Abstract
Personality disorders (PDs) are often described as stable, which ignores the important dynamic processes and shifts that are observed clinically in individuals with PD. The current study examined patterns of variability in problematic interpersonal functioning, a core feature of personality pathology. Participants (N=150) were assessed for personality pathology at baseline and also completed the Inventory of Interpersonal Problems–Circumplex Scales at baseline and every three months over the course of a year. Baseline PD was used to predict individual means and variability parameters in generalized interpersonal distress, agentic problems, and communal problems across repeated assessments. Disorders associated with disinhibition predicted variability in generalized distress and agentic problems, whereas only antagonism related disorders predicted variability in communal problems. These associations reveal dynamic processes involved in multiple dimensions of personality pathology and suggest that future research on instability is needed that expands beyond the historical focus on borderline PD.
Keywords: Interpersonal Problems, Personality Disorders, Interpersonal Instability, Dynamic Processes
The Diagnostic and Statistical Manual of Mental Disorders (DSM) conceptualizes personality disorders (PDs) as “personality traits [that] are inflexible and maladaptive” (p. 647; American Psychiatric Association, 2013). This formulation emphasizes a view of personality and its pathology as being largely static and unresponsive to the environment and shifts in the internal states of the individual. Two of the general criteria of PD (Criterion B – pattern is inflexible and pervasive across a broad range of personal and social situations; Criterion D – pattern is stable and of long duration) elaborate and reinforce this position. However, accumulating research suggests that a comprehensive understanding of personality (Fleeson, 2001; Fleeson & Noftle, 2008; Moskowitz & Zuroff, 2004, 2005) and PD must accommodate dynamic processes, shifts, and vacillations, in addition to consistency in maladaptive behavior (Lenzenweger, Johnson, & Willett, 2004; Russell et al., 2007; Trull et al., 2008). Recently we found that borderline personality pathology predicted instability in style of interpersonal problems over the course of a year (Wright, Hallquist, Beeney, & Pilkonis, 2013). These findings motivate further investigations that will (a) examine whether additional PD diagnoses predict interpersonal problem instability, and (b) given that the DSM PDs reflect heterogeneous constructs, examine the underlying dimensions of these disorders as predictors of instability.
Evolving Conceptions on Stability of Personality and its Pathology
Inherent in the definition of personality is an assumption of consistency in attributes and behavior, from which it follows that PDs are characteristically stabile in their dysfunction. However, basic personality science now recognizes that although personality is highly stable in many respects, it is also characterized by dynamic processes that play out across various time-scales, ranging from momentary fluctuation in specific behaviors (e.g., Fleeson, 2001; Fleeson & Noftle, 2008; Larsen, 1987; Moskowitz & Zuroff, 2004, 2005) to maturational trends that span years to decades (Roberts, Walton, & Viechtbauer, 2006). Moreover, although stability is observed in the aggregate (i.e., high mean and rank-order stability coefficients) individuals differ considerable in the degree and pattern of change over time (Donnellan et al., 2007; Mroczek & Spiro, 2003; Wright, Pincus, & Lenzenweger, 2011; 2012), motivating searches for the determinants of instability and change (e.g., Donnellan et al., 2007; Roberts et al., 2003).
Converging lines of evidence from prospective multi-year longitudinal studies and those employing momentary assessments paint a similar picture of PDs as comprised of dynamic processes that unfold from moments (Coifman et al., 2012; Russell et al., 2007; Sadikaj et al., 2010, 2013; Trull et al., 2008) to years (Grilo et al., 2004; Johnson et al., 2000; Lenzenweger, 1999; Morey & Hopwood, 2013; Zanarini et al., 2012). Although these findings contrast with traditional conceptions of PD as chronic and stable, research has also shown that certain features, namely psychosocial impairments, are enduring even as other features wax and wane (Gunderson et al., 2011; Skodol et al., 2005; Zanarini et al., 2010). Taken together, this suggests that PD is an amalgam of relatively more stable and more dynamic features, with an emerging focus on dynamic processes in PD that play out across a wide range of temporal resolutions. However, there is a need for better understanding those aspects of PD that are consistent and those that vary over time, and what predicts variability in functioning over time. This is because different levels of (in)stability imply differences in psychology processes. For instance, erratic functioning over time might be reflective of shifting self-states, emotional reactivity, or a general impairment in self-regulation. In contrast, behavioral consistency might suggest a maintenance process that preserves the individual’s pattern of functioning across time. Determining the diagnostic features associated with instability in certain domains may yield initial insights into the mechanisms by which PD is expressed and maintained.
Characterizing Change, Variability, and Instability
Any study of processes relies on quantifying stability, change, or variability over time in some system. Articulations of variability differ in their calculation, meaning, and by extension implications in the study of dynamic processes. Depending on the specific research question, one may be interested in structured change over time in the form of parameterized (e.g., linear) trajectories or alternatively unstructured variability or instability in the form of temporal shifts that do not follow any specified pattern. In contemporary research, structured change is most often calculated using growth curve models that provide estimates of a sample’s mean trajectory and variability in individual trajectories of the same shape around the mean. This is a useful technique when studying orderly change that follows a specific pattern, and as such is frequently employed in developmental research to capture gradual maturational change.
However, not all processes can be hypothesized to follow gradual patterned change, and instead what are of interest are irregular shifts in functioning and returns. When considered over time, irregular vacillations have been referred to as instability (e.g., Ebner-Priemer et al., 2007; Trull et al., 2008), and can be quantified in terms of the total (or average) amount of change between successive (i.e., consecutive) time-points (see e.g., Larsen, 1987 or Jahng et al., 2009 for a detailed discussion of these issues). Importantly, instability is distinguishable conceptually and quantitatively from structured change trajectories. Symptomatic exacerbations and resolutions in response to life stressors are examples of the types of shifts that may be appear as stark deviations from a gradual trajectory, and knowing the predictors of these types of shifts are likely to be of value to practitioners.
Predictors of Instability
Studies on instability of behavior and functioning in PD have thus far understandably concentrated on borderline personality disorder (BPD), which is explicitly defined in terms of instability in a variety of domains (e.g., affect, relationships, impulsivity; American Psychiatric Association, 2013), (see Santangelo, Bohus, & Ebner-Primer, in press or Wright, 2011 for reviews). Notable findings include documented differences between individuals with BPD and community controls in variability of interpersonal behavior in momentary interactions (Russell et al., 2007), and differences between individuals with BPD and those with depression in affective variability (Trull et al., 2008). Initial investigations on gross instability have provided the foundation for subsequent work that has elucidated nuanced processes by examining more complex sequences of behavior within individuals with BPD (e.g., Coifman et al., 2012; Sadikaj et al., 2010, 2013).
However, contemporary clinical theories of personality pathology generally posit that all forms of PD are interactive phenomena, with the individual acting in context (Hill, Pilkonis, & Bear, 2011; Kernberg, 1984; Linehan, 1993; Pincus et al., 2010). Pathology emerges in the dynamic interplay of the person interacting with his or her environment, often responding with maladaptive behaviors as they seek to regulate in the face of (real or perceived) adversity. This may manifest in ebbs and flows of patient functioning in treatment, contrasting periods of greater integration and health, followed by dysregulation and symptomatic flare-ups, and back again.
More importantly, an exclusive focus on any single diagnostic category caries with it all the known issues with DSM diagnoses (Krueger & Eaton, 2010). These include high rates of disorder covariation (i.e., comorbidity; Lilienfeld et al., 1994) and within disorder heterogeneity (Clarkin et al., 1983; Hallquist & Pilkonis, 2012; Lenzenweger et al., 2008; Samuel & Widiger, 2008; Widiger & Sanderson, 1995; Wright et al., 2013). Indeed, the serious limitations of the DSM PD model have prompted a shift towards focusing on fundamental domains of functioning that cut across traditional diagnostic categories (Livesley et al., 1998). This perspective has emerged in the novel DSM-5 Section III model of PD (American Psychiatric Association, 2013; Krueger et al., 2011) and is represented in the National Institute of Mental Health’s Research Domain Criteria (RDoC) initiative (Cuthbert & Kozak, 2013; Sanislow et al., 2010). By focusing on transdiagnostic dimensions that are more closely aligned with basic psychological domains, neurobiological circuits, and behavioral pathways, challenges with the extant system can be resolved, and the actual features involved in the expression of a given phenomenon can be clarified. A further implication is that PD constructs should be treated as dimensional, especially given the lack of empirical support for current diagnostic thresholds (Balsis et al., 2011; Trull & Durrett, 2005). Therefore, although we previously examined BPD as a predictor of shifts in interpersonal problem severity and style over the course of a year, whether these predictions generalize to other PD constructs and/or whether dimensions that cut across diagnoses can clarify the domains that are predictive of instability remains an open question.
