Abstract
African-American (AA) men are significantly more likely to die of prostate cancer (PrCA) than other racial groups, and there is a critical need to identify strategies for providing information about PrCA screening and the importance of informed decision making (IDM). To assess whether a computer-based IDM intervention for PrCA screening would be appropriate for AA men, this formative evaluation study examined their (1) PrCA risk and screening knowledge, (2) decision-making processes for PrCA screening, (3) usage of, attitudes toward, and access to interactive communication technologies (ICTs), and (4) perceptions regarding a future novel computer-based PrCA education intervention. A purposive convenience sample of 39 AA men aged 37–66 years in the Southeastern United States were recruited through faith-based organizations to participate in one of six 90-minute focus groups and complete a 45-item descriptive survey. Participants were generally knowledgeable about PrCA; however, few engaged in IDM with their doctor and few were informed about the associated risks and uncertainties of PrCA screening. Most participants used ICTs on a daily basis for various purposes including health information seeking. Most participants were open to a novel computer-based intervention if the system was easy to use and its animated avatars were culturally appropriate. Because study participants had low exposure to IDM for PrCA, but frequently used ICTs, IDM interventions using ICTs (e.g, computers) hold promise for AA men and should be explored for feasibility and effectiveness. These interventions should aim to increase PrCA screening knowledge and stress the importance of participating in IDM with their doctor.
Keywords: Technology, Prostate Cancer Screening, Informed Decision Making, Minority Health
Background
With 233,000 men estimated to be diagnosed with and 29,480 to die of prostate cancer (PrCA) in 2014, the disease is the most commonly diagnosed non-skin cancer and the second leading cause of cancer death among all men in the U.S. (American Cancer Society, 2014). Despite its high incidence and relatively low mortality, there is a pronounced disparity in the incidence and mortality rates between African-American (AA) and European-American (EA) (i.e. White) men (Siegel, Naishadham, & Jemal, 2012; U.S. Cancer Statistics Working Group, 2013). AA men have an incidence rate of PrCA that is over 50% higher than in EAs on average (American Cancer Society, 2011, 2014). In the Southeastern U.S., AAs tend to have a higher mortality from most cancers (including PrCA) than people in other parts of the country (Hébert, Daguise, Hurley, Wilkerson, Mosley, Adams & Bolick, Aldrich, 2009; Wagner, Hurley, Hébert, McNamara, Bayakly, & Vena, 2012). In particular, Hébert et al., 2009 discovered that AAs in South Carolina are 60% more likely to die from PrCA than EAs. Owing in part to these racial disparities is the fact that PrCA has very different implications in AAs, in whom the disease tends to be more aggressive (Drake, Keane, Mosley, Adams, Elder, Modayil, Ureda, & Hebert, 2006). The disparities between AAs in comparison to other races and recent longitudinal research has led to considerable controversy regarding the benefits of PrCA screening (Andriole et al., 2009; Barry, 2009; Schroder, et al., 2009; Smith, Cokkinides, & Brawley, 2012; U.S. Preventive Services Task Force, 2011). Whereas some non-profit and grassroots organizations embrace the lifesaving potential of prostate-specific antigen (PSA) screening (a blood test) (Mitka, 2009; National Medical Association, 2011; Us TOO International, 2011), some professional organizations and medical and research experts disagree about its efficacy (U.S. Preventive Services Task Force, 2011). The American Cancer Society (ACS) recommends that men make an informed decision with their doctor about whether or not to be screened for the disease (American Cancer Society, 2014). The Centers for Disease Control and Prevention’s Task Force on Community Preventive Services defines informed decision making (IDM) as: “when an individual understands the nature of the disease or condition being addressed; understands the clinical service and its likely consequences, including risks, