Abstract
Amyotrophic lateral sclerosis (ALS) is the most common fatal motor neuron disease in adults. Numerous studies indicate that ALS is a systemic disease that affects whole body physiology and metabolic homeostasis. Using a mouse model of the disease (SOD1G86R), we investigated muscle physiology and motor behavior with respect to muscle metabolic capacity. We found that at 65 days of age, an age described as asymptomatic, SOD1G86R mice presented with improved endurance capacity associated with an early inhibition in the capacity for glycolytic muscle to use glucose as a source of energy and a switch in fuel preference toward lipids. Indeed, in glycolytic muscles we showed progressive induction of pyruvate dehydrogenase kinase 4 expression. Phosphofructokinase 1 was inhibited, and the expression of lipid handling molecules was increased. This mechanism represents a chronic pathologic alteration in muscle metabolism that is exacerbated with disease progression. Further, inhibition of pyruvate dehydrogenase kinase 4 activity with dichloroacetate delayed symptom onset while improving mitochondrial dysfunction and ameliorating muscle denervation. In this study, we provide the first molecular basis for the particular sensitivity of glycolytic muscles to ALS pathology.
Keywords: amyotrophic lateral sclerosis, exercise, glucose, lipids, muscle
Introduction
Amyotrophic lateral sclerosis (ALS) is the most common adult motor neuron disease. Although historically defined as an age-related neurodegenerative disease specifically affecting upper and lower motor neurons, 145 years of research has now identified for ALS to be unquestionably more complex than initially described. In recent years, several non-neuronal cells including microglia (Boillée et al, 2006), astrocytes (Yamanaka et al, 2008), and skeletal muscle (Wong & Martin, 2010) have been proposed to influence the course of the disease. Moreover, mutations in an increasing number of genes have been associated with familial and sporadic forms of ALS (Chen et al, 2013). In accordance with this genetic heterogeneity, ALS has recently been redefined as a ‘syndrome’, regrouping complex and diverse pathophysiological and clinical manifestations that transgress the motor system (Andersen & Al-Chalabi, 2011; Hardiman et al, 2011).
Numerous studies indicate that ALS is a systemic disease that affects whole body physiology and energy homeostasis. In 2001, a systematic analysis of energy expenditure rates in a population of sporadic ALS patients revealed that two-thirds of these patients were hypermetabolic (Desport et al, 2001). These observations were further confirmed and extended to familial ALS cases in follow-up reports (Desport et al, 2005; Bouteloup et al, 2009). ALS patients as well as mouse models of ALS present with weight loss and reduced fat mass, altered glucose and lipid handling, and increased resting energy expenditure (Dupuis et al, 2011). In mice, reduced lipid stores and increased resting energy expenditure precede motor symptoms (Dupuis et al, 2004). Interestingly, the burden of these metabolic alterations appears to affect the neurodegenerative process. Indeed, metabolic alterations correlate with duration of survival, and clinical data suggest that an imbalance in energy metabolism has a negative impact on the pathogenic process (Desport et al, 1999; Jawaid et al, 2010). Moreover, increased dietary lipid content offers neuroprotection and extends survival in mouse models of ALS (Dupuis et al, 2004; Mattson et al, 2007), while restricting calorie intake exacerbated motor symptoms in ALS mice (Pedersen & Mattson, 1999). Although the origin of metabolic dysfunction in ALS remains unclear, many of the metabolic modifications observed at the systemic level in ALS patients and related mouse models imply that skeletal muscle contributes to ALS progression.
At rest, skeletal muscle accounts for 20–30% of the total energy expenditure. Given that skeletal muscle plays a critical role in maintaining metabolic homeostasis, altered energy balance in this tissue over extended periods of time may represent a risk factor for the development of ALS. Interestingly, thorough mapping of neuromuscular junction (NMJ) denervation patterns in the SOD1G93A mouse model of ALS revealed increased susceptibility of glycolytic fibers to undergo denervation. The loss of fast fatigable motor units composed of large motor neurons innervating type IIb fast glycolytic fibers before any apparent motor symptoms (Frey et al, 2000; Hegedus et al, 2008) suggests that the metabolic signature of glycolytic fibers may predispose them to NMJ dismantlement, one of the first pathologic events in the course of the disease (Fischer et al, 2004). Indeed, we have previously shown that promotion of muscle-specific hypermetabolism is sufficient to induce some hallmarks of ALS including destruction of the neuromuscular junction (NMJ) and the death of motor neurons (Dupuis et al, 2009). Collectively, these data suggest that metabolic changes in skeletal muscle could contribute to early destabilization of the NMJ in ALS.
In this study, we investigated early muscle metabolic alterations that might account for the metabolic imbalance and early NMJ denervation observed in SOD1G86R mice. We report an early alteration in muscle metabolic homeostasis in SOD1G86R mice. The switch toward lipid use in glycolytic muscle precedes NMJ denervation detected by EMG and the increase in expression of denervation markers. By administering dichloroacetate (DCA) to SOD1G86R mice, we reversed metabolic imbalance, improved metabolic function, and normalized the expression of denervation markers in SOD1G86R mice. Our results reveal an early metabolic pathology in skeletal muscle that contributes to the severity of the disease and adds new insight into the already complex ALS syndrome.
Results
Asymptomatic SOD1G86R mice have increased aerobic capacity
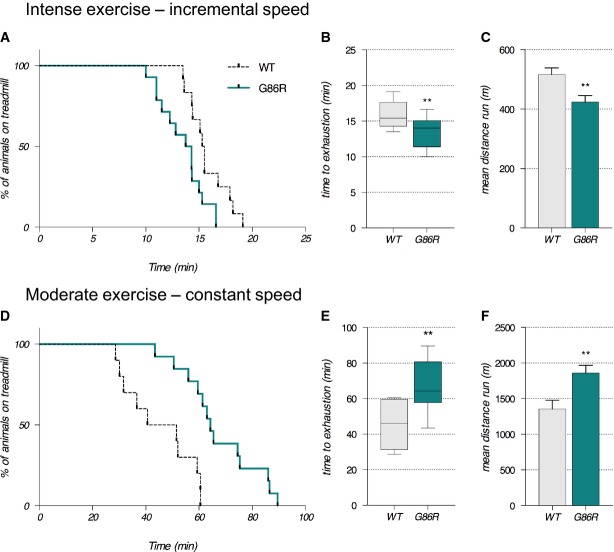
During ALS disease progression, a progressive shift in skeletal muscle fiber subtype from fast twitch to slow twitch would presumably result in a concomitant shift toward more oxidative metabolism (Dengler et al, 1990; Frey et al, 2000; Pun et al, 2006; Deforges et al, 2009). Thus, we aimed to determine whether SOD1G86R mice would have improved capacity to support endurance exercise. We compared anaerobic versus aerobic capacities of 65-day-old asymptomatic SOD1G86R mice using two exercise paradigms on a treadmill apparatus: an intense anaerobic exercise that recruits glycolytic fast-twitch fibers (Fig1A–C) and a low-intensity endurance exercise that mobilizes slow-twitch oxidative muscle fibers (Fig1D–F). As shown in Fig1A, when treadmill speed was progressively increased in the intense anaerobic exercise paradigm, 65-day-old SOD1G86R mice had significantly poorer performance than their WT littermates; SOD1G86R mice ran on the treadmill for an average of 13.50 min (median at 14.33), while their WT littermates spent an average of 15.78 min (median at 15.50) on the treadmill (Fig1B). Accordingly, SOD1G86R mice ran a total distance that was 17.6% shorter than the distance covered by their WT littermates (Fig1C). By contrast, when challenged with a moderate exercise paradigm that is representative of an endurance workout (Fig1D–F), SOD1G86R mice proved to have significantly greater endurance than their WT littermates (Fig1D). In response to moderate exercise, SOD1G86R mice ran an average of 67.34 min (median at 65.43) before reaching exhaustion, while their WT littermates ran an average of 46.10 min (median at 59.33) prior to exhaustion (Fig1D). Indeed, the resistance of SOD1G86R mice to reach exhaustion when subjected to this exercise paradigm resulted in them running a total distance that was 36% greater than the distance covered by their WT littermates (Fig1E).
Figure 1.
- A–F (A–C) Exercise performance on a treadmill apparatus using an intense exercise (incremental speed paradigm) that relies solely on anaerobic metabolism. (D–F) Exercise performance on a treadmill apparatus using a moderate exercise (constant sub-maximal speed) that relies on the recruitment of aerobic metabolism and that is representative of endurance exercise. (A, D) Kaplan–Meier curves representing values corresponding to the percentage of mice still running at a given time point. (B, E) Median values of the time that mice ran are represented in the min to max graphical representation; 15.5 min for wild-type (WT) and 14.33 min for SOD1G86R in (B); 59.33 min for WT and 65.43 min for SOD1G86R in (E). (C, F) Mean distance run ± SEM by WT and SOD1G86R mice in (C) and by WT and SOD1G86R mice in (F).
Data information: G86R versus WT, P = 0.017 in (A), **P = 0.0078 in (B), **P = 0.008 in (C) and P = 0.036 in (D) (Mantel–Cox test), **P = 0.0078 in (E), and **P = 0.0061 in (F) (Student's t-test), n = 10 and 13 for WT and SOD1G86R, respectively.
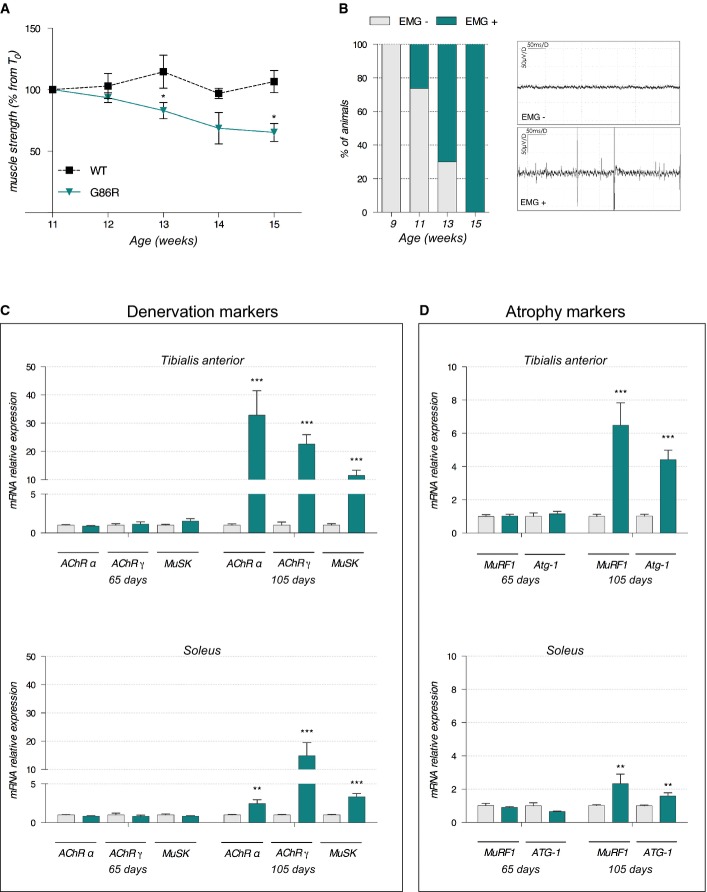
Given that skeletal muscle possesses the capacity to adapt metabolically to physical and functional challenges (Constable et al, 1987; Bassel-Duby & Olson, 2006), the enhanced aerobic capacity and poor anaerobic capacity of SOD1G86R mice might occur as a consequence of muscle denervation. In this study, we assessed the expression of AChRα and AChRγ, two subunits of the nicotinic acetylcholine receptor, and Musk, a muscle-specific kinase, all of which are rapidly overexpressed after denervation or when muscle electrical activity is absent (Duclert & Changeux, 1995; Valenzuela et al, 1995). However, at 65 days of age SOD1G86R mice did not present with any sign of denervation regardless of the metabolic capacity of muscle; muscle grip strength was comparable to that of WT littermates (Fig2A), EMG profiles were normal (Fig2B), and the mRNA expression of molecular markers of denervation (Fig2C) and atrophy (Fig2D) in glycolytic tibialis anterior (TA) or oxidative soleus muscles was similar to WT levels. By contrast, at 105 days when SOD1G86R mice are paralyzed and grip strength is decreased (Fig2A), all SOD1G86R presented with increased spontaneous activity on their EMG profiles (Fig2B). Moreover, induction of denervation and atrophy markers was more pronounced in the TA than in the soleus (Fig2C and D). These data support previous observations that in ALS, glycolytic muscles are more severely affected by disease pathology than oxidative muscles (Dengler et al, 1990; Frey et al, 2000; Pun et al, 2006). We therefore focused our subsequent analysis on the glycolytic TA.
Figure 2.
- Grip test was performed to measure mouse muscle strength at different time points during disease progression. Graph represents the mean of percentage from initial force measured at 11 weeks ± SEM. At 13 weeks, *P = 0.03; at 14 weeks, P = 0.06; at 15 weeks, *P = 0.04 (n = 8 for WT and SOD1G86R, respectively, at 11–15 weeks, two-way ANOVA followed by Fisher's LSD post hoc test).
- Electromyography (EMG) recordings were performed weekly during disease development, starting from 9 weeks of age. Spontaneous electrical activity was considered as positive EMG only for peak-to-peak amplitudes > 50 μV. Left: The percentage of mice presenting with positive EMG in each age group are represented. Right: Representative examples of negative (EMG−) and positive (EMG+) electromyography profiles (n = 10 for WT and SOD1G86R, respectively, at 9–13 weeks and n = 8 and 7 for WT and SOD1G86R, respectively, at 15 weeks).
