on day 8 (webappendix p 22). With the exception of pigment atrophy at the lower border of the original detachment site in patient NP15, all the other postoperative retinal assessments were unremarkable.
None of the patients had serious adverse events, and the vector was found in samples of tears and blood only transiently after surgery (webappendix pp 9–10). Exposure to subretinal AAV at the doses used did not lead to a harmful immune response (webappendix p 11–16).
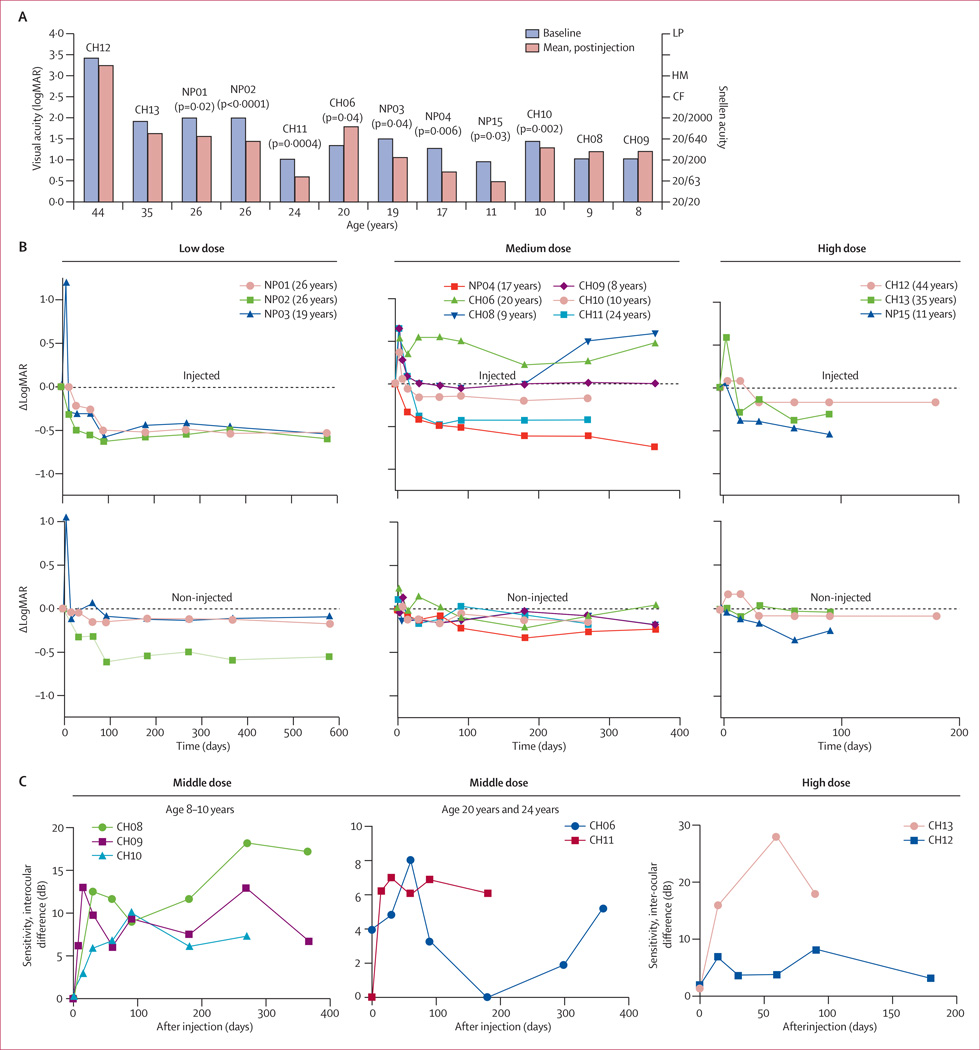
All 12 individuals reported improved vision in dimly lit environments in the injected eyes starting 2 weeks after surgery. Improvements in visual acuity were substantial and stable in the three patients given the vector at a low dose,15,20 three given the middle dose (NP04, CH10, and CH11), and one administered the high dose (NP15). Visual acuity worsened in one patient (CH06; figure 2; webappendix p 18 and pp 23–24). For the other individuals, no substantial gains or losses in visual acuity were noted in the injected or non-injected eyes (webappendix pp 23–24). The improvement was not associated with age; however the baseline visual acuity was higher in children than in adults (p=0·04; webappendix p 17).
Figure 2. Visual acuity and full-field sensitivity and dark adaptometry changes after injection with adeno-associated virus-mediated delivery of wild-type retinal pigment epithelium (AAV2-hRPE65v2).
