Abstract
Backgrounds/Aims
The post-operative complications and clinical course of pancreaticoduodenectomy (PD) largely depend on the pancreaticojejunostomy (PJ). Several methods of PJ are in clinical use. We analyzed the early results of binding pancreaticojejunostomy (BPJ), a technique reported by SY Peng.
Methods
We retrospectively reviewed the clinical results of patients who received BPJ in Inha University Hospital from 2006 to 2011. 21 BPJs were performed with Peng's method. The definition of postoperative pancreatic fistula (PF) was a high amylase content (>3 times the upper normal serum value) of the drain fluid (of any measurable volume), at any time on or after the 3rd post-operative day. The pancreatic fistula was graded according to the International Study Group for Pancreatic Fistula (ISGPF) guidelines.
Results
Of the 21 patients who received BPJ, 11 were male. The median age was 61.2 years. PD surgery included 4 cases of Whipple's procedures and 17 cases of pylorus-preserving PD. According to the post-operative course, 16 patients recovered well with no evidence of PF. A total of 5 patients (23.8%), including 3 grade A PFs and 2 grade C PFs, suffered from a pancreatic fistula. 3 patients with grade A PF recovered with conservative management.
Conclusions
The BPJ appears to be a relatively safe procedure based on this preliminary study, but further study is needed to validate its safety.
Keywords: Binding pancreaticojejunostomy, Pancreaticoduodenectomy, Pancreatic fistula
INTRODUCTION
Pancreaticoduodenectomy (PD) is the treatment of choice for periampullary cancer (pancreatic head cancer, distal common bile duct cancer, duodenum third portion cancer, ampulla of Vater cancer, etc.).1,2 Pancreatic fistula (PF) is the most common and most serious complication after PD.3,4,5 As the postoperative morbidity and clinical course are determined by the development status of PF, many surgeons have tried to find safer methods for pancreatic anastomosis. But most of the studies are known to have high rates of PF.
In 2003, Peng and colleagues presented a new method called "binding pancraticojejunostomy (BPJ)" for pancreatic anastomosis after PD.6 This method revives the concept of the intussusception of the body of the pancreas remnant into the jejunum. As Peng et al reported no pancreatic anastomotic leakage with the BPJ method, a remarkable finding that was published in the literature.6,7,8,9,10
The aim of this study is to evaluate the early results of BPJ and review our experience of BPJ.
METHODS
A total of 21 patients underwent Peng's BPJ procedures from 2006 to 2011 in Inha University Hospital. We retrospectively reviewed the clinical findings including the age, sex, past history, co-morbidity, laboratory test results and radiologic findings. The main pancreatic duct size was measured by using imaging modalities such as computed tomography (CT), endoscopic retrograde cholangiopancreatography (ERCP) and magnetic resonance cholangiopancreatography (MRCP) or by direct measurement at the operative field. Pancreatic duct dilatations were deemed to be present if the main pancreatic duct was 3 mm or more in size. The texture of the pancreas was determined by the surgeon in the operation field.
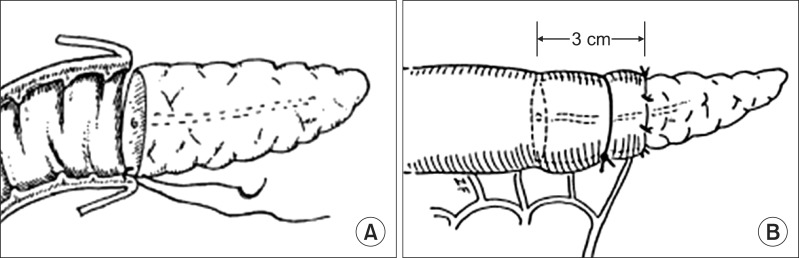
BPJs were done following Peng`s method.6,7,8,9 After everting 3 centimeters of the distal cut end of the jejunum, the exposed jejunal mucosa was destroyed with electric coagulation. The pancreatic stump and the everted jejunum were brought together and sutured with silk. The everted jejunum was then wrapped over the pancreatic stump and sutured to the pancreas with a few stitches for fixation. Lastly, at 1 cm from the cut end of the jejunum, a 2-0 Vicryl tie was looped around the entire circumference of the anastomosis (Fig. 1).
Fig. 1.