- Relative mRNA levels of denervation markers AChR (subunits α and γ) and MuSK were evaluated by qPCR at the indicated ages (65 and 105 days) in tibialis anterior (upper panels) and soleus (lower panels) of WT and SOD1G86R mice. Graphs represent mean fold change ± SEM from age-matched WT (n > 5). ***P-values versus WT: < 0.0001 for AChRα, AChRγ, and MuSK in tibialis anterior; and **P-values versus WT: 0.001 for AChRα, and ***P-values versus WT: 0.0007 for AChRγ, 0.0002 for MuSK in soleus (n=7 and 8 for WT and SOD1G86R, respectively, at 65 days; n = 5 and 6 for WT and SOD1G86R, respectively, at 105 days; two-way ANOVA followed by Fisher's LSD post hoc test).
- Relative mRNA levels of muscle atrophy markers MuRF1 and Atg-1 were measured by qPCR at the indicated ages (65 and 105 days) in tibialis anterior (upper panels) and soleus (lower panels). Graphs represent mean fold change ± SEM from age-matched WT. ***P-values versus WT: < 0.0001 for MuRF1 and Atg-1 in tibialis anterior; and **P-values versus WT: 0.007 for MuRF1 and P = 0.006 for Atg-1 in soleus (n = 7 and 8 for WT and SOD1G86R, respectively, at 65 days, n = 5 and 6 for WT and SOD1G86R, respectively, at 105 days, two-way ANOVA followed by Fisher's LSD post hoc test).
Muscle glucose metabolism is inhibited in asymptomatic SOD1G86R mice
Glycolysis is the only metabolic pathway that provides a source of high-energy substrates for anaerobic exercise. Given that impaired glycolytic performance in SOD1G86R mice cannot be explained by denervation or atrophy, we hypothesized that reduced anaerobic performance was due to defective glucose utilization. In order to verify whether glucose metabolism is altered in SOD1G86R mice, we first analyzed their response to glucose and insulin. The glucose tolerance test (Supplementary Fig S1A) showed that at 65 days, SOD1G86R mice presented with higher blood glucose at 30 and 45 min when compared to WT littermates, suggesting that initial glucose clearance is delayed in SOD1G86R mice. However, after 120 min blood glucose levels were similar between WT and SOD1G86R mice, suggesting that there may be increased glucose uptake between 30 and 120 min in SOD1G86R mice. The response to insulin was also delayed in SOD1G86R mice when compared to WT littermates (Supplementary Fig S1B). These data show an alteration in glucose handling in SOD1G86R mice at the asymptomatic stage of disease.
To determine whether altered glucose handling occurred at the level of skeletal muscle, we assessed the activity of phosphofructokinase 1 (PFK1), the rate-limiting enzyme of glycolysis, in TA cytosolic homogenates (Fig3A). When compared to WT littermates, SOD1G86R mice had a significant 23% reduction in PFK1 enzymatic activity at 65 days of age. By the end stage of disease (105 days of age), PFK1 activity was reduced by 88.8% in SOD1G86R mice when compared to WT littermates. This was accompanied by a 5-fold down-regulation in the expression of Pfk1 mRNA in SOD1G86R mice (Supplementary Fig S1C). Interestingly, a 4-fold down-regulation in the expression of Pfk1 mRNA was also observed in SOD1G93A mice, another ALS mouse model, at the end stage of disease (Supplementary Fig S2B).
Figure 3.
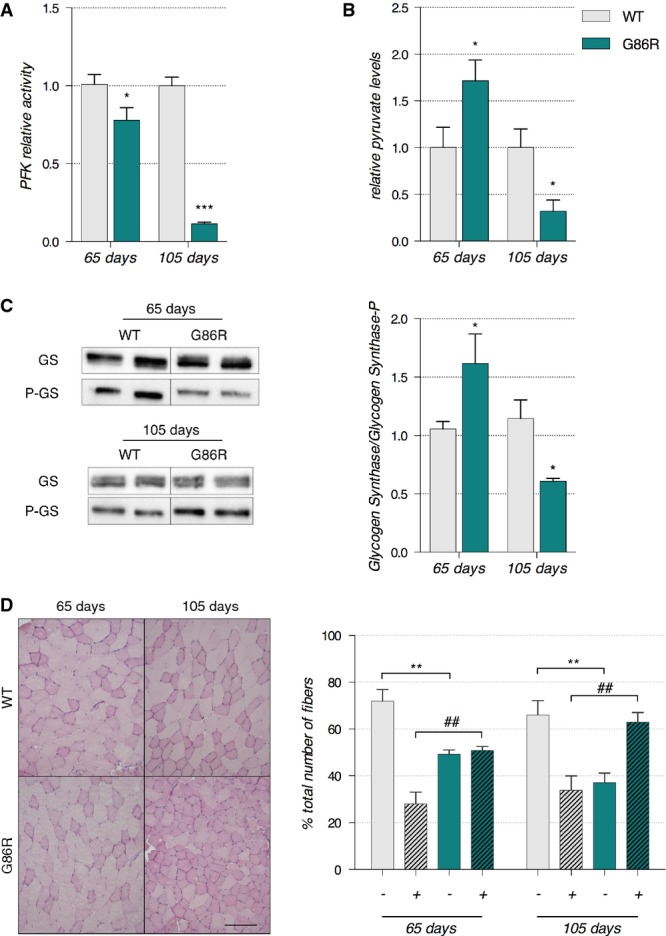
- Enzymatic activity of phosphofructokinase in whole tibialis anterior muscle cytosolic homogenates is expressed as mean fold change ± SEM from age-matched WT at 65 days of age *P = 0.016 (WT n = 6, SOD1G86R n = 7) and 105 days of age ***P < 0.0001 (n = 5/genotype), two-way ANOVA followed by Fisher's LSD post hoc test. Data shown are representative of two independent experiments having similar results.
- Pyruvate was measured in whole tibialis anterior muscle tissue homogenates. The mean fold change ± SEM compared to age-matched WT are represented with *P = 0.019 at 65 days of age (n = 5/genotype) and *P = 0.041 at 105 days of age (n = 4/genotype), two-way ANOVA followed by Fisher's LSD post hoc test. Data shown are representative of two independent experiments having similar results.
- Left: Representative Western blot showing glycogen synthase and phosphorylated glycogen synthase levels. Right: Quantification represents the mean ratio of optical densities of glycogen synthase/P-glycogen synthase ± SEM. At 65 days of age n = 6/genotype, *P = 0.0162, and at 105 days of age n = 5/genotype, *P = 0.0163, two-way ANOVA followed by Fisher's LSD post hoc test.
- Left: Representative microphotographs of PAS staining from WT and SOD1G86R tibialis anterior cross-sections at 65 and 105 days of age showing glycogen-negative (light pink) and glycogen-positive (dark pink) fibers. Scale bar: 200 μm. Right: Quantification of glycogen-negative (−) and glycogen-positive (+) fibers at 65 and 105 days of age. For (−) fibers: **P-values versus WT: 0.0026 at 65 days and 0.0074 at 105 days, for (+) fibers: ##P-values versus WT: 0.0025 at 65 days and 0.0073 at 105 days (n = 5/genotype at 65 days and n = 4/genotype at 105 days, two-way ANOVA followed by Fisher's LSD post hoc test).
Glycolysis is regulated by a number of upstream and downstream components. Pyruvate is the end product of glycolysis and a downstream component in the glycolytic pathway that inhibits muscle PFK1 while glycogen synthase is a key enzyme that converts glucose to glycogen. Thus, we assessed pyruvate levels, glycogen synthase activity, and glycogen accumulation in the TA of SOD1G86R mice and WT littermates at the asymptomatic and symptomatic stages of disease. Pyruvate was 1.7-fold more concentrated in 65-day-old SOD1G86R mice than in age-matched WT littermates (Fig3B). By 105 days of age, symptomatic SOD1G86R mice had a significant reduction in pyruvate levels when compared to WT littermates. Changes in the expression of pyruvate levels in SOD1G86R mice occurred concurrently with altered activity of glycogen synthase and altered glycogen accumulation. At 65 days of age, SOD1G86R mice had decreased phosphorylation of glycogen synthase (Fig3C) and a corresponding increase in glycogen accumulation (Fig3D). By contrast, glycogen synthase phosphorylation in SOD1G86R mice at 105 days of age was dramatically increased, indicating the inhibition of its activity. The increased synthesis of glycogen and its subsequent accumulation was quantified in transverse sections of TA stained by periodic acid-Schiff (PAS) (Fig3D).
Pyruvate dehydrogenase kinase 4 up-regulation in glycolytic muscle tissue is an early event
In skeletal muscle, pyruvate levels are primarily governed by pyruvate dehydrogenase complex (PDH) activity, which itself is inhibited when phosphorylated by pyruvate dehydrogenase kinase 4 (PDK4). Thus, we assessed the expression levels of Pdk4 mRNA by RT–qPCR. As shown in Fig4A, at 65 days of age SOD1G86R mice had a 2.2-fold increase in Pdk4 mRNA levels in TA when compared to WT mice (Fig4A). At the end stage of disease, Pdk4 mRNA expression was 8.9-fold higher in SOD1G86R mice when compared to age-matched WT littermates. Noticeably, in the soleus muscle of SOD1G86R mice, Pdk4 expression was comparable to that of WT mice at 65 and 105 days of age (Supplementary Fig S3). By contrast, Pdk2 transcript levels were similar between SOD1G86R mice and WT littermates in TA and in soleus at 65 days of age, but decreased by 2- and 0.3-fold in these respective muscles at 105 days of age (Fig4A and Supplementary Fig S3). In SOD1G93A mice (Supplementary Fig S2C and D), Pdk4 mRNA levels were transiently increased by 50% at onset when mice develop signs of hindlimb weakness, prior to returning to control levels at end stage, while Pdk2 transcript levels were decreased by 50% from onset to end stage when compared to WT littermates. In muscle biopsies of definite ALS patients (Supplementary Fig S4), Pdk4 mRNA levels were increased 3-fold while Pdk2 mRNA levels remained unchanged when compared to controls.
Figure 4.
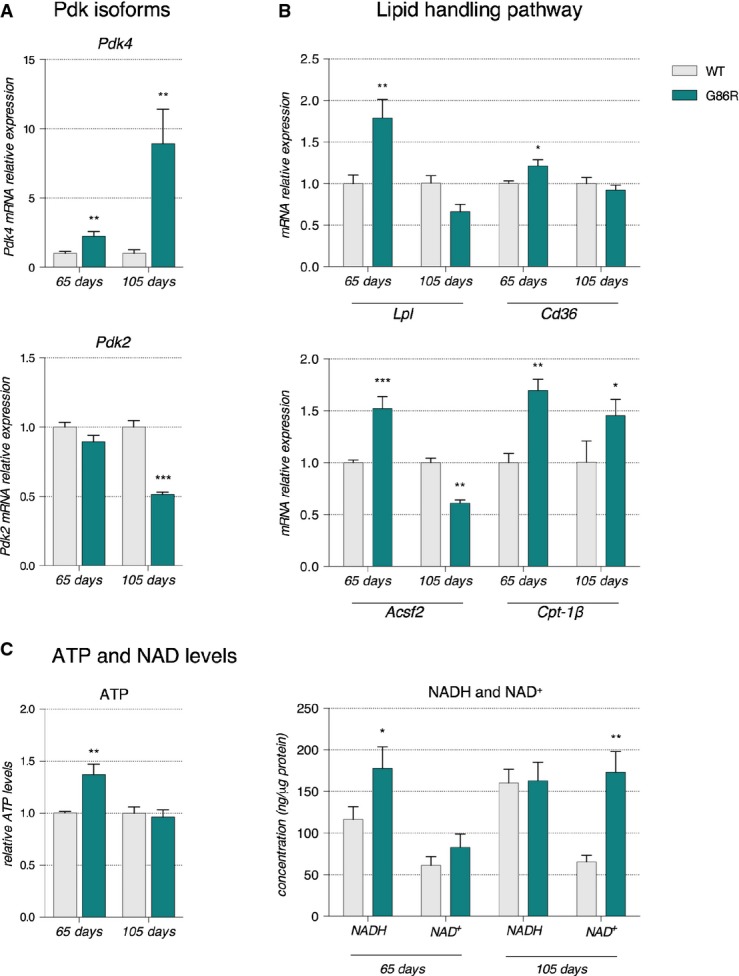
- Relative mRNA levels of Pdk4 and Pdk2 evaluated by qPCR at the indicated ages in tibialis anterior of WT and SOD1G86R mice. Graphs represent mean fold change ± from age-matched WT. Pdk4: **P-values versus WT: 0.014 at 65 days and 0.018 at 105 days; Pdk2: ***P-value versus WT < 0.0001 at 105 days. n = 7 and 8 for WT and SOD1G86R, respectively, at 65 days; n = 5/genotype at 105 days, two-way ANOVA followed by Fisher's LSD post hoc test.
- Relative mRNA levels of genes involved in lipid handling evaluated by qPCR at the indicated ages in tibialis anterior of WT and SOD1G86R mice. Graphs represent mean fold change ± SEM from age-matched WT. P-values versus WT: Lpl **P = 0.0009, Cd36 *P = 0.051, Acsf2 ***P < 0.0001 at 65 days, **P = 0.0059 at 105 days and Cpt-1β **P = 0.01 at 65 days and *P = 0.02 at 105 days (n = 6 and 7 for WT and SOD1G86R, respectively, at 65 days; n = 10 and 8 for WT and SOD1G86R, respectively, at 105 days, two-way ANOVA followed by Fisher's LSD post hoc test).
- Relative levels of (left) ATP and (right) NADH and NAD+ measured in total tibialis anterior homogenates of WT and SOD1G86R mice. Left: Graphs represent mean fold change ± SEM in ATP from age-matched WT. **P = 0.002 (n = 9 and 12 for WT and SOD1G86R, respectively, at 65 days; n = 10/genotype at 105 days, two-way ANOVA followed by Fisher's LSD post hoc test). Right: The amounts of NADH and NAD+ relative to protein content in whole tibialis anterior homogenates are represented as mean ± SEM. *P = 0.027 and **P = 0.001 (n = 5, Student's t-test).