The Current Study
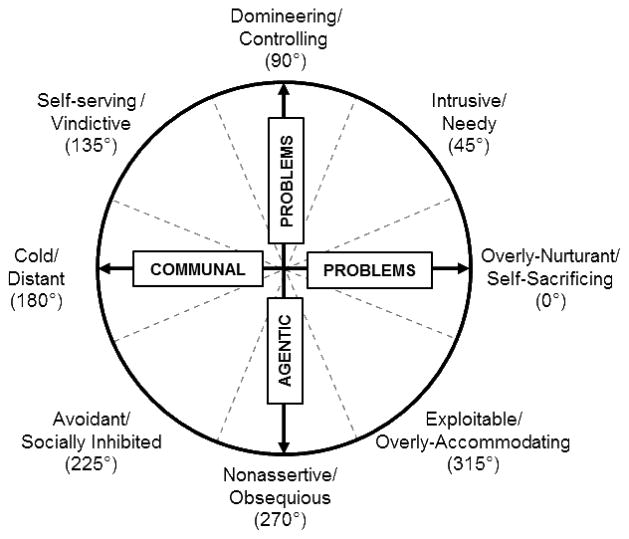
The purpose of the current study is to examine which features of PD are predictive of shifts or variability in interpersonal problem severity and style. Our focus is on interpersonal problems, given that impaired social and interpersonal functioning represents one of, if not the central, impairment in PD (Benjamin, 1996; Hopwood et al., 2013; Luyten & Blatt, 2013; Meyer & Pilkonis, 2005; Pincus, 2005). We use the interpersonal circumplex (IPC; Figure 1) as a comprehensive conceptual and quantitative model for organizing interpersonal functioning. Specifically, we use the Inventory of Interpersonal Problems–Circumplex Scales (IIP-C; Alden, Wiggins, & Pincus, 1990), which is comprised of behavioral excesses and inhibitions characteristic of many forms of personality pathology (Pincus & Wiggins, 1990). A further attractive feature of the IIP-C is that it differentiates between severity (generalized interpersonal distress) and style (agentic and communal problem dimensions) in the manifestation of interpersonal problems (Tracey, Rounds, & Gurtman, 1996).
Figure 1.
The Inventory of Interpersonal Problems – Circumplex Scales
We evaluated interpersonal problem instability on a time scale that is clinically informative by assessing participants at five points over a year (i.e., baseline and every three months) to mimic typical assessment periods of PD treatment studies (Clarkin et al., 2007; Leichsenring & Leibing, 2003; Linehan et al., 2006). As mentioned above, in a previous study with this sample, we established that BPD is a predictor of instability in agentic and communal problems but not generalized distress (Wright et al., 2013). Here we examined whether the other nine DSM PDs predicted similar or distinct patterns of variability in the interpersonal domains. Subsequently we evaluated whether broad crosscutting domains of personality pathology—antagonism, detachment, disinhibition, and negative affectivity (i.e., the pathological “Big-4”; Widiger & Simonsen, 2005)—explain and clarify patterns of interpersonal problem instability.
Although our aims are exploratory to some extent, given that prior research has almost exclusively focused on variability in functioning as a property of BPD, we hypothesized that other disorders that share features with BPD would also predict shifts in interpersonal problems over time. Specifically, we predicted that paranoid, antisocial, histrionic, and narcissistic PDs, all disorders with significant antagonism components (Hopwood et al., 2012; Kotov et al., 2011), would also exhibit unstable patterns in interpersonal style. Antagonistic behavior, at least as it manifests itself in anger and aggression, can be difficult to maintain over the long-term. Remaining actively at odds with others is rarely sustainable. Therefore, we predicted that antagonism and PDs with antagonistic features would lead to shifts in interpersonal problems reflective of the “ins and outs” of relationships over time. Additionally, we anticipated that antisocial PD symptoms, which are most strongly associated with the externalizing spectrum or disinhibition domain (Kotov et al., 2011), might also be associated with instability over time. Similar to antagonism, disinhibition can place one at odds with other forces in the environment, either through a large faux pas that results in serious consequences or a consistent pattern of irresponsibility that meets intolerance and a reaction from others. These consequences often result in a shift in behavior. Additionally, disinhibition can also lead to impulsivity and rash behavior prompted by affective dysregulation (Whiteside & Lynam, 2001). Thus, we predicted that disinhibition would be related to interpersonal instability. Finally, we anticipated that negative affectivity would predict interpersonal instability, given the centrality of emotional lability to this domain. In contrast to these hypotheses, we expected detachment, and associated PDs such as schizoid and avoidant, would be negatively related to instability.
Method
Participants and Recruitment
The sample consisted of 150 participants (M age = 44.9, SD = 10.4, Range = 22 to 61 years old; 65% female), recruited from general outpatient psychiatric clinics (n=75) and the community (n = 75). The recruitment procedures for the current study sample have been described in detail elsewhere (Scott et al., 2013). Briefly, the recruitment criteria were designed to sample the full range of BPD severity (i.e., 0–9 criteria). Participants identified primarily as white (57%) or African American (38%). Thirteen participants (9%) had not completed high school, 28 (19%) were high school graduates, 63 (42%) had some college or vocational training, 28 (19%) had completed a four-year college degree, and 18 (12%) had attended graduate or professional school. Sixty-five participants (43%) were employed, and 46 (31%) reported an annual household income of less than $10,000. The University of Pittsburgh Institutional Review Board approved all study procedures.
Assessment Procedures
At the initial assessment meeting, study clinicians described the study in detail and obtained written, informed consent. Participants completed a battery of self-report questionnaires and clinical interviews at intake, and then completed selected self-report questionnaires at three-month follow-up intervals over the course of the year (i.e., five assessment points). Interviewers were trained clinicians who had a master’s or doctoral degree and at least five years of experience. Clinical interviewers were blind to participants’ initial screening responses regarding BPD features. At the conclusion of each participant’s interviews, a consensus diagnostic case conference was conducted by a research team comprised of at least three judges. At the case conferences, interviewers presented all historical and concurrent information collected during the intake process. Consensus-rated diagnostic measures were completed in the case conference sessions. A complete description of the consensus rating process used in this research program has been provided in previous reports (Pilkonis et al., 1995; Scott et al., 2013). In the current sample, 63.3% of participants met the criteria for a diagnosis of one or more clinical syndromes; of these diagnoses, the majority were mood (73.7%), anxiety (49.5%), and substance-related (31.6%) disorders. A majority (56.7%) of the sample met the criteria for a diagnosis of one or more personality disorders, of which BPD (30.6%) and PD not otherwise specified (30.6%) were the most common. Table 1 includes a summary of the rates of PD diagnoses in the sample.
Table 1.
Descriptive statistics of sample PD features
| Disorder | Dimensional Scores
|
Diagnosis Level
|
|||||
|---|---|---|---|---|---|---|---|
| Min | Max | M | SD | Na | % of Totala | % of PD Diagnoses | |
| Paranoid | 0 | 9 | 0.95 | 1.6 | 5 | 3.3 | 5.9 |
| Schizoid | 0 | 8 | 0.55 | 1.39 | 3 | 2.0 | 3.5 |
| Schizotypal | 0 | 12 | 0.41 | 1.4 | 2 | 1.3 | 2.4 |
| Antisocial | 0 | 10 | 1.39 | 2.36 | 9 | 6.0 | 10.6 |
| Borderline | 0 | 12 | 2.62 | 3.3 | 26 | 17.3 | 30.6 |
| Histrionic | 0 | 10 | 0.99 | 1.69 | 4 | 2.7 | 4.7 |
| Narcissistic | 0 | 10 | 1.41 | 2.06 | 4 | 2.7 | 4.7 |
| Avoidant | 0 | 14 | 1.54 | 2.58 | 18 | 12.0 | 21.2 |
| Dependent | 0 | 8 | 0.71 | 1.19 | 1 | 0.7 | 1.2 |
| Obsessive-Compulsive | 0 | 10 | 1.45 | 2.03 | 8 | 5.3 | 9.4 |
| PD-NOS | -- | -- | -- | -- | 25 | 16.7 | 29.4 |
| No Diagnosis | -- | -- | -- | -- | 65 | 43.3 | -- |
Note. N=150. PD = Personality Disorder; PD-NOS = PD-Not Otherwise Specified.
