Abstract
Objective
To explore high-stakes surgical decision making from the perspective of seniors and surgeons.
Background
A majority of older chronically ill patients would decline a low-risk procedure if the outcome was severe functional impairment. However, 25 percent of Medicare beneficiaries have surgery in their last three months of life, which may be inconsistent with their preferences. How patients make decisions to have surgery may contribute to this problem of unwanted care.
Methods
We convened four focus groups at senior centers and two groups of surgeons in Madison and Milwaukee, Wisconsin, where we showed a video about a decision regarding a choice between surgery and palliative care. We used qualitative content analysis to identify themes about communication and explanatory models for end-of-life treatment decisions.
Results
Seniors(N = 37) and surgeons (N = 17) agreed that maximizing quality of life should guide treatment decisions for older patients. However, when faced with an acute choice between surgery and palliative care, seniors viewed this either as a choice between life and death or a decision about how to die. Although surgeons agreed that very frail patients should not have surgery they held conflicting views about presenting treatment options.
Conclusions
Seniors and surgeons highly value quality of life but this notion is difficult to incorporate in acute surgical decisions. Some seniors use values to consider a choice between surgery and palliative care, while others view this as a simple choice between life and death. Surgeons acknowledge challenges framing decisions and describe a clinical momentum that promotes surgical intervention.
Introduction
Operations on older patients with chronic illnesses are common and increasing1 such that 25 percent of Medicare beneficiaries will have a surgical procedure within the last three months of life.2 Surgery on frail elderly patients generally has a limited ability to prolong survival or return patients to the quality of life they had before surgery.3, 4 As a majority of older, chronically ill patients report they would decline even a low-risk intervention if the likely outcome was severe functional impairment,5 surgery can burden older frail patients with aggressive treatments they do not want. Because patients who receive surgery near the end of life are more likely to spend time in intensive care (ICU) or have a prolonged hospitalization,2 a decision to proceed with surgery can start a clinical trajectory that is inconsistent with personal preferences and goals.
Surgeons are often called upon in acute situations to consider invasive treatments that significantly impact patients' quality of life. These pivotal encounters are made more difficult because the surgeon and patient rarely have a pre-existing relationship and patients' preferences are often not precisely defined in an advance directive or may change during a specific acute illness.6-8 Furthermore, surgeons' conversations are framed by the structure of informed consent which functions poorly as a vehicle for decision making.9 Although shared decision making holds promise for improving high-stakes clinical decision making by aligning patients' values with the appropriate treatment choice, contemporary efforts to improve shared decision making between patients and surgeons have focused on the out patient setting.10, 11
Given the disconnect between the widely-held beliefs of older patients and the treatments they receive at the end of life, we theorize that the decision to proceed with surgery for frail elderly patients who are unlikely to benefit from surgery contributes to the problem of unwanted care. In this paper we explore the challenges of high-stakes surgical decision making from the perspective of seniors and surgeons using qualitative content analysis of focus group discussions.
Methods
We developed a tool to help structure in-the-moment conversations between surgeons and patients that would help align surgical treatments with the outcomes frail elderly patients prefer. We then recruited seniors and surgeons in Wisconsin for focus groups to provide feedback and refine our communication tool called “best case/worst case.”12 Although the primary aim of our study was to seek input on the tool (results described in a different manuscript), both seniors and surgeons also reported their experiences and beliefs about making difficult treatment decisions. In this study, we analyze the content about high-stakes, in-the-moment decisions in the setting of a choice between surgery and palliative care.
Focus Group Participants
We convened four focus groups at senior centers and two groups of surgeons in Madison and Milwaukee, WI. We used purposeful sampling to target senior centers with different socio-economic and ethnic-racial backgrounds. We included English-speaking adults age 60 and older who reported experience with a difficult medical decision for themselves or a loved one in the past 10 years. We then sub-selected those who expressed interest in the study by age and sex.
We included surgeons who practice general, vascular, cardiothoracic and neurologic surgery from private and academic practices who in the last 3 months had treated at least one elderly patient with a non-elective surgical problem and at least one patient who required admission to the intensive care unit (ICU). We used a snowball sampling technique whereby 2 investigators (MLS, KJB) emailed 5 surgeons in their local area and asked each surgeon to identify 5-10 surgeons who might meet our inclusion criteria; these surgeons were then invited to participate. Study investigators were subsequently blinded to the identification of all surgeon-respondents with the exception of one member of the research team (NMS) who invited 10 surgeons from each city who expressed interest and met inclusion criteria based on the surgeon's practice characteristics, age, and gender.