PDK4 expression is stimulated by various parameters including skeletal muscle denervation, increased fatty acid (FA) use through β-oxidation (Jeong et al, 2012), and transcription factors peroxisome proliferator-activated receptors β/δ (PPARβ/δ) and forkhead Box O1A (FOXO1).
NMJ dysfunction could participate in Pdk4 up-regulation
To determine whether denervation could be responsible for the induction of Pdk4 expression seen in ALS mice and patients, we used two complementary paradigms: a mild sciatic nerve crush that induces a transient denervation, and a chronic denervation obtained by sciatic nerve axotomy in WT mice. After sciatic nerve crush, mice were observed for paralysis of the ipsilateral hindlimb, sacrificed at various times (3 h to 8 weeks post-crush) and gene expression levels were measured in TA ipsilateral and contralateral to the site of nerve crush. Supplementary Fig S5A shows the rapid loss of the innervated NMJs starting from 1 day post-crush (DPC) to 5 DPC and the progressive reinnervation already visible after 1 week post-crush (WPC). As shown in Supplementary Fig S5B, the expression of AChRα started to increase (2-fold induction) at 1 DPC, reached a plateau between 3 DPC and 1 WPC with a 40- to 60-fold induction, and then returned to control level by weeks 4 and 8. Pdk4 mRNA levels were increased by 50% during the early phase of synaptic destabilization with no significant changes on Pdk2 mRNA levels (Supplementary Fig S5B). By contrast, Pparβ/δ and Foxo1 (Supplementary Fig S5B) expression were rapidly and transiently stimulated by 2-fold. After sciatic nerve axotomy (Supplementary Fig S6), AChRα, Pdk4, Pparβ/δ, and Foxo1 were still induced after 2 weeks of chronic denervation in both TA and soleus muscle while Pdk2 mRNA levels were decreased. Collectively, these results show that NMJ destabilization and denervation could underlie Pdk4 induction in TA muscle observed in SOD1G86R mice.
Pdk4 up-regulation is associated with an increase of the lipid handling pathway
Hence, we sought to better understand the metabolic significance of Pdk4 up-regulation through RT–qPCR analyses of genes involved in lipid handling. When compared to WT littermates, 65-day-old SOD1G86R mice had a significant increase in the expression of genes encoding lipoprotein lipase (Lpl, 81.2%), Cd36 (18.7%), acylCoA synthetase (Acsf2, 50%), and carnitine palmitoyl transferase 1B (Cpt-1β, 70%) (Fig4B). At the end stage of disease, the expression of Lpl and Cd36 in SOD1G86R mice was comparable to that of WT littermates, while Acsf2 was decreased by 40% and Cpt-1β was increased by 45% (Fig4B). In SOD1G93A mice (Supplementary Fig S2E and F), Cpt-1β and Lpl were decreased at the onset stage of disease and stayed below control levels until disease end stage. Only at this latter stage were Pparβ/δ and Foxo1 mRNA levels significantly repressed or increased (Supplementary Fig S2G and H).
Increased expression of genes encoding an enzyme that hydrolyses triglycerides to facilitate the uptake of free fatty acids (LPL) (Mead et al, 2002), a membrane translocase that promotes FA entry into the cell (CD36), an enzyme that catalyses the conversion of FA to AcylCoA (ACSF2), and the rate-limiting enzyme for β-oxidation responsible for the FA transfer into the mitochondria (CPT-1B) (McGarry et al, 1983) in asymptomatic SOD1G86R mice suggests that fatty acids intake is increased into glycolytic muscle tissue when ALS occurs. Taken together with the increased expression of Pdk4, our data indicate that higher levels of β-oxidation exist in glycolytic muscle prior to denervation. Given that adenosine triphosphate (ATP) and reduced nicotinamide adenine dinucleotide (NADH) are two energetic substrates produced by β-oxidation and oxidative phosphorylation in the mitochondria that are known to stimulate PDK activity (for review, see Harris et al, 2002), we measured the variation in these molecules in the TA of SOD1G86R mice and WT littermates at 65 and 105 days of age. We evidenced a significant increase in ATP and NADH levels (1.37- and 1.49-fold change, respectively) in 65-day-old SOD1G86R mice compared to WT while NAD+ levels were comparable (Fig4C). Interestingly, ATP and NADH levels were similar between SOD1G86R mice and WT littermates at 105 days of age while NAD+ levels were increased 2.6-fold. Finally, mRNA levels of Pparβ/δ and Foxo1 were increased in 65-day-old SOD1G86R mice (Fig5A and B). Further, mRNA levels of citrate synthase, the first enzyme of the Krebs cycle, were comparable to WT at 65 days of age but significantly reduced at end stage (Fig5C). These data, together with the inhibition of glycolysis described in the previous section, clearly demonstrate that an early change in fuel preference from glucose toward lipids in glycolytic muscle fibers occurs before denervation in SOD1G86R mice.
Figure 5.
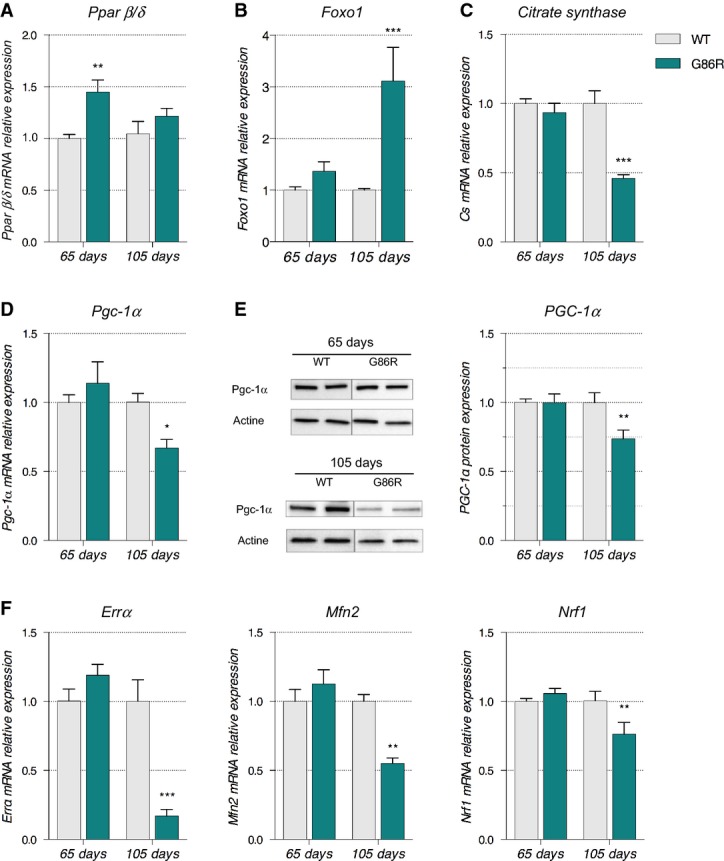
- A–D Relative mRNA levels of (A) Pparß/δ, (B) Foxo1, (C) citrate synthase, and (D) Pgc-1α were evaluated by qPCR at the indicated ages in tibialis anterior of WT and SOD1G86R mice. Graphs represent mean fold change ± SEM from age-matched WT. P-values versus WT: Pparβ/δ **P = 0.0016 at 65 days; Foxo1 ***P = 0.0001 at 105 days, citrate synthase ***P < 0.0001 at 105 days, Pgc-1α *P = 0.0104 at 105 days (n = 7 and 8 for WT and SOD1G86R, respectively, at 65 days; n = 5/genotype at 105 days, two-way ANOVA followed by Fisher's LSD post hoc test).
- E Representative Western blot of PGC-1α and respective actin that was used for normalization. PGC-1α protein levels in tibialis anterior muscle tissue are represented as mean fold change ± SEM from age-matched WT. **P-values versus WT: 0.02 (n = 6/genotype at 65 days; n = 5/genotype at 105 days, two-way ANOVA followed by Fisher's LSD post hoc test).
- F Relative mRNA levels of ERRα, Mfn2, and Nrf1 were evaluated by qPCR at the indicated ages in tibialis anterior of WT and SOD1G86R mice. Graphs represent mean fold change ± SEM from age-matched WT. P-values versus WT: ERRα ***P < 0.0001, Mfn2 **P = 0.002 and Nrf1 **P = 0.009 (n = 6–7 and 7–8 for WT and SOD1G86R, respectively, at 65 days; n = 5 and 6 for WT and SOD1G86R, respectively, at 105 days, two-way ANOVA followed by Fisher's LSD post hoc test).
The metabolic switch in glycolytic muscle occurs independent of PGC-1α
The processes that promote the mobilization and use of fatty acids for ATP synthesis during moderate exercise are subjected to multiple regulatory steps. Typically, increased oxidative capacity and lipid use in muscle is accompanied by a switch in muscle fiber subtype, a phenomenon that is facilitated by peroxisome proliferator-activated receptor gamma co-activator 1-alpha (PGC-1α), the master regulator of mitochondrial biogenesis and function (Wu et al, 1999; Lin et al, 2002). We thus analyzed the expression of PGC-1α in the TA of SOD1G86R mice. At 65 days of age, Pgc-1α mRNA and protein levels were similar between SOD1G86R and WT mice (Fig5D and E), whereas they were significantly decreased at 105 days of age in SOD1G86R mice. Importantly, at the end stage of the disease the decrease in PGC-1α protein levels correlated with a decrease in the mRNA expression of the main target genes of PGC-1α pathway, estrogen-related receptor α (ERRα), mitofusin 2 (Mfn2), and nuclear respiratory factor 1 (Nrf1) (Puigserver, 2005; Villena & Kralli, 2008) (Fig5E). ERRα mRNA expression was reduced by more than 5-fold, Mfn2 mRNA levels were decreased by 2-fold, and Nrf1 was decreased by 30% in SOD1G86R mice when compared to WT animals at 105 days (Fig5F). In addition, mitochondrial DNA quantification indicated a decreased number of mitochondria in TA of SOD1G86R mice toward the end stage of disease (Fig6A). Interestingly, this decrease in mitochondrial DNA was not observed in the soleus muscle. These data suggest that increased activation of the lipid oxidation pathways in skeletal muscle of SOD1G86R mice occurs independently of PGC-1α and that this metabolic change does not have the support of the mitochondrial machinery of the cell. Presumably, this would have deleterious effects due to accumulation of β-oxidation by-products and ROS (Bonnard et al, 2008). Indeed, glutathione peroxidase 1 (GPX1), an important indicator of oxidative stress, was increased in the TA but not the soleus of SOD1G86R mice at end stage of disease (Fig6B).
Figure 6.
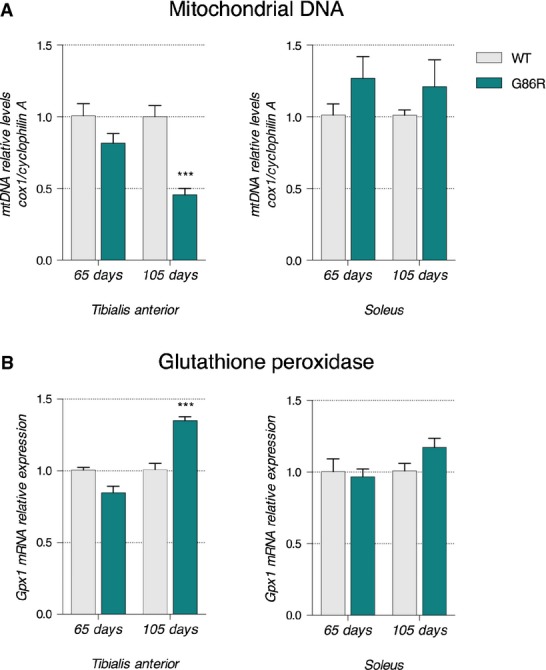
- Mitochondrial DNA (mtDNA) was quantified using qPCR. Relative mtDNA levels are expressed as the ratio between mitochondrial-encoded gene Cox1 and the nuclear-encoded gene cyclophilin A. Graphs represent mean fold change ± SEM from age-matched WT for tibialis anterior (left panel) and soleus (right panel) of WT and SOD1G86R mice. ***P < 0.0001 (n = 5 and 4 for WT and SOD1G86R, respectively, at 65 days; n = 6/genotype at 105 days, two-way ANOVA followed by Fisher's LSD post hoc test).
- Relative mRNA levels of Gpx1 were measured by qPCR at the indicated ages in tibialis anterior (left panel) and soleus (right panel) of WT and SOD1G86R mice. Graphs represent mean fold change ± SEM from age-matched WT. ***P < 0.0001 (n = 7 and 8 for WT and SOD1G86R, respectively, at 65 days; n = 9 and 8 for WT and SOD1G86R, respectively, at 105 days, two-way ANOVA followed by Fisher's LSD post hoc test).
Restoring metabolic equilibrium facilitates weight gain and delays the onset of motor symptoms and denervation in SOD1G86R mice
In order to ascertain whether decreased glycolytic capacity in SOD1G86R mice significantly impacts weight loss (due to the mobilization of fat) and muscle function and pathology that is commonly observed in ALS (Dupuis et al, 2011), mice were treated with dichloroacetate (DCA), a halogenated organic acid that inhibits the activity of PDK and facilitates the entry of pyruvate into the Krebs cycle and the oxidation of glucose. By inhibiting PDK and preventing PDH phosphorylation, we aimed to force metabolism toward glucose oxidation (Abdel-Aleem, 1996), thereby reversing the metabolic alterations observed in SOD1G86R mice, preventing weight loss, reducing the toxic effects of lipids on mitochondria, and delaying denervation in glycolytic muscle fibers. We administered DCA daily in drinking water from 60 to 95 days of age. At the beginning of treatment (T0), SOD1G86R mice in both treated (DCA) and non-treated (CT) groups were significantly leaner that WT mice (Supplementary Fig S7A). Over five weeks of treatment, SOD1G86R mice that received drinking water (CT) maintained their initial weight. By contrast, SOD1G86R mice receiving DCA increased their initial weight by 10.8%, an increase that was similar to that observed in CT WT mice over the same treatment period (Supplementary Fig S7A and B). DCA had no effect on the weight gain of WT animals (Supplementary Fig S7A and B).