Columns sum > 150 and > 100% due to PD comorbidity.
Measures
PD Symptoms
Clinician-rated PD symptoms were assessed at baseline using a DSM checklist that was rated by the consensus team using all available information from intake, including responses from administration of the Structured Interview for DSM-IV Personality (SIDP-IV; Pfohl, Blum, & Zimmerman, 1997). The individual DSM-IV diagnostic criteria were rated on a 0–2 scale (0 = absent, 1 = present, 2 = strongly present). The clinician-rated dimensional scores were calculated by summing these scores. A randomly selected subsample (n = 15) of SIDP-IV interviews were videotaped and rated by four clinical judges for calculation of interrater reliability. ICC’s were calculated based on one-way random effect models, and demonstrated adequate inter-diagnostician agreement for PD dimensional scores (Mdn ICC = .78; Range = .61 for histrionic to .89 for dependent). Table 1 contains descriptive statistics of the PD dimensional scores.
Interpersonal Problems
Interpersonal problems were measured using the Inventory of Interpersonal Problems – Circumplex Scales (IIP-C; Horowitz et al., 2000). The IIP-C is a 64-item self-report measure of interpersonal problems. Items assess behaviors that an individual does in excess (i.e., “I…too much”) or finds difficult to do (“It is hard for me to…”). The IIP-C contains eight, 8-item scales (i.e., octant scales; see Figure 1) whose internal consistencies across all assessment points ranged from .77 to .91 (Mdn = .84). Scores from the octant scales were combined using circumplex weighting procedures to derive scores for the primary dimensions of Agentic Problems and Communal Problems. The IIP-C’s dimensional scores were created from standardized octant scores using the normative sample from Horowitz et al. (2000) to facilitate interpretation. Importantly, each domain is bipolar, such that agentic problems range from being forceful and controlling to being overly submissive and servile, whereas communal problems range from being cold and withdrawn to overly nurturing and smothering. As such, both high and low scores are indicative of interpersonal problems, and significant positive and negative correlations both signify higher levels of pathology. In addition, generalized distress (i.e., severity) was computed as the average octant scale score in our analyses (Tracey et al., 1996). The dimensional scores for agentic and communal problems provide measures of problems in each domain, net of general severity.
Analyses
First, we calculated one-year individual means (iMs) and instability scores for the interpersonal problem domains of generalized distress, agentic, and communal problems. The interpersonal problem domain iMs were the average of an individual’s scores across the five assessment points. Instability was operationalized as an individual’s mean square of successive differences (iMSSD; Ebner-Priemer et al., 2009; von Neumann et al., 1941) in interpersonal problem scores across the five assessment points. The iMSSD accounts for temporal sequencing of assessments and “de-trends” the data such that the score is net of orderly change in the data and reflects the average shifts between consecutive time-points (Ebner-Priemer et al., 2009). Thus, high scores reflect irregular and erratic shifts from one assessment to the next, whereas low scores reflect a more orderly or gradual trajectory across time. Following this, we regressed iMs and iMSSDs on the 10 DSM PD dimensional scores in univariate regression models. Subsequently, to refine our understanding of the mechanisms driving average levels of interpersonal problems and their instability, we conducted an exploratory factor analysis (EFA) to establish the major transdiagnostic dimensions present in our data, which were used to predict iMs and instability in an exploratory structure equation modeling (ESEM) framework. ESEM is an attractive solution for investigating structural relations among constructs when data complexity is high (e.g., when non-ignorable cross-loadings exist in the hypothesized structural model), while retaining the benefits of a latent variable modeling framework (e.g., accounting for measurement error). ESEM combines EFA solutions for latent variables with the ability to model structural paths (i.e., regression paths) among predictors and outcomes. Here we employ this technique in order to model EFA based PD dimensions that can be used as predictors of interpersonal problem iMs and iMSSDs. Within this model iMs and iMSSDs for generalized distress, agentic, and communal problems were regressed on each of the transdiagnostic personality pathology dimensions simultaneously in multivariate models.1
Results
Attrition over the course of the study was minimal, with 139 participants (93%) completing all five assessments, with a total of 736 assessments (98%) completed out of a possible 750. The impact of missing data was negligible, so we used all available data in analyses.
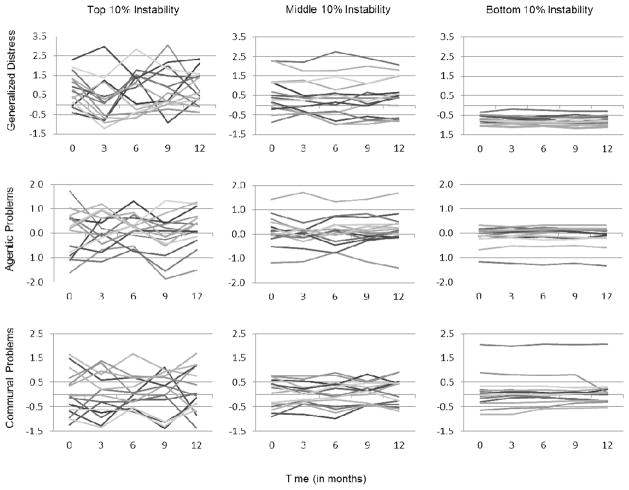
Predicting Year-Long Individual Means and Instability from DSM PD Diagnoses
Descriptive statistics for iMs and iMSSDs can be found in Table 2. To further illustrate the type of instability that is being modeled here, Figure 2 presents the upper, middle, and lower 10% of participants based on their iMSSDs. Note the wide range of instability present in the sample, with those participants in the upper range exhibiting widely varying scores over time. Results of univariate and multiple regression analyses predicting iMs and iMSSDs from baseline PD dimensional scores can be found in Table 3. With the exception of obsessive-compulsive and schizotypal, all PDs significantly predicted the generalized distress when entered as univariate predictors iM. In multiple regression models, only borderline and avoidant symptoms predicted generalized distress. Baseline histrionic and antisocial symptoms predicted higher average dominance related problems (i.e., problems with high agency), whereas baseline avoidant and dependent symptoms were predictive of relatively higher submissiveness related problems (i.e., problems with lower agency) in univariate models. When all PD dimensions were entered as predictors, only antisocial features were predictive of domineering problems and avoidant were predictive of submissiveness problems. When entered as single predictors, histrionic symptoms were the only significant predictor of higher communal problem iMs, but problems with low communion were predicted by schizoid, antisocial, and avoidant PD symptoms. In multivariate models only antisocial dimension predicted problems with low communion.
Table 2.
Descriptive Statistics for Coefficients of Year-Long Means and Individual Instability
| Coefficient | Individual Means (iMs)
|
Individual Instabilities (iMSSDs)
|
||||||
|---|---|---|---|---|---|---|---|---|
| Min | Max | M | SD | Min | Max | M | SD | |
| Generalized Distress | −1.11 | 2.49 | 0.37 | 0.89 | 0.00 | 3.06 | 0.27 | 0.44 |
| Agentic Problems | −1.55 | 1.52 | −0.08 | 0.55 | 0.00 | 0.77 | 0.13 | 0.15 |
| Communal Problems | −1.74 | 2.04 | 0.03 | 0.49 | 0.00 | 1.79 | 0.13 | 0.20 |
Note. N = 150. Mean coefficients reflect average of five assessment points, Instabilities reflect iMSSD scores from all five assessment points.
Figure 2.
Plot of generalized distress, agentic problems, and communal problems scores for the upper, middle, and lower 10% of instability scores in each domain.
Table 3.