(A) Correlation of age with visual acuity in the injected eye. Visual acuity at baseline was compared with the mean visual acuity after injection (all timepoints included); a worsened visual acuity was noted in CH06. p values for Significant differences are reported. (B) Change in logarithm of the minimum angle of resolution (LogMAR) scores in the injected and contralateral non-injected eyes is indicated as a function of time for patients given low, medium, and high doses of vector. LogMAR score was normalised to 0 at baseline for each individual. (C) Most patients in the middle and high dose groups were tested for full-field sensitivity to white light before and after injection. LP=light perception. HM=hand motion. CF=counting fingers.
There was no clearcut dose effect with respect to improvements in visual acuity in the injected or non-injected eyes. Figure 2B shows that, with the exception of CH06, visual acuities improved or remained stable. Although the visual acuity of the injected eye in patient CH08 might have worsened at the most recent visits, further results will be needed from tests done on the designated days (webappendix pp 6–8) to find out whether this change is Significant.
We noted an improvement in the visual field of all 12 patients (figure 1). Although visual-field tests in patients with severe impairment show substantial variability,22,23 the enlargements exceeded the variation in the contralateral non-injected eye (figure 1).
The extent of improvement in visual fields in the injected eyes correlated with the amount of salvageable retina that was targeted, effects of immediate postoperative head-positioning on the borders of the detachment, and map of the visual field at baseline (figure 1). For example, the visual fields improved substantially in patients CH08, CH09, and CH10, given injections to regions that had initially had restricted function but had viable retina as noted with ophthalmoscopy and optical coherence tomography. Further, if the injection covered regions of healthy retina that had previously had scotomas, the visual field increased as the scotomas were obliterated (eg, CH11; figure 1). Nevertheless, the postinjection visual fields often expanded in regions larger than the region targeted during surgery (eg, CH10, NP15; figure 1). Although the volume injected was larger (300 µL vs 150 µL), covering a large part of the retina, the fields did not improve as much in older individuals (>19 years—eg, patients CH12 and CH13) as they did in younger individuals (≤19 years—eg, patients CH08, CH09, and NP15). This difference is probably caused by the loss of viable photoreceptors with advanced disease in older individuals.
Most individuals given middle and high doses were tested for full-field sensitivity to white light before and after injection; NP04 and NP15 were not tested because the equipment was not available. All individuals had bilaterally diminished full-field sensitivity at baseline. After injection, a large interocular difference (ie, difference in sensitivity between injected and non-injected eyes) in full-field sensitivity was noted in five (CH08, CH09, CH10, CH11, and CH13) of seven individuals when we used stringent criteria to assess the response (3 SDs from the average of the interocular difference in normal-sighted individuals; figure 2C). Only the injected eyes showed improved sensitivity (figure 2C). Improvements in full-field sensitivity were especially noteworthy in the youngest patients, who gained several log units of sensitivity.