Surgical technique of binding pancreaticojejunostomy presented by Peng et al.6 (A) The pancreatic stump and the everted jejunum are brought together and sutured with silk. Care is taken to suture the mucosa only. (B) The remnant of the pancreas in the lumen of the jejunum is looped around and ligated together. A bundle of vessels is spared to maintain an intact blood supply to the jejunum cut end.
Postoperatively, oral feeding was allowed after gas passage and no evidence of leakage was found. The quantity of the drain output was measured each day after the operation until the drain was removed. Drain fluid amylase was checked on postoperative days 1, 3, 5 and 7. The drain was removed if the drain output was less than 20 cc/day and the fluid amylase was lower than the serum level. Somatostatin analogues were administered three times a day until postoperative day 7.
The definition of postoperative pancreatic fistula is a high amylase content (>3 times the upper normal serum value) of the drain fluid (of any measurable volume) at any time on or after the 3rd postoperative day. And the pancreatic fistula was graded using the International Study Group for Pancreatic Fistula (ISGPF) guidelines.11 A Grade A PF was a transient fistula, with no clinical impact, no peri-pancreatic fluid collection on CT scan, no sepsis and no prolongation of the hospital stay. This grade had little or no effect on the management. A Grade B PF had a clinical impact, required the placement of a peri-pancreatic drain or repositioning of the drain to drain a fluid collection. This group was associated with prolongation of the hospital day, and patients were often discharged with a drain in situ and observed in an outpatients setting. A PF of grade C had a serious clinical impact. This group required percutaneous drainage, major changes in the management, usually in an ICU setting, and possible reoperation to salvage a difficult situation (total pancreatectomy etc). Grade C PFs were associated with sepsis requiring aggressive antibiotics, octreotide and other intensive care support (Table 1).
Table 1.
A definition and the grading system of pancreatic fistula by the International Study Group for Pancratic fistula (ISGPF)
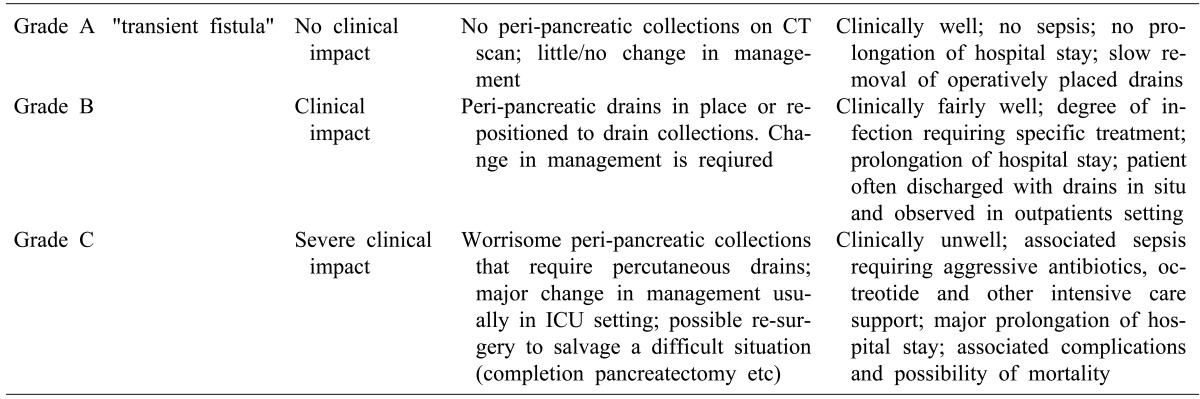
Definition: "Output via an operatively placed drain (or a subsequently placed percutaneous drain) of any measureable volume of drain fluid on or after postoperative day 3, with an amylase content greater than 3 times the upper normal serum value"
RESULTS
Of the 21 patients who underwent BPJ, 11 were male. The median age was 61.2 years (range 32-77). PD surgery included 4 cases of Whipple's procedures and 17 cases of pylorus-preserving PD (PPPD). The causative diagnoses were 3 cases of pancreatic head cancer, 5 cases of distal common bile duct cancer, 8 cases of ampulla of Vater cancer, 2 cases of duodenal tumor, 2 cases of chronic pancreatitis and 1 case of duodenal trauma. The texture of the pancreatic parenchyma was soft in 13 patients and hard in 8 patients (Table 2).
Table 2.