Standardized regression coefficients for individual PD dimensions predicting interpersonal problem domain longitudinal means and instabilities
| PD Symptoms | Longitudinal Means
|
Instability
|
||||
|---|---|---|---|---|---|---|
| Generalized Distress | Agentic Problems | Communal Problems | Generalized Distress | Agentic Problems | Communal Problems | |
| Univariate Models | ||||||
| Paranoid | .31*** | .10 | −.14 | .09 | .08 | .26** |
| Schizoid | .17* | −.15 | −.25** | −.02 | .04 | −.02 |
| Schizotypal | .16 | −.11 | −.14 | −.10 | .08 | −.06 |
| Histrionic | .17* | .19* | .19* | .06 | .04 | .26** |
| Narcissistic | .21* | .16 | −.03 | .04 | −.06 | .00 |
| Antisocial | .20* | .31*** | −.21** | .42*** | .29*** | .09 |
| Borderline | .57*** | .10 | .04 | .11 | .28*** | .30*** |
| Avoidant | .49*** | −.42*** | −.18* | −.02 | .04 | .02 |
| Dependent | .32*** | −.18* | .06 | .01 | .10 | .06 |
| Obsessive-Compulsive | .07 | −.01 | −.15 | −.10 | −.06 | .08 |
| Multivariate Models | ||||||
| Paranoid | .08 | .11 | −.10 | .09 | .03 | .24** |
| Schizoid | .10 | .01 | −.14 | .05 | .03 | .05 |
| Schizotypal | −.04 | −.04 | .01 | −.14 | .09 | −.16† |
| Histrionic | −.03 | .07 | .18† | .07 | −.08 | .20* |
| Narcissistic | .07 | .06 | −.00 | −.04 | −.15 | −.19* |
| Antisocial | .00 | .28** | −.33*** | .47*** | .20* | −.05 |
| Borderline | .48*** | .01 | .12 | −.27* | .23* | .27* |
| Avoidant | .34*** | −.42*** | −.12 | −.07 | −.05 | −.02 |
| Dependent | .01 | −.05 | .03 | .07 | .06 | −.08 |
| Obsessive-Compulsive | .02 | .09 | −.16† | −.04 | .00 | .10 |
Note. N = 150. PD = Personality disorder. Univariate model coefficients for borderline PD were previously presented in Wright, Hallquist, Beeney, & Pilkonis, 2013.
p < .10,
p < .05,
p < .01,
p < .001
Relatively fewer PD dimensional scores were predictive of iMSSDs when entered alone as predictors. Instability in generalized distress was uniquely predicted by antisocial symptoms, agentic problem instability was predicted antisocial and borderline symptoms, and communal problem instability was predicted by paranoid, histrionic, and borderline symptoms. To ensure the robustness of these results we reran all analyses controlling for all other disorders and found that the pattern and magnitude of significant coefficients was highly stable.2 However, two additional interesting effects emerged. Notably, when controlling for all PD dimensions, borderline now negatively predicted generalized distress instability, and narcissistic PD negatively predicted instability in communal problems. In other words, each of these effects was evidence of greater stability in distress and communal problems for borderline and narcissistic, respectively.
Refining the Prediction of Individual Means and Instability
To refine the variables used as predictors of interpersonal problem iMs and iMSSDs, we conducted an EFA to uncover the transdiagnostic dimensions in our data. We ran a series of oblique Geomin rotated EFAs in Mplus 7.11 (Muthén & Muthén, 2012) with the 10 DSM PD dimensional scores as observed variables. Consistent with our expectations, the four-factor model provided excellent fit to the data (χ211 = 14.08, p = .23; RMSEA = .043, p = .52; CFI = .99, SRMR = .02) and including a fifth factor provided a non-significant increase in model fit (Δχ26 = 11.61, p = .07). Factor loadings of the final model can be found in Table 4 and bear an easily interpretable “pathological big-four” pattern (Widiger & Simonsen, 2005). We labeled the first factor Detachment, based on high loadings from schizoid, schizotypal, avoidant, and a negative loading from histrionic symptoms. This was followed by disinhibition, which had antisocial, borderline, and obsessive-compulsive (negatively) as its strongest markers. Next, antagonism had strong loadings from narcissistic, histrionic, paranoid, and obsessive-compulsive symptoms. Finally, negative affectivity was marked most strongly by dependent, avoidant, and borderline PDs. We did not find evidence for a fifth domain related to oddity, peculiarity, or psychoticism, as is frequently, but not always, articulated as part of the higher-order structure of pathological personality domains (Watson, Clark, & Chmielewski, 2008; Widiger & Simonsen, 2005; Wright & Simms, 2014). This is in part because schizotypal PD is the only marker of this domain, and therefore it is unlikely to emerge as a unitary dimension, and, more specific to this sample, rates of relevant symptomatology were relatively low.
Table 4.
Factor loadings from oblique geomin rotated factor model
| PD Symptoms | Detachment | Disinhibition | Antagonism | Negative Emotionality |
|---|---|---|---|---|
| Paranoid | .11 | .14 | .42 | −.03 |
| Schizoid | .77 | −.01 | .00 | .01 |
| Schizotypal | .55 | −.01 | .27 | −.01 |
| Histrionic | −.31 | .18 | .47 | .07 |
| Narcissistic | −.18 | .00 | .60 | −.09 |
| Antisocial | .02 | .62 | −.12 | −.04 |
| Borderline | .01 | .76 | .06 | .38 |
| Avoidant | .50 | .04 | .01 | .46 |
| Dependent | −.03 | −.04 | −.03 | .89 |
| Obsessive-Compulsive | .08 | −.42 | .56 | .03 |
Note. N = 150. PD = Personality disorder. Factor loadings > |.30| bolded.
We next used this factor solution as the basis for a target rotated ESEM, with the iMs and iMSSDs for the interpersonal problem domains regressed simultaneously on all four personality pathology dimensions. Separate models were run for the iMs and iMSSDs.3 Both the iM (χ2(29) = 43.11, p = .04; RMSEA = .057, p = .35; CFI = .97, SRMR = .03) and iMSSD (χ2(29) = 54.91, p = .003; RMSEA = .077, p = .08; CFI = .92, SRMR = .04) models achieved satisfactory fit to the data. Multivariate models were run to account for the fact that within individuals, these four dimensions of personality pathology are not orthogonal, but rather vary in configuration across persons. Table 5 catalogues the regression pathways from each of the ESEM analyses. We found that one-year averages in generalized interpersonal distress were most strongly predicted most strongly by negative affectivity, followed by detachment and disinhibition, whereas antagonism was not a significant predictor. All personality pathology domains were predictive of Agentic problems, but in opposing ways: detachment and negative affectivity were associated with more submissive problems, whereas disinhibition and antagonism were associated with higher average levels of domineering problems. Detachment and disinhibition were associated with problems of low communion. Instability in general distress and agentic problems was uniquely associated with disinhibition, although communal problem instability was predicted by antagonism. To ensure that these results were robust to initial values, we reran models for each iMSSD individually controlling for the corresponding iM. In each case the pattern of results and magnitude of coefficients remained the same.
Table 5.
Multivariate regression coefficients from exploratory structural equation model
| Longitudinal Means
|
Instability
|
|||||
|---|---|---|---|---|---|---|
| Generalized Distress | Agentic Problems | Communal Problems | Generalized Distress | Agentic Problems | Communal Problems | |
|
| ||||||
| Detachment | .36 (.09) | −.41 (.12) | −.47 (.11) | .04 (.10) | .12 (.11) | −.15 (.11) |
| Disinhibition | .33 (.11) | .30 (.10) | −.31 (.12) | .47 (.09) | .34 (.11) | .04 (.10) |
| Antagonism | .10 (.10) | .28 (.12) | .03 (.14) | −.13 (.12) | −.06 (.06) | .29 (.12) |
| Negative Emotionality | .59 (.09) | −.45 (.12) | .14 (.13) | −.02 (.10) | .16 (.10) | .13 (.12) |
Note. N=150. All regression coefficients presented in standardized values. Standard errors are in parentheses. Bolded values significant at p < .05.
