Abstract
Objective
To examine associations between relative, friend, and partner support, as well as size and source of weekly social network, on mortality risk in the Aerobics Center Longitudinal Study (ACLS).
Patients and Methods
In a mail-back survey completed between January 1, 1990 and December 31, 1990, adult ACLS participants (n=12,709) answered questions regarding whether they received social support from relatives, friends, and spouse/partner (yes or no for each), and the number of friends and relatives they had contact with at least once per week. Participants were followed until December 31, 2003 or death. Cox proportional hazard regression evaluated the strength of the associations, controlling for covariates.
Results
Participants (25% women) averaged 53.0 years at baseline. During a median 13.5 years of follow-up, 1,139 deaths occurred. Receiving social support from relatives reduced mortality risk 19% (HR 0.81, 95% CI 0.68–0.95). Receiving spousal/partner support also reduced mortality risk 19% (HR 0.81, 95% CI 0.66-.99). Receiving social support from friends was not associated with mortality risk (HR 0.90, 95% CI 0.75–1.09), however, participants reporting social contact with 6 or 7 friends on a weekly basis had a 24% lower mortality risk than those in contact with ≤ 1 friend (HR 0.76, 95% CI 0.58–0.98). Contact with 2–5 or ≥8 friends was not associated with mortality risk, nor was number of weekly relative contacts.
Conclusions
Receiving social support from one’s spouse/partner and relatives and maintaining weekly social interaction with 6–7 friends reduced mortality risk. Such data may inform interventions to improve long-term survival.
Epidemiological and clinical research has established social relations as one of several key domains relevant to behavioral medicine. 1 In 1988, House and colleagues published a seminal review of prospective and experimental studies demonstrating a causal link between social relations and mortality risk.2 Research on the topic has continued in recent decades, and in 2010 a meta-analysis of 148 studies found that having stronger social relationships was associated with a 50% increased likelihood of survival (OR=1.50, CI=1.42–1.59) across age, gender, initial health status, and cause of death.3 The protective effect was found irrespective of whether structural aspects, such as frequency of social participation4 and diversity of social network,5 or functional aspects, such as marital quality6 and perceived social support,7 of social relationships were measured. A 2013 meta-analysis by Tay and colleagues reiterated the protective effect of both structural and functional aspects of social relations in an extensive review of reviews.8
These reviews provide clear evidence of a relationship between social relations and mortality risk, yet important questions remain. From a functional perspective, does the source of social support (e.g., partner, relative or friend) matter? If so, which source(s) is (are) most important? In terms of structural aspects of social relations, is there a minimum social network size required to reap health benefits? And, is more always better, or is there a threshold effect? Answering these questions could facilitate the application of this extensive knowledge base to the development of therapies or interventions to help various medical conditions, including cardiovascular disease (CVD) and cancer;9 indeed, poor social relations have consistently been associated with increased risk of major CVD, which remains the major threat to health in most of the world.1, 10, 11 Therefore, the purpose of this study is to examine the associations between relative, friend, and partner support, as well as size (and source) of weekly social network, on mortality risk in the Aerobics Center Longitudinal Study (ACLS).
Patients and Methods
Participants
The ACLS is a cohort study that investigates the relationship of a variety of health factors to chronic diseases.12 Data were obtained from patients of the Cooper Clinic in Dallas, Texas. Many patients were sent by their employers for preventive medical examination, some were referred by their personal physicians, whereas others were self-referred. The present study consists of 12,709 men and women ages 18–90 who completed a mail-back survey in 1990. The study protocol was approved annually by the institutional review board of the Cooper Institute.
