Abstract
Introduction
We report the first prospective analysis of human factors elements contributing to invasive procedural never events using a validated Human Factors Analysis and Classification System (HFACS).
Methods
From 8/2009 - 8/2014 surgical and invasive procedural “Never Events” (retained foreign object, wrong site/side procedure, wrong implant, wrong procedure) underwent systematic causation analysis promptly after the event. Contributing human factors were categorized using Reason's 4 levels of error causation and 161 HFACS subcategories (nano-codes).
Results
During the study approximately 1.5 million procedures were performed and 69 never events were identified. A total of 628 contributing human factors nano-codes were identified. Action-based errors (n=260) and preconditions to actions (n=296) accounted for the majority of the nano-codes across all four types of events, with individual cognitive factors contributing half of the nano-codes. The most common action nano-codes were confirmation bias (n=36) and failed to understand (n=36). The most common pre-condition nano-codes were channeled attention on a single issue (n=33) and inadequate communication (n=30).
Conclusion
Targeting quality and system improvement interventions addressing cognitive factors and team resource management as well as perceptual biases may reduce errors and further improve patient safety. These results delineate targets to further reduce never events from our healthcare system.
INTRODUCTION
It is estimated that physicians operating on bilateral structures have a 25 percent lifetime risk of wrong site surgery and an average size surgical center reports about one retained foreign object (RFO) per year.1 Wrong site/side surgery, wrong implant, wrong procedure and RFOs have been termed “Never Events” and are included in the 29 serious reportable healthcare events as defined by the National Quality Forum and the Joint Commission.2,3 Never events can lead to serious physical or psychological harm for the patient, the teams caring for the patient, and the patient provider relationship.4 At an institutional level, such events add a serious financial burden as a consequence of their medical-legal implications as well as a negative impact on a center's reputation. Therefore, a better understanding of why these events occur and efforts directed at reducing their frequency are important for patient safety, provider well-being and society.
The current incidence of never events in the US is poorly understood. Prospectively collected data on the incidence of never events are limited and most studies involve voluntary reporting to external agencies with inherent bias. Retrospective analysis suggests a never events rate of one in 12,248 operations in the United States5 and 1 in every 20,000 procedures in the National Health System in the UK.6 Studies investigating adverse events and events like retained foreign objects suggest that the rate may be higher.7 In addition, there is concern that the frequency of retained foreign objects may be increasing.5
Healthcare professionals and systems engineers have been working to improve conditions in the operating room (OR) and procedural environment for over a century to ensure these events do not occur. Based on a systems safety approach, the majority of medical errors are believed to be the product of inadequately designed systems which permit predictable human errors.8 This concept has been formalized by Reason as the “Swiss cheese” model where events occur as the result of a problem passing undetected through minor defects in multiple layers of a system's defences resulting in a serious, potentially fatal, event to occur.9 Another concept, Perrow's theory of “Normal accidents”, holds that in modern high-risk systems, the degree of system complexity, tight coupling of processes, and the inability of a single individual or small group of individuals to manage all the potential interactions inevitably will lead to accidents with catastrophic potential.10 Both theories imply that errors and accidents cannot be designed around as people make mistakes. Many problems arise from small beginnings and organizational failures may play a significant role. However, individuals remain at the tip of the spear in both contributing to and potentially preventing errors.10 With a better understanding of human-system interactions, significant gains have been made to understand why these events occur and to re-engineer the systems to prevent them in the future.11
While systems play a major role in allowing errors to escape system notice, an essential component of medical care are the individuals, who have the potential to recover from system error.12 Understanding the contributing human factors and their effect in medical errors is essential. Once an event occurs, root cause analysis (RCA) is a standard method within healthcare organizations to evaluate medical errors. Unfortunately, RCAs with the resultant education initiatives and system redesign alone may not be sufficient to eliminate never events.13 Human factors analysis, which is widely used in other industries, can enhance RCAs and provide an additional perspective on the system. To allow systematic analysis of human factors in military aviation accidents, Shappell and Wiegmann developed and validated the Human Factors Analysis and Classification System (HFACS).14 The HFACS methodology has been validated across several industries15, including medicine.16,17 In this study, we review the results from the prospectively applied HFACS methodology to surgical and procedural never events at our institution
METHODS
From August 31, 2009 to August 31, 2014, an electronic incident reporting system captured all reported (including anonymously reported) patient events and near misses for the quality management team at a tertiary-care hospital. All cases of wrong site/ side surgery, wrong procedure, wrong implant, and unintended retention of a foreign object after surgery or other invasive procedure were considered never events and included in our analysis. Surgical or other invasive procedural never events underwent RCA with involved team members individually and at a joint meeting. The joint meeting included the team members involved (physicians, nurses, technicians, residents), quality management, clinical practice and administrative leadership. The meetings occurred as contemporaneously as possible after the event was discovered to quickly determine the contributing systems and human factor. For the majority of the reporting period RFOs were reviewed within 48 hours and all events were reviewed on average within two days of identification.