Daily administration of DCA was able to reverse the changes in Pdk4, Pparβ/δ, and Foxo1 mRNA expression in SOD1G86R mice (DCA) when compared to non-DCA-treated SOD1G86R mice (CT, Fig7A–C). At the cessation of treatment, Pfk1, Acsf2, and citrate synthase mRNA levels in DCA-treated SOD1G86R mice were comparable to DCA-treated WT mice (Fig7D–F), indicating successful restoration of glycolysis and activation of the Krebs cycle. Importantly, CT SOD1G86R mice presented with significantly reduced Pfk1 and citrate synthase expression when compared to DCA-treated SOD1G86R mice and/or CT WT mice. DCA treatment was also able to preserve the expression of Pgc-1α and its target gene Mfn2 in DCA-treated SOD1G86R mice at levels comparable to that seen in CT WT and DCA-treated WT mice (Fig7G and H). The increase in the expression of genes involved in mitochondrial biogenesis was accompanied by a decrease in the expression of the Gpx1 (Fig7I). Notably, and in support of our results above, 95-day-old CT SOD1G86R mice presented with a significant decrease in the expression of Pgc-1α and Mfn2 mRNA and an increase in the expression of Gpx1 mRNA (Fig7G–I). Collectively, these data suggest that DCA is able to restore glycolytic function while decreasing oxidative stress in glycolytic muscle of SOD1G86R mice.
Figure 7.
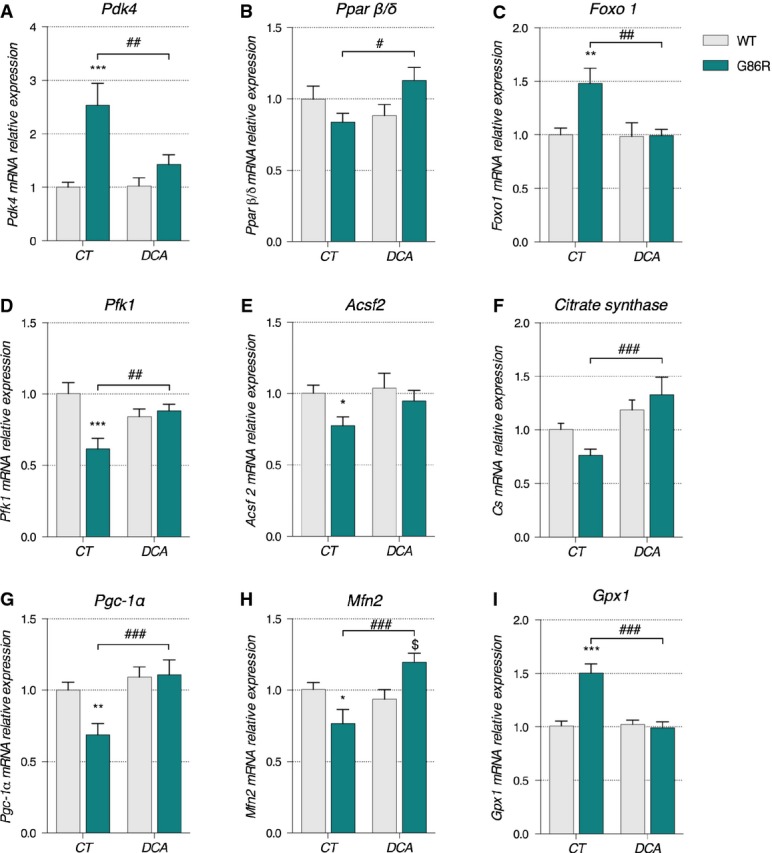
- A–I Relative mRNA levels of (A) Pdk4, (B) Pparβ/δ, (C) Foxo1, (D) Pfk1, (E) Acsf2, (F) citrate synthase, (G) PGC-1α, (H) Mfn2, and (I) Gpx1 were evaluated by qPCR in tibialis anterior of control (CT) or DCA-treated (DCA) WT and SOD1G86R mice. Graphs represent mean fold change ± SEM from CT WT group. P-values versus WT: Pdk4 ***P = 0.002 and ##P = 0.0039, Pparβ/δ #P = 0.0178, Foxo1 **P = 0.0033 and ##P = 0.0038, Pfk1 ***P = 0.0002 and ##P = 0.0080, Acsf2 *P = 0.0437, citrate synthase ###P = 0.0004, Pgc-1α **P = 0.0084 and ###P = 0.0009, Mfn2 *P = 0.0272, $P = 0.0145 and ###P = 0.0002 and Gpx1 ***P < 0.0001 and ###P < 0.0001 (n = 9/genotype in CT groups, n = 9 and 8 for WT and SOD1G86R, respectively, in DCA group, two-way ANOVA followed by Fisher's LSD post hoc test).
At a functional level, DCA was able to almost completely preserve muscle strength. While CT SOD1G86R mice lost 30% of their grip strength, DCA-treated SOD1G86R mice only lost 8% of their grip strength when compared to initial grip force at the initiation of treatment (Fig8A). This increased grip strength was associated with an increase in both oxidative and glycolytic muscle fiber size in TA (Supplementary Fig S7D and E). Analysis of mRNA expression of muscle atrophy markers showed a more modest improvement (Fig8B). Murf-1 mRNA expression was reduced from a 1.6-fold increase in the non-treated CT SOD1G86R mice to 1.3-fold increase in DCA-treated SOD1G86R mice. Similarly, Atg-1 mRNA expression was decreased from a 1.7-fold increase in CT SOD1G86R mice to a 1.4-fold increase in DCA-treated SOD1G86R mice. DCA treatment also prevented the increase in the expression of the denervation markers (Fig8C). The increase in expression of AChRα mRNA in DCA-treated SOD1G86R mice was only 3.2-fold as compared to an 8.8-fold increase in CT SOD1G86R mice. AChRγ mRNA was increased by 3.9-fold in DCA-treated SOD1G86R mice as compared to a 15.87-fold increase measured in CT SOD1G86R mice. Lastly, MuSK gene expression was also lower following treatment with DCA, decreasing from a 2-fold increase in CT SOD1G86R mice to a 1.3-fold increase in DCA-treated SOD1G86R mice. WT mice treated with DCA did not present with any modifications of these atrophy or denervation markers. Altogether, these results demonstrate that by facilitating the equilibrium between glucose and lipid oxidation through the administration of DCA, we are able to promote weight gain, restore mitochondrial gene expression, improve muscle strength, and decrease the expression of denervation markers in SOD1G86R mice.
Figure 8.
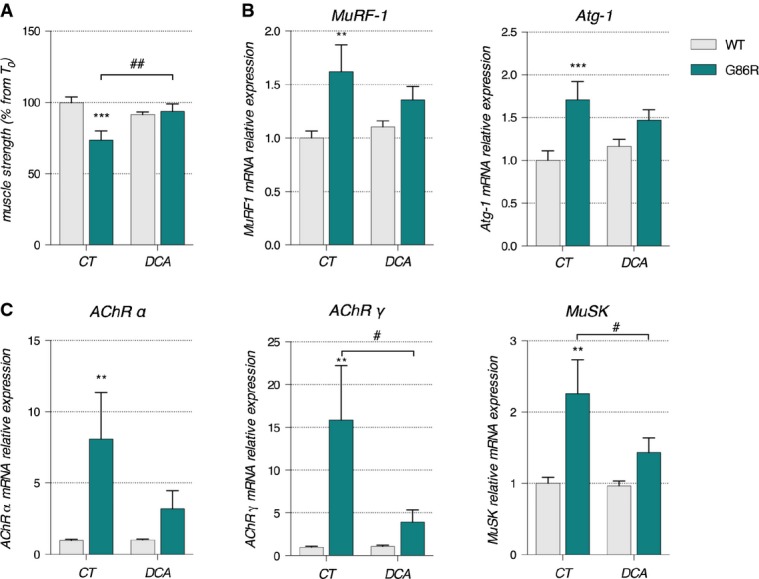
- Grip strength is represented as mean of percent from T0 for each experimental group ± SEM. ##P = 0.0045 and ***P = 0.0003 (n = 9/genotype in CT groups, n = 9 and 8 for WT and SOD1G86R, respectively, in DCA group, two-way ANOVA followed by Fisher's LSD post hoc test).
- Relative mRNA levels of muscular atrophy markers Murf1 and Atg-1 were measured by qPCR in tibialis anterior of control (CT) or DCA-treated (DCA) WT and SOD1G86R mice. Graphs represent mean fold change ± SEM from CT WT group. **P = 0.0079 and ***P = 0.0018 (n = 9/genotype in CT groups, n = 9 and 8 for WT and SOD1G86R, respectively, in DCA group, two-way ANOVA followed by Fisher's LSD post hoc test).
- Relative mRNA levels of denervation markers AChRα, AChRγ, and MuSK were measured by qPCR in tibialis anterior of control (CT) or DCA-treated (DCA) WT and SOD1G86R mice. Graphs represent mean fold change ± SEM from CT WT group. **P = 0.015 for AChRα, #P = 0.028 and **P = 0.074 for AChRγ, #P = 0.042 and **P = 0.0029 for MuSK (n = 9/genotype in CT groups, n = 9 and 8 for WT and SOD1G86R, respectively, in DCA group, two-way ANOVA followed by Fisher's LSD post hoc test).
Discussion
Here, we provide evidence of a change in the metabolic capacity of glycolytic muscle in SOD1G86R mice. A switch from glucose metabolism to lipid metabolism occurs early in the disease process and prior to any detectable motor and clinical (EMG alteration) symptoms. By improving glycolytic capacity in SOD1G86R mice through administration of DCA, we promoted a delay in the onset of motor symptoms and amelioration of muscle denervation and atrophy. Thus, we demonstrate for the first time that an early switch to lipid metabolism in skeletal muscle may underlie early pathological mechanisms associated with NMJ destabilization in ALS.
The decreased capacity for SOD1G86R mice to endure acute physical exercise that solicits anaerobic metabolism in muscle occurred before any measurable muscle weakness or overt denervation (Figs1 and 2). This low resistance to intense exercise contrasted their enhanced endurance capacity during acute aerobic exercise. This observation suggests that SOD1G86R mice acquire new properties in skeletal muscle that enhance global aerobic capacity and promote endurance ability. It is plausible that altered glucose and insulin responses in SOD1G86R mice (Supplementary Fig S1) might underlie this change in exercise capacity since insulin plays a critical role in driving glucose uptake into skeletal muscle for use as an energy substrate. Indeed, high incidences of glucose intolerance have been observed in patients diagnosed with sporadic ALS (Pradat et al, 2010). However, as basal glucose uptake in extensor digitorum longus (EDL: another glycolytic muscle) of the SOD1G93A mouse model of ALS is normal before overt denervation (Smittkamp et al, 2014), it would seem unlikely that altered insulin sensitivity underlies the metabolic changes observed in this study.
Endurance exercise is also supported by slow-twitch oxidative type I fibers while intense exercise requires movements involving strength and speed that are generated by fast-twitch glycolytic type IIb fibers (Bassel-Duby & Olson, 2006). Given that a switch in fiber type from glycolytic to oxidative fibers has been described in ALS patient muscle biopsies (Telerman-Toppet & Coërs, 1978), and in the SOD1G93A mouse model of ALS (Atkin et al, 2005; Hegedus et al, 2008; Deforges et al, 2009), the observed alteration in exercise capacity in SOD1G86R mice might also reflect a switch of muscle fiber type. In line with this, enhanced aerobic capacity is typically observed after endurance training, and this occurs concurrent with measurable changes in fiber type composition (Pette & Staron, 2001).
PFK1 is the rate-limiting enzyme of the glycolysis, and an increase in glycogen synthase activity and glycogen accumulation in skeletal muscle is characteristic of a muscle that is subjected to endurance training (Vestergaard, 1999). Thus, the increase in endurance capacity in SOD1G86R mice mirrors a profound alteration of fuel preference in muscle fibers. In accordance with this, we observed a progressive decrease of PFK1 activity, and an increase in glycogen synthase activity and glycogen accumulation in skeletal muscle. The initial decrease in PFK1 activity in SOD1G86R mice may be an adaptive response to the progressive accumulation of pyruvate and increased FA uptake, two well-known potent inhibitors of PFK1 (Massao Hirabara et al, 2003). Furthermore, as the entry of glucose into muscle fibers in ALS mice is not affected early in disease (Dupuis et al, 2004; Smittkamp et al, 2014), our data suggest that glucose is rerouted toward glycogen stores rather than being used as an immediate energy source. By the end stage of disease, reduced activities of PFK1 and glycogen synthase, together with an increase of glycogen stores and reduced levels of pyruvate, demonstrate inhibition of the glycolytic pathway. Collectively, these observations suggest that glycolytic muscle is no longer able to mobilize glycogen stores to produce energy and that the inhibition of glycolysis appears to originate downstream of PFK1 (Fig9).
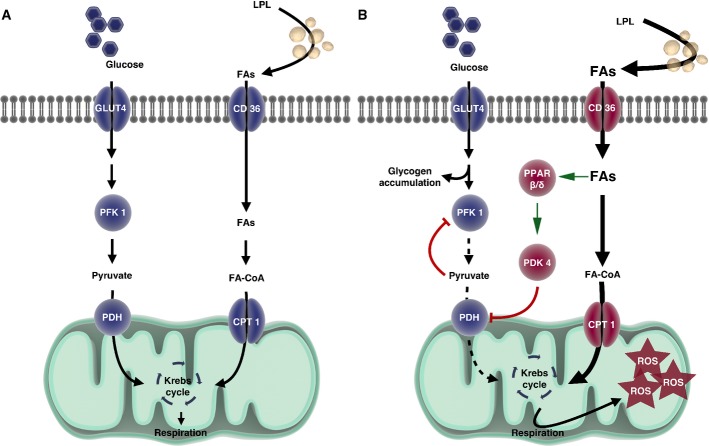
Figure 9.