Measurements
All participants included in the current study completed a mail-back survey in 1990 between January 1 and December 31; the midpoint of survey completion (6/30/90) served as the baseline date for calculating follow-up time. The survey was developed by researchers at the Cooper Institute. Participants provided information on smoking habits (never, former, or current smoker), alcohol intake (drinks per week), physical activity habits (physically inactive or not), and marital status (married or not). Consuming >14 drinks/wk for men and 7 drinks/wk for women was defined as heavy alcohol drinking. Physically inactive was defined as reporting no leisure-time walking or jogging in the three months prior to the examination. Self-reported height and weight were used to calculate body mass index (BMI) as weight in kilograms divided by height in meters squared. Self-reported history of physician diagnosis of diabetes, hypertension, and high serum cholesterol were considered for chronic conditions.
Social support
As part of the mail-back survey developed by researchers at the Cooper Institute, participants indicated whether or not they received social support (“Do you receive support from relatives and friends? Social support can be instrumental or emotional. Instrumental Support includes financial aid, information, help with family or work, advice, food, or transportation. Emotional Support includes affection, sympathy, trust, encouragement, or guidance. Please indicate whether or not you receive social support from each of the groups listed [Spouse or Partner, Relatives, Friends, and Overall relationships] by circling NO or YES.”). The questionnaire also asked participants how many relatives and friends they had contact with at least once per week (“How often do you have social contacts with relatives or friends? Circle one [Daily, Weekly, Monthly, Yearly, Never] per group [Relatives, Friends].”). Participants were instructed to answer the latter question ‘for relatives and friends with whom you do not live’.
Mortality follow-up
Participants were followed from June 30, 1990 (midpoint of 1990 survey completion) until date of death or until December 31, 2003. Mortality surveillance was conducted using the National Death Index, and the underlying cause of death was determined from the National Death Index report or by nosologist’s review of the official death record from the department of vital records in the participant’s state of residence. Follow-up time was computed as the difference between June 30, 1990 and the date of death for decedents or December 31, 2003 for survivors.
Statistical analysis
Continuous variables were summarized using mean ± SD and categorical variables were summarized using frequency (%). Continuous variables were compared using Student’s t-test and categorical variables were compared using the Chi square test. Separate Cox proportional hazards regression analyses were performed to assess the association between receiving social support from relatives, spouse/partner, and friends (compared to not receiving support from these sources) and mortality risk. Covariates included age, gender, BMI (model 1), plus current smoking (yes/no), heavy alcohol intake (yes/no), and physical inactivity (yes/no) (model 2), plus presence of hypertension, high serum cholesterol, and diabetes at baseline (model 3). Additional Cox proportional hazards regression analyses were performed to assess the association between size of weekly social network (number of relatives in contact with at least once weekly, number of friends in contact with at least once weekly) and mortality risk. For relatives, three categories were compared: 1–3 relatives (reference) versus 4–6 and ≥7. For friends, 5 categories were compared: ≤1 weekly contact (reference) versus 2–3, 4–5, 6–7, and ≥8 weekly contacts. These categories were based on the distribution of the respective variables and logical grouping of the data. All analyses were performed using SAS, version 9.3 (SAS Institute, Inc., Cary, NC). All p values are two-sided with an α-level of 0.05.
Results
Participants (25% women) averaged 53.0 (SD 11.3) years of age at baseline and were followed for a median 13.5 (range 12.4) years. During follow-up, 1,139 deaths occurred. In terms of weekly social network size, participants reported being in contact with 3.6 (SD 3.3) relatives and 6.9 (SD 8.0) friends per week. In terms of social support, 84% of participants reported receiving support from relatives, 88% reported receiving support from friends, and 91% reported receiving support from their spouse/partner. Table 1 presents participant characteristics by gender.
Table 1.