Each focus group session was audio recorded and transcribed verbatim and identifying information of respondents was redacted. Seniors and surgeons gave written informed consent and received cash honoraria at the completion of the 90-minute session. This study was approved by the Social Sciences Institutional Review Board of the University of Wisconsin-Madison.
Focus Group Guide
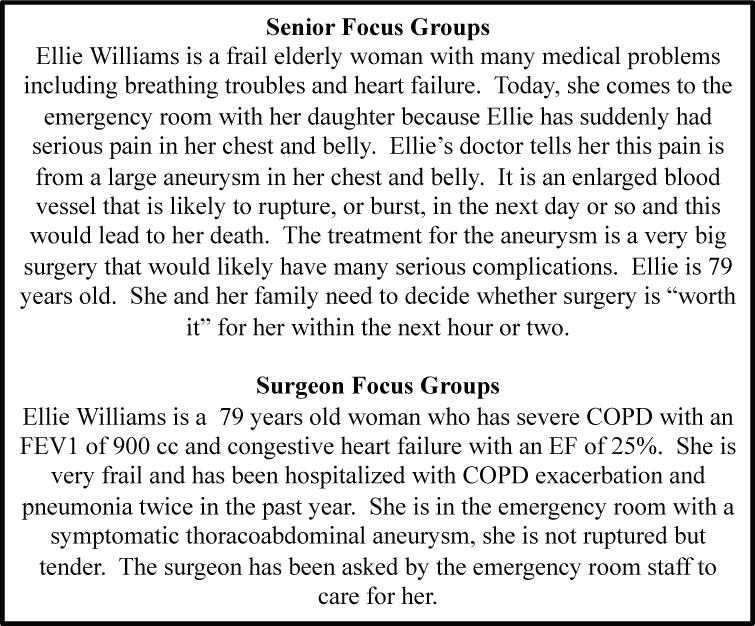
A trained moderator from the University of Wisconsin Survey Center facilitated each 90 minute session. Seniors were prompted to describe their experience making a decision that was preference-sensitive by asking participants to describe a medical decision that involved a “trade-off” between desirable and undesirable outcomes. The facilitator then described a scenario about a frail, 79 year-old woman with multiple comorbidities and a tender thoracoabdominal aneurysm (TAA) (see Box1), and asked participants to describe what they might want to know if they had to make a decision about surgical treatment. (for focus group guide, see Supplemental Digital Content 1)
Next, the moderator showed a 7-minute video of a surgeon discussing treatment options for TAA with the patient described in the scenario. The surgeon in the video used our novel communication tool called “best case/worse case” to present treatment options as a choice between surgery and palliative care.12,13 (for transcript, see Supplemental Digital Content 2) Two vascular surgeons independently reviewed the video to confirm that the presentation accurately represented the range of outcomes for surgery and palliative care based on the patient's comorbidities. The facilitator then asked seniors questions derived from the Decision Aid Acceptability Scale13 and Decisional Conflict Scale14 that were modified to fit the focus group format. Focus group participants completed a short anonymous exit survey that included demographic questions and the Control Preferences Scale.15
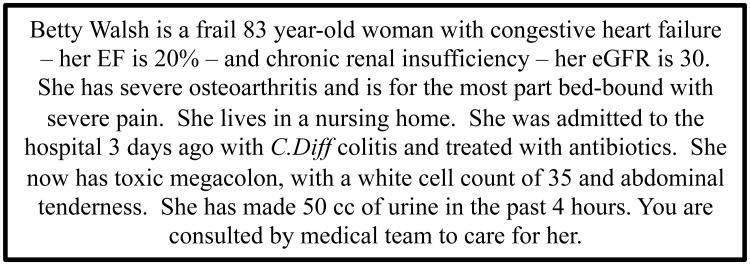
Surgeon focus groups followed the same format with two modifications. First, surgeons were asked to describe the challenges of talking with frail, elderly patients about surgery. Then the moderator described a frail 83-year-oldwoman with multiple comorbidities, including dementia, who presented with toxic mega colon from C. difficile colitis (see Box 2). We instructed surgeons to assume the role of consulting surgeon and queried them about their discussion of treatment options with this patient and her family. Surgeons then watched the same video shown to seniors of an older woman with a tender TAA and were asked modified questions from the Decision Aid Acceptability Scale13 and Decisional Conflict Scale.14
Analysis
We used content analysis to analyze each written transcript inductively without pre-formulated hypotheses or theories.16 After independent analysis of the first transcript by all seven investigators, at least three members of the research team convened to discuss each coded phrase or idea. This procedure was repeated for each subsequent transcript using the technique of constant-comparison, whereby codes were continually refined against previous uses of the code17 ultimately developing a catalogue of consensus codes that we used for all 6 focus group transcripts. This allowed for new codes to arise as they presented in the data and for continual refinement of codes as patterns emerged. We used the group process of code reconciliation to generate higher level concepts about patient-surgeon communication, decisional needs of seniors and explanatory models about end-of-life treatment decisions. We ceased conducting focus groups when we reached theoretical saturation, i.e. when concepts, themes and trends were found to have a predictable degree of regularity within the data. We used NVivo software (QSR International) for data management.