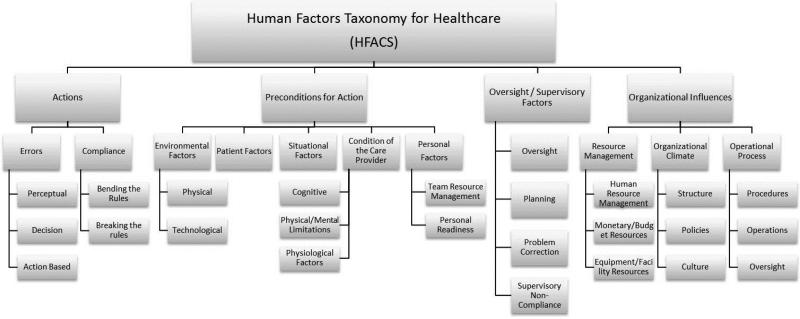
In addition to the standard review, a trained quality management specialist coded each event using the HFACS tool modified by Diller et al (Appendix).16 Following Reason's categories, the never events were described under four categories: (1) unsafe actions, (2) preconditions for unsafe actions, (3) oversight/supervisory factors, and (4) organizational influences (Figure 1). Unsafe actions include issues with protocol compliance (e.g. bending the rules or breaking the rules) or errors, such as perceptual errors (e.g. misunderstanding a situation) and decision errors (e.g. inadequate treatment). Preconditions for actions included environmental, patient, situational and behavioral factors. Examples of preconditions include poor hand-offs or inadequate operative lighting. Oversight/supervisory factors included factors such as supervisor oversight, planning difficulties, staffing deficiencies, and supervisor non-compliance. Lastly, organizational influences include inadequacies in organizational culture or operational processes.
Figure 1.
HFACS categories and sub-categories with selected nano-codes
Each of these error contributing categories and subcategories are divided into a total of 161 specific human behaviors or system situations, termed nano-codes. The HFACS data were then entered into a secure electronic database. In addition to the prospective HFACS coding, the type of procedure, date and timing, and outcome data were obtained by review of the electronic medical record. Six patients were excluded from medical record review as they had not provided research authorization. Event rates were compared by type and error causation. Subgroup analysis of the 161 nano-codes within the four larger categories was performed. Student's t-test and Chi square test were used for statistical analysis.
RESULTS
During the 5-year period over 1.5 million operations and other invasive procedures were performed. A total of 70 never events underwent RCA. Sixty-nine never events were coded prospectively using the HFACS coding system. HFACS data were not collected during one RCA due to unavailability of HFACS trained personnel. Forty of the coded never events occurred in an operating room while the remainder (n=29) occurred in a procedural area, such as endoscopy or interventional radiology.