Baseline participant characteristics.
| Characteristic | Males | Females | P value | ||
|---|---|---|---|---|---|
|
| |||||
| Number of participants | Mean (SD) | Number of participants | Mean (SD) | ||
| Age (years) | 9489 | 53.4 (11.1) | 3220 | 52.1 (11.7) | <.001 |
| BMI (kg/m2) | 7781 | 25.4 (4.9) | 2951 | 22.7 (4.8) | <.001 |
| Follow-up years | 9489 | 13.0 (1.9) | 3220 | 13.2 (1.5) | <.001 |
| No. relatives in contact with at least once weekly | 7008 | 3.5 (3.3) | 2548 | 4.0 (3.4) | <.001 |
| No. friends in contact with at least once weekly | 7692 | 7.0 (8.0) | 2527 | 6.6 (7.8) | .02 |
| Characteristic | Number of participants | N (%) | Number of participants | N (%) | P value |
| Current smokers | 9366 | 842 (9.0) | 3171 | 170 (5.4) | <.001 |
| Heavy Drinkersa | 9489 | 753 (8.0) | 3220 | 308 (9.6) | .004 |
| Physical inactivity b | 9200 | 2761 (30.0) | 3117 | 903 (29.0) | .27 |
| Self-reported baseline conditions | |||||
| High serum cholesterol | 9489 | 2088 (22.0) | 3220 | 574 (17.8) | <.001 |
| Diabetes mellitus | 9489 | 168 (1.8) | 3220 | 43 (1.3) | .10 |
| Hypertension | 9489 | 1712 (18.0) | 3220 | 372 (11.6) | <.001 |
| Married | 9482 | 8439 (89.0) | 3219 | 2568 (79.8) | <.001 |
| No. reporting support from relatives c | 9409 | 7642 (81.2) | 3181 | 2918 (91.7) | <.001 |
| No. reporting support from friends c | 9408 | 8083 (85.9) | 3193 | 3049 (95.5) | <.001 |
| No. reporting support from spouse c | 9122 | 8212 (90.0) | 2854 | 2661 (93.2) | <.001 |
Abbreviations: BMI, body mass index; No., number; SD, standard deviation.
Defined as > 14 and >7 drinks/week for men and woman, respectively.
Defined as no self-reported leisure time walking or jogging in 3 months prior to survey completion.
Responded ‘yes’ to question, ‘Do you receive support?’.
Table 2 shows the associations between different sources of social support and mortality risk by model. When running the fully adjusted model, participants reporting family support had a 19% lower risk of mortality as compared to participants reporting no family support (P=.01). Participants reporting spousal/partner support also had a 19% lower risk of mortality as compared to participants reporting no spousal/partner support (P=.04). Support from friends was not significantly related to mortality risk (P=.29).
Table 2.
Risk of mortality by source of social support received.
| Model 1 a | Model 2 b | Model 3 c | ||
|---|---|---|---|---|
|
|
||||
| Source of support | N (deaths) | HR (95% CI) | HR (95% CI) | HR (95% CI) |
| Friend | ||||
| No | 1469 (172) | Referent | Referent | Referent |
| Yes | 11132 (946) | 0.92 (0.76–1.10) | 0.91 (0.76–1.10) | 0.90 (0.75–1.09) |
| Relative | ||||
| No | 2030 (238) | Referent | Referent | Referent |
| Yes | 10560 (876) | 0.84 (0.71–0.98)* | 0.81 (0.68–0.95)* | 0.81 (0.68–0.95)* |
| Spouse | ||||
| No | 1103 (145) | Referent | Referent | Referent |
| Yes | 10873 (890) | 0.80 (0.66–0.97)* | 0.82 (0.67–1.00) | 0.81 (0.66–0.99)* |
Abbreviations: HR=hazard ratio; CI=confidence interval
Adjusted for age, gender, and body mass index.
Adjusted for above covariates plus current smoking (yes/no), heavy alcohol intake (>14 and 7 drinks/week for men and women, respectively, or no), and physical activity (leisure time walk and/or jog, yes/no).
Adjusted for above covariates plus presence of hypertension, high serum cholesterol, and diabetes at baseline.