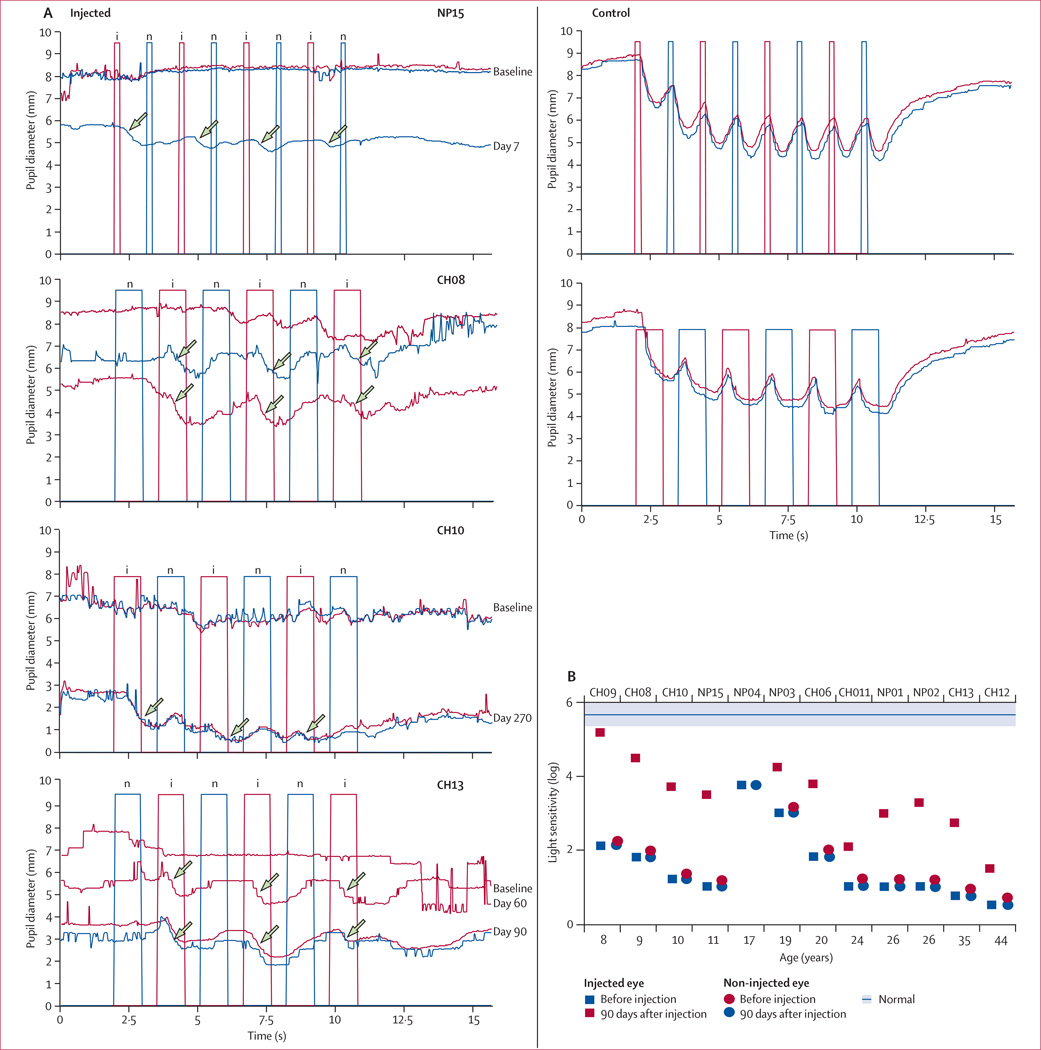
Pupillary responses improved in the injected eyes of all 11 individuals tested. Figure 3 shows the representative responses from patients given the middle and high doses of AAV2-hRPE65v2 (including children and an adult). The pupil diameter (for the largest of the two pupils) immediately before the first exposure to light for patient CH08 was 8·6 mm at baseline, 7·8 mm at day 14, 8·55 mm at day 365; CH10, 8·0 mm at baseline, 9·1 mm at day 270; CH13, 7·8 mm at baseline, 5·6 mm at day 60, 5·6 mm at day 90; and NP15, 8·0 mm at baseline, and 8·3 mm at day 7. Improved responses were detectable as early as day 7 after injection (in patient NP15) and were present even in the eye that was not injected with the entire subretinal dose because the patient (CH10) had a foveal dehiscence. When the injected eye was illuminated with light, both pupils constricted; when the control, non-injected eye was illuminated with light, minimum constriction of the pupil was seen (figure 3). Analyses of the variables of the pupillary light response showed substantial differences between the injected and control eyes in the amplitude and velocity of constriction (webappendix p 19).
Figure 3. Objective evidence of improvement in pupillary light reflexes.
(A) Improved pupillary light reflexes—as a function of time after injection and after alternating stimulation of the injected (i, red columns) and non-injected (n, blue columns) eyes—are shown in representative recordings from patients after injection of middle and high doses of the vector. Red and blue curves represent diameters of the right and left pupils, respectively; however, only one pupil is shown for patient NP15 (day 7 after surgery) because the other was atropinised. Recorded light intensity was 0·04 lux for patients NP15 and CH08, 0·4 lux for CH10, and 10·0 lux for CH13. Days after injection are indicated. Alternating stimuli were presented 2 s after recording was initiated. In the panel for patient NP15, each stimulus was presented in 200 ms with 1 s spaces between the flashes. In the panels for patients CH08, CH10, and CH13, stimuli were presented in 1 s with 600 ms spaces between the flashes. Traces in each panel are shifted vertically to compare responses obtained at different timepoints. Control pupillary light responses (actual pupil diameters) measured in normal-sighted individuals at 4 lux are shown for comparison. (B) Correlation of improvements in full-field sensitivity with age (and baseline retinal sensitivity). The light sensitivities are not shown for patient NP15 because his data were analysed at day 60. The intensity at which the pupillary light response was eliminated from the test eye before injection and at which the relative afferent pupillary defect developed after injection was identified as the lower limit of sensitivity. The mean and SD of sensitivity of normal-sighted individuals in the age range of the patients is indicated by a blue line and shading, respectively.