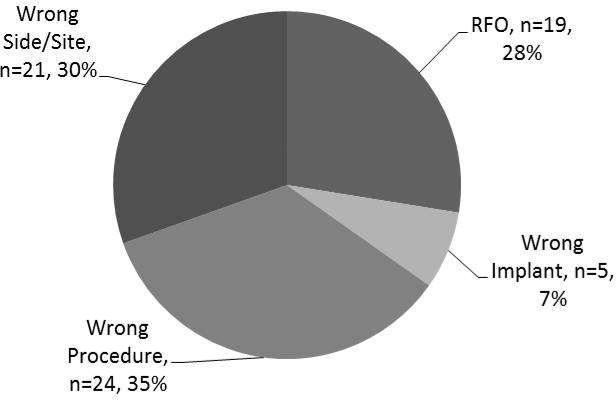
The rate of never events was estimated to be 1 in 22,000 procedures performed. The distribution of never events by type is depicted in Figure 2. There was a mean of 14 never events per year over the course of the study with variation year to year (range 7 to 20). Of the never events included in our analysis, 24 (35%) occurred during major operations, 3 (4%) during minimally invasive surgeries. Forty-two events (61%) occurred during minor cases: anesthetic blocks and line placements (n=16, 23%), interventional radiology procedures (n=15, 22%), endoscopy (n=5, 7%) and other minor skin and soft tissue procedures (n=6, 9%). Of the 19 RFO's, 7 (37%) involved retained wires, tubing or needles, 10 (53%) involved other objects and 2 (11%) involved surgical sponges.
Figure 2.
Distribution of never events by type showing about one-third contribution of wrong side/site surgery, wrong procedure, and retained foreign object compared to a small number of wrong implants
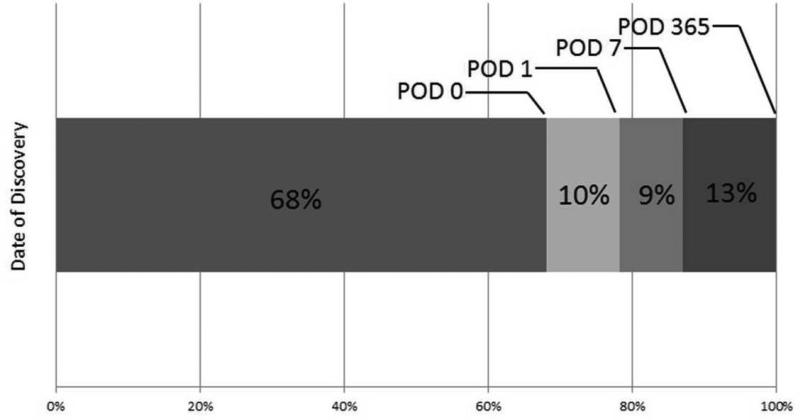
The majority of the events (68%) were discovered on the day of the index procedure, an additional 10% by post-procedure day one. Of note, many surgeons at our institution routinely obtain post-procedure X-rays for cases in which a major body cavity is entered. Within the first week, 87% of events were detected, and the remaining events were discovered by one year post procedure (Figure 3). There was no intraoperative or 30-day mortality as a result of a never event in this series. There was one 30-day mortality that was deemed unrelated to the never event. A significant proportion of patients (52%) required an additional operation or procedure as a result of the event. RFOs and wrong implants required an additional operation or procedure in 75% and 60%, respectively, while wrong procedure and wrong side/site surgery had a reoperation rate of 45% and 42%, respectively (p=0.082). Of all events reviewed here, 8% (n=5) of the procedures concluded after 5 p.m. of which three (5%) started after 5 p.m. Seven events (11%) occurred in emergency cases, three of those cases were conducted after 5 p.m. Combined, 13% (n=9) of all events occurred either after hours or during emergency cases, with 56% (n=5) of those being RFOs.
Figure 3.