P<.05
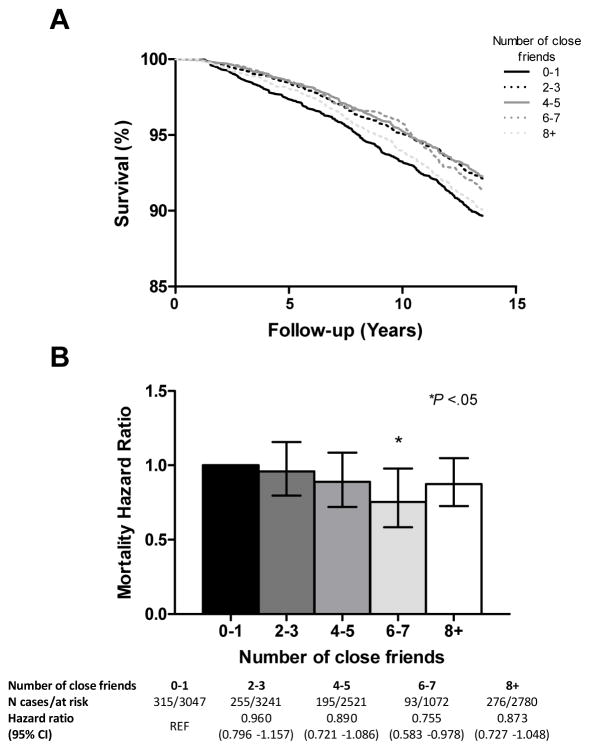
When running the fully adjusted model, participants reporting contact with 6 or 7 friends on a weekly basis had a 24% lower risk of dying than those in contact with ≤ 1 friend (P=.03). Contact with 2–5 or ≥8 friends was not significantly associated with mortality risk (2–3 friends, P=.67; 4–5 friends, P=.24; ≥8 friends, P=.15). These findings are graphically depicted in Figure 1. There was no significant relationship between number of weekly relative contacts and mortality risk in any model (full model p values: 2–3 relatives, P=.95; 4–5 relatives, P=.79; 6–7 relatives, P=.77; ≥8 relatives, P=.66).
Figure 1. Influence of size of weekly friend network on mortality risk.
A. Kaplan-Meier survival curve for size of weekly social network (friends, only) and incident all-cause mortality. B. Results of Cox regression analysis adjusted for age, gender, body mass index, current smoking, heavy alcohol intake, physical inactivity, and presence of hypertension, high serum cholesterol, and diabetes at baseline. Abbreviations: CI=confidence interval
Discussion
In a large cohort from the ACLS, perceived support from one’s spouse/partner and relatives, as well as weekly social interaction with a network of 6–7 friends, was associated with lower long-term mortality risk. When the sources were reversed, the effects did not stand-perceived social support from friends did not affect mortality risk, nor did the quantity of weekly familial contacts. Our findings suggest that source of social relations matters; further, source and type of social relations will be important to consider together in potential intervention efforts to improve health and longevity.
In the current study, both structural (size of weekly friend network) and functional (perceptions of social support from partner/relatives) aspects of social relations had health consequences, although it is likely that interacting with 6–7 friends weekly and receiving social support from partners/relatives might influence mortality risk via different mechanisms. The idea that structural and functional aspects of social relations affect health via different pathways has been noted in previous investigations.3, 13 The stress-buffering model may explain the protective effects of partner/spousal and relative social support in the ACLS; perceived social support may lead to less threatening appraisals of life hassles and daily events, thereby decreasing the negative effects of stress on mental and physical health.14–16 In this manner, social support may protect against CVD as well as improve neuroendocrine and immune function.8, 13 Although there is surely some overlap in mechanisms 13, the risk reduction associated with having a weekly social network of friends may be attributed to the sense of self-esteem, purpose, and security that comes with ones role in that network, or simply protection from social loneliness.16–18 Social networks can also influence health behaviors (for better or for worse).13 As the influence was protective in the ACLS, individuals who interacted with 6–7 friends each week may have led more active lifestyles, perhaps in terms of less sedentary time and/or more mental stimulation.