Discussion
The motivating factor for this study was the observation that there are rich individual differences in the stability of behavior over time, and these have been shown to relate to BPD (Russell et al., 2007; Trull et al., 2008; Wright et al., 2013), but research linking behavioral instability and other PD (i.e., non-BPD) features is lacking. In an effort to begin to address this research gap, we calculated individual means and instability coefficients for three complementary aspects of problematic interpersonal functioning (generalized interpersonal distress, agentic problems, and communal problems) over the course of one year, and prospectively predicted these values from personality pathology at baseline. Broadly we found that individual PD dimensions and factor analytically derived transdiagnostic PD dimensions (a) predicted individual means in ways that were highly consistent with a large body of cross-sectional research (Horowitz, 2004), and (b) were more selectively predictive of instability.
Disorders known to exhibit higher levels of distress (i.e., borderline, avoidant, dependent, paranoid) demonstrated moderate to strong associations with mean levels of generalized interpersonal distress over the course of the year, whereas antisocial, narcissistic, histrionic, and schizoid PD symptoms were only associated with modest rates of mean interpersonal distress, also consistent with their conceptualization. Only schizotypal and obsessive-compulsive symptoms were unrelated to generalized distress. When controlling for all PDs BPD and avoidant symptoms accounted for all of these associations. Associations with stylistic interpersonal elements were generally more modest, but were consistent with prior cross-sectional research (e.g., antisocial PD is associated with hostile dominant interpersonal behavior; Pincus & Wiggins, 1990).
When considering the associations between individual PD dimensional scores and instability coefficients, we found that antisocial, borderline, paranoid, and histrionic all were predictive of some form of instability. We have previously reported that borderline pathology is associated with instability in agentic and communal domains of interpersonal style (Wright et al., 2013). In our prior study we discussed how these results clarify the oft-noted lack of association between BPD and specific interpersonal style (e.g., Salzer et al., 2013; Wright et al., 2013). Of note is that BPD features are predictive of greater stability in distress when accounting for the remaining PD features, consistent with the construct’s definition.
The current analyses show that paranoid and histrionic PD symptoms are also predictive of instability in communal problems, whereas antisocial PD symptoms are predictive of instability in agentic interpersonal problems. Instability in generalized distress is uniquely associated with antisocial symptoms. It could be argued that those disorders that share instability in communal problems also each share a difficulty with appropriately negotiating closeness in relationships. To be sure, dependent and schizoid PDs are also associated with difficulties in managing closeness in relationships. One possibility is that dependent and schizoid pathology are associated with consistent patterns of difficulties (i.e., over- and under-involvement, respectively), whereas the difficulties in paranoid, histrionic, and borderline pathology are better characterized by fits and starts or lurches towards and away from closeness. Much has been written about this aspect of BPD (Benjamin, 1996; Gunderson, 2001; Linehan, 1993), but less so as it plays out in the other two diagnoses (cf. Horowitz, 1991).
The results of individual disorders need to be considered in the context of mean endorsement of problems. For instance, histrionic PD is associated with higher average agentic-communal problems, such that vacillation on the communal dimension would suggest difficulties of going in and out of intrusiveness. Alternatively, paranoid PD is associated with average problems of low communion, and thus variability likely reflects shifts between neutrality and withdrawal. Within individuals both the average level of behavior and vacillation around this mean flesh out the picture of the person as they progress through time. Thus, a fully appreciation of the implication of these results requires the consideration of the “set-point” in which the variability occurs.
The fact that antisocial PD exhibited such a strong relationship with generalized distress instability was unanticipated. Therefore our interpretation of this result is necessarily post-hoc to some degree. Nonetheless this finding, coupled with the fact that at the zero-order level antisocial PD exhibited only modest correlations with average distress, and was completely unassociated when controlling for other PDs, suggests interesting possibilities for the patterning of interpersonal distress in individuals high in antisocial symptoms. Interpreted in the context of little to no association with average distress, instability may be reflective of a pattern of markedly low distress and concern that is relatively stable, punctuated by performing impulsive and antagonistic acts (e.g., infractions, hostility, etc.), that evokes briefer periods of elevated distress when there are natural consequences (e.g., legal troubles, negative social feedback) or when one’s goals are blocked, which are more variable as outcomes. Alternatively it may be that individuals high in antisocial PD are quite different from each other in their average level, and some spend considerable time in low distress, with occasional spikes when faced with environmental challenges, whereas others are high in distress, consistently riding a wave of ups and downs in as a consequence of their impulsive actions. Indeed, these results are consistent with prior meta-analytic findings that show little to know association between antisocial symptoms with distress related traits on average (e.g., certain facets of Neuroticism; Samuel & Widiger, 2008), but also argue for future research that investigates dynamic processes in negative affectivity and interpersonal distress among those high in antisocial PD. Studying variability over time in this way may serve to clarify otherwise unanticipated associations in the study of PD.
We have emphasized the search for predictors of instability, but the other side of this coin would be predictors of stability or rigidity in functioning. Rigidity even plays a prominent role in the description of some PD constructs, for instance obsessive-compulsive PD has this as a formal criterion. We did find some evidence for stability in the aforementioned negative association between BPD features and distress instability. Additionally, narcissistic features were significant negative predictors of communal problem instability when controlling for other PD features, and schizotypal PD features approached significance as a negative predictor as well. The lack of significant findings with obsessive-compulsive features may reflect that the rigidity is more specific to other domains (e.g., cognitive) or plays out on a different time-scale (e.g., momentary disagreements that arise from adhere to one’s specific views).
With respect to the second set of results, we found that a four-factor model captured the pattern of covariation among the individual disorder constructs and represented dimensions we labeled Detachment, Disinhibition, Antagonism, and Negative Emotionality. The model that emerged not only excellently fit the data, but also was made up of three factors (Detachment, Disinhibition, and Negative Emotionality) that were highly concordant with quantitative dimensional models of mental disorders (e.g., Kotov et al., 2011; Markon, 2010) and higher-order dimensional trait based models (e.g., Calabrese et al., 2012; Livesley et al., 1998; Wright et al., 2012; Widiger, 1998). However, the domain we have interpreted as Antagonism deviates in structure from many prior findings, especially when understood in relation to normal trait models (Saulsman & Page, 2004; Samuel & Widiger, 2008). Clear convergence can be found with prior results in the large loadings by narcissistic and paranoid PD symptoms. Yet notably absent is a significant loading from antisocial PD symptoms, and unexpected was the significant loadings from obsessive-compulsive and histrionic PD symptoms. Furthermore, the DSM-5 Section III trait model places antisocial traits within a domain clearly marked by antagonism. Although certain pervious findings might suggest that BPD should have loaded on the Antagonism factor as well (Kotov et al., 2011), just as much research would argue against specific associations with interpersonal dimensions (e.g., Pincus & Wiggins, 1990; Wright et al., 2013). Similarly, although antisocial symptoms are usually associated with the antagonism spectrum, this varies to some degree across studies (cf. Røysamb et al., 2011). Also, although somewhat controversial, the DSM-5 Section III model has placed histrionic related traits within the Antagonism domain. Thus, although we have chosen to interpret this factor as Antagonism here, it should be recognized that it deviates in certain respects from prior findings, and therefore may represent a variant that emphasizes certain aspects of the construct and not others.
In terms of predicting individual means and instability, all dimensions were associated with agentic problem means, but in divergent ways. Problems of low communion were associated with higher Detachment and Disinhibition, and generalized distress was significantly associated with all dimensions with the exception of Antagonism. The associations with instabilities clarified the results of the individual disorders, by demonstrating that Disinhibition was predictive of fluctuation in generalized distress and agentic problems, while Antagonism was predictive of vacillation in communal problems.
It is noteworthy that we have found conceptual replication for Moskowitz and Zuroff’s (2004, 2005) finding that Antagonism (i.e., low agreeableness) is predictive of interpersonal variability, even though they sampled normative range interpersonal behavior within days across several weeks, whereas we sampled problematic behavior every few months for a year. It may be that a capacity for being at odds with others is a reliable predictor of relational problems, but these are unstable. Contrastingly, we did not find that Negative Affectivity was predictive of instability, whereas Moskowitz and Zuroff found that it was a robust predictor of daily interpersonal behavior. This may be due to the fact that NEO based inventories include content related to impulsiveness within neuroticism, whereas impulsivity may be better located within a domain of Disinhibition when considering maladaptive dimensions of personality (De Fruyt et al., 2013; Wright & Simms, 2014). Accordingly, the UPPS model (Whiteside & Lynam, 2001) further clarifies the structure of the related aspects of Disinhibition and Negative Affectivity with the elaboration of a construct such as Urgency, which captures the tendency to act in reckless and impulsive manner when under distress. Therefore, what may be most predictive of certain forms of interpersonal instability may be a propensity to become disinhibited when distressed. This would be consistent with our findings here, in so far as the Disinhibition domain included as strong markers both antisocial and borderline symptoms, in addition to (negative) obsessive-compulsive symptoms. Future studies should be developed that target negative affect and impulsivity within the same sample to disentangle, in a more fine-grained fashion, the precise driver of these effects.