- Under normal conditions in WT mice, both glucose and lipids enter the cell and are used as cellular fuels. In this situation, both pathways are used and are driven by PDK4 according to needs and fuel availability.
- In the case of ALS, metabolic flexibility is lost because of chronically increased PDK4 and subsequent inhibition of PDH and PFK1 leading to glycogen accumulation. Increased lipid use through β-oxidation that can only function under aerobic conditions may underlie the greater endurance capacity in SOD1G86R mice. With time, the cell produces more reactive oxygen species, thereby inducing cellular damage.
Data information: CD36, CD36 antigen/fatty acid translocase, CPT1, carnitine palmitoyl transferase 1, FAs, fatty acids, FA-CoA, acyl-fatty acids, GLUT4, glucose transporter 4, LPL, lipoprotein lipase, PDH, pyruvate dehydrogenase complex, PDK4, pyruvate dehydrogenase kinase 4, PFK1, phosphofructokinase 1, ROS, reactive oxygen species. Drawing was performed with the website Somersault1824 (http://www.somersault1824.com).
In contrast to inhibition of glycolysis in SOD1G86R mice, the lipid pathway was stimulated at 65 days of age and remained functional until the end stage of disease (Fig4B and C). It is known that increased endurance should correlate with increased release of fatty acids from lipid stores, and enhanced uptake by muscle tissue (Talanian et al, 2010). Previous observations of decreased fat pad mass and respiratory quotient at an early stage in SOD1G86R mice (Dupuis et al, 2004) and increased lipid clearance in these mice (Fergani et al, 2007) are indicative of increased lipid use. Moreover, in patients diagnosed with sporadic ALS, Pradat and colleagues reported increased circulating free fatty acids (FFAs) (Pradat et al, 2010). Altogether, these observations indicate that muscle tissue of SOD1G86R is the potential site of abnormal lipid consumption. The question raised from these observations was whether the more ‘efficient’ oxidation during exercise is due to a given group of muscles that work more efficiently or whether other groups of muscles are becoming oxidative to participate in the exercise task. The latter appears to occur since fiber type switching toward more oxidative metabolism (Deforges et al, 2009), and increased expression of genes encoding enzymes involved in lipid metabolism (Dupuis et al, 2004; Fergani et al, 2007) is observed at later, symptomatic stages of disease in ALS mouse models. In line with this, we show an early increase in the gene expression of important components in lipid mobilization and uptake (Lpl, Cd36, ACSF2, and Cpt-1B, Fig4B), and increased β-oxidation by-products (ATP and NADH at 65 days) that activate PDK4 and inhibit PDH activity (Denton et al, 1975) in fast-twitch glycolytic muscle.
PDK4 appears to play a pivotal role in the switch in fuel preference by orchestrating substrate competition in SOD1G86R glycolytic muscle fibers. In skeletal muscle, PDK4 is the most highly expressed pyruvate dehydrogenase kinase isoform and is considered to be a critical regulator of pyruvate dehydrogenase (PDH) activity (Bowker-Kinley et al, 1998). In this study, we show that Pdk4 expression is induced not only in two mutant SOD1 mouse models but also in sporadic ALS patients (Fig1, Supplementary Figs S2 and S4). These data show that the induction of Pdk4 expression is not specific to SOD1 mutations but is rather an ALS-specific phenomenon. By phosphorylating PDH, PDK4 completely inhibits the entry of pyruvate into the Krebs cycle, thus hampering glucose oxidation (for review, see Holness & Sugden, 2003). PDH and PDK4 are known to act as metabolic homeostat in response to energy imbalance. Indeed, PDK4 transcription is increased during prolonged exercise, after both short-term high-intensity and prolonged low-intensity exercise or during fasting, situations that represent metabolic states where the whole body glucose availability is in deficit (Spriet et al, 2004; Watt et al, 2004; Jeong et al, 2012). Pdk4 expression is controlled directly or indirectly by various transcription factors/transcriptional coactivators or stimuli, including PPARβ/δ, FOXO1, PGC-1α, ERRα, or FAs. In C2C12 mouse myoblasts, nutrient deprivation induces Pdk4 gene expression (Furuyama et al, 2003). In rat muscle tissue, triglyceride infusion leads to increased plasma FA and increased expression of Pdk4 mRNA (Kim et al, 2006). Moreover, it has been shown that in response to increased entry of FA in skeletal muscle or to fasting, induction of PPARβ/δ stimulates FOXO1 transcription, which in turn activates Pdk4 expression (Nahlé et al, 2008). Here, we show that Pdk4 activation might occur in response to the increase in Pparβ/δ and Foxo1 mRNAs, rather than via the classical transcription factors PGC-1α/ERRα. If this were the case, then an increase of FA release due to the induction of Lpl and Acsf2 would stimulate PDK4 expression via PPARβ/δ and FOXO1, which would in turn facilitate FA oxidation by conserving pyruvate for oxaloacetate formation to allow entry of acetyl-coA into the Krebs cycle (Fig1). In SOD1G93A mice, although induction of Pdk4 expression is detected at the onset (63–75 days old), the global metabolic profile of the mice differs from the one found in SOD1G86R mice. It is highly likely that the observed differences are a result of profound mitochondrial alterations which have been described in the SOD1G93A mice as early as post-natal day 30 (for review, see Vinsant et al, 2013a, b).
The question of the role of NMJ destabilization in the metabolic switch clearly remains open. We showed here that synaptic alteration/dysfunction obtained 24 h after sciatic nerve crush is sufficient to induce an early but transient increase in Pdk4 mRNA, which then returns to initial levels despite a sustained increase in the levels of AChRα mRNA, an accepted marker of NMJ denervation. In the SOD1G86R, Pdk4 mRNA is induced before any detectable sign of denervation by EMG and before the increased expression of the denervation makers used in this study. However, we cannot exclude a lack of sensitivity of our techniques. In the SOD1G93A mice, denervation events have been detected at 30 days of age through a detailed study of the NMJ by electron microscopy (Vinsant et al, 2013a,b), and impaired neuromuscular transmission has been detected at 28–42 days of age (Rocha et al, 2013), long before the onset of motor symptoms. Here, we showed that, at the same period, Pdk4 mRNA levels are comparable to those found in WT mice. Altogether, these data show that NMJ dysfunction or destabilization might participate to the Pdk4 mRNA induction.
Another interesting aspect of the mechanism described here is the consequence of prolonged use of lipids as an energy substrate. Increased β-oxidation of fatty acids leads to the generation of lipid by-products that contribute to lipotoxicity and ROS production (Zhang et al, 2010; Aon et al, 2014). ROS accumulation in muscle tissue of SOD1G86R mice is an early event in the course of the pathology that precedes overt signs of denervation (Halter et al, 2010). Here, we show an up-regulation of Gpx1, an indicator of ROS accumulation, in the TA but not in the soleus muscle of SODG86R mice in the advanced stages of the disease. It is expected that this chronic/long-term activation of lipid use would have toxic effects on mitochondria (Bonnard et al, 2008), which might explain the observed decrease of citrate synthase (Fig5C), the decrease in the expression of genes responsible for mitochondrial dynamics, and the reduction in the quantity of mtDNA specific to glycolytic muscle (Fig6). Indeed, rescuing muscle mitochondria in a mouse model for ALS through the overexpression of muscle-specific PGC-1α has been shown to prevent muscle atrophy and improve mitochondrial function (Da Cruz et al, 2012). Although PGC-1α is often considered as the main ‘fiber type regulator’ that contributes to muscle physiological plasticity under normal physiological conditions, PGC-1α is down-regulated with disease progression in our SOD1G86R mice and can therefore not account for the induction of Pdk4. Alternatively, muscle-specific over-expression of PPARβ/δ in skeletal muscle results in a greater number of oxidative type 1 fibers (Luquet et al, 2003), and over-expression of constitutively active PPARβ/δ results in mitochondrial biogenesis and a shift from fast-twitch to slow-twitch fibers (Wang et al, 2004). Thus, the early switch of fuel preference in ALS mice could be driven by the increased expression of PPARβ/δ. Altogether, these findings show that metabolic imbalance in muscle fibers of SOD1G86R mice is an early event. As glycolytic muscle fibers become progressively unable to use glucose as an energy substrate, they switch to lipid use to maintain a sufficient amount of energy supply. Intriguingly, this mechanism is specific to glycolytic muscle fibers as the deregulations observed in the TA differ from that seen in the oxidative soleus muscle.
Because PDK4 appears to be a key player in the switch in fuel preference by suppressing glucose utilization, we used the halogenated carboxylic acid DCA, a specific inhibitor of PDK, to restore glucose metabolism and muscle metabolic plasticity. Indeed, maintaining PDH in its unphosphorylated active form will re-activate PDH function and recover glucose metabolism by restoring glucose oxidation (Whitehouse & Randle, 1973). In a model of statin-induced muscle atrophy, DCA treatment has been shown to increase glucose oxidation in type IIb muscle fibers and reduce the expression of markers of protein degradation (Mallinson et al, 2012). This is in line with the results presented here. In this study, we demonstrate that DCA treatment exerts protective effects on muscle fibers in the SOD1G86R mice by restoring the ability of glycolytic muscle to use glucose as fuel. When compared to non-DCA-treated SOD1G86R mice, those supplemented with DCA show a decrease in the mRNA expression of Pdk4, Foxo1, and Pparβ/δ in parallel with an induction of Pfk1 and citrate synthase. Moreover, DCA-treated SOD1G86R mice also had decreased expression of denervation and atrophy markers when compared to untreated SOD1G86R mice. At a functional level, this was reflected by a preservation of muscle strength and the presence of larger muscle fibers in DCA-treated SOD1G86R mice compared to untreated SOD1G86R mice. DCA treatment in SOD1G86R mice also exerted beneficial metabolic effects in the whole organism by stimulating weight gain during disease development, which is similar to what has been observed after DCA treatment of statin-induced myopathy in mice (Mallinson et al, 2012). It is important to note that DCA treatment was able to restore some of the biochemical parameters that govern fuel use in SOD1G86R mice (Fig7). We observed an up-regulation of mRNA expression of Pgc-1α and Mfn2, a PGC-1α target gene that is involved in mitochondrial dynamics. While DCA has not been shown to directly regulate the PGC-1α pathway, it has been shown to reverse the inhibition of PGC-1α and mitochondrial biogenesis that is induced in myotubes by chronic inhibition of glucose oxidation with pyruvate (Philp et al, 2010). The beneficial effects on mitochondrial metabolism following DCA treatment in SOD1G86R mice were also reflected by comparable levels of Gpx1 in DCA-treated SOD1G86R mice and CT- and DCA-treated WT mice. Collectively, these data show that restoration of metabolic equilibrium in glycolytic muscle fibers is able to protect muscle mitochondria and prevent oxidative stress, while also preventing denervation and atrophy.
DCA has previously been used in the SOD1G93A mouse model of ALS (Miquel et al, 2012). By limiting pyruvate turnover to lactate and facilitating the entry of pyruvate into the Krebs cycle, DCA reduced astrogliosis and motor neuron death (Miquel et al, 2012). This indicates that PDK activation may be a common mechanism in astrocytes and muscle. Interestingly, Miquel and colleagues also demonstrated that DCA-treated SOD1G93A mice presented with a marked improvement in the structure of NMJs in the extensor digitorum longus (glycolytic muscle fiber) but not soleus (oxidative muscle fiber). Taken together with our data showing an effect of DCA in restoring glycolysis in muscle, one can conclude that DCA treatment exerts its protective effects through stabilizing the NMJ. However, based on the action of DCA on both muscle and astrocytes, we cannot conclude whether the normalization of glycolytic muscle metabolism is sufficient in itself to maintain the positive effect observed at the NMJ. However, our data provide convincing evidence that DCA treatment promotes the use of glucose as the preferred energy substrate (instead of lipids), thereby preventing denervation and maintaining function at NMJ.
In conclusion, our study provides compelling evidence to support a dramatic change in glycolytic muscle metabolism that specifically alters muscle metabolic plasticity in highly susceptible glycolytic fibers. Importantly, these metabolic alterations occur very early in the course of the disease. These data, in combination with our sciatic nerve crush and axotomy experiments, suggest that glycolytic defects might be due to additional events distinct from denervation. However, early changes of synaptic functionality might contribute to early stages of the metabolic switch, which in turn could contribute to further NMJ changes and a self-propagating process. Importantly, since altered metabolic plasticity might underlie the susceptibility of glycolytic fibers to denervation while limiting the capacity for muscle to become re-innervated, this would have detrimental effects on the rate of disease progression. By demonstrating the involvement of multiple cell types in ALS pathology and identifying a possible common metabolic thread between glycolytic muscle and astroglia in ALS pathogenesis, our work further exemplifies the complexity of ALS. Finally, our work has important therapeutic implications as we present evidence to suggest that by improving metabolic function in murine ALS animal model through DCA, it is possible to improve motor function, maintain muscular integrity, and delay denervation.
Materials and Methods
Ethics statement
All experiments performed with mice followed current European Union (Directive 2010/63/EU) and Australian regulations. They were approved by the regional ethics committee CREMEAS 35 under number AL/01/20/09/12 and by The University of Queensland Animal Ethics Committee (ethics number SBMS/562/12/MNDRIA). They were performed in accordance with national guidelines and in strict compliance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health (USA) by authorized investigators.
For human biopsies, the study was approved and performed under the ethical guidelines issued by our institution (University Hospital of Strasbourg) for clinical studies. The diagnostic procedures were conducted according to the Strasbourg University Hospital Ethical Committee, and informed written consent was obtained from all patients.
Muscle biopsy collection
We studied biopsies from the left deltoid muscle of eleven patients with sporadic ALS. According to the El Escorial criteria, all patients had definite ALS. The control group included seven patients subjected to a standard surgical diagnosis procedure without significant neurological history. All patients gave written informed consent before biopsy. Tissues were immediately frozen in liquid nitrogen and stored at −80°C until use.