The protective effect of weekly social interaction peaked at 6–7 friends, and began to decline when the weekly friend network exceeded 7 people. This finding suggests that 6–7 friends may be the health-enhancing ‘sweet spot’ in mid-life, as fewer friends may not provide the level of stimulation needed to maximize health benefits and more friends may yield no additional benefits.
The importance of source may speak to a core difference in what people seek in friends versus family relationships during adulthood. It is plausible that relatives and partners are expected to provide support during this phase of life, whereas friendships are maintained primarily for socialization/social life; the expectations for these relationships may dictate the pathway to health benefits. For example, a 2004 meta-analysis of psychosocial intervention studies found that spouse and spouse/adult child engagement reduced depressive symptoms and morality risk, respectively,19 whereas two reviews of peer-support interventions found limited to no benefit.20, 21
We also should consider the possible influence of giving support. A 2003 study of older married couples showed that mortality was reduced in individuals providing emotional support to their spouse and instrumental support to friends, relatives and neighbors. When giving support was considered, receiving support had no effect on mortality.22 In a similar vein, a 2013 study by Poulin et al. found that helping close others (i.e., friends or family members) by providing tangible assistance (e.g., shopping, childcare) buffered the association between stress and mortality. 23 In this ACLS sample (average age 53, 87% married), it is possible that giving support was more predominant in spouse and relative relationships than friendships, and thus this unmeasured element could partially explain the greater risk reduction.
Strengths & Limitations
Major strengths of this study include its longitudinal design and large sample size. This study makes an important contribution to the social relations -health literature by providing insight into the importance of the source of social support, as well as the size and source of one’s weekly social network. A limitation of this study is its generalizability to other populations, as the ACLS is composed largely of well-educated, white individuals of middle-to-high socioeconomic status. Further, a large number of Cooper Clinic patients are business executives referred by their companies for preventive medical examination, with the majority of executives being men. Although the current sample was only 25% female, a large meta-analysis of 148 studies found consistent protective effects of social relationships across the sexes.3
For the purposes of this study, our analyses included all participants that reported receiving support irrespective of reported satisfaction with support; small percentages of participants (2.6% receiving friend support, 3.8% receiving relative support and 6.3% receiving spousal/partner support) reported being dissatisfied with their support, and future research may wish to further investigate the influence of satisfaction with support on health outcomes. Further, the measures of social relations provided by the Cooper Institute’s questionnaire are very basic; complex measures of social integration have been shown to be more predictive of the relationship between social relations and long-term mortality risk.3 This may suggest that the relationship between social relations and mortality is even stronger than observed in the current study.
Implications & Future research
Our findings have important implications for chronic disease prevention and treatment efforts, as source of support as well as size (and source) of weekly social network influenced the relationship between social relations and mortality. Rather than evaluating changes in social relations as a secondary or tertiary outcome, clinical and public health interventions should be designed primarily to foster social support and interaction. Some work has already been done in this area in clinical research, with social support interventions improving mortality outcomes in patients with CVD.19 As the current study showed that perceived social support from partners and relatives, but not friends, was associated with lower mortality risk, innovative clinical and public health interventions should also be designed to foster relationship building/strengthening in relatives and partners outside of clinical settings. Just as we design interventions to promote healthy eating and smoking cessation, it may be worthwhile to design individual-level interventions that teach interpersonal communication skills; interdisciplinary collaborations might explore modifying existing psychiatric treatments, such as interpersonal psychotherapy, for use with non-clinical populations. Larger scale strategies may include social marketing efforts to de-stigmatize and promote family and marriage counseling, or efforts to encourage primary care physicians to discuss the importance of social relations with patients (similar to those of the Exercise is Medicine® group advocating for the discussion of physical activity in clinical settings 24). Indeed, a shift in the greater public health mindset must take place, as social support affects health as much as traditional health behaviors (e.g., healthy diet, physical activity) that are commonly the focus of intervention work.3
For individuals who are unmarried, widowed or not close with relatives, pet ownership may be an alternative to human social support. The stress- buffering effects of having one’s pet present under stressful circumstances can exceed the benefits associated with a friend or spouse being present.25 Simply thinking about one’s pet has been shown to help pet owners stave off feelings of loneliness and isolation.26 There is evidence that even unfamiliar dogs can attenuate cortisol and heart rate responses to stress better than human (friend) social support.27 Further, there is a growing body of evidence suggesting that dog ownership may increase physical activity levels.28 Although facilitating pet ownership may, again, seem outside the realm of a traditional clinical or public health intervention, the convincing, consistent evidence of the protective effects of social relations requires a conceptual broadening and subsequent innovative intervention designs.