Postoperative day which never event was discovered indicating that the majority (87%) of events were discovered in the first week after surgery
Human Factors Analysis
Each event had a mean of nine contributing human factors nano-codes (range1-21) associated with it. A total of 628 nano-codes were identified across all events. The nano-codes were grouped by four major error causes (Table 1). The relative frequency of identified error type to event demonstrated that preconditions to actions (n=296; 47%) and unsafe actions (n=260; 41%) accounted for the majority of the nano-codes across all four types of events. Oversight and supervisory factors (n=47; 7.5%) and organizational factors (n=25; 4%) were coded significantly less often as contributing to the event compared to preconditions to actions and actions (p < 0.001). The distribution of nano-codes indicated that RFOs and wrong implants had more nano-codes per event while wrong procedure and wrong side/site had less (p <0.001) (Table 2). The nano-codes encountered within each of Reason's four levels of errors were as follows:
Table 1.
HFACS* categories with number of nano-codes by event type.
| Actions | Organizational Influences | Oversight / Supervisory Factors | Preconditions for Actions | Total | |
|---|---|---|---|---|---|
| Retained foreign object | 102 | 9 | 16 | 94 | 221 |
| Wrong implant | 24 | 1 | 5 | 32 | 62 |
| Wrong procedure | 78 | 6 | 12 | 99 | 195 |
| Wrong side/site | 56 | 9 | 14 | 71 | 150 |
| Total | 260 | 25 | 47 | 296 | 628 |
Human Factors Analysis and Classification System
Table 2.
Distribution of nano-codes per event type.
| # Of Events | Maximum # of nano-codes per event | Average # of nano-codes per event | Median # of nano-codes per event | |
|---|---|---|---|---|
| Retained foreign object | 18 | 20 | 12 | 14 |
| Wrong implant | 5 | 21 | 13 | 11 |
| Wrong procedure | 24 | 18 | 8 | 7 |
| Wrong side/site | 22 | 12 | 7 | 7 |
I. Preconditions for Actions
Preconditions for actions were the most commonly coded contributing factors to events (n=296). Within the preconditions, physical factors (e.g. lighting and construction) were rarely coded (n=2, 0.7%); whereas, technology was coded 74 times (25%). The most commonly coded contributing technological factors were lack of interface between systems, electronic medical records factors and lack of automation. Patient factors, including obesity and complex anatomy, contributed 12% (n=35) of the precondition nano-codes. Situational factors such as emergent situations were coded as contributing in 1% (n=3). Conditions of the care providers, specifically cognitive factors, were coded 113 times (38%). The most commonly noted cognitive factors were: channeled attention on a single issue, overconfidence, inadequate vigilance, and distractions. Physical and mental limitations of providers were not identified as a contributing factor (n=0). Lastly, personnel factors, including personal readiness and behavioral factors, were also identified (n=69; 23%). The most commonly coded behavioral factor was inadequate communication (n=32, 46%).
II. Unsafe Actions
The second most commonly coded category was unsafe actions (n=260; 41%), consisting of errors (n=227, 87%) and compliance (n= 33, 13%). The most common sub-type of error was decision errors, which are “honest” errors in cognitive thought (n=103; 45%), with failure to understand being the most commonly identified nano-code. Action-based errors, which are errors in thinking that occur without significant conscious thought, were commonly coded (n=80; 35%). The most common action-based error was failure to follow a verification process (n=80; 31%). Lastly, perceptual errors, errors made based on inaccurate information, were also frequently coded as a contributing factor (n=44; 17%). Confirmation bias, a bias that leads a person to interpret information in a way that confirms one's beliefs, was the most commonly coded perceptual error (n=36, 82%). Compliance issues, such as failing to follow institutional policies and procedures or standards of practice, were coded 33 times (13%). This included bending the rules (n=22; 67%) and breaking the rules (n=11; 33%).
III. Oversight and Supervisory Factors
The third major category of HFACS, oversight and supervisory issues, was coded 47 times (8%) as contributing to events. This category includes oversight factors such as supervision, planning factors, problem correction deficiencies, and supervisory non-compliance.
IV. Organizational Influences
Lastly, an organizational influence was the least commonly coded HFACS category (n=25; 4%). This category includes resources management, organizational climate, and operational processes.