Baseline tests showed that the pupillary light responses in individuals with type 2 Leber’s congenital amaurosis were much less sensitive than those reported in unaffected individuals (controls; figure 3). Baseline responses to a dim stimulus (<0·04 lux) after a 40-min dark adaptation in patients given low, middle, and high doses of the vector were negligible (figure 3).
The responsiveness to light of the injected eye was consistently greater than that of the contralateral non-injected eye in patients after injection of AAV2-hRPE65v2. For CH08, for example (figure 3A), when a dim stimulus (0·04 lux for 200 ms) was initially delivered to the injected eye at baseline, minimum response was noted in either eye. After injection, the eye responded vigorously. Repetition of the pattern of the relative afferent pupillary defect was noted with successive alternating flashes up to the latest timepoint (eg, from day 14 and to day 365 for CH08, day 270 for CH10, and day 90 for CH13 (figure 3A), showing that the pupillary light responses were happening in the injected eye, while the non-injected eye remained defective.
Significant differences were noted in amplitudes and velocities between the injected eyes versus non-treated eyes in most individuals; the exception was patient CH11 (webappendix p 19). The differences persisted throughout the follow-up with different intensities of light. Although, little difference was noted in response between patient NP04’s injected and non-injected eyes, stimulation with light at 0·04 lux resulted in a Significant difference in velocity between the injected and control eyes (p=0·003; webappendix p 19). Every individual had at least a 2 log unit increase in pupillary-light-response sensitivity in the injected eye. An 8-year-old patient (CH09) had nearly the same (high) level of light sensitivity as did normal-sighted individuals.
The final level of sensitivity in all patients after injection correlated with age (Spearman correlation coefficient (r) −0·80, p=0·002) and baseline sensitivity (0·50, p=0·09; figure 3B). In the analysis of correlation between age and the successive reductions from baseline in light intensity, r was −0·61 (p=0·03), suggesting that young individuals are more likely to have step changes in light intensity in the eye injected with AAV2-hRPE65v2. Such changes were not noted in the contralateral non-injected eye. The average change in light sensitivity in the injected eyes was about 2·2 log units in individuals aged 8–11 years (highest change was noted in patient CH09 [3·8 log units]), and about 1·2 log units in those aged 19–44 years (p=0·04 for difference in light sensitivity).
Full-field scotopic and photopic electroretinographic responses were flat in all individuals before and after injection even with the use of fast Fourier analysis.24 However, multifocal electroretinography could be done in two patients after injection as a result of a reduction in nystagmus. Because of nystagmus, multifocal electroretinography could only be done at baseline for patient NP15. By contrast, results suggested photopic responses in one part of the injected retina at day 30 and then in several other parts at day 60 (webappendix p 25–26) and day 90 (data not shown). Similarly, tests done after subretinal injection in patient NP04 suggested waveforms in the left part of the retina (figure 1) but not in the contralateral (non-injected) retina (figure 3). Similar results were noted in the injected retina of patient CH09 at day 365 (data not shown) although the results of the contralateral non-injected eye were not recorded.
Nystagmus results for patients given low-dose gene therapy are presented elsewhere.20 When patients were tested for their ability to navigate a standardised obstacle course before administration of AAV2-hRPE65v2, 11 of 12 had great difficulty, especially in dim light, as assessed by the number of errors and time taken. Patient NP04 was not tested at low-light levels. After injection, four children (CH08, CH09, CH10, and NP15) given AAV2-hRPE65v2 had substantial improvement in their ambulation when tested with only the injected eye covered (webappendix pp 20–21 and p 27; webvideos 1–6). They were unable to navigate the course accurately when only their non-injected eye was not covered. These patients could also navigate the course with fewer errors and often more quickly than at baseline with their injected eyes not covered (webappendix p 20–21 and p27; webvideos 1–6).