Patients' characteristics
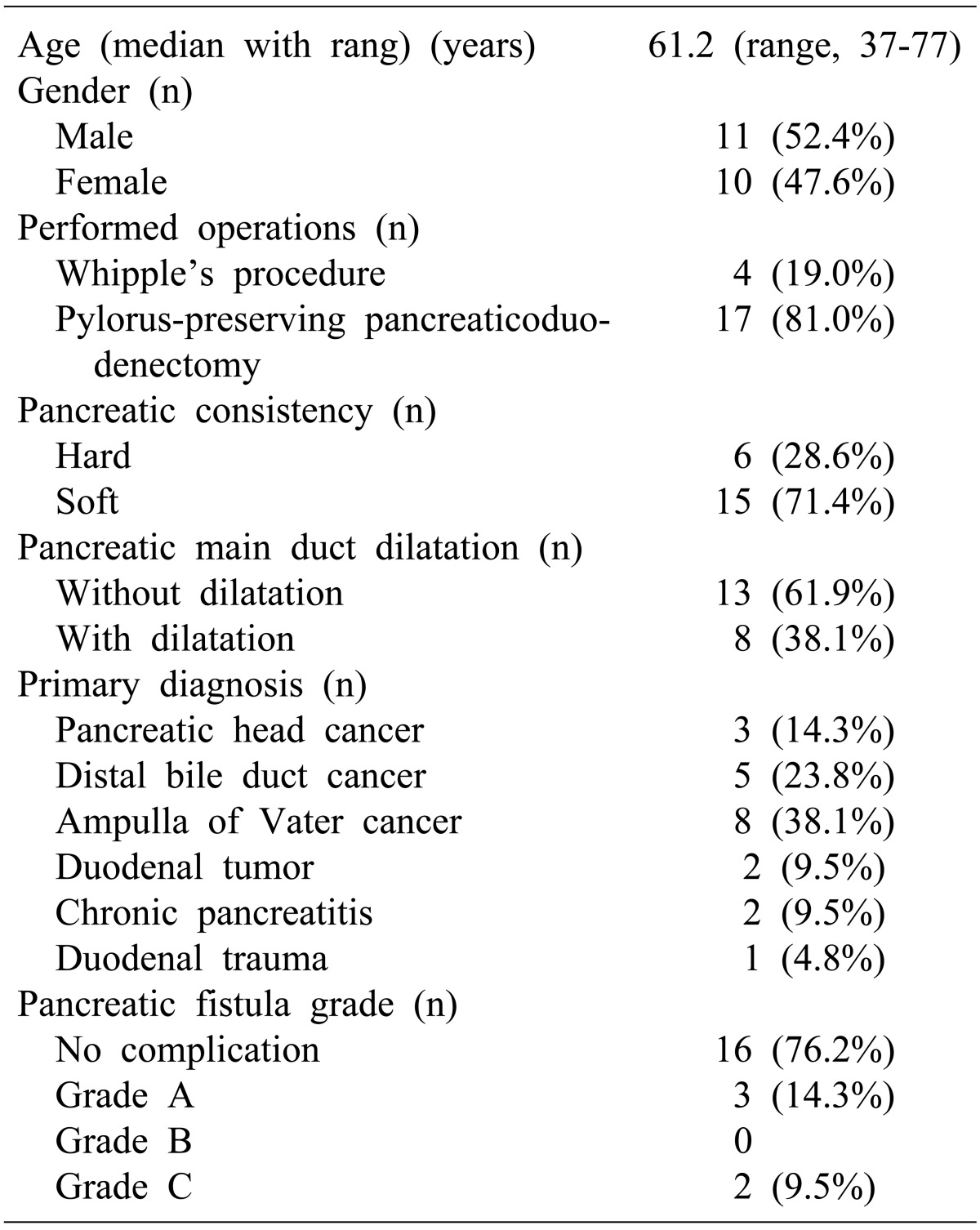
According to the post-operative course, 16 patients recovered well with no evidence of PF and 5 patients (23.8%) suffered from a pancreatic fistula. Three patients with grade A PF recovered with conservative management. Two patients were included in the grade C PF group; one patient received total pancreatectomy due to a persistent pancreatic fistula and bleeding, and one patient expired because of intraperitoneal abscess and sepsis.