Researchers
The research team has shared experience of high-stakes decision making in critically ill elderly patients and represents an intentional collection of diverse professional backgrounds: surgery (MJN, KJB, MLS), intensive care (KJB), internal medicine (JMK, TCC), palliative care (KJB, TCC) patient advocacy (NMS, MEG) and public health (NMS).These different professional identities allowed us to consider a variety of interpretations of the data and manage assumptions and role-based biases throughout analysis.
Results
Thirty-seven seniors and seventeen surgeons participated in the focus groups. Participants had a range of educational backgrounds, nearly 75% of senior participants were women and over 80% of surgeon participants were men. The majority of seniors preferred to have either a major role in decision making or share some responsibility with their doctor. (Table 1)
Table 1. Participant Characteristics.
| Seniors (N=37) | Number (%) |
|---|---|
| Male | 10 (27) |
|
| |
| Age, (yr) | |
| 60-69 | 15 (41) |
| 70-79 | 10 (27) |
| >80 | 12 (32) |
|
| |
| Race/Ethnicity* | |
| White | 26 (70) |
| Black or African American | 3 (8) |
| Hispanic | 5 (13) |
| Other | 1 (3) |
|
| |
| Education* | |
| Some high school or less | 1 (3) |
| High school diploma or GED | 10 (27) |
| Occasional college or some college | 9 (24) |
| College degree | 9 (24) |
| Professional or graduate degree | 6 (16) |
|
| |
| Seniors' Decision Making Preferences† | |
| I prefer to make the decision about which treatment I will receive. | 4 (11) |
| I prefer to make the final decision about my treatment after seriously considering my doctor's opinion. | 18 (49) |
| I prefer that my doctor and I share responsibility for deciding which treatment is best for me. | 6 (16) |
| I prefer that the doctor makes the final decision about treatment that will be used, but seriously considers my opinion. | 1 (3) |
| I prefer leaving all decisions about my treatment to my doctors. | 0 (0) |
| Multiple responses | 7 (19) |
|
| |
| Surgeons (N=17) | |
|
| |
| Male | 14 (82) |
|
| |
| Specialty‡ | |
| General (colorectal, surgical oncology, trauma) | 10 (59) |
| Vascular | 4 (24) |
| Cardiothoracic | 4 (24) |
| Neurosurgery | 2 (12) |
|
| |
| Practice Location | |
| Academic | 12 (71) |
| Private Practice | 5 (29) |
Two seniors did not respond
One senior did not respond
Several surgeons practiced general and vascular surgery i.e. percentage >100%
During discussions about aging and long-term goals, both seniors and surgeons voiced strongly held beliefs about the importance of maintaining independence and quality of life at the end of life. When presented with an in-the-moment treatment decision, seniors used two models to evaluate the choice between surgery and palliative care, one of which did not incorporate previously stated preferences about quality of life. Likewise, surgeons described the presentation of treatment options in this setting using a variety of choice constructions and identified forces beyond the decision-making conversation that promote surgical intervention.
Seniors on quality of life
There was broad consensus among seniors about the desire to maintain quality of life near the end of life, worry about the potential for dying poorly, and fear of living in a nursing home. Seniors regularly asserted that quality of life, and not life prolongation, should guide medical decision making for older patients. They were particularly concerned about their future ability to converse with relatives, ambulate, avoid suffering, and make decisions. Seniors noted that loss of independence was abhorrent and frequently endorsed death as preferable in comparison to prolonged life where they would be dependent on family or other care providers for basic needs. One senior said, “If I'm going to go, then you just take me at 79 when my mind is good, my health is good, and, I mean, my brain is good, because I don't want to live [to] 80 and be dependent.”