Discussion
All 12 patients given AAV2-hRPE65v2 in one eye showed improvement in retinal function. The effect was stable during follow-up. The results support our hypothesis that the response to subretinal gene therapy depends on the extent of retinal degeneration and, therefore, the age of the patient.14
Assessment of global retinal function showed clinically meaningful vision in patients. The most noteworthy result was the ability of children to navigate an obstacle course independently and accurately, even in dim light. Objective tests provided quantitative evidence for the improved retinal function and sensitivity in these and other individuals. Pupillometry, a sensitive and robust test that provides quantitative information about the response of the entire retina to light, showed a strong miotic response after illumination of the injected eye (but not the control eye). The improvements in the pupillary responses were easily assessed through measurement of the amplitude and velocity of constriction.25,26 There was a stronger pupillary light reflex after illumination of the injected eye when compared with the non-injected eye (ie, an acquired relative afferent pupillary defect or Marcus Gunn pupil) as early as 7 days after injection (patient NP15). The gain in light sensitivity in the injected eye was up to 4 log units. Objective measurement of eye movements showed a reduction in nystagmus in most patients after injection of the gene vector. Suppression of nystagmus indicates improvement in fixation—ie, the ability of the eye to maintain alignment with an object.27 Most subretinal injections targeted the macula, and by contrast with a patient in another study,28 there was no change in fixation (or increase in amplitude of nystagmus). Because of the improvement in nystagmus in our patients, we were able to do multifocal electroretinography in three individuals after injection; a signal was seen in the electroretinographs of all of these patients. Improvement was not seen with full-field flash electroretinography because the total area of the treatment zones in all patients was too small to generate a gross electrical response.
Results of subjective tests corroborated the improvements noted with those of objective tests. Visual behaviour in the children—as assessed by the ability to walk—showed substantial improvements after treatment (webvideos 1–6). Six individuals had substantial improvements in standard tests of visual acuity or visual fields that could alter their designation as legally blind. We could not find a correlation with dose, baseline vision, or other variables with improvement in visual acuity after treatment. Ultimately, patients may not be able to attain normal acuity (eg, 20/20) because of the amblyopic effect of congenital nystagmus that prevents high-resolution central vision as a result of image blur from unsteady fixation. Although central vision is important for normal activities of daily living, visual acuity represents only a small proportion of total retinal and visual function, so the other features of vision might benefit when patients are treated with retinal gene therapy.
Increases in the size of the visual fields in the injected eyes roughly correlated with the area of the retina covered by the injected genome vector. A greater than predicted increase in the size of the visual field, however, probably resulted from immediate postoperative positioning of the patient.15 Small shifts in the original retinal detachment in the immediate postoperative period might have contributed to the enlargement of the visual fields in individuals with viable retinal cells. Such shifts in the patients with extensive degeneration were unlikely to expand the visual fields. Diffusion of the vector into other parts of the retina did not seem to contribute to the enlargement of the visual fields as these other parts might have previously undergone complete degeneration. This hypothesis is substantiated by the finding that the retinas of older patients had widespread degeneration and improved less.
The injected eyes were more sensitive to light than were the non-injected eyes, which showed no change, during full-field sensitivity testing. The light stimulus in this test is projected externally rather than directed at selected areas of the retina by focal laser, as in microperimetry.17,19,28 Although full-field tests and pupillometry show improvements in only the vector-injected retinas, a mild bilateral improvement of visual function (eg, visual acuity) was noted in many patients. Although the underlying mechanisms remain to be elucidated, three potential explanations are that, like microperimetry, full-field tests are subjective, and the results might improve because of patient learning effect; an improvement in nystagmus after injection of one eye could result in improved resolution of the other eye;15,20 and changes in how the visual signal is processed (central nervous system plasticity) might affect the visual outcome in the non-injected eye after administration of gene therapy to just one eye. Thus bilateral simultaneous or immediately consecutive treatment of both eyes might have a synergistic effect.
Overall, the results of objective and subjective tests support our hypothesis that the greatest improvement in visual function with subretinal gene therapy will occur in young individuals. Although young patients had better visual function at baseline than did older individuals, they also had the greatest overall improvement in vision.
Subretinal gene therapy seemed safe at all administered doses. Treatment with the vector did not elicit local or systemic adverse events. The foveal dehiscence that was apparent during subretinal injection in a patient resolved immediately after surgery and did not seem to be related to the investigational product. We subsequently modified the procedure so that hydrodynamic stress, and therefore the likelihood of, foveal dehiscence, or development of a macular hole was kept to a minimum. We did not note any signs of inflammation or acute retinal toxicity after injection. However, the presence of PCR-detectable (but non-quantifiable) vector in blood after injection in two patients with widespread retinal degeneration suggests that transient systemic exposure can occur after administration of a high dose or in individuals with widespread outer retinal atrophy. In future studies, we do not plan to use doses higher than 1·5×1011 vector genomes per injection in case we have reached the dose ceiling in terms of potential toxicity.