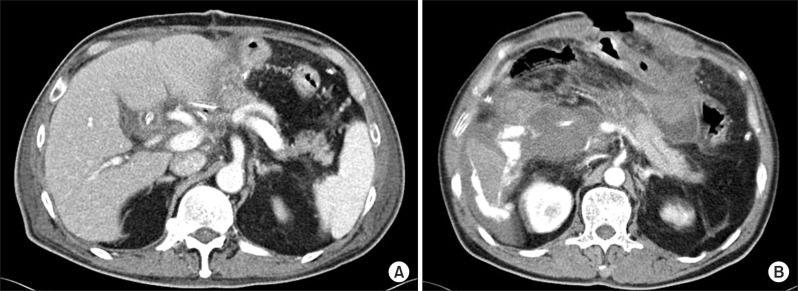
A patient who received total pancreatectomy for grade C PF after BPJ was a 75 year old man. He received PD due to cancer of the ampulla of Vater. Dilatation of the pancreas duct was identified and the texture of the pancreas was soft. He had diabetes mellitus, hypertension, and a surgical history of subtotal gastrectomy for ulcer perforation. Reoperation was performed on postoperative day 9 due to a hemoperitoneum. In the operation field, the pancreaticojejunostomy was totally disrupted and bleeding was found at the cut surface of the pancreas, and thus completion pancreatectomy was performed. He was discharged on postoperative day 66 (Fig. 2A).
Fig. 2.
Presentation of morbidity and mortality cases. (A) Computed tomography 7 days after BPJ due to an ampulla of Vater cancer. There was a minimal amount of fluid collection in the subhepatic space. In the operative field, the pancreaticojejunostomy had become totally disrupted and there was bleeding at the cut surface of the pancreas. The patient underwent completion pancreatectomy. (B) Computed tomography at 11 days after pylorus-preserving pancreaticoduodenectomy due to distal bile duct cancer. There was a loculated hematoma with high attenuated fluid in the right subphrenic, subcapsular space and the right anterior pararenal spaces. This suggested extravasation of the contrast media with active bleeding. The patient received completion pancreatectomy, but he expired due to intraperitoneal abscess and multi-organ failure.
A patient with grade C PF who expired was a 69 year old man. PPPD was done for the distal common bile duct cancer. Pancreatic duct dilatation was not observed and the texture of the pancreas was soft. Oral intake was allowed at postoperative day 8 due to a large amount of drain output. Reoperation was done on postoperative day 11 because of postoperative bleeding (Fig. 2B). During the operation, an arterial bleeding point was found at the right hepatic artery originating from the superior mesenteric artery. At postoperative day 18, he underwent completion pancreatectomy. During the operation, the pancreaticojejunostomy seemed to be intact but profuse pus was observed around the pancreaticojejunostomy. The patient expired from sepsis and multi-organ failure on postoperative day 97.
DISCUSSION
PF is a serious complication after PD. It is a major cause of postoperative morbidity and mortality and a variety of methods of have been introduced in the past. But most of the studies have reported a rate of pancreatic fistula of 30-50% in the literature. Because of that, the best procedure for pancreatic anastomosis is still under debate.
Yang et al. compared pancreatic digestive continuities after PD among many methods of reconstruction.12 His study included 10 reports about pancreatic reconstruction methods and a total of 1,408 patients were included in his study. He reported that the mortality and morbidity related with PF showed no significant difference between the pancreaticogastrostomy group and the pancreaticojejunostomy group. Compared to conventional pancreaticojejunostomy, the BPJ group has a statistically low rate of PF and postoperative complications.
Peng et al. published a report about BPJ in 2002.6 He reported a 0% rate of PF in 115 patients. In 2007, he reported a new randomized prospective study of 200 patients and the results of the BPJs were superior to conventional PJs.8 Based on our experience, the rate of PF development was not 0% but it was still lower than that for conventional PJs. This result was not associated with the texture of the pancreatic parenchyma or dilatation of the pancreatic ducts. This means that BPJ is a good procedure for patients without pancreatic duct dilatation. And patients with no leakage after BPJs showed good results clinically. Nevertheless, the morbidity, reoperation rate and mortality were similar. Of course our study was small thus we admit that we could not over the learning curve. But we found similar results from other studies too.
It is hard to mobilize the pancreas in patients who have a hard texture of the pancreas due to inflammation. More effort and a longer operation time are needed to dissect these types of pancreases.