Animals
FVB/N males overexpressing murine SOD1 with the G86R mutation or C57/Bl6 males overexpressing human SOD1 with the G93A mutation [B6.Cg-Tg(SOD1-G93A)1Gur/J] were genotyped as described previously (Gurney et al, 1994; Ripps et al, 1995). Wild-type littermates were used as controls. SOD1G93A mice were studied at predefined stages of disease progression (Ngo et al, 2012). Male Thy1-YFP mice on FVB background (Feng et al, 2000) were used for direct identification of presynaptic terminals after nerve crush. Mice were group-housed (2–5 per cage) in a temperature- and humidity-controlled environment at 23°C and under a 12-h light/dark cycle. Mice had access to water and regular A04 chow ad libitum. Mice with a body weight outside of the standard at the time of the selection were excluded from the experiments. Blinded investigators were employed to minimize the effect of subjective bias when assessing results.
Exercise paradigms
The week before starting the experiment, all animals were acclimated to the treadmill exercise (Treadmill Control, Letica, Spain) by running at 25 cm/s with a 5° inclination for 5 min for 3 days. Mice were tested at 65–66 days of age.
Intense anaerobic exercise
A maximal incremental test was carried out. The incline was set at + 10° and the speed at 40 cm/s and was maintained at this rate for 2 min. The speed was then increased by 3 cm/s every 90 s until exhaustion of the animal. The speed at which each mouse stopped running was considered to be the maximal running speed (Vmax).
Low-intensity endurance exercise
To determine maximal endurance capacity, a rectangular test was established. All mice ran at 80% of the Vmax attempt during the maximal incremental test. The incline was set at + 10°, and after 2 min of acclimation at 40 cm/s, the speed was maintained at 80% of the Vmax until exhaustion.
The criterion for exhaustion was a time of 5 s spent on the electrical grid without running. Blood samples from the tip of the tail were obtained immediately at the end of exercise to measure blood lactate using a lactate pro-LT device (Lactate Pro LT-1710, Arkray®, China).
Muscle grip strength
Muscle grip strength was measured using a strength meter (Bioseb Grip test, Bioseb, France). Animals were placed over a metallic grid that they instinctively grab to stop the involuntary backward movement carried out by the manipulator until the pulling force overcomes their grip strength. Each animal was pulled over the entire length of the metallic grid until it lost its grip. Grip strength, expressed in Newton, was recorded over three trials for each animal in each test session. The maximal grip strength was obtained by averaging the three grip strength scores for each animal. All recordings were performed by the same blinded investigator to minimize variability in the experimental procedure.
Electromyography
All recordings were performed with a standard EMG apparatus (Dantec, Les Ulis, France) in accordance with the guidelines of the American Association of Electrodiagnosis Medicine (AAEM). Mice were anesthetized with 100 mg/kg ketamine chlorhydrate and 5 mg/kg xylazine and maintained at 36°C over a thermostatic blanket. In order to minimize variability, all recordings were performed by the same blinded investigator. Recordings were monitored for 2 min with a concentric needle electrode (9013S0011, diameter 0.3 mm; Medtronic, USA) inserted into the gastrocnemius muscle. A monopolar needle electrode (9013R0312, diameter 0.3 mm; Medtronic) was inserted into the tail of the mouse to ground the system. Recordings showing voluntary activity were discarded. Spontaneous activity (mainly fibrillations) characteristic of muscle denervation was differentiated from voluntary activity (regular discharges that disappear with muscular relaxation) by visual and auditory inspection. Spontaneous activity with a peak-to-peak amplitude of at least 50 μV was considered to be significant.
Glucose tolerance test and insulin tolerance test
65-day-old male transgenic and non-transgenic mice were fasted for 18 h (starting at 6 PM) prior to the glucose tolerance test (GTT) or fasted for 4 h (starting at 9 AM) prior to the insulin tolerance test (ITT). Blood glucose levels were evaluated using a commercial FreeStyle Papillon InsuLinx glucometer (Abbot, France). Blood was drawn from a small incision at the tip of the tail. For GTTs, initial blood glucose was measured prior to an IP injection of 2 g/kg body mass of glucose. For ITTs, insulin from bovine pancreas (Sigma-Aldrich, USA) was injected IP (0.5 U/kg body mass) after initial blood glucose was measured. Changes in blood glucose were followed for 120 min with measurements taken every 15 min for both GTTs and ITTs. For each mouse, blood glucose was expressed as the percentage of initial blood glucose concentration (T0).
Sciatic nerve crush and axotomy
Axotomy of the sciatic nerve was performed on 8- to 9-week-old non-transgenic FVB/N male mice. Sciatic nerve crush was performed on 8- to 9-week-old non-transgenic or Thy1-YFP male mice on a FVB background. Mice were anesthetized by intraperitoneal injection of 100 mg/kg ketamine chlorhydrate and 5 mg/kg xylazine. The sciatic nerve was exposed at mid-thigh level and either crushed with a fine forceps for 30 s (mild nerve crush) or sectioned using microscissors (axotomy). For the sham animals, skin was opened and the sciatic nerve was exposed without additional manipulation. The skin incision was sutured, and mice were allowed to recover. Contralateral hindlimbs served as control. The efficiency of nerve crush was confirmed 24 h after injury by gait abnormalities and defects in paw flexion when the mouse was held by the tail. Mice were sacrificed by lethal injection of pentobarbital at different time points following the surgical intervention. Muscles were dissected, snap-frozen for biochemistry (FVB/N mice), or fixed with 4% buffered paraformaldehyde for 30 min for NMJ analysis (Thy1-YFP mice).
NMJ analysis
Fixed muscles from Thy1-YFP mice were cut into bundles. Bundles were incubated 1 h with tetramethyl rhodamine-conjugated α-bungarotoxin (αBGT, 1 μg/ml in PBS; Sigma). Fluorescence staining was monitored with a laser-scanning microscope (confocal Leica SP5 Leica Microsystems CMS GmbH). Z-stacks of 2-μm optical sections were analyzed using ImageJ freeware (http://rsbweb.nih.gov/ij/).
Dichloroacetate treatment
The pharmacological treatment consisted in daily administration of dichloroacetate (DCA; Sigma-Aldrich) in drinking water at a concentration corresponding to a daily dose of 500 mg/kg body mass as previously described (Miquel et al, 2012). The concentration was calculated based on a predicted water intake of 5 ml/day/animal (Bachmanov et al, 2002). For each genotype, male wild-type and SOD1G86R littermate mice were randomly allocated into experimental groups. Mice with a body weight outside of the standard at the time of the selection were excluded. Water intake was carefully monitored throughout the duration of the experiment. Standard drinking water was used as a control (CT). Mouse weights were monitored weekly by an investigator who was blinded to mouse genotypes and treatment groups.
Quantitative RT–PCR
Frozen muscle samples were homogenized in 1 ml/100 mg tissue TRIzol reagent (Invitrogen, USA) together with a stainless bead. Two 3-min homogenization cycles were performed in a TissueLyser (Qiagen, Germany) at 30 Hz. RNA was extracted using chloroform/isopropyl alcohol/ethanol and stored at −80°C. One microgram of total RNA was used to synthesize cDNA using Iscript reverse transcriptase (Bio-Rad, USA) and oligo-dT primer as specified by the manufacturer. Gene expression was measured using the 2× SYBR green SsoAdvanced reagent (Bio-Rad) according to the manufacturer's instructions on a Bio-Rad iCycler. PCR was performed under optimized conditions as follows: 95°C denaturation for 30 s, followed by 40 cycles of 10 s at 95°C and 30 s at 60°C. The extended list of primers (Eurogentec, Belgium) is provided in Supplementary Table S1. Relative expression was achieved by calculating the ratio between the cycle number (Ct) at which signal crossed a threshold set within the logarithmic phase of the gene of interest and that of TBP housekeeping gene. Ct values were means of duplicates.
Quantification of mitochondrial DNA
Snap-frozen tissue was digested in KTT buffer (Tris 10 mM pH 9, Triton X-100 0.1%, KCl 50 mM) with 2% proteinase K (Sigma-Aldrich) overnight at 54°C under constant agitation. Proteinase K was inactivated at 100°C for 5 min. RNA was degraded with 0.3 μg/μl RNase for 1 h at 37°C. Total DNA was extracted using a mix of Roti-Phenol reagent (Roth, USA), chloroform, and isoamyl alcohol (25/24/1). DNA was quantified using RT–qPCR (initial denaturation step at 98°C for 2 min, followed by 40 cycles of 10 s at 98°C and 20 s at 62°C). The relative mtDNA levels were calculated by normalizing the relative expression of mitochondrial Cox1 to the relative expression of the nuclear cyclophilin A. Primer sequences are provided in Supplementary Table S1.
Western blotting
Snap-frozen muscle tissue was pulverized in a TissueLyser (Qiagen) for 2 × 20 s under liquid nitrogen using stainless steel beads. Tissue powder was homogenized in RIPA lysis buffer (50 mM Tris pH 7.4, 150 mM NaCl, 1 mM EDTA, 1% Triton X-100, 0.1% SDS, 0.5% sodium deoxycholate) at 1 ml/100 mg tissue containing 1:100 protease inhibitor cocktail (Calbiochem, USA) and phosphatase inhibitor cocktails 2 and 3 (Sigma-Aldrich, Germany). Determination of protein concentration was carried out using a BCA Assay Reagent Kit (UP95424 Uptima, France). Protein was denaturated by boiling, resolved by sodium dodecyl sulfate–polyacrylamide gel electrophoresis and transferred to 2-μm nitrocellulose membranes (Bio-Rad, France) using a semi-dry Transblot Turbo system (Bio-Rad, France). After using a chemiluminescent blocker (Millipore, France), membranes were probed with primary antibodies against Glycogen Synthase Rabbit mAb (Cell Signaling; Cat#3886; 1:500), Phospho-Glycogen Synthase Ser641 (Cell Signaling; Cat#3891; 1:500), PGC-1α (Millipore; Cat#AB3242, 1:1,000), and total actin (Sigma-Aldrich; Cat#A2103, 1:10,000). Primary antibodies were detected with anti-rabbit HRP (P.A.R.I.S; Cat#BI2407, 1:5,000). The protein bands were detected by chemiluminescence using ECL Lumina Forte (Millipore) and a chemiluminescence detector (Bio-Rad, France).
Phosphofructokinase enzymatic activity
For biochemical analysis, mice were sacrificed and tissues were quickly dissected, frozen in liquid nitrogen, and stored at −80°C until use. All chemicals were purchased from Sigma-Aldrich. Frozen tibialis anterior muscles were pulverized with a mortar and pestle under liquid nitrogen. The powder was resuspended in five volumes (w/v) of extraction buffer containing 20 mM Tris–HCl pH 7.5, 0.15 M NaCl, and Protease inhibitor cocktail (Calbiochem, USA). Samples were homogenized by vortexing for 3 min prior to incubation for 10 min on roller at room temperature. After a final homogenization by vortexing for 2 min, samples underwent centrifugation for 15 min at 10,000 g at 4°C. The supernatant was used for the assay of PFK activity and determination of protein concentration as described above.
PFK activity was determined at 25°C in 96-well microplates in a total volume of 240 μl. An aliquot (10 μl) of tissue extract was added to 200 μl of reaction cocktail solution (50 mM Tris–HCl pH 8.0, 3 mM MgCl2, 3 mM DTT, 0.1 mM EGTA, 0.3 mM NADH, 2 mM fructose-6-phosphate, 10 IU aldolase, 80 IU triose phosphate isomerase, 14 IU glycerol-3-phosphodeshydrogenase, and 10 μl of distilled water). The reaction was started with the addition of 20 μl of 10-mM ATP. PFK activity was measured every minute over 20 min and calculated from the linear rate of change in absorbance at 340 nm (Tristar LB 941 apparatus, Berthold Technologies, Germany). Calculations were based on the extinction coefficient of 6.22 × 10−3 M for NADH and corrected by the volume of the sample added, to obtain nmol of NADH oxidized/min/μl of sample. As one mole of NADH corresponds to one mole of PFK, the activity of PFK was calculated for each sample relative to the protein concentration of each sample.
Intermediary metabolites
All intermediary metabolites analyzed were extracted from fresh snap-frozen tissue. Quantification was performed using commercial colorimetric assays for pyruvate (K609-100; BioVision, USA), ATP (K354-100; BioVision), and NAD+ and NADH (ab65348; Abcam, UK). Samples were deproteinized using 10-kDa cutoff spin filters (ab93349; Abcam), and assays were performed according to manufacturer's instructions. The optical densities for all assays were obtained using a Tristar LB 941 multimode plate reader (Berthold Technologies, France), and raw concentration values were calculated as indicated by the manufacturer.
Histochemistry and morphometry
Glycogen deposition in muscle biopsies was determined using the standard periodic acid-Schiff (PAS) stain. Transverse (10 μm) TA sections were obtained from snap-frozen tissue embedded in TissueTek O.C.T. compound (Sakura, Japan) on a cryostat (Leica CM 3050S, Germany) at −24°C. Freshly cut sections were briefly dried at 37°C for 30 min. Sections were then incubated for 10 min in periodic acid 1% (Roth, Germany), followed by 30 min in Schiff's reagent (Roth, Germany) prior to a 5-min counterstain in Mayer's solution (Roth, Germany). After thorough washing, slides were dehydrated with successive alcohol–toluene baths and mounted in Roti-Histokitt (Roth, Germany). Microphotographs were obtained with an Eclipse E800 microscope (Nikon, France). Counts were performed by an investigator who was blinded to animal genotypes using National Institutes of Health IMAGE version 1.62 software (USA).
