Dear editor
We read with interest the paper by Anwar et al.1 The authors have described a technique to bare Descemet’s membrane (DM) by multiple lamellar dissection of the deep corneal stroma when stromal injection of air fails to achieve a big bubble (BB) in deep anterior lamellar keratoplasty (DALK).
The technique is a variation of the principle of exploiting “microdetachments” of DM dissecting successive layers of the deep stroma until the desired residual thickness is achieved. The text and the video illustrate the technique well and we agree that this is a useful option when there is a failure to obtain a BB in DALK. However, we suggest that the conclusions they have drawn both in the text and the narration of the video are incorrect.
It is well known now that when air is injected into the corneal stroma three types of BB can be achieved.2 1) Type 1 BB where the air separates Dua’s layer (DL) from the deep stroma creating a large central bubble of around 8 to 9 mm in diameter. This is the preferred type of bubble in DALK, as DL confers additional strength to the recipient cornea as the authors have stated. After excising the recipient stroma, the complex of host DL and DM and endothelial cells is retained. 2) Type 2 BB wherein the DM is separated from the posterior surface of DL by the air bubble. This BB is larger with a thinner wall and more susceptible to tears and bursting. 3) Mixed BB when the above two coexist, usually type 1 is complete and type 2 is partial but both can be complete. In our experience during DALK surgery, about 80%–85% of the BB is type 1 and 15%–20% is type 2 or mixed. It has recently come to light that the plane of cleavage between DL and deep stroma can be accessed by fungi in corneal infections and even mechanically by blunt dissection (Dua HS et al and Hardik P et al, unpublished data, 2015) during DALK or preparation of tissue for pre-Descemet’s endothelial keratoplasty.3,4 When the plane is mechanically accessed during DALK, the host’s retained tissue complex is as described above with a type 1 BB. The surface of this tissue complex gives a rough appearance (Figure 1A) related to broken strands or fibers of collagen that are stretched when DL is separated from the deep stroma. These strands or fibers can be seen to extend between the posterior surface of the deep stroma and the anterior surface of DL during mechanical dissection and have to be severed or cut. In comparison the surface of the DM (type 2 BB) appears very smooth and featureless (Figure 1B).
Figure 1.
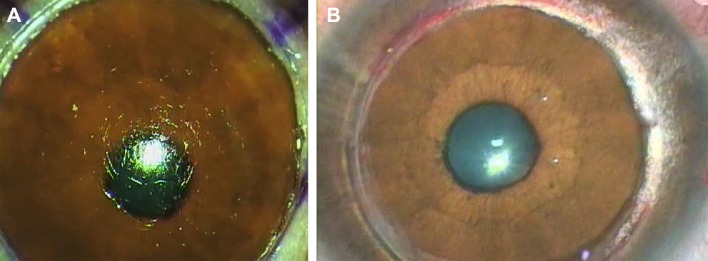
Difference between type 1 and type 2 big bubbles.
Notes: (A) The anterior surface of the Dua’s layer after creation of a type 1 big bubble. The broken strands or fibers of collagen give the surface a rough-looking appearance and is characteristic of cleavage having occurred between deep corneal stroma and the anterior surface of Dua’s layer. (B) The anterior surface of the Descemet’s membrane exposed after creation of a type 2 big bubble. The surface is very smooth and featureless with no visible fibers. This type of bubble is more susceptible to rupture or tear as it is not protected by Dua’s layer.
In the images and video provided by Anwar et al, they have in fact reached and nicely dissected in the plane between DL and stroma and not bared the DM. The appearance of the surface of the host’s retained deep tissue is like that in Figure 1A. Moreover, in the video at several places and especially when the last quadrant is being excised, the strands or fibers between DL and deep stroma are clearly visible. These facts strongly suggest that they were dissecting in the plane analogous to a type 1 BB. Moreover, the formation of a type 1 BB commences with the appearance of small pockets of air between DL and deep stroma which become confluent to produce the full BB.2 In Figure 6B, Anwar et al have illustrated with arrows the microdetachment of the DM. Careful examination of the microdetachment reveals a layer, Dua’s layer, of eosinophilic stained tissue anterior to the darkly stained DM. This is a small pocket of air between DL and deep stroma and not a microdetachment of DM. Such a pocket can be accessed and allow cleavage in that plane by blunt dissection as the authors have very clearly demonstrated. We congratulate the authors for developing and sharing this technique, but we suggest that they present this technique as one that preserves DL and hence is more akin to a type 1 BB with all the advantages especially adding strength to the transplanted eye.5 Theoretically, it is possible to find the plane between DL and DM by mechanical dissection but carries a much greater risk of DM tear or rupture.
Disclosure
The authors have no conflicts of interest to disclose.
Footnotes
Disclosure
The authors have no conflicts of interest to disclose.
References
- 1.Anwar DS, Kruger MM, Mootha VV. Blunt scissors stromal dissection technique for deep anterior lamellar keratoplasty. Clin Ophthalmol. 2014;8:1849–1854. doi: 10.2147/OPTH.S63300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dua HS, Faraj LA, Said DG, Gray T, Lowe J. Human corneal anatomy redefined: a novel pre-Descemet’s layer (Dua’s layer) Ophthalmology. 2013;120(9):1778–1785. doi: 10.1016/j.ophtha.2013.01.018. [DOI] [PubMed] [Google Scholar]
- 3.Liu Z, Zhang P, Liu C, Zhang W, Hong J, Wang W. Split of Descemet’s membrane and pre-Descemet’s layer in fungal keratitis: new definition of corneal anatomy incorporating new knowledge of fungal infection. Histopathology. 2015;66(7):1046–1049. doi: 10.1111/his.12568. [DOI] [PubMed] [Google Scholar]
- 4.Agarwal A, Dua HS, Narang P, et al. Pre-Descemet’s endothelial keratoplasty (PDEK) Br J Ophthalmol. 2014;98(9):1181–1185. doi: 10.1136/bjophthalmol-2013-304639. [DOI] [PubMed] [Google Scholar]
- 5.Zaki AA, Elalfy MS, Said DG, Dua HS. Deep anterior lamellar keratoplasty-triple procedure: a useful clinical application of the pre-Descemet’s layer (Dua’s layer) Eye (Lond) 2015;29(3):323–326. doi: 10.1038/eye.2014.273. [DOI] [PMC free article] [PubMed] [Google Scholar]