In conventional PJ, most of the PFs were treated with close observation and supportive care. But with BPJ, a pancreatic fistula was caused by total disruption of the anastomosis. Because of that, a PF in BPJ is life-threatening and requires more procedures to be performed like percutaneous drainage or a reoperation. We suggest that more aggressive pancreas mobilization in a BPJ leads to postoperative bleeding or an insufficient blood supply for the anastomosis. Also, the post-operative fluid collection is not associated with PF, but careful attention is needed for its management because it can be related to other medical problems.
BPJ is a safe procedure and the rate of PF is very low. Our preliminary results are not as good as the results of Peng, but the rate of PF was lower than with other methods.
The main limitation of this study is its retrospective nature and the small size of the patient group that was drawn from a single institution. Further multicenter studies with larger patient groups are needed for the acquisition of more comprehensive data for BPJ.
In summary, BPJ appears to be a safe method of pancreatic anastomosis and it had a low rate of PF. But the morbidity and mortality were similar to those of conventional PJ. More efforts and study are required to achieve lower morbidity and mortality rates after PD.
Footnotes
This work was supported by Inha University Research Grant
References
- 1.Shrikhande SV, Qureshi SS, Rajneesh N, et al. Pancreatic anastomoses after pancreaticoduodenectomy: do we need further studies? World J Surg. 2005;29:1642–1649. doi: 10.1007/s00268-005-0137-3. [DOI] [PubMed] [Google Scholar]
- 2.Kakita A, Yoshida M, Takahashi T. History of pancreaticojejunostomy in pancreaticoduodenectomy: development of a more reliable anastomosis technique. J Hepatobiliary Pancreat Surg. 2001;8:230–237. doi: 10.1007/s005340170022. [DOI] [PubMed] [Google Scholar]
- 3.Winter JM, Cameron JL, Campbell KA, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: A single-institution experience. J Gastrointest Surg. 2006;10:1199–1211. doi: 10.1016/j.gassur.2006.08.018. [DOI] [PubMed] [Google Scholar]
- 4.Büchler MW, Friess H, Wagner M, et al. Pancreatic fistula after pancreatic head resection. Br J Surg. 2000;87:883–889. doi: 10.1046/j.1365-2168.2000.01465.x. [DOI] [PubMed] [Google Scholar]
- 5.Mathur A, Pitt HA, Marine M, et al. Fatty pancreas: a factor in postoperative pancreatic fistula. Ann Surg. 2007;246:1058–1064. doi: 10.1097/SLA.0b013e31814a6906. [DOI] [PubMed] [Google Scholar]
- 6.Peng S, Mou Y, Cai X, et al. Binding pancreaticojejunostomy is a new technique to minimize leakage. Am J Surg. 2002;183:283–285. doi: 10.1016/s0002-9610(02)00792-4. [DOI] [PubMed] [Google Scholar]
- 7.Peng SY, Wang JW, Li JT, et al. Binding pancreaticojejunostomy--a safe and reliable anastomosis procedure. HPB (Oxford) 2004;6:154–160. doi: 10.1080/13651820410016598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peng SY, Wang JW, Lau WY, et al. Conventional versus binding pancreaticojejunostomy after pancreaticoduodenectomy: a prospective randomized trial. Ann Surg. 2007;245:692–698. doi: 10.1097/01.sla.0000255588.50964.5d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peng SY, Wang JW, Hong de F, et al. Binding pancreaticoenteric anastomosis: from binding pancreaticojejunostomy to binding pancreaticogastrostomy. Updates Surg. 2011;63:69–74. doi: 10.1007/s13304-011-0067-6. [DOI] [PubMed] [Google Scholar]
- 10.Buc E, Flamein R, Golffier C, et al. Peng's binding pancreaticojejunostomy after pancreaticoduodenectomy: a French prospective study. J Gastrointest Surg. 2010;14:705–710. doi: 10.1007/s11605-009-1125-y. [DOI] [PubMed] [Google Scholar]
- 11.Shrikhande SV, D'Souza MA. Pancreatic fistula after pancreatectomy: evolving definitions, preventive strategies and modern management. World J Gastroenterol. 2008;14:5789–5796. doi: 10.3748/wjg.14.5789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang SH, Dou KF, Sharma N, et al. The methods of reconstruction of pancreatic digestive continuity after pancreaticoduodenectomy: a meta-analysis of randomized controlled trials. World J Surg. 2011;35:2290–2297. doi: 10.1007/s00268-011-1159-7. [DOI] [PubMed] [Google Scholar]