The SDH staining was performed as follows: freshly dried cryostat sections (14 μm) were incubated for 5 min at room temperature (19–21°C) in a medium composed of 2 ml of nitroblue tetrazolium stock solution (100 ml phosphate-buffered saline at pH 7.6, 6.5 mg KCN, 185 mg EDTA, 100 mg NB), 0.2 ml succinate stock solution (2.7 g sodium succinate, 20 ml distilled water), and 0.7 mg phenazine methosulfate. The sections were rinsed in acetone gradient, cleared, and mounted in glycerin jelly. Microphotographs were obtained with an Eclipse E800 microscope (Nikon). Muscle fiber cross-sectional area of SDH-positive oxidative fibers and SDH-negative glycolytic fibers was determined from digitized muscle sections, using ImageJ software (http://imagej.nih.gov). The cross-sectional area of 50 individual fibers/category and mouse was determined from the number of pixels within manually outlined fiber boundaries by an investigator who was blinded to genotypes and treatment groups.
Statistical analysis
No previous statistical calculation was employed to determine sample size. Instead, sample size in our experiments was chosen based on usual procedures and best practices in the field (Ludolph et al, 2010). Unless otherwise indicated, data are expressed as the mean ± SEM. For each figure, statistical tests are justified as appropriate. The significance of the difference between two groups was determined with a two-tailed Student's t-test. Multiple comparisons were analyzed by analysis of variance (ANOVA) followed by Fisher's least significant difference (Fisher's LSD) post hoc test. For axotomy experiments, paired t-tests were performed to compare between muscle ipsilateral and contralateral to the crush for each mouse. Statistical tests used and the number of samples or animals are specified in the respective figure legends. Differences with P-values ≤ 0.05 were considered significant. Statistical analysis was performed using Graphpad Prism version 6.0e (GraphPad, USA).
The paper explained
Problem
Amyotrophic lateral sclerosis is the most common adult motor neuron disorder characterized by motor neuron death and muscular atrophy, which ultimately leads to death. To date, there is no efficient therapy for this fatal disease. ALS has a very important metabolic component as, in patients, energy deficit negatively impacts disease progression and correlates with poorer prognosis. Muscle denervation in disease progression seems to be a dynamic process of denervation and reinnervation that is different for the different muscle fiber types, with the glycolytic muscle fibers being the first affected. In the present work, we investigated potential metabolic mechanisms that may be coupled to the muscle–nerve dialogue and NMJ stability and that may account for the metabolic imbalance described in patients.
Results
The most important finding of our study in this neuromuscular disease is an increase in endurance capacity during prolonged oxidative exercise associated with a switch in fuel preference in glycolytic muscle fibers toward lipid oxidation, prior to motor symptoms. The increased expression of genes involved in lipid handling is accompanied by a decrease in expression and activity of PFK1, the rate-limiting enzyme of glycolysis. Glycolysis inhibition is a bottom-to-top process, orchestrated by PDK4, a mitochondrial enzyme that blocks the entry of pyruvate, the end product of glycolysis, into the TCA cycle. The increase in lipid use is not accompanied by an increase in mitochondrial biogenesis, but is associated with mitochondrial deficit and increased oxidative stress. We further show that it is possible to pharmacologically modulate this pathway and restore metabolic equilibrium. By doing so, we were able to prevent denervation and muscular atrophy and improve metabolic profile in our ALS mouse model.
Impact
We show for the first time that muscle tissue suffers metabolic alterations early in the course of disease development, alterations that influence the course of the pathology. These alterations are specific to glycolytic muscle fibers and therefore can explain the sensitivity of glycolytic fibers to atrophy and denervation. By exploring this mechanism, we pinpoint the molecular components involved in these modifications. We identify a potential therapeutic target in this pathway, which, if targeted, may improve prognosis and quality of life for ALS patients.
Acknowledgments
This work was supported by funds from ‘Association pour la Recherche sur la Sclérose Latérale Amyotrophique et autres Maladies du Motoneurone’ (FR), ‘Association pour la recherche et le développement de moyens de lutte contre les maladies neurodégénératives’ (AREMANE) (J.P.L.) ‘André Combat la SLA’ (U1118 INSERM), and European Community's Health Seventh Framework Programme under grant agreement No. 259867 (Euro-MOTOR) (U1118 INSERM and AH). LP is granted by ‘Association Française de lutte contre les Myopathies’ and AV is granted by ‘Region Alsace’ and INSERM. STN acknowledges the support of an Motor Neurone Disease Research Institute of Australia Bill Gole Fellowship and MNDRIA Graham Smith MND Research Grant, The University of Queensland, and The Australian Academy of Science. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. We thank Jérôme Sinniger, Annie Picchinenna and Marie José Ruivo for excellent technical assistance. We are also indebted to Drs Floriane Imhoff-White and Bastien Fricker for their aid with part of the initial SOD1G86R mouse experiments. We thank the ‘plate-forme d'imagerie’ from Neuropole/INSERM/UDS for technical assistance with confocal imaging.
Author contributions
LP, STN, JZ, J-PL, and FR conceived and designed the experiments and interpreted data. LP, AS, AV, AH, SD-G, and AE-L performed the experiments. LP, AS, SD-G, A-LB, JZ, STN, J-PL, and FR carried out the data analysis. LP, STN, J-PL, and FR wrote the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Supporting Information
Supplementary Figures S1–S7 and Supplementary Table S1
Review Process File
References
- Abdel-Aleem S. Regulation of fatty acid oxidation by acetyl-CoA generated from glucose utilization in isolated myocytes. J Mol Cell Cardiol. 1996;28:825–833. doi: 10.1006/jmcc.1996.0077. [DOI] [PubMed] [Google Scholar]
- Andersen PM, Al-Chalabi A. Clinical genetics of amyotrophic lateral sclerosis: what do we really know? Nat Rev Neurol. 2011;7:603–615. doi: 10.1038/nrneurol.2011.150. [DOI] [PubMed] [Google Scholar]
- Aon MA, Bhatt N, Cortassa SC. Mitochondrial and cellular mechanisms for managing lipid excess. Front Physiol. 2014;5:282. doi: 10.3389/fphys.2014.00282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkin JD, Scott RL, West JM, Lopes E, Quah AK, Cheema SS. Properties of slow- and fast-twitch muscle fibres in a mouse model of amyotrophic lateral sclerosis. Neuromuscul Disord. 2005;15:377–388. doi: 10.1016/j.nmd.2005.02.005. [DOI] [PubMed] [Google Scholar]
- Bachmanov AA, Reed DR, Beauchamp GK, Tordoff MG. Food intake, water intake, and drinking spout side preference of 28 mouse strains. Behav Genet. 2002;32:435–443. doi: 10.1023/a:1020884312053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassel-Duby R, Olson EN. Signaling pathways in skeletal muscle remodeling. Annu Rev Biochem. 2006;75:19–37. doi: 10.1146/annurev.biochem.75.103004.142622. [DOI] [PubMed] [Google Scholar]
- Boillée S, Yamanaka K, Lobsiger CS, Copeland NG, Jenkins NA, Kassiotis G, Kollias G, Cleveland DW. Onset and progression in inherited ALS determined by motor neurons and microglia. Science. 2006;312:1389–1392. doi: 10.1126/science.1123511. [DOI] [PubMed] [Google Scholar]
- Bonnard C, Durand A, Peyrol S, ChanseaumeE CM, Morio B, Vidal H, Rieusset J. Mitochondrial dysfunction results from oxidative stress in the skeletal muscle of diet-induced insulin-resistant mice. J Clin Invest. 2008;118:789–800. doi: 10.1172/JCI32601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouteloup C, Desport JC, Clavelou P, Guy N, Derumeaux-Burel H, Ferrier A, Couratier P. Hypermetabolism in ALS patients: an early and persistent phenomenon. J Neurol. 2009;256:1236–1242. doi: 10.1007/s00415-009-5100-z. [DOI] [PubMed] [Google Scholar]
- Bowker-Kinley MM, Davis WI, Wu P, Harris RA, Popov KM. Evidence for existence of tissue-specific regulation of the mammalian pyruvate dehydrogenase complex. Biochem J. 1998;329:191–196. doi: 10.1042/bj3290191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S, Sayana P, Zhang X, Le W. Genetics of amyotrophic lateral sclerosis: an update. Mol Neurodegener. 2013;8:28. doi: 10.1186/1750-1326-8-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constable SH, Favier RJ, McLane JA, Fell RD, Chen M, Holloszy JO. Energy metabolism in contracting rat skeletal muscle: adaptation to exercise training. Am J Physiol Cell Physiol. 1987;253:C316–C322. doi: 10.1152/ajpcell.1987.253.2.C316. [DOI] [PubMed] [Google Scholar]
- Da Cruz S, Parone P, Lopes VS, Lillo C, McAlonis-Downes M, Lee SK, Vetto AP, Petrosyan S, Marsala M, Murphy AN, et al. Elevated PGC-1α activity sustains mitochondrial biogenesis and muscle function without extending survival in a mouse model of inherited ALS. Cell Metab. 2012;15:778–786. doi: 10.1016/j.cmet.2012.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deforges S, Branchu J, Biondi O, Grondard C, Pariset C, Lécolle S, Lopes P, Vidal PP, Chanoine C, Charbonnier F. Motoneuron survival is promoted by specific exercise in a mouse model of amyotrophic lateral sclerosis. J Physiol. 2009;587(Pt 14):3561–3572. doi: 10.1113/jphysiol.2009.169748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dengler R, Konstanzer A, Kuther G, Hesse S, Wolf W, Struppler A. Amyotrophic lateral sclerosis: macro-EMG and twitch forces of single motor units. Muscle Nerve. 1990;13:545–550. doi: 10.1002/mus.880130612. [DOI] [PubMed] [Google Scholar]
- Denton RM, Randle PJ, Bridges BJ, Cooper RH, Kerbey AL, Pask HT, Severson DL, Stansbie D, Whitehouse S. Regulation of mammalian pyruvate dehydrogenase. Mol Cell Biochem. 1975;9:27–53. doi: 10.1007/BF01731731. [DOI] [PubMed] [Google Scholar]
- Desport JC, Preux PM, Truong TC, Vallat JM, Sautereau D, Couratier P. Nutritional status is a prognostic factor for survival in ALS patients. Neurology. 1999;53:1059–1063. doi: 10.1212/wnl.53.5.1059. [DOI] [PubMed] [Google Scholar]
- Desport JC, Preux PM, Magy L, Boirie Y, Vallat JM, Beaufrère B, Couratier P. Factors correlated with hypermetabolism in patients with amyotrophic lateral sclerosis. Am J Clin Nutr. 2001;74:328–334. doi: 10.1093/ajcn/74.3.328. [DOI] [PubMed] [Google Scholar]
- Desport JC, Torny F, Lacoste M, Preux PM, Couratier P. Hypermetabolism in ALS: correlations with clinical and paraclinical parameters. Neurodegener Dis. 2005;2:202–207. doi: 10.1159/000089626. [DOI] [PubMed] [Google Scholar]
- Duclert A, Changeux JP. Acetylcholine receptor gene expression at the developing neuromuscular junction. Physiol Rev. 1995;75:339–368. doi: 10.1152/physrev.1995.75.2.339. [DOI] [PubMed] [Google Scholar]
- Dupuis L, Oudart H, René F, Gonzalez de Aguilar JL, Loeffler JP. Evidence for defective energy homeostasis in amyotrophic lateral sclerosis: benefit of a high-energy diet in a transgenic mouse model. Proc Natl Acad Sci USA. 2004;101:11159–11164. doi: 10.1073/pnas.0402026101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupuis L, Gonzalez de Aguilar JL, Echaniz-Laguna A, Eschbach J, René F, Oudart H, Halter B, Huze C, Schaeffer L, Bouillaud F, et al. Muscle mitochondrial uncoupling dismantles neuromuscular junction and triggers distal degeneration of motor neurons. PLoS One. 2009;4:e5390. doi: 10.1371/journal.pone.0005390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupuis L, Pradat PF, Ludolph AC, Loeffler JP. Energy metabolism in amyotrophic lateral sclerosis. Lancet Neurol. 2011;10:75–82. doi: 10.1016/S1474-4422(10)70224-6. [DOI] [PubMed] [Google Scholar]
- Feng G, Mellor RH, Bernstein M, Keller-Peck C, Nguyen QT, Wallace M, Nerbonne JM, Lichtman JW, Sanes JR. Imaging neuronal subsets in transgenic mice expressing multiple spectral variants of GFP. Neuron. 2000;28:41–51. doi: 10.1016/s0896-6273(00)00084-2. [DOI] [PubMed] [Google Scholar]
- Fergani A, Oudart H, Gonzalez De Aguilar JL, Fricker B, René F, Hocquette JF, Meininger V, Dupuis L, Loeffler JP. Increased peripheral lipid clearance in an animal model of amyotrophic lateral sclerosis. J Lipid Res. 2007;48:1571–1580. doi: 10.1194/jlr.M700017-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer LR, Culver DG, Tennant P, Davis AA, Wang M, Castellano-Sanchez A, Khan J, Polak MA, Glass JD. Amyotrophic lateral sclerosis is a distal axonopathy: evidence in mice and man. Exp Neurol. 2004;185:232–240. doi: 10.1016/j.expneurol.2003.10.004. [DOI] [PubMed] [Google Scholar]