Seniors believed that living in a nursing home would lead to personal suffering, loneliness, depression and a downward trajectory toward the end of life. Only one senior expressed a positive view of nursing homes based on her mother's experience at a “good” nursing home. Seniors viewed living in a nursing home as so undesirable that if long-term residence in a nursing home was described as a possible outcome of a medical decision this would force the option most likely to prevent nursing home residence. For example, during the initial discussion about trade-offs, one senior describing her choice about pacemaker insertion said, “I didn't have a choice… I'd have to go to a nursing home and be taken care of, or get the pacemaker.”
Choosing between surgery and palliative care
Although seniors largely asserted that quality of life and avoidance of dependency should guide medical decisions for older patients, when presented with a specific choice between surgery and palliative care for a patient with a tender TAA where the best postoperative outcome was described as functional dependence in a nursing home, many respondents did not use this information to determine their choice. Instead, seniors in all four focus groups understood the decision to have surgery or palliative care in one of two ways: 1) a choice between life and death, or 2) a choice about how to die. (Table 2)
Table 2. How seniors decide between surgery and palliative care.
| Decision Construct | Underlying reasoning | Quotes |
|---|---|---|
| Life or death | Imperative to choose life
|
|
It's better to die trying
|
|
|
Life is better than stated
|
|
|
| How to die | Death is the outcome of surgery and supportive care
|
|
Desire to control how death occurs
|
|
Choosing Life or Death
Within the life-or-death framework seniors asserted that it was obligatory to choose life and thus choose surgery. This sentiment was expressed in various ways; a moral imperative to continue living; a religious act - putting faith in God to decide between life and death; and a notion that it is not acceptable to choose death. Seniors reported that failure to do everything possible to stay alive or a decision to take a less aggressive stance would be associated with profound guilt; declining any life prolonging measure was evading responsibility to live and choosing death would disappoint others. Several seniors expressed dismay that palliative care was presented as an option; they believed all interventions that had a chance of preventing death should be done without question or deliberation. Some seniors noted that it was not up to them to make life or death decisions and appealed to divine intervention, for example “if someone said that was going to rupture in a day or so, I would do everything possible, and I would say, I'm having that surgery and put it in the Lord's hands.”
Seniors also explained that it was preferable to die during attempts to prolong life: they believed it was better to die trying. This conviction hinged on two beliefs; 1) that surgery was something that could be attempted and then easily stopped if the outcome was undesirable and 2) when death is the outcome of surgery it is painless. Although the surgeon in the video specifically noted that perioperative death would occur much later in the ICU and did not mention intraoperative death as a possibility, seniors maintained a belief that if death were to occur it would be in the operating room, something they viewed as painless. Furthermore, seniors valued death in the operating room as it satisfied the need to pursue life and avoided the emotional hazards associated with deciding to withdraw life sustaining treatments later. Thus surgery was a good choice because if death occurred, it was both painless and out of the patient's control.
Seniors' rationale for choosing surgical intervention was also based on doubt about the accuracy of the information provided. They believed the surgeon was concealing the possibility that surgery would go “well” and despite the surgeon's statements to the contrary they believed that by choosing surgery the patient could lead “a normal life” afterwards. Seniors' distrust of information was not necessarily directed at the surgeon; instead they felt betrayed by medicine in general. They struggled to believe that medical technology had nothing else to offer a frail, elderly woman with multiple comorbidities and asymptomatic TAA. Seniors made requests for a “second or third opinion” and insisted “there must be other options.” Several seniors wanted to know what a “successful” surgery would look like as opposed to a markedly reduced functional state that was described in the best case scenario with surgery.
Choosing how to die
Seniors who considered palliative care as a legitimate treatment strategy viewed death as the likely outcome of both surgery and palliative care. (Table 2) Although they noted that the patient might live longer if she chose to have surgery, they believed that the patient's condition after surgery would be highly undesirable. They reasoned that the patient would ultimately die even with surgery, therefore surgical intervention and life prolongation was not worthwhile. Within this construct they made statements about how they would want their own death to proceed: they wanted it to be peaceful and without undue burden on their families. They wanted to maximize comfort, pain control and time with family members. For example, “he's telling me… I'm going to die anyway, so I'd rather say goodbye to my family and just give me pain control … so I'd tell them bye.”