The clinical benefits of subretinal gene therapy were sustained at the 2-year follow-up. The visual recovery noted in the children confirms the hypothesis that efficacy will be improved if treatment is applied before retinal degeneration has progressed. Assessment of whether the treatment alters the natural progression of the retinal degeneration will be possible in follow-up studies.
The success of this gene therapy study in children provides the foundation for gene therapy approaches to the treatment of other forms of Leber’s congenital amaurosis and of additional early onset retinal diseases.
Supplementary Material
Acknowledgments
The CHOP, a non-profit entity with a mission to develop novel therapeutics for inherited disorders, was the main source of funding for this study. The Visual Function Questionnaire-25 was developed by RAND (Santa Monica, CA, USA) and funded by National Eye Institute-National Institutes of Health (Bethesda, MD, USA). The Foundation Fighting Blindness (Owings Mills, MD, USA) sponsored CHOP-PENN Pediatric Center for Retinal Degenerations, Research to Prevent Blindness (New York, NY, USA), Macula Vision Research Foundation (West Conshohocken, PA, USA), Paul and Evanina Mackall Foundation Trust at the Scheie Eye Institute, and F M Kirby Foundation (Philadelphia, PA, USA). This work was also supported with grants from Telethon (Naples, Italy; numbers TIGEM-P21 to AA, EMS, and SB at TIGEM, and GGP07180 to FS); Regione Campania Convenzione (66 del DPR 382/80 to FS); and European Union (018933 Clinigene and 223445 AAVEYE to AA). We thank the Foundation for Retinal Research and Associazione Italiana Amaurosi Congenita di Leber for their support. FC is a doctoral student supported by the Fund for Scientific Research (FWO) Flanders grant (1.1.387.07.N.00). This study is also supported by FWO Flanders grants (1.2.843.07.N.01, 1.5.244.05 to EDB and OZP 3G004306 to EDB and BPL) and Fund for Research in Ophthalmology (FRO 2008). The project was supported with a grant (UL1-RR-024134) from the National Center for Research Resources. KAH and ES are investigators at the Howard Hughes Medical Institute. We are indebted to the patients and their families for their continuous support of the study; to the medical, operating room, anaesthesia, and nursing staff at CHOP; and physicians and staff in the Division of Ophthalmology at CHOP. We give special thanks to Michael Ward, Laureen Murphy Kotzer, and Ivy Kuhn, for their clinical expertise. We thank the members of the CHOP institutional review board and their chairperson Mark Schreiner, and David Brint, Richard Hurwitz, Mark Blumenkranz, and David Birch for their invaluable guidance; and Edward Pugh Jr, Valder Arruda, Elias Traboulsi, Robert Nelson, Andrea Ballabio, and Alfredo Ciccodicola for helpful discussions. We thank Stuart Fine and Monte Mills for their support; and John Andrews-Labenski, Fred Letterio, Sohani Amarasekera, Karly Brint, Mohammed Toure, Nicholas Volpe Jr, Kalyani Bhatt, Daniel Bennett, Michael Bennett, Mettine H A Bos, William Bennett, Carmela Ziviello, Armida Faella, Anna Nesti, Angelo Torre, Sonali Joyce, Vito de Novellis, Ida Marabese, Liza Africa, Jitin Bajaj, Gary Pien, and Valentina Di Iorio for technical and clinical assistance; and Katherine H Maguire for editing the videos. The content of this report is solely the responsibility of the authors and does not necessarily represent the views of the funding sources, National Center for Research Resources, or the National Institutes of Health (both Bethesda, MD, USA).
AMM and JB are co-inventors of a pending patent for a method to treat or slow the development of blindness, but both waived any financial interest in this technology in 2002. JB served on a Scientific advisory board for Ceregene in 2006–08, and presented a seminar at Novartis in 2009. KAH has served as a consultant for Tacere and as a Scientific advisory board member for Amsterdam Molecular Therapeutics, but there was no retinal research involved; been a speaker at the invitation of Genzyme, a company with a research programme in AAV; and is the director Center for Cellular and Molecular Therapeutics at CHOP, which sponsors the clinical trial. JFW has served as a consultant for Genzyme and Tacere, but there was no retinal research involved; and is an inventor on patents describing methods for AAV vector manufacturing. FM has served as a consultant for Arthrogen, but there was no retinal research involved; is an inventor of a patent of composition and methods for the detection and modulation of T-cell responses to the AAV capsid.