Indeed, our findings suggest that individual differences in instability implicate processes that play out on the order of months, yet they do not reveal the mechanisms. Research is required that will provide insight in to the driving forces involved in shifts in interpersonal functioning over time. Another consideration is that the temporal resolution at which behavior is sampled will dictate the interpretation of the instability parameters. For instance, it is possible that mechanisms driving instability in momentary interpersonal behavior may lead to similar results as those reported here, in which individuals were assessed at three-month intervals. Some of our results argue for this. Yet it would be imprudent to assume that this is the case based on the current level of evidence. More research with telescoping levels of analysis (e.g., intensively sample behavior within an interaction in a laboratory, ecological momentary assessment, daily diaries, and monthly assessments), all within the same sample, is needed to clarify the issues involved and to begin to capture the basic mechanisms of PD.
We would be remiss if we did not mention two limitations associated with this study. First, the measures of interpersonal problems relied exclusively on self-report. Although this approach is consistent with the majority of personality pathology research (Bornstein, 2003), a fuller understanding of instability would benefit from other-reported and clinician-reported interpersonal dysfunction. In particular, informants would help clarify the extent to which our results reflect changes in behavior observable to others versus shifts in self-perception. The level of consistency between self- and other-report may have implications for the conceptualization of personality pathology and clinical practice with individuals affected by it. It is notable, however, that the baseline assessments were based on clinical interviews, and the individual means and instability scores were based on self-report, and thus these results are robust to the well known attenuation of associations across informants. As such our findings reflect conservative estimates of the links between PD and interpersonal problem instability.
An additional potential limiting factor is the sampling strategy that was not random, but rather prioritized selecting individuals to cover the range of BPD criteria. This may have introduced some unforeseen bias when considering analyses using other diagnostic features as predictors. Although this cannot be ruled out, we note that the overall rates of PD diagnoses and patterns of PD are highly consistent with those observed in psychiatric populations (see Zimmerman, Chelminski, & Young, 2008). This sampling strategy may have also influenced our specific pattern of loadings on the dimensions of the structural model, leading to a disinhibition domain that was more strongly marked by BPD that might otherwise be expected, and a failure of antisocial PD to load on the antagonism domain.
In sum, we have found that there are rich individual differences in the level of interpersonal problem stability over the course of one year. Furthermore, we demonstrated that BPD is not the sole predictor of instability, suggesting that future studies should be developed explicitly to study several candidate predictors of instability. Similarly, future studies focusing on BPD should consider including measures that capture crosscutting domains in personality and its pathology. In fact, our results argue that transdiagnostic dimensions of personality pathology underlie instability in interpersonal problems. These dimensions speak to the range of DSM-defined PDs, but provide a potentially more parsimonious framework for understanding variability in interpersonal problems. The findings reported here further serve to affirm a view of PD as a dynamic and interactive process that plays out over various levels of temporal resolution from the macro- (i.e., years; Wright et al., 2011) to the micro-level (i.e., moments; Sadikaj et al., 2013), and everything in between.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health (R01MH056888, Pilkonis; F32MH097325, Wright; K01MH101289, Scott; K01MH086713, Stepp; K01MH097091, Hallquist). The opinions expressed are solely those of the authors and not necessarily those of the funding source.
Footnotes
In our previous work we found that mean levels of interpersonal problem domains were highly stable over the course of the year in this sample, and there was relatively little in the way of individual differences in trajectories around the very stable mean (Wright et al., 2013). In fact, we showed that BPD was not predictive of linear change in any of the interpersonal domains despite being predictive of instability defined as iMSSDs. Despite these prior null results, we also examined whether the remaining nine PD dimensional scores and transdiagnostic dimensions were predictive of structured change in the form of linear growth curve trajectories. However, baseline PD was virtually unrelated to individual differences in rates of linear change. Therefore we do not include an expanded treatment of these null results. Recall, that structured linear change is conceptually and quantitatively dissociable from prediction of instability in successive scores, and therefore these null results do not detract from the associations with instability we otherwise observe.
Preliminary analyses indicated that age and sex were unrelated to all outcomes except a modest correlation between sex and communal problem means (r = .20), therefore these variables were not included in further analyses.
A model combining the simultaneous prediction of all iMs and iMSSDs was attempted, but resulted in significant problems with estimation as evidenced by Heywood cases in the factor loading patterns.
References
- Alden LE, Wiggins JS, Pincus AL. Construction of circumplex scales of the Inventory of Interpersonal Problems. Journal of Personality Assessment. 1990;55:521–536. doi: 10.1080/00223891.1990.9674088. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- Balsis S, Lowmaster S, Cooper LD, Benge JF. Personality disorder diagnostic thresholds correspond to different levels of latent pathology. Journal of Personality Disorders. 2011;25:115–127. doi: 10.1521/pedi.2011.25.1.115. [DOI] [PubMed] [Google Scholar]
- Benjamin LS. An interpersonal theory of personality disorders. In: Clarkin J, Lenzenweger M, editors. Major theories of personality disorder. New York: Guilford; 1996. pp. 141–220. [Google Scholar]
- Bornstein RF. Behaviorally referenced experimentation and symptom validation: A paradigm for 21st-century personality disorder research. Journal of Personality Disorders. 2003;17:1–18. doi: 10.1521/pedi.17.1.1.24056. [DOI] [PubMed] [Google Scholar]
- Calabrese WR, Rudick MM, Simms LJ, Clark LA. Development and Validation of Big Four Personality Scales for the Schedule for Nonadaptive and Adaptive Personality—Second Edition (SNAP-2) Psychological assessment. 2012;24(3):751. doi: 10.1037/a0026915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarkin JF, Levy KN, Lenzenweger MF, Kenberg OF. Evaluating Three Treatments for Borderline Personality Disorder: A Multiwave Study. American Journal of Psychiatry. 2007;164:922–928. doi: 10.1176/ajp.2007.164.6.922. [DOI] [PubMed] [Google Scholar]
- Clarkin JF, Widiger TA, Frances A, Hurt SW, Gilmore M. Prototypic typology and the borderline personality disorder. Journal of Abnormal Psychology. 1983;92(3):263–275. doi: 10.1037//0021-843x.92.3.263. [DOI] [PubMed] [Google Scholar]
- Coifman KG, Berenson KR, Rafaeli E, Downey G. From negative to positive and back again: Polarized affective and relational experience in borderline personality disorder. Journal of Abnormal Psychology. 2012;121:668–679. doi: 10.1037/a0028502. [DOI] [PubMed] [Google Scholar]
- Cuthbert BN, Kozak MJ. Constructing constructs for psychopathology: The NIMH research domain criteria. Journal of Abnormal Psychology. 2013 doi: 10.1037/a0034028. [DOI] [PubMed] [Google Scholar]