These seniors believed that life as it was before the patient developed a tender TAA was not a possible outcome of surgical intervention. Thus, they would prefer to avoid suffering that could not restore their previous health state. One senior said, “No, I wouldn't go through the surgery when he say[s] to you, I know I'm going to die anyway… I don't want to deal with a nursing home or be unable to do stuff by myself, so I'd rather just go on and not suffer anymore.” Seniors who used this construction to evaluate treatment options viewed death as a natural event and palliative care as a rational and acceptable option. These seniors also desired control over the dying process. For example, “death is natural for everybody. It's just, I think everyone would like to have some control over how they're going to die.”
Surgeons on quality of life
Like seniors, surgeons emphasized the importance of quality of life when evaluating treatment options for older patients, and noted that morbidity was a far more important outcome than mortality. Surgeons were less precise about their definition of poor quality of life describing it as “loss of function” or “permanent functional difficulties.” Surgeons similarly reported that living in a nursing home was “miserable” or a “fate worse than death” and shared concerns about the power of the nursing home to motivate decision making.
Presentation of options
There was consensus, though not unanimous, that both the patient with a tender TAA and the patient with toxic megacolon described in the surgeons' focus group script had non-survivable problems and that even with surgery the outcome was decidedly poor. Surgeons agreed that there was ethical tension between their obligation to limit the burdens of surgery to patients who would have a valuable outcome and their duty to rescue the critically ill patient. Surgeons differed about the right way to frame this treatment discussion and noted how difficult it was to communicate their professional opinion that even though surgery could be done, it should not be done.
Some surgeons believed the likelihood of a good outcome was so small and the burdens of treatment were so high, that they would not offer surgery to the patients we described or others they described with similarly non-salvageable conditions. (Table 3) For example, “Sometimes people want something done I won't ethically [or] morally do. I'm not in favor of cutting off a septic leg in an 88-year-old comatose lady from a nursing home because there's no future.” Surgeons gave two explanations for this strategy 1) they would not want their own mother operated on under these circumstances and 2) their professional duty required that they avoid burdening patients with an intervention when there was no reasonable expectation for survival.
Table 3.
Surgeons' presentation of treatment options for very frail patients.
| Choice Presentation | Rationale | Quotes |
|---|---|---|
|
No choice Surgery is not offered |
|
|
| Biased choice |
|
|
| Simple choice |
|
|
Other surgeons reported that they would offer and perform surgery if the patient and/or family insisted, but they would frame the decision-making conversation in a way that would bias the choice against surgery. For example, “I mean, you, we've made our decision that probably this patient really doesn't warrant a surgery … And so you make that decision when you go see that patient, and you're going to steer the patient and the family in the direction of conservative [treatment] …” Still others noted they would present the decision for surgery or palliative care as an individual choice about the trade offs between risks and benefits; they would present the options and let the patient and family to decide whether surgery should be performed. “… I see my job to try and help them understand what their options are. Their job is to choose, you know.”
Clinical Momentum
Surgeons expressed resignation that the patients described would have an operation, regardless of the value of surgery for the patient. This was attributed to factors outside the surgeon's control; end-of-the-day or middle-of-the-night consults, inadequate time for decision making, and expectations from consulting physicians. Surgeons noted that before they even spoke with the patient or family the operating room had been called, in good faith by someone trying to expedite care, and that it was just easier to operate than to explain to the family why surgery was not the right treatment.
Surgeons described a progression of clinical momentum whereby the diagnosis of a surgical problem pushed the care trajectory along an inevitable course towards intervention that they were unable to stop. Surgeons believed that patients and families presume a surgical consultation signals surgery is the appropriate treatment strategy. Surgeons also held referring physicians accountable for starting a process that did not consider the patient's overall health. For example, “I'll get some woman in the office who's 75, smoked all her life, on oxygen, in a wheelchair, on anti-coagulated [sic] for her heart disease. Somebody gets a mammogram. They find a little spot. They biopsy the little spot. It's a little cancer. She'll show up with six family members who are just all, you know, this cancer has got to be treated, when the woman has got a life expectancy probably less than two years.” Another surgeon described an emergency consultation for a patient with severe dementia and subdural hemorrhage. He was frustrated and baffled that he had been asked by the emergency room physician to treat the patient's acute bleeding. “[I told him] well, the best-case scenario is I get her back to being [an]end-stage Alzheimer's patient who's completely aphasic and not ambulatory. And they go, ‘oh, we guess we never thought of that.’”