DISCUSSION
The 1999 report by the Institute of Medicine, To Err Is Human, was intended to promote recognizing, preventing, and mitigating harm from medical error—with the overall goal to stimulate system wide changes in health care to improve patient safety.18 Unfortunately, what the report is most often remembered for is how many hospital deaths result from medical errors. Despite the increased awareness that this and subsequent reports generated, medical errors have continued to occur at alarming rates.19
Systems engineering approaches have been utilized in the industrial realm and succeeded in significantly reducing the rates of injury. The use of these practices in the surgical and procedural environment has had a major impact on reducing never events.20 An example is the introduction of a bar-coded surgical sponge counting system, which reduced the frequency of retained sponges in our institution from an estimated 29 to 2 per 1.5 million procedures.21 This represents a 93% reduction in retained sponges and supports the previously advocated use of technology to reduce retained foreign objects.22 Given the success of implementing systems to prevent retained sponges, we suggest similar systems-based strategies should be implemented to mitigate cognitive and perceptual errors. As our data show, systems engineering, though significant and important in mitigation of error, is not the complete solution.
Our data demonstrate that in addition to the system, individual human factors play a significant role in determining if and when never events occur. Humans make up the largest part of the health care system, play a pivotal role in patient care, and also play a significant role in determination of error. Thus, HFACS can assist us in analyzing which factors are linked to each type of error and provide targets for intervention and mitigation. We found that cognitive factors contribute significantly to error; the three most frequently coded nano-codes belonged to that group and represented about half of all nano-codes. Communication failures were the fourth most frequent nano-code group. This suggests that leading up to an event an individual's (or team's) cognitive capacity may be outpaced by the cognitive demand. The cognitive capacity is taxed through increased patient or procedure related complexity23, use of increasingly complex technology, along with an increase in the number of varying team members.24 The outpaced cognitive capacity may then lead to individuals not following procedures as intended, as was described by Mallet et al.25 Of note, both cases of retained sponges in our cohort occurred after 5 p.m. during major cases and despite bar-code scanning. For both cases, numerous contributing factors were cited including several cognitive factors (confirmation bias, mental fatigue and channeled attention on a single issue), compliance errors and communication factors.
Interestingly, almost two-thirds of the events occurred in minor procedures, where surgical complexity itself does not play a leading role. Our institution has previously instituted the universal protocol to prevent wrong side/site surgery, preoperative team briefings or huddles before a case is started, a procedural pause just before incision, and debriefings using the WHO recommended safety checklist. Despite these measures, events continue to occur, albeit at reduced rates. Further evaluation of the mechanisms of cognitive failures in these ‘minor procedures’ should be undertaken.
Our results suggest that RFOs and wrong implants had more contributing factors per event than wrong procedure and wrong side/site surgery. Further analysis should be done to better understand the difference between event mechanisms. We also need to understand if the defined systems and procedures in place at our institution to prevent RFO's and wrong implants are more in number or more effective than the safety layers in place to prevent wrong side/site surgery and wrong procedures.
To our knowledge, this is the first report of a validated human factors analysis applied prospectively to surgical and procedural never events. Our study provides human factors data from RCAs, prospectively collected by a trained patient safety specialist which also represents a limitation of our study. A single, non-clinician reviewer was responsible for coding the cases into HFACS, which may have resulted in the under-coding of patient and situational factors. For example, a number of events occurred during emergently scheduled procedures; however, this was not a commonly coded situational factor (n=3). This could be due to coding oversight; alternatively, other human factors may have been judged causative rather than the emergency scheduling.