- Donnellan MB, Conger RD, Burzette RG. Personality Development From Late Adolescence to Young Adulthood: Differential Stability, Normative Maturity, and Evidence for the Maturity-Stability Hypothesis. Journal of personality. 2007;75(2):237–264. doi: 10.1111/j.1467-6494.2007.00438.x. [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer UW, Eid M, Kleindienst N, Stabenow S, Trull TJ. Analytic strategies for understanding affective (in) stability and other dynamic processes in psychopathology. Journal of abnormal psychology. 2009;118(1):195. doi: 10.1037/a0014868. [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer UW, Kuo J, Kleindienst N, Welch SS, Reisch T, Reinhard I, Bohus M. State affective instability in borderline personality disorder assessed by ambulatory monitoring. Psychological Medicine. 2007;37(7):961–970. doi: 10.1017/S0033291706009706. [DOI] [PubMed] [Google Scholar]
- Fleeson W. Toward a structure-and process-integrated view of personality: Traits as density distributions of states. Journal of personality and social Psychology. 2001;80(6):1011. [PubMed] [Google Scholar]
- Fleeson W, Noftle EE. Where does personality have its influence? A supermatrix of consistency concepts. Journal of personality. 2008;76(6):1355–1386. doi: 10.1111/j.1467-6494.2008.00525.x. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Shea MT, Sanislow CA, Skodol AE, Gunderson JG, Stout RL, McGlashan TH. Two-year stability and change of schizotypal, borderline, avoidant and obsessive-compulsive personality disorders. Journal of Consulting and Clinical Psychology. 2004;72(5):767–775. doi: 10.1037/0022-006X.72.5.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunderson JG. Borderline personality disorder: A clinical guide. Washington, DC: American Psychiatric Press; 2001. [Google Scholar]
- Gunderson JG, Stout RL, McGlashan TH, Shea MT, Morey LC, Grilo CM, Skodol AE. Ten-year course of borderline personality disorder: psychopathology and function from the Collaborative Longitudinal Personality Disorders Study. Archives of general psychiatry. 2011;68(8):827. doi: 10.1001/archgenpsychiatry.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallquist MN, Pilkonis PA. Refining the phenotype of borderline personality disorder: Diagnostic criteria and beyond. Personality Disorders: Theory, Research, and Treatment. 2012;3:228–246. doi: 10.1037/a0027953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill J, Pilkonis PA, Bear J. Social domains, personality, and interpersonal functioning. In: Horowitz L, Strack S, editors. Handbook of interpersonal psychology: theory, research, assessment, and therapeutic interventions. New York: Wiley; 2010. pp. 281–296. [Google Scholar]
- Hopwood CJ, Morey LC, Donnellan MB, Samuel DB, Grilo CM, McGlashan TH, Skodol AE. Ten-Year Rank-Order Stability of Personality Traits and Disorders in a Clinical Sample. Journal of Personality. 2013;81(3):335–344. doi: 10.1111/j.1467-6494.2012.00801.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Thomas KM, Markon KE, Wright AGC, Krueger RF. DSM-5 personality traits and DSM-IV personality disorders. Journal of Abnormal Psychology. 2012;121(2):424–432. doi: 10.1037/a0026656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Wright AGC, Ansell EB, Pincus AL. The interpersonal core of personality pathology. Journal of Personality Disorders. 2013;27(3):271–295. doi: 10.1521/pedi.2013.27.3.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz LM. Interpersonal foundations of psychopathology. Washington, DC: American Psychological Association; 2004. [Google Scholar]
- Horowitz LM, Alden LE, Wiggins JS, Pincus AL. Manual for the inventory of interpersonal problems. United States of America: Psychological Corporation; 2000. [Google Scholar]
- Horowitz MJ. Hysterical personality style and the histrionic personality disorder. Lanham, MD, US: Jason Aronson; 1991. (rev. ed.) [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Skodol AE, Hamagami F, Brook JS. Age-related change in personality disorder trait levels between early adolescence and adulthood: a community-based longitudinal investigation. Acta Psychiatrica Scandinavica. 2000;102(4):265–275. doi: 10.1034/j.1600-0447.2000.102004265.x. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-Behavioral Treatment of Borderline Personality Disorder. Guilford Press; 1993. [Google Scholar]
- Morey LC, Hopwood CJ. Stability and Change in Personality Disorders. Annual review of clinical psychology. 2013;9:499–528. doi: 10.1146/annurev-clinpsy-050212-185637. [DOI] [PubMed] [Google Scholar]
- Moskowitz DS, Zuroff DC. Flux, pulse, and spin: Dynamic additions to the personality lexicon. Journal of Personality and Social Psychology. 2004;86:880–893. doi: 10.1037/0022-3514.86.6.880. [DOI] [PubMed] [Google Scholar]
- Moskowitz DS, Zuroff DC. Robust predictors of flux, pulse, and spin. Journal of Research in Personality. 2005;39:130–147. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén and Muthén; 2012. [Google Scholar]
- Kernberg OF. Severe Personality Disorders. New Haven, CT: Yale University Press; 1984. [Google Scholar]
- Krueger RF, Eaton NR. Personality Traits and the Classification of Mental Disorders. Personality Disorders: Theory, Research, and Treatment. 2010;1(2):97–118. doi: 10.1037/a0018990. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Eaton NR, Derringer J, Markon KE, Watson D, Skodol AE. Personality in DSM–5: Helping delineate personality disorder content and framing the metastructure. Journal of personality assessment. 2011;93(4):325–331. doi: 10.1080/00223891.2011.577478. [DOI] [PubMed] [Google Scholar]
- Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan Q, Zimmerman M. New dimensions in the quantitative classification of mental illness. Archives of general psychiatry. 2011;68(10):1003. doi: 10.1001/archgenpsychiatry.2011.107. [DOI] [PubMed] [Google Scholar]
- Larsen RJ. The stability of mood variability: A spectral analytic approach to daily mood assessments. Journal of Personality and Social psychology. 1987;52(6):1195. [Google Scholar]
- Leichsenring F, Leibing E. The effectiveness of psychodynamic therapy and cognitive behavior therapy in the treatment of personality disorders: a meta-analysis. American journal of psychiatry. 2003;160(7):1223–1232. doi: 10.1176/appi.ajp.160.7.1223. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF. Stability and change in personality disorder features: The Longitudinal Study of Personality Disorders. Archives of General Psychiatry. 1999;56(11):1009. doi: 10.1001/archpsyc.56.11.1009. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Clarkin JF, Yeomans FE, Kernberg OF, Levy KN. Refining the phenotype of borderline personality disorder using finite mixture modeling: Implications for classification. Journal of Personality Disorders. 2008;22:313–331. doi: 10.1521/pedi.2008.22.4.313. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Johnson MD, Willett JB. Individual growth curve analysis illuminates stability and change in personality disorder features: the longitudinal study of personality disorders. Archives of General Psychiatry. 2004;61(10):1015. doi: 10.1001/archpsyc.61.10.1015. [DOI] [PubMed] [Google Scholar]
- Lilienfeld SO, Waldman ID, Israel AC. A critical examination of the term and concept of ‘comorbidity’ in psychopathology research. Clinical Psychology Science and Practice. 1994;1:71–83. [Google Scholar]
- Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, et al. Two-Year randomized controlled trial and follow-up of Dialectical Behavior Therapy vs. therapy by experts for suicidal behaviors and Borderline Personality Disorder. Archives of General Psychiatry. 2006;63:757–766. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- Livesley WJ, Jang KL, Vernon PA. Phenotypic and genetic structure of traits delineating personality disorder. Archives of General Psychiatry. 1998;55(10):941. doi: 10.1001/archpsyc.55.10.941. [DOI] [PubMed] [Google Scholar]
- Luyten P, Blatt SJ. Interpersonal Relatedness and Self-Definition in Normal and Disrupted Personality Development: Retrospect and Prospect. American Psychologist. 2013 doi: 10.1037/a0032243. [DOI] [PubMed] [Google Scholar]
- Markon KE. Modeling psychopathology structure: a symptom-level analysis of Axis I and II disorders. Psychological Medicine. 2010;12(2):273. doi: 10.1017/S0033291709990183. [DOI] [PubMed] [Google Scholar]
- Meyer B, Pilkonis PA. An attachment model of personality disorders. In: Lenzenweger MF, Clarkin JF, editors. Major theories of personality disorder. 2. New York: Guilford Press; 2005. pp. 231–281. [Google Scholar]
- Mroczek DK, Spiro A. Modeling intraindividual change in personality traits: Findings from the Normative Aging Study. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2003;58(3):P153–P165. doi: 10.1093/geronb/58.3.p153. [DOI] [PubMed] [Google Scholar]