Recent studies and reviews have found strong relationships between social relations and mortality when using complex social integration measures.3, 8, 29 These measures consider various structural aspects of social relations, such as social network size, social participation (e.g., frequency of attending social activities, religious services, or going out to eat), and sense of communality. In addition to social-cognitive interventions that promote supportive interpersonal relationships, social-ecological interventions that alter the physical environment may help promote social integration, especially as our society ages. Kweon and Sullivan found that inner-city older adults who reported using green outdoor common spaces had stronger neighborhood social ties and felt a stronger sense of community.30 Transportation is also a key element of social connectedness, making public transit accessibility and/or community walkability plausible environmental targets based on the community.31
Lastly, researchers should also continue to investigate how social relations are influenced by the use of online social networking sites (e.g., Facebook, Twitter), as there is substantial potential for positive interventions. One cross-sectional study suggests that social networking sites may have a positive influence on relationship development due to greater ease of self-disclosure,32 while another found that Facebook may be used as an outlet for individuals who are lonely and dissatisfied with their interpersonal relationships.33 An experimental study with undergraduate students found that posting Facebook status updates decreased loneliness and increased feelings of connectedness with friends on a daily basis.34 As online social networking sites continue to grow in popularity, it will be important to investigate whether digital social networks provide the same protective health benefits as physical social networks.
Conclusion
Social relationships and interactions are vital to human flourishing. Our findings speak to the differential role of friends and family members in providing health-enhancing social support and interaction, and suggest a possible ‘ideal’ weekly social network size. In order for these findings to inform behavioral care and intervention work, a conceptual shift must occur that awards improving social relations the same health behavior status as physical activity, diet and tobacco use- just as an active lifestyle and healthy diet lower mortality risk, so too does receiving support from loved ones and staying socially engaged. Further, a ‘one size does not fit all’ approach will be needed in behavioral care delivery and intervention design to aid individuals in making healthy changes despite increasingly fast-paced, high-stress lifestyles.1
Acknowledgments
All authors contributed substantially to this work. Drs. Blair, Sui and Becofsky developed the idea for the study. Drs. Becofsky and Shook conducted the statistical analyses and wrote the manuscript. Drs. Blair, Sui, Wilcox and Lavie provided expert input and guidance during manuscript preparation.
This work was supported by National Institutes of Health grants AG06945, HL62508, R21DK088195, and in part supported by an unrestricted research grant from The Coca-Cola Company.
List of Abbreviations
- ACLS
Aerobics Center Longitudinal Study
- CVD
Cardiovascular disease
Footnotes
Dr. Katie Becofsky, Dr. Robin Shook, Dr. Xuemei Sui, Dr. Sara Wilcox, and Dr. Carl J. Lavie have no conflict of interest to report.