Our study suggests that in addition to aforementioned systems approaches and interventions to improve communication, attention should be paid to the cognitive capacity - cognitive workload balance in the OR and procedural practices. The cognitive workload may be affected by team composition, technology interfaces, time pressures, individual fatigue and others.24 A first step to influence this balance is to increase awareness about cognitive and other human factors contributing to never events across many layers of the institution, including administrative teams. Measures to decrease the cognitive workload should be considered, which affect everything from patient and staff scheduling, to supply chain management, information technology, teaching and gaining independence in the operating room. If the workload cannot be decreased, there may be options to share the cognitive workload between team members. This will require team member engagement, and maintaining stable teams will be helpful to accomplish this as suggested in the study by Xiao et al (24). Our institution has implemented a ‘speak-up’ campaign to break down traditional hurdles in communication. We are currently piloting team-based engagement in the OR to assess if this will create the necessary human factors redundancy to reduce never events. While we may not be able to prevent providers from making cognitive errors, we can create systems that acknowledge when these errors may be occurring, provide assistance and therefore prevent the subsequent negative consequences for patients. These results delineate targets to further reduce never events from our healthcare system. Targeting interventions to address cognitive factors and team resource management as well as perceptual biases may reduce errors and further improve patient safety.
Supplementary Material
ACKNOWLEDGEMENTS
Research reported in this manuscript was supported in part by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under award number K23DK93553. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding: Research reported in this manuscript was supported in part by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under award number K23DK93553. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
ABBREVIATIONS
- HFACS
Human Factors Analysis and Classification System
- RFO
retained foreign object
- OR
operating room
- RCA
root cause analysis
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented at the 10th Annual Academic Surgical Congress in Las Vegas, NV, February 3-5, 2015
DISCLOSURES
Cornelius Thiels - Nothing to disclose
Tarun Mahan Lal - Nothing to disclose
Joseph Nienow - Nothing to disclose
Kalyan Pasupathy - Nothing to disclose
Renaldo Blocker - Nothing to disclose
Johnathon Aho - Nothing to disclose
Timothy Morgenthaler - Nothing to disclose
Robert Cima - Nothing to disclose
Susan Hallbeck - Dr. Hallbeck receives grant funding from Stryker Endoscopy. This funding is not perceived as constituting a conflict of interest for the submitted manuscript.
Juliane Bingener - Dr. Bingener is supported through a research grant (NIDDK), specified research through Nestle and Stryker Endoscopy, has received travel support from Intuitive Surgical, and serves on the Surgeon Advisory Board for Titan Medical. She perceives no conflict of interest as it relates to this manuscript. Other than Dr. Bingener's time, no financial support was provided for the preparation of this manuscript.
REFERENCES
- 1.Tichansky D, Morton J, Jones D. The SAGES Manual of Quality, Outcomes, and Patient Safety. New York: 2012. [Google Scholar]
- 2.Serious Reportable Events In Healthcare—2011 Update: A Consensus Report. Washington DC: 2011. [Google Scholar]
- 3.The Joint Commission. Sentinel Event Policy and Procedures. 2013 [Google Scholar]
- 4.Vincent C. Understanding and responding to adverse events. N Engl J Med. 2003 Mar 13;348(11):1051–6. doi: 10.1056/NEJMhpr020760. [DOI] [PubMed] [Google Scholar]
- 5.Mehtsun WT, Ibrahim AM, Diener-West M, Pronovost PJ, Makary MA. Surgical never events in the United States. Surgery. 2013 Apr;153(4):465–72. doi: 10.1016/j.surg.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 6.Provisional publication of never events reported as occurring between 1 April and 31 October 2014. AMA News; London: 2014. [Google Scholar]