- Pfohl B, Blum N, Zimmerman M. Structured Interview for DSMIV Personality. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- Pilkonis PA, Heape CL, Proietti JM, Clark SW. The reliability and validity of two structured diagnostic interviews for personality disorders. Archives of General Psychiatry. 1995;52:1025–1033. doi: 10.1001/archpsyc.1995.03950240043009. [DOI] [PubMed] [Google Scholar]
- Pincus AL. A contemporary integrative interpersonal theory of personality disorders. In: Clarkin J, Lenzenweger M, editors. Major theories of personality disorder. 2. New York: Guilford; 2005. pp. 282–331. [Google Scholar]
- Pincus AL, Lukowitsky MR, Wright AGC. The interpersonal nexus of personality and psychopathology. In: Millon T, Krueger RF, Simonsen E, editors. Contemporary directions in psychopathology: Scientific Foundations for the DSM-V and ICD-11. New York, NY: Guilford Press; 2010. pp. 523–552. [Google Scholar]
- Pincus AL, Wiggins JS. Interpersonal problems and conceptions of personality disorders. Journal of Personality Disorders. 1990;4:342–352. [Google Scholar]
- Roberts BW, Caspi A, Moffitt TE. Work experiences and personality development in young adulthood. Journal of Personality and Social Psychology. 2003;84(3):582. [PubMed] [Google Scholar]
- Roberts BW, Walton KE, Viechtbauer W. Patterns of mean-level change in personality traits across the life course: a meta-analysis of longitudinal studies. Psychological bulletin. 2006;132(1):1–25. doi: 10.1037/0033-2909.132.1.1. [DOI] [PubMed] [Google Scholar]
- Røysamb E, Kendler KS, Tambs K, Ørstavik RE, Neale MC, Aggen SH, Reichborn-Kjennerud T. The joint structure of DSM-IV Axis I and Axis II disorders. Journal of abnormal psychology. 2011;120(1):198. doi: 10.1037/a0021660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell JJ, Moskowitz DS, Zuroff DC, Sookman D, Paris J. Stability and variability of affective experience and interpersonal behavior in borderline personality disorder. Journal of Abnormal Psychology. 2007;116:578–588. doi: 10.1037/0021-843X.116.3.578. [DOI] [PubMed] [Google Scholar]
- Sadikaj G, Moskowitz DS, Russell JJ, Zuroff DC, Paris J. Quarrelsome behavior in borderline personality disorder: Influence of behavioral and affective reactivity to perceptions of others. Journal of Abnormal Psychology. 2013;122:195–207. doi: 10.1037/a0030871. [DOI] [PubMed] [Google Scholar]
- Sadikaj G, Russell JJ, Moskowitz DS, Paris J. Affect dysregulation in individuals with borderline personality disorder: Persistence and interpersonal triggers. Journal of Personality Assessment. 2010;92:490–500. doi: 10.1080/00223891.2010.513287. [DOI] [PubMed] [Google Scholar]
- Salzer S, Streeck U, Jaeger U, Masuhr O, Warwas J, Leichsenring F, et al. Patterns of interpersonal problems in borderline personality disorder. Journal of Nervous and Mental Disease. 2013;201(2):94–98. doi: 10.1097/NMD.0b013e3182532b59. [DOI] [PubMed] [Google Scholar]
- Sanislow CA, Pine DS, Quinn KJ, Kozak MJ, Garvey MA, Heinssen RK, Cuthbert BN. Developing constructs for psychopathology research: research domain criteria. Journal of abnormal psychology. 2010;119(4):631. doi: 10.1037/a0020909. [DOI] [PubMed] [Google Scholar]
- Santangelo P, Bohus M, Ebner-Priemer UW. Ecological Momentary Assessment in Borderline Personality Disorder: A Review of Recent Findings and Methodological Challenges. Journal of Personality Disorders. doi: 10.1521/pedi_2012_26_067. (in press) [DOI] [PubMed] [Google Scholar]
- Scott LN, Kim Y, Nolf KA, Hallquist MN, Wright AGC, Stepp SD, Morse JQ, Pilkonis PA. Preoccupied attachment and emotional dysregulation: Specific aspects of borderline personality disorder or general dimensions of personality pathology? Journal of Personality Disorders. 2013;27(4):473–495. doi: 10.1521/pedi_2013_27_099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skodol AE, Gunderson JG, Shea MT, McGlashan TH, Morey LC, Sanislow CA, Stout RL. The collaborative longitudinal personality disorders study (CLPS): Overview and implications. Journal of personality disorders. 2005;19(5):487–504. doi: 10.1521/pedi.2005.19.5.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracey TJG, Rounds JB, Gurtman MB. Examination of the general factor with the interpersonal circumplex structure: Application to the Inventory of Interpersonal Problems. Multivariate Behavior Research. 1996;31:441–466. doi: 10.1207/s15327906mbr3104_3. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Durrett CA. Categorical and dimensional models of personality disorder. Annual Review of Clinical Psychology. 2005;1:355–380. doi: 10.1146/annurev.clinpsy.1.102803.144009. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Solhan MB, Tragesser SL, Jahng S, Wood PK, Piasecki TM, Watson D. Affective instability: Measuring a core feature of borderline personality disorder with ecological momentary assessment. Journal of Abnormal Psychology. 2008;117(3):647. doi: 10.1037/a0012532. [DOI] [PubMed] [Google Scholar]
- Von Neumann J, Kent RH, Bellinson HR, Hart BT. The mean square successive difference. The Annals of Mathematical Statistics. 1941;12(2):153–162. [Google Scholar]
- Widiger TA. Four out of five ain’t bad. Archives of General Psychiatry. 1998;55:865–866. doi: 10.1001/archpsyc.55.10.865. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Sanderson CJ. Towards a dimensional model of personality disorders in DSM-IV and DSM-V. In: Livesley WJ, editor. The DSM-IV Personality Disorders. New York: Guilford Press; 1995. pp. 433–458. [Google Scholar]
- Widiger TA, Simonsen E. Alternative dimensional models of personality disorder: Finding a common ground. Journal of personality disorders. 2005;19(2):110–130. doi: 10.1521/pedi.19.2.110.62628. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and individual differences. 2001;30(4):669–689. [Google Scholar]
- Wright AGC. Quantitative and qualitative distinctions in personality disorder. Journal of Personality Assessment. 2011;93(4):370–379. doi: 10.1080/00223891.2011.577477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Hallquist MN, Beeney JE, Pilkonis PA. Borderline personality pathology and the stability of interpersonal problems. Journal of Abnormal Psychology. 2013;122(4):1094–1100. doi: 10.1037/a0034658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Hallquist MN, Morse JQ, Scott LN, Stepp SD, Nolf KA, Pilkonis PA. Clarifying interpersonal heterogeneity in borderline personality disorder using latent mixture modeling. Journal of Personality Disorders. 2013;27(2):125–143. doi: 10.1521/pedi.2013.27.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Pincus AL, Lenzenweger MF. Development of personality and the remission and onset of personality pathology. Journal of Personality and Social Psychology. 2011;101(6):1351–1358. doi: 10.1037/a0025557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Pincus AL, Lenzenweger MF. Interpersonal development, stability, and change in young adulthood. Journal of Personality. 2012;80(5):1339–1372. doi: 10.1111/j.1467-6494.2012.00761.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Simms LJ. On the structure of personality disorder traits: Conjoint analyses of the CAT-PD, PID-5, and NEO-PI-3 trait models. Personality Disorders: Theory, Research, and Treatment. doi: 10.1037/per0000037. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Thomas KM, Hopwood CJ, Markon KE, Pincus AL, Krueger RF. The hierarchical structure of DSM-5 pathological personality traits. Journal of Abnormal Psychology. 2012;121(4):951–957. doi: 10.1037/a0027669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. The 10-year course of psychosocial functioning among patients with borderline personality disorder and axis II comparison subjects. Acta Psychiatrica Scandinavica. 2010;122(2):103–109. doi: 10.1111/j.1600-0447.2010.01543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. Attainment and stability of sustained symptomatic remission and recovery among patients with borderline personality disorder and axis II comparison subjects: a 16-year prospective follow-up study. The American journal of psychiatry. 2012;169(5):476–483. doi: 10.1176/appi.ajp.2011.11101550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman M, Chelminski I, Young D. The frequency of personality disorders in psychiatric patients. Psychiatric Clinics of North America. 2008;31(3):405–420. doi: 10.1016/j.psc.2008.03.015. [DOI] [PubMed] [Google Scholar]