- Frey D, Schneider C, Xu L, Borg J, Spooren W, Caroni P. Early and selective loss of neuromuscular synapse subtypes with low sprouting competence in motoneuron diseases. J Neurosci. 2000;20:2534–2542. doi: 10.1523/JNEUROSCI.20-07-02534.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuyama T, Kitayama K, Yamashita H, Mori N. Forkhead transcription factor FOXO1 (FKHR)-dependent induction of PDK4 gene expression in skeletal muscle during energy deprivation. Biochem J. 2003;375:365–371. doi: 10.1042/BJ20030022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurney ME, Pu H, Chiu AY, Dal Canto MC, Polchow CY, Alexander DD, Caliendo J, Hentati A, Kwon YW, Deng HX, et al. Motor neuron degeneration in mice that express a human Cu, Zn superoxide dismutase mutation. Science. 1994;264:1772–1775. doi: 10.1126/science.8209258. [DOI] [PubMed] [Google Scholar]
- Halter B, Gonzalez de Aguilar JL, René F, Petri S, Fricker B, Echaniz-Laguna A, Dupuis L, Larmet Y, Loeffler JP. Oxidative stress in skeletal muscle stimulates early expression of Rad in a mouse model of amyotrophic lateral sclerosis. Free Radic Biol Med. 2010;48:915–923. doi: 10.1016/j.freeradbiomed.2010.01.014. [DOI] [PubMed] [Google Scholar]
- Hardiman O, van den Berg LH, Kiernan MC. Clinical diagnosis and management of amyotrophic lateral sclerosis. Nat Rev Neurol. 2011;7:639–649. doi: 10.1038/nrneurol.2011.153. [DOI] [PubMed] [Google Scholar]
- Harris RA, Bowker-Kinley MM, Huang B, Wu P. Regulation of the activity of the pyruvate dehydrogenase complex. Adv Enzyme Regul. 2002;42:249–259. doi: 10.1016/s0065-2571(01)00061-9. [DOI] [PubMed] [Google Scholar]
- Hegedus J, Putman CT, Tyreman N, Gordon T. Preferential motor unit loss in the SOD1 G93A transgenic mouse model of amyotrophic lateral sclerosis. J Physiol. 2008;586:3337–3351. doi: 10.1113/jphysiol.2007.149286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holness MJ, Sugden MC. Regulation of pyruvate dehydrogenase complex activity by reversible phosphorylation. Biochem Soc Trans. 2003;31:1143–1151. doi: 10.1042/bst0311143. [DOI] [PubMed] [Google Scholar]
- Jawaid A, Murthy SB, Wilson AM, Qureshi SU, Amro MJ, Wheaton M, Simpson E, Harati Y, Strutt AM, York MK, et al. A decrease in body mass index is associated with faster progression of motor symptoms and shorter survival in ALS. Amyotroph Lateral Scler. 2010;11:542–548. doi: 10.3109/17482968.2010.482592. [DOI] [PubMed] [Google Scholar]
- Jeong JY, Jeoung NH, Park KG, Lee IK. Transcriptional regulation of pyruvate dehydrogenase kinase. Diabetes Metab J. 2012;36:328–335. doi: 10.4093/dmj.2012.36.5.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YI, Lee FN, Choi WS, Lee S, Youn JH. Insulin regulation of skeletal muscle PDK4 mRNA expression is impaired in acute insulin-resistant states. Diabetes. 2006;55:2311–2317. doi: 10.2337/db05-1606. [DOI] [PubMed] [Google Scholar]
- Lin J, Wu H, Tarr PT, Zhang CY, Wu Z, Boss O, Michael LF, Puigserver P, Isotani E, Olson EN, et al. Transcriptional co-activator PGC-1 alpha drives the formation of slow-twitch muscle fibres. Nature. 2002;418:797–801. doi: 10.1038/nature00904. [DOI] [PubMed] [Google Scholar]
- Ludolph AC, Bendotti C, Blaugrund E, Chio A, Greensmith L, Loeffler JP, Mead R, Niessen HG, Petri S, Pradat PF, et al. Guidelines for preclinical animal research in ALS/MND: a consensus meeting. Amyotroph Lateral Scler. 2010;11:38–45. doi: 10.3109/17482960903545334. [DOI] [PubMed] [Google Scholar]
- Luquet S, Lopez-Soriano J, Holst D, Fredenrich A, Melki J, Rassoulzadegan M, Grimaldi PA. Peroxisome proliferator-activated receptor delta controls muscle development and oxidative capability. FASEB J. 2003;17:2299–2301. doi: 10.1096/fj.03-0269fje. [DOI] [PubMed] [Google Scholar]
- Mallinson JE, Constantin-Teodosiu D, Glaves PD, Martin EA, Davies WJ, Westwood FR, Sidaway JE, Greenhaff PL. Pharmacological activation of the pyruvate dehydrogenase complex reduces statin-mediated upregulation of FOXO gene targets and protects against statin myopathy in rodents. J Physiol. 2012;590:6389–6402. doi: 10.1113/jphysiol.2012.238022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massao Hirabara S, de Oliveira Carvalho CR, Mendonça JR, Piltcher Haber E, Fernandes LC, Curi R. Palmitate acutely raises glycogen synthesis in rat soleus muscle by a mechanism that requires its metabolization (Randle cycle) FEBS Lett. 2003;541:109–114. doi: 10.1016/s0014-5793(03)00316-8. [DOI] [PubMed] [Google Scholar]
- Mattson MP, Cutler RG, Camandola S. Energy intake and amyotrophic lateral sclerosis. Neuromolecular Med. 2007;9:17–20. doi: 10.1385/nmm:9:1:17. [DOI] [PubMed] [Google Scholar]
- McGarry JD, Mills SE, Long CS, Foster DW. Observations on the affinity for carnitine, and malonyl-CoA sensitivity, of carnitine palmitoyltransferase I in animal and human tissues. Demonstration of the presence of malonyl-CoA in non-hepatic tissues of the rat. Biochem J. 1983;214:21–28. doi: 10.1042/bj2140021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mead JR, Irvine SA, Ramji DP. Lipoprotein lipase: structure, function, regulation, and role in disease. J Mol Med (Berl) 2002;80:753–769. doi: 10.1007/s00109-002-0384-9. [DOI] [PubMed] [Google Scholar]
- Miquel E, Cassina A, Martínez-Palma L, Bolatto C, Trías E, Gandelman M, Radi R, Barbeito L, Cassina P. Modulation of astrocytic mitochondrial function by dichloroacetate improves survival and motor performance in inherited amyotrophic lateral sclerosis. PLoS One. 2012;7:e34776. doi: 10.1371/journal.pone.0034776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahlé Z, Hsieh M, Pietka T, Coburn CT, Grimaldi PA, Zhang MQ, Das D, Abumrad NA. CD36-dependent regulation of muscle FoxO1 and PDK4 in the PPAR delta/beta-mediated adaptation to metabolic stress. J Biol Chem. 2008;283:14317–14326. doi: 10.1074/jbc.M706478200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngo ST, Baumann F, Ridall PG, Pettitt AN, Henderson RD, Bellingham MC, McCombe PA. The relationship between Bayesian motor unit number estimation and histological measurements of motor neurons in wild-type and SOD1(G93A) mice. Clin Neurophysiol. 2012;123:2080–2091. doi: 10.1016/j.clinph.2012.01.028. [DOI] [PubMed] [Google Scholar]
- Pedersen WA, Mattson MP. No benefit of dietary restriction on disease onset or progression in amyotrophic lateral sclerosis Cu/Zn-superoxide dismutase mutant mice. Brain Res. 1999;833:117–120. doi: 10.1016/s0006-8993(99)01471-7. [DOI] [PubMed] [Google Scholar]
- Pette D, Staron RS. Transitions of muscle fiber phenotypic profiles. Histochem Cell Biol. 2001;115:359–372. doi: 10.1007/s004180100268. [DOI] [PubMed] [Google Scholar]
- Philp A, Perez-Schindler J, Green C, Hamilton DL, Baar K. Pyruvate suppresses PGC1alpha expression and substrate utilization despite increased respiratory chain content in C2C12 myotubes. Am J Physiol Cell Physiol. 2010;299:C240–C250. doi: 10.1152/ajpcell.00438.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pradat PF, Bruneteau G, Gordon PH, Dupuis L, Bonnefont-Rousselot D, Simon D, Salachas F, Corcia P, Frochot V, Lacorte JM, et al. Impaired glucose tolerance in patients with amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2010;11:166–171. doi: 10.3109/17482960902822960. [DOI] [PubMed] [Google Scholar]
- Puigserver P. Tissue-specific regulation of metabolic pathways through the transcriptional coactivator PGC1-alpha. Int J Obes (Lond) 2005;29(Suppl 1):S5–S9. doi: 10.1038/sj.ijo.0802905. [DOI] [PubMed] [Google Scholar]
- Pun S, Santos AF, Saxena S, Xu L, Caroni P. Selective vulnerability and pruning of phasic motoneuron axons in motoneuron disease alleviated by CNTF. Nat Neurosci. 2006;9:408–419. doi: 10.1038/nn1653. [DOI] [PubMed] [Google Scholar]
- Ripps ME, Huntley GW, Hof PR, Morrison JH, Gordon JW. Transgenic mice expressing an altered murine superoxide dismutase gene provide an animal model of amyotrophic lateral sclerosis. Proc Natl Acad Sci USA. 1995;92:689–693. doi: 10.1073/pnas.92.3.689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocha MC, Pousinha PA, Correia AM, Sebastião AM, Ribeiro JA. Early changes of neuromuscular transmission in the SOD1(G93A) mice model of ALS start long before motor symptoms onset. PLoS One. 2013;8:e73846. doi: 10.1371/journal.pone.0073846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smittkamp SE, Morris JK, Bomhoff GL, Chertoff ME, Geiger PC, Stanford JA. SOD1-G93A mice exhibit muscle-fiber-type-specific decreases in glucose uptake in the absence of whole-body changes in metabolism. Neurodegener Dis. 2014;13:29–37. doi: 10.1159/000351606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spriet LL, Tunstall RJ, Watt MJ, Mehan KA, Hargreaves M, Cameron-Smith D. Pyruvate dehydrogenase activation and kinase expression in human skeletal muscle during fasting. J Appl Physiol. 2004;96:2082–2087. doi: 10.1152/japplphysiol.01318.2003. [DOI] [PubMed] [Google Scholar]
- Talanian JL, Holloway GP, Snook LA, Heigenhauser GJF, Bonen A, Spriet LL. Exercise training increases sarcolemmal and mitochondrial fatty acid transport proteins in human skeletal muscle. Am J Physiol Endocrinol Metab. 2010;299:E180–E188. doi: 10.1152/ajpendo.00073.2010. [DOI] [PubMed] [Google Scholar]
- Telerman-Toppet N, Coërs C. Motor innervation and fiber type pattern in amyotrophic lateral sclerosis and in Charcot-Marie-Tooth disease. Muscle Nerve. 1978;1:133–139. doi: 10.1002/mus.880010205. [DOI] [PubMed] [Google Scholar]
- Valenzuela DM, Stitt TN, DiStefano PS, Rojas E, Mattsson K, Compton DL, Nuñez L, Park JS, Stark JL, Gies DR, et al. Receptor tyrosine kinase specific for the skeletal muscle lineage: expression in embryonic muscle, at the neuromuscular junction, and after injury. Neuron. 1995;15:573–584. doi: 10.1016/0896-6273(95)90146-9. [DOI] [PubMed] [Google Scholar]
- Vestergaard H. Studies of gene expression and activity of hexokinase, phosphofructokinase and glycogen synthase in human skeletal muscle in states of altered insulin-stimulated glucose metabolism. Dan Med Bull. 1999;46:13–34. [PubMed] [Google Scholar]
- Villena JA, Kralli A. ERRalpha: a metabolic function for the oldest orphan. Trends Endocrinol Metab. 2008;19:269–276. doi: 10.1016/j.tem.2008.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinsant S, Mansfield C, Jimenez-Moreno R, Del Gaizo MV, Yoshikawa M, Hampton TG, Prevette D, Caress J, Oppenheim RW, Milligan C. Characterization of early pathogenesis in the SOD1(G93A) mouse model of ALS: part I, background and methods. Brain Behav. 2013a;3:335–350. doi: 10.1002/brb3.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinsant S, Mansfield C, Jimenez-Moreno R, Del Gaizo MV, Yoshikawa M, Hampton TG, Prevette D, Caress J, Oppenheim RW, Milligan C. Characterization of early pathogenesis in the SOD1(G93A) mouse model of ALS: part II, results and discussion. Brain Behav. 2013b;3:431–457. doi: 10.1002/brb3.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang YX, Zhang CL, Yu RT, Cho HK, Nelson MC, Bayuga-Ocampo CR, Ham J, Kang H, Evans RM. Regulation of muscle fiber type and running endurance by PPARdelta. PLoS Biol. 2004;2:e294. doi: 10.1371/journal.pbio.0020294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt MJ, Heigenhauser GJF, LeBlanc PJ, Inglis JG, Spriet LL, Peters SJ. Rapid upregulation of pyruvate dehydrogenase kinase activity in human skeletal muscle during prolonged exercise. J Appl Physiol. 2004;97:1261–1267. doi: 10.1152/japplphysiol.00132.2004. [DOI] [PubMed] [Google Scholar]
- Whitehouse S, Randle PJ. Activation of pyruvate dehydrogenase in perfused rat heart by dichloroacetate. Biochem J. 1973;134:651–653. doi: 10.1042/bj1340651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong M, Martin LJ. Skeletal muscle-restricted expression of human SOD1 causes motor neuron degeneration in transgenic mice. Hum Mol Genet. 2010;19:2284–2302. doi: 10.1093/hmg/ddq106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Z, Puigserver P, Andersson U, Zhang C, Adelmant G, Mootha V, Troy A, Cinti S, Lowell B, Scarpulla R, et al. Mechanisms controlling mitochondrial biogenesis and respiration through the thermogenic coactivator PGC-1. Cell. 1999;98:115–124. doi: 10.1016/S0092-8674(00)80611-X. [DOI] [PubMed] [Google Scholar]
- Yamanaka K, Chun SJ, Boillee S, Fujimori-Tonou N, Yamashita H, Gutmann DH, Takahashi R, Misawa H, Cleveland DW. Astrocytes as determinants of disease progression in inherited amyotrophic lateral sclerosis. Nat Neurosci. 2008;11:251–253. doi: 10.1038/nn2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Keung W, Samokhvalov V, Wang W. Lopaschuk GD (2010) Role of fatty acid uptake and fatty acid beta-oxidation in mediating insulin resistance in heart and skeletal muscle. Biochim Biophys Acta. 2010;1801:1–22. doi: 10.1016/j.bbalip.2009.09.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figures S1–S7 and Supplementary Table S1
Review Process File