Discussion
Seniors and surgeons universally agreed that maximizing quality of life and avoiding loss of independence should guide treatment decisions for older patients. However, when faced with an acute choice between surgery and palliative care where the best surgical outcome is described as prolonged hospitalization and long-term nursing home care, seniors viewed this either as a choice between life and death or a decision about how to die. Seniors who saw this decision as a life or death choice felt it was morally unacceptable to choose death and it would be better to die in the operating room where death would be determined by the surgeon and/or God. Others believed that surgery would only prolong the dying process and expressed a desire to control how they die emphasizing comfort and time with family.
Although surgeons agreed that very frail patients should not have surgery they held conflicting views about how to present treatment options; some surgeons would not offer surgery, others would heavily favor palliative care and some would state the options and let the patient or family decide. Surgeons noted several factors beyond their control that contribute to a clinical momentum promoting surgical intervention despite professional concerns that surgery is not valuable. These findings are important because they suggest that misunderstandings and faulty expectations determine the outcome of high-stakes surgical decision making. Observation of these challenges to surgical decision making presents an opportunity to assist frail elderly patients and their families in the setting of acute surgical illness and has important implications for surgeons, patients and policy makers.
For surgeons, it is critical to appreciate and dispel false assumptions about treatment outcomes for frail elderly patients. It is not surprising that patients who feel it is better to die trying would choose an operation with 60% mortality because they believe that death would occur painlessly and out of their control in the operating room. As intra operative death is a rare occurrence, surgeons need to illustrate the cascade of postoperative complications and interventions that typically precede postoperative death rather than simply stating the statistical probability of death. Surgeons will also need to describe the range of surgical outcomes for the individual patient within the context of the patient's overall prognosis with careful attention to the patient's health trajectory before surgical illness. Given patient skepticism and popular notions about the capacity of modern medicine18 this may require support from surgical colleagues or the patient's primary care physician. While the logistics of this strategy are onerous, the chance to avoid an unwanted burdensome intervention may be invaluable to the patient and his/her family. Furthermore, such efforts may prevent surgeon frustration, dismay and emotional accountability stemming from downstream withdrawal of postoperative life supporting treatments.19-21,20
For patients, our data show that aligning personal preferences with treatment decisions is extremely difficult in the acute setting. Because physicians in general discuss treatments and fail to offer information about long-term prognosis22-24 patients and their families are woefully unprepared for an acute event and struggle to place a decision about surgery within the larger context of their overall health. Instead they use heuristics to choose surgery 25 and may not incorporate their previously stated preferences and values about quality of life. These overly simplified decisions may lead to unwanted invasive treatments at the end of life. We are hopeful that some seniors were able to do the harder work of imagining their reaction to future health states and could see that the best outcome of surgery was a state where quality of life was not acceptable. Future efforts to improve decision making will need to focus on helping patients move from intuitive-emotional decision making and embrace effortful and more analytic decision making.26
For policy makers, specifically hospital administrators, we have identified a link between current systems to encourage efficiency and unwanted care. Hospital processes that increase efficiency may benefit patients through provision of earlier treatment, reduced length of stay and decreased hospital costs. However, these same efficiencies inhibit opportunity for deliberation between doctors and patients about whether intervention is even appropriate. This is further compounded by messages inferred from physicians requesting surgical consultation and family expectations to produce a powerful force of clinical momentum that favors intervention and is difficult to reverse with a simple conversation between surgeon and patient.
Our study highlights an ethical tension for surgeons about how to discuss possible treatments for patients who are unlikely to survive postoperatively. When surgeons present surgery as a possible option, patients and their families may view surgery as beneficial even though the surgeon thinks differently.27 The harms that ensue from this misunderstanding include not only the burden of unwanted treatment at the end of life but also decisional regret for family members who assume responsibility for a treatment decision leading to their loved one's death if they decline surgery. In addition, our data highlight that seniors prefer to make difficult decisions in conjunction with their physician rather than choose from a menu of treatment options. As such, a better strategy would focus the discussion on prognosis and goals (as opposed to treatments and choices) and culminate with a strong recommendation from the surgeon. While many acute surgical illnesses do not predictably lead to grim outcomes like those described in our focus group, it is important to recognize and avoid the unnecessary damage incurred by presenting patients and families with a choice when the benefits of surgery are so limited.22
Our study has several limitations. The focus group script was designed to elicit feedback regarding a communication tool, thus there were no prompts or mechanism to explore the themes described herein more fully. The surgeon in the video noted that death was the most likely outcome of surgery and stated that choosing supportive care was an “acknowledgment” that the aneurysm would be fatal. Although this structure is significantly different than “if we don't operate you will die,” the conversation portrayed in the video may have influenced the “life or death” construct our senior respondents reported. While we purposefully selected seniors who had experience making difficult medical decisions, all participants were community dwelling and presumably had some distance from the prospect of acute illness. Consistent with prospect theory, less healthy participants may have expressed stronger preferences for life sustaining interventions 28 or have a broader definitions about acceptable quality of life. Further more our study was not designed to examine how religious belief influences decisions but it is likely that such beliefs impact these difficult choices.29 Finally, surgeons in Wisconsin may have distinctly different viewpoints on invasive treatments at the end of life given known geographic variations in treatment styles.30
Conclusions
Although seniors and surgeons highly value quality of life at the end of life, this notion is difficult to incorporate in acute surgical decisions. Some seniors are able to use their values to consider a choice between surgery and palliative care, while others view this as a simple choice between life and death, and choosing life is obligatory. Surgeons acknowledge significant challenges framing decisions about surgery with limited value and cite forces beyond the decision-making conversation that promote surgical intervention.