Footnotes
Contributors
AMM, JWM, FS, and JB participated in the design of the clinical trial. AMM, EAP, FT, SR, KAM, XZ, and FS did the surgical and clinical procedures. AMM, AA, JFW, FT, FM, JLB, SR, KAM, BH, OZ, EMS, CA, TMR, JS, FS, and JB obtained and maintained the equipment and supplies for the study. AMM, JFW, EAP, FM, JLB, KSS, NJV, FS, and JB participated in the design of specific assays. AMM, FT, SR, AF, KAM, SB, LR, FC, EDB, ES, BPL, and FS participated in patient selection. AMM, KAH, AA, JFW, KAM, EMS, CA, JWM, and FS were responsible for the regulatory issues. KAH, JFW, JLB, BH, OZ, and JB generated and validated the clinical vector. EAP, FT, SR, KAM, DCC, XZ, LR, CA, FS, and JB tested the use of the vector in patients. AMM, EAP, FT, FM, JLB, GY, KAM, SB, JIWM, BH, OZ, FC, EDB, AL, JWM, BPL, FS, and JB did the data analysis. AMM and JB wrote the report. AMM was the principal investigator for the clinical trial. All authors participated in reviewing the report.
Conflicts of interest
The other authors declare that they have no conflicts of interest.
References
- 1.Aleman TS, Jacobson SG, Chico JD, et al. Impairment of the transient pupillary light reflex in Rpe65(−/−) mice and humans with Leber congenital amaurosis. Invest Ophthalmol Vis Sci. 2004;45:1259–1271. doi: 10.1167/iovs.03-1230. [DOI] [PubMed] [Google Scholar]
- 2.Lorenz B, Gyurus P, Preising M, et al. Early-onset severe rod-cone dystrophy in young children with RPE65 mutations. Invest Ophthalmol Vis Sci. 2000;41:2735–2742. [PubMed] [Google Scholar]
- 3.Simonelli F, Ziviello C, Testa F, et al. Clinical and molecular genetics of Leber’s congenital amaurosis: A multicenter study of Italian patients. Invest Ophthalmol Vis Sci. 2007;48:4284–4290. doi: 10.1167/iovs.07-0068. [DOI] [PubMed] [Google Scholar]
- 4.Perrault I, Rozet JM, Gerber S, et al. Leber congenital amaurosis. Mol Genet Metab. 1999 Oct;68:200–208. doi: 10.1006/mgme.1999.2906. [DOI] [PubMed] [Google Scholar]
- 5.den Hollander AI, Roepman R, Koenekoop RK, Cremers FP. Leber congenital amaurosis: genes, proteins and disease mechanisms. Prog Retinal Eye Res. 2008;27:391–419. doi: 10.1016/j.preteyeres.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Moiseyev G, Chen Y, Takahashi Y, Wu B, Ma J. RPE65 is the isomerohydrolase in the retinoid visual cycle. Proc Natl Acad Sci USA. 2005;102:12413–12418. doi: 10.1073/pnas.0503460102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jin M, Li S, Moghrabi WN, Sun H, Travis GH. Rpe65 is the retinoid isomerase in bovine retinal pigment epithelium. Cell. 2005;122:449–459. doi: 10.1016/j.cell.2005.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Redmond TM, Yu S, Lee E, et al. Rpe65 is necessary for production of 11-cis-vitamin A in the retinal visual cycle. Nature Genet. 1998;20:344–351. doi: 10.1038/3813. [DOI] [PubMed] [Google Scholar]
- 9.Redmond TM, Poliakov E, Yu S, Tsai J, Lu Z, Gentleman S. Mutation of key residues of RPE65 abolishes its enzymatic role as isomerohydrolase in the visual cycle. Proc Natl Acad Sci USA. 2005;102:13658–13663. doi: 10.1073/pnas.0504167102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Acland GM, Aguirre GD, Bennett J, et al. Long-term restoration of rod and cone vision by single dose rAAV-mediated gene transfer to the retina in a canine model of childhood blindness. Mol Ther. 2005;12:1072–1082. doi: 10.1016/j.ymthe.2005.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jacobson SG, Aleman TS, Cideciyan AV, et al. Identifying photoreceptors in blind eyes caused by RPE65 mutations: prerequisite for human gene therapy success. Proc Natl Acad Sci USA. 2005;102:6177–6182. doi: 10.1073/pnas.0500646102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dejneka N, Surace E, Aleman T, et al. Fetal virus-mediated delivery of the human RPE65 gene rescues vision in a murine model of congenital retinal blindness. Mol Ther. 2004;9:182–188. doi: 10.1016/j.ymthe.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 13.Bennicelli J, Wright J, Komaromy A, et al. Reversal of visual deficits in animal models of leber congenital amaurosis within weeks after treatment using optimized AAV2-mediated gene transfer. Mol Ther. 2008;16:458–465. doi: 10.1038/sj.mt.6300389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.NIH. Bethesda: National Institutes of Health; 2005. Dec 13, [accessed July 25, 2009]. Recombinant DNA Advisory Committee. 2005. http://www.webconferences.com/nihoba/13_dec_2005.html. [Google Scholar]