Dr. Steven N. Blair has received research funding from the following organizations/companies: National Institutes of Health, Department of Defense, Body Media, The Coca-Cola Company. He is on Scientific/Medical Advisory Boards for the following organizations/companies: Technogym, Santech, Clarity, International Council on Active Aging, Cancer Fit Steps for Life. Other institutional affiliations include: Pennington Biomedical Research Center, University of Texas Southwestern Medical School, University of Miami, Palo Alto Medical Clinic, International Life Sciences Institute, American College of Sports Medicine, OA Action Alliance, Beijing Sports University, Singapore Health Promotion Board, British Journal of Sports Medicine.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rozanski A. Behavioral cardiology: Current advances and future directions. J Am Coll Cardiol. 2014;64(1):100–110. doi: 10.1016/j.jacc.2014.03.047. [DOI] [PubMed] [Google Scholar]
- 2.House JS, Landis KR, Umberson D. Social realtionships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 3.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: A meta-analytic review. PLoS Med. 2010;7(7):e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Avlund K, Lund R, Holstein BE, Due P, Sakari-Rantala R, Heikkinen RL. The impact of structural and functional characteristics of social relations as determinants of functional decline. J Gerontol B Psychol Sci Soc Sci. 2004;59(1):S44–51. doi: 10.1093/geronb/59.1.s44. [DOI] [PubMed] [Google Scholar]
- 5.Barefoot JC, Gronbaek M, Jensen G, Schnohr P, Prescott E. Social network diversity and risks of ischemic heart disease and total mortality: Findings from the Copenhagen city heart study. Am J Epidemiol. 2005;161(10):960–967. doi: 10.1093/aje/kwi128. [DOI] [PubMed] [Google Scholar]
- 6.Coyne JC, Rohrbaugh MJ, Shoham V, Sonnega JS, Nicklas JM, Cranford JA. Prognostic importance of marital quality for survival of congestive heart failure. Am J Cardiol. 2001;88(5):526–529. doi: 10.1016/s0002-9149(01)01731-3. [DOI] [PubMed] [Google Scholar]
- 7.Cornman JC, Goldman N, Glei DA, Weinstein M, Chang MC. Social ties and perceived support: Two dimensions of social relationships and health among the elderly in taiwan. J Aging Health. 2003;15(4):616–644. doi: 10.1177/0898264303256215. [DOI] [PubMed] [Google Scholar]
- 8.Tay L, Tan K, Diener E, Gonzalez E. Social relations, health behaviors, and health outcomes: A survey and synthesis. Applied Psychol Health Wellbeing. 2013;5(1):28–78. doi: 10.1111/aphw.12000. [DOI] [PubMed] [Google Scholar]
- 9.Lavie CJ, Milani RV, O’Keefe JH, Lavie TJ. Impact of exercise training on psychological risk factors. Prog Cardiovasc Dis. 2011;53(6):464–470. doi: 10.1016/j.pcad.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 10.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: The emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45(5):637–651. doi: 10.1016/j.jacc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 11.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99(16):2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 12.Blair SN, Kohl HW, 3rd, Paffenbarger RS, Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA. 1989;262(17):2395–2401. doi: 10.1001/jama.262.17.2395. [DOI] [PubMed] [Google Scholar]
- 13.Uchino BN. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29(4):377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- 14.Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer-Verlag; 1984. [Google Scholar]
- 15.Cohen S, Hebert TB. Health psychology: Psychological factors and physical disease from the perspective of human psychoneuroimmunology. Annu Rev Psychol. 1996;47:113–142. doi: 10.1146/annurev.psych.47.1.113. [DOI] [PubMed] [Google Scholar]
- 16.Uchino BN. Social suport and physical health: Understanding the health consequences of relationships. Yale University; 2004. [Google Scholar]
- 17.Stroebe W, Stroebe M. The social psychology of social support. New York: Guilford Press; 1996. [Google Scholar]