- 7.Stahel PF, Sabel AL, Victoroff MS, Varnell J, Lembitz A, Boyle DJ, et al. Wrong-site and wrong-patient procedures in the universal protocol era: analysis of a prospective database of physician self-reported occurrences. Arch Surg. 2010 Oct;145(10):978–84. doi: 10.1001/archsurg.2010.185. [DOI] [PubMed] [Google Scholar]
- 8.Hallbeck MS, Koneczny S, Büchel D, Matern U. Ergonomic usability testing of operating room devices. Stud Health Technol Inform. 2008 Jan;132:147–52. [PubMed] [Google Scholar]
- 9.Reason J. Human error: models and management. BMJ. 2000 Mar 18;320(7237):768–70. doi: 10.1136/bmj.320.7237.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perrow C. Living with high-risk technologies. Princeton University Press: John Wiley and Sons Ltd; New Jersey: 1999. [Google Scholar]
- 11.Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat A-HS, Dellinger EP, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009 Jan 29;360(5):491–9. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 12.Hu Y-Y, Greenberg CC. Patient safety in surgical oncology: perspective from the operating room. Surg Oncol Clin N Am. 2012 Jul;21(3):467–78. doi: 10.1016/j.soc.2012.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu AW, Lipshutz AKM, Pronovost PJ. Effectiveness and efficiency of root cause analysis in medicine. JAMA. 2008 Feb 13;299(6):685–7. doi: 10.1001/jama.299.6.685. [DOI] [PubMed] [Google Scholar]
- 14.Wiegmann D, Shappell S. Human Error Approach to Aviation Accident Analysis: The Human Factors Analysis and Classification System. Aldershot. 2003 [Google Scholar]
- 15.Olsen NS, Shorrock ST. Evaluation of the HFACS-ADF safety classification system: inter-coder consensus and intra-coder consistency. Accid Anal Prev. 2010 Mar;42(2):437–44. doi: 10.1016/j.aap.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Diller T, Helmrich G, Dunning S, Cox S, Buchanan A, Shappell S. The Human Factors Analysis Classification System (HFACS) applied to health care. Am J Med Qual. 29(3):181–90. doi: 10.1177/1062860613491623. [DOI] [PubMed] [Google Scholar]
- 17.ElBardissi AW, Wiegmann DA, Dearani JA, Daly RC, Sundt TM. Application of the human factors analysis and classification system methodology to the cardiovascular surgery operating room. Ann Thorac Surg. 2007 Apr;83(4):1412–8. doi: 10.1016/j.athoracsur.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 18.Kohn L, Corrigan J, Donaldson M. To Err is Human: Building a Safer Health System. Washington, D.C.: 1999. [PubMed] [Google Scholar]
- 19.Landrigan CP, Parry GJ, Bones CB, Hackbarth AD, Goldmann DA, Sharek PJ. Temporal trends in rates of patient harm resulting from medical care. N Engl J Med. 2010 Nov 25;363(22):2124–34. doi: 10.1056/NEJMsa1004404. [DOI] [PubMed] [Google Scholar]
- 20.Cuschieri A. Nature of human error: implications for surgical practice. Ann Surg. 2006 Nov;244(5):642–8. doi: 10.1097/01.sla.0000243601.36582.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cima RR, Kollengode A, Clark J, Pool S, Weisbrod C, Amstutz GJ, et al. Using a data-matrix-coded sponge counting system across a surgical practice: impact after 18 months. Jt Comm J Qual Patient Saf. 2011 Feb;37(2):51–8. doi: 10.1016/s1553-7250(11)37007-9. [DOI] [PubMed] [Google Scholar]
- 22.Hariharan D, Lobo DN. Retained surgical sponges, needles and instruments. Ann R Coll Surg Engl. 2013 Mar;95(2):87–92. doi: 10.1308/003588413X13511609957218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lowndes B, Hallbeck M. The use of human factors and ergonomics to promote safety and efficiency in the operating room, with an emphasis on minimally invasive surgery. Hum Factors Ergon Manuf Serv Ind. 2014;24(3):308–317. [Google Scholar]
- 24.Xiao Y, Jones A, Zhang BB, Bennett M, Mears SC, Mabrey JD, et al. Team Consistency and Occurrences of Prolonged Operative Time, Prolonged Hospital Stay, and Hospital Readmission: A Retrospective Analysis. World J Surg. 2014 Dec 4; doi: 10.1007/s00268-014-2866-7. [Epub ahead of print] Published online. DOI 10.1007/s00268-014-2866-7. [DOI] [PubMed] [Google Scholar]
- 25.Mattett R, Conroy M, Zaidain Saslaw L, Moffatt-Bruce S. Preventing Wrong Site, Procedure, and Patient Events Using a Common Cause Analysis. Am J Med Qual. 2012 Jan-Feb;27(1):21–9. doi: 10.1177/1062860611412066. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.