- 15.Maguire AM, Simonelli S, Pierce EA, et al. Safety and efficacy of gene transfer for Leber congenital amaurosis. N Engl J Med. 2008;358:2240–2248. doi: 10.1056/NEJMoa0802315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bainbridge J, Smith A, Barker S, et al. Effect of gene therapy on visual function in Leber’s congenital amaurosis. N Engl J Med. 2008;358:2231–2239. doi: 10.1056/NEJMoa0802268. [DOI] [PubMed] [Google Scholar]
- 17.Cideciyan AV, Aleman TS, Boye SL, et al. Human gene therapy for RPE65 isomerase deficiency activates the retinoid cycle of vision but with slow rod kinetics. Proc Natl Acad Sci USA. 2008;105:15112–15117. doi: 10.1073/pnas.0807027105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hauswirth W, Aleman T, Kaushal S, et al. Treatment of Leber congenital amaurosis due to RPE65 mutations by ocular subretinal injection of adeno-associated virus gene vector: short-term results of a phase I trial. Hum Gene Ther. 2008;19:979–990. doi: 10.1089/hum.2008.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cideciyan AV, Hauswirth W, Aleman TS, et al. Human RPE65 gene therapy for Leber congenital amaurosis: persistence of early visual improvements and safety at one year. Hum Gene Ther. 2009;20:999–1004. doi: 10.1089/hum.2009.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simonelli F, Maguire A, Testa F, et al. Gene therapy for Leber’s congenital amaurosis is safe and effective through 1·5 years after vector administration. Mol Ther. doi: 10.1038/mt.2009.277. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bennicelli J, Wright JF, Komaromy A, et al. Reversal of blindness in animal models of Leber congenital amaurosis using optimized AAV2-mediated gene transfer. Mol Ther. 2008;358:2282–2284. doi: 10.1038/sj.mt.6300389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berson EL, Sandberg MA, Rosner B, Birch DG, Hanson AH. Natural course of retinitis pigmentosa over a 3-year interval. Am J Ophthalmol. 1985;99:240–251. doi: 10.1016/0002-9394(85)90351-4. [DOI] [PubMed] [Google Scholar]
- 23.Seiple W, Clemens C, Greenstein V, Carr R, Holopigian K. Test-retest reliability of the multifocal electroretinogram and Humphrey visual fields in patients with retinitis pigmentosa. Doc Ophthalmol. 2004;109:255–272. doi: 10.1007/s10633-005-0567-0. [DOI] [PubMed] [Google Scholar]
- 24.Pugh E, Jr, Lamb T. Amplification and kinetics of the activation steps in phototransduction. Biochim Biophys Acta. 1993;1141:111–149. doi: 10.1016/0005-2728(93)90038-h. [DOI] [PubMed] [Google Scholar]
- 25.Bergamin O, Kardon R. Latency of the pupil light reflex: sample rate, stimulus intensity, and variation in normal subjects. Invest Ophthalmol Vis Sci. 2004;45:1259–1271. doi: 10.1167/iovs.02-0468. [DOI] [PubMed] [Google Scholar]
- 26.Lorenz B, Gyurus P, Preising M, Bremser DG. Early-onset severe rod-cone dystrophy in young children with RPE65 mutations. Invest Ophthalmol Vis Sci. 2003;44:1546–1554. [PubMed] [Google Scholar]
- 27.Jacobs J, Dell’Osso L, Hertle R, Acland G, Bennett J. Eye movement recordings as an effectiveness indicator of gene therapy in RPE65-deficient canines: Implications for the ocular motor system. Invest Ophthalmol Vis Sci. 2004;45:1259–1271. doi: 10.1167/iovs.05-1233. [DOI] [PubMed] [Google Scholar]
- 28.Cideciyan A, Hauswirth W, Aleman T, et al. Vision 1 year after gene therapy for Leber’s congenital amaurosis. N Engl J Med. 2009;361:725–727. doi: 10.1056/NEJMc0903652. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.