- 18.Thoits PA. Multiple identies and psychological well-being: A reformulation and test of the social isolation hypothesis. Am Sociol Rev. 1983;48:174–187. [PubMed] [Google Scholar]
- 19.Martire LM, Lustig AP, Schulz R, Miller GE, Helgeson VS. Is it beneficial to involve a family member? A meta-analysis of psychosocial interventions for chronic illness. Health Psychol. 2004;23(6):599–611. doi: 10.1037/0278-6133.23.6.599. [DOI] [PubMed] [Google Scholar]
- 20.Parry M, Watt-Watson J. Peer support intervention trials for individuals with heart disease: A systematic review. Eur J Cardiovasc Nurs. 2010;9(1):57–67. doi: 10.1016/j.ejcnurse.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 21.Eysenbach G, Powell J, Englesakis M, Rizo C, Stern A. Health related virtual communities and electronic support groups: Systematic review of the effects of online peer to peer interactions. BMJ. 2004;328(7449):1166. doi: 10.1136/bmj.328.7449.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brown SL, Nesse RM, Vinokur AD, Smith DM. Providing social support may be more beneficial than receiving it: Results from a prospective study of mortality. Psychol Sci. 2003;14(4):320–327. doi: 10.1111/1467-9280.14461. [DOI] [PubMed] [Google Scholar]
- 23.Poulin MJ, Brown SL, Dillard AJ, Smith DM. Giving to others and the association between stress and mortality. Am J Public Health. 2013;103(9):1649–1655. doi: 10.2105/AJPH.2012.300876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Swift DL, Lavie CJ, Johannsen NM, et al. Physical activity, cardiorespiratory fitness, and exercise training in primary and secondary coronary prevention. Circ J. 2013;77(2):281–292. doi: 10.1253/circj.cj-13-0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Allen K, Blascovich J, Mendes WB. Cardiovascular reactivity and the presence of pets, friends, and spouses: The truth about cats and dogs. Psychosom Med. 2002;64(5):727–739. doi: 10.1097/01.psy.0000024236.11538.41. [DOI] [PubMed] [Google Scholar]
- 26.McConnell AR, Brown CM, Shoda TM, Stayton LE, Martin CE. Friends with benefits: On the positive consequences of pet ownership. J Pers Soc Psychol. 2011;101(6):1239–1252. doi: 10.1037/a0024506. [DOI] [PubMed] [Google Scholar]
- 27.Polheber JP, Matchock RL. The presence of a dog attenuates cortisol and heart rate in the Trier Social Stress Test compared to human friends. J Behav Med. 2014;37(5):860–867. doi: 10.1007/s10865-013-9546-1. [DOI] [PubMed] [Google Scholar]
- 28.Christian HE, Westgarth C, Bauman A, et al. Dog ownership and physical activity: A review of the evidence. J Phys Act Health. 2013;10(5):750–759. doi: 10.1123/jpah.10.5.750. [DOI] [PubMed] [Google Scholar]
- 29.Barger SD. Social integration, social support and mortality in the US National Health Interview Survey. Psychosom Med. 2013;75(5):510–517. doi: 10.1097/PSY.0b013e318292ad99. [DOI] [PubMed] [Google Scholar]
- 30.Kweon BS, Sullivan WC, Wiley AR. Green common spaces and the social integration of innercity older adults. Environ Behav. 1998;30(6):832–858. [Google Scholar]
- 31.Emlet CA, Moceri JT. The importance of social connectedness in building age-friendly communities. J Aging Res. 2012;2012:1–9. doi: 10.1155/2012/173247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Steijn WM, Schouten AP. Information sharing and relationships on social networking sites. Cyberpsych Behav Soc Netw. 2013;16(8):582–587. doi: 10.1089/cyber.2012.0392. [DOI] [PubMed] [Google Scholar]
- 33.Lemieux R, Lajoie S, Trainor NE. Affinity-seeking, social loneliness, and social avoidance among facebook users. Psychol Rep. 2013;112(2):545–552. doi: 10.2466/07.PR0.112.2.545-552. [DOI] [PubMed] [Google Scholar]
- 34.Deters FG, Mehl MR. Does posting facebook status updates increase or decrease loneliness? An online social networking experiment. Soc Psychol Person Sci. 2013;4(5):579–586. doi: 10.1177/1948550612469233. [DOI] [PMC free article] [PubMed] [Google Scholar]