Supplementary Material
Figure 1. Thoracoabdominal Aneurysm Scenario.
Figure 2. Toxic Megacolon Scenario: Surgeon Focus Groups.
Acknowledgments
The authors would like to thank Ken Croes, PhD from the UW Survey Center for his moderation of the focus groups, Layton “Bing” Rikkers, MD for his role as study champion, the Collaborative Center for Health Equity (ICTR CCHE), and the Community-Academic Aging Research Network (CAARN) for their help with focus group participant recruitment, the Qualitative Research Group (ICTR QRG) and Nora Jacobson, PhD for assistance with study design and presentation of results and Bob Arnold, MD for his comments on an earlier version of this manuscript.
Financial Support: Dr. Schwarze is supported by a training award (KL2TR000428) from the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant (UL1 TR000427) and the Greenwall Foundation (Greenwall Faculty Scholars Program.) The project described was also supported by the National Institute for Minority Health and Health Disparities Center of Excellence program, through the UW Collaborative Center for Health Equity (CCHE) grant (5P60MD003428.) These funding sources had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; and preparation, review, or approval of the manuscript for publication. No other financial support was declared for the remaining authors.
Footnotes
Reprints will not be available from the authors.
References
- 1.Barnato AE, McClellan MB, Kagay CR, et al. Trends in inpatient treatment intensity among Medicare beneficiaries at the end of life. Health Serv Res. 2004;39:363–75. doi: 10.1111/j.1475-6773.2004.00232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwok AC, Semel ME, Lipsitz SR, et al. The intensity and variation of surgical care at the end of life: a retrospective cohort study. Lancet. 2011;378:1408–13. doi: 10.1016/S0140-6736(11)61268-3. [DOI] [PubMed] [Google Scholar]
- 3.Finlayson E, Zhao S, Boscardin WJ, et al. Functional status after colon cancer surgery in elderly nursing home residents. J Am Geriatr Soc. 2012;60:967–73. doi: 10.1111/j.1532-5415.2012.03915.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Finlayson E, Fan Z, Birkmeyer JD. Outcomes in octogenarians undergoing high-risk cancer operation: a national study. J Am Coll Surg. 2007;205:729–34. doi: 10.1016/j.jamcollsurg.2007.06.307. [DOI] [PubMed] [Google Scholar]
- 5.Fried TR, Bradley EH, Towle VR, et al. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346:1061–6. doi: 10.1056/NEJMsa012528. [DOI] [PubMed] [Google Scholar]
- 6.White DB, Arnold RM. The evolution of advance directives. JAMA. 2011;306:1485–6. doi: 10.1001/jama.2011.1430. [DOI] [PubMed] [Google Scholar]
- 7.Fagerlin A, Schneider CE. Enough. The failure of the living will. Hastings Cent Rep. 2004;34:30–42. [PubMed] [Google Scholar]
- 8.Sudore RL, Fried TR. Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med. 2010;153:256–61. doi: 10.1059/0003-4819-153-4-201008170-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pecanac KE, Kehler JM, Brasel KJ, et al. It's Big Surgery: Preoperative Expressions of Risk, Responsibility, and Commitment to Treatment After High-Risk Operations. Ann Surg. 2014;259:458–463. doi: 10.1097/SLA.0000000000000314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaplan AL, Crespi CM, Saucedo JD, et al. Decisional Conflict in Economically Disadvantaged Men With Newly Diagnosed Prostate Cancer: Baseline Results From a Shared Decision-Making Trial. Cancer. 2014 doi: 10.1002/cncr.28755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.An introduction to patient decision aids. BMJ. 2013;347:f4147. doi: 10.1136/bmj.f4147. [DOI] [PubMed] [Google Scholar]
- 12.Schwarze ML, Kehler JM, Campbell TC. Navigating High Risk Procedures with More than Just a Street Map. J Palliat Med. 2013;16:1169–1171. doi: 10.1089/jpm.2013.0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O'Connor A, Cranney A. [Accessed July 7, 2013];User Manual - Acceptability. 1996 document on the Internet. Available at: http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Acceptability.pdf.
- 14.O'Connor AM. [Accessed January 23, 2014];Decisional Conflict Scale. 1993 [updated 2005]. Available at: www.ohri.ca/decisionaid.
- 15.Degner LF, Sloan JA, Venkatesh P. The Control Preferences Scale. Can J Nurs Res. 1997;29:21–43. [PubMed] [Google Scholar]
- 16.Kondracki NL, Wellman NS, Amundson DR. Content analysis: review of methods and their applications in nutrition education. J Nutr Educ Behav. 2002;34:224–30. doi: 10.1016/s1499-4046(06)60097-3. [DOI] [PubMed] [Google Scholar]
- 17.Mays N, Pope C. Assessing quality in qualitative research. BMJ. 2000;320:50–52. doi: 10.1136/bmj.320.7226.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O'Rourke M. What's Wrong With Me? The New Yorker. New York, NY: Condé Nast; 2013. pp. 32–37. [Google Scholar]
- 19.Cassell J, Buchman TG, Streat S, et al. Surgeons, intensivists, and the covenant of care: administrative models and values affecting care at the end of life--Updated. Crit Care Med. 2003;31:1551–7. [PubMed] [Google Scholar]
- 20.Schwarze ML, Bradley CT, Brasel KJ. Surgical “buy-in”: the contractual relationship between surgeons and patients that influences decisions regarding life-supporting therapy. Crit Care Med. 2010;38:843–8. doi: 10.1097/CCM.0b013e3181cc466b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bosk CL. Error Rank Responsibility. Chicago: The University of Chicago Press; 1979. pp. 36–70. [Google Scholar]
- 22.Russ AJ, Kaufman SR. Family perceptions of prognosis, silence, and the “suddenness” of death. Cult Med Psychiatry. 2005;29:103–23. doi: 10.1007/s11013-005-4625-6. [DOI] [PubMed] [Google Scholar]
- 23.Smith AK, Williams BA, Lo B. Discussing overall prognosis with the very elderly. N Engl J Med. 2011;365:2149–51. doi: 10.1056/NEJMp1109990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lamont EB, Christakis NA. Prognostic disclosure to patients with cancer near the end of life. Ann Intern Med. 2001;134:1096–105. doi: 10.7326/0003-4819-134-12-200106190-00009. [DOI] [PubMed] [Google Scholar]
- 25.Tversky A, Kahneman D. Judgment under Uncertainty: Heuristics and Biases. Science. 1974;185:1124–31. doi: 10.1126/science.185.4157.1124. [DOI] [PubMed] [Google Scholar]
- 26.Kahneman D. Thinking Fast and Slow. New York, NY: Farrar, Straus and Giroux; 2011. [Google Scholar]
- 27.Blinderman CD, Krakauer EL, Solomon ML. Time to Revise the Approach to Determining Cardiopulmonary Resuscitation Status. JAMA. 2012;307:917–918. doi: 10.1001/jama.2012.236. [DOI] [PubMed] [Google Scholar]
- 28.Winter L, Parker B. Current health and preferences for life-prolonging treatments: an application of prospect theory to end-of-life decision making. Soc Sci Med. 2007;65:1695–707. doi: 10.1016/j.socscimed.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 29.Boyd EA, Lo B, Evans LR, et al. “It's not just what the doctor tells me:” factors that influence surrogate decision-makers' perceptions of prognosis. Crit Care Med. 2010;38:1270–5. doi: 10.1097/CCM.0b013e3181d8a217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barnato AE, Herndon MB, Anthony DL, et al. Are regional variations in end-of-life care intensity explained by patient preferences?: A Study of the US Medicare Population. Med Care. 2007;45:386–93. doi: 10.1097/01.mlr.0000255248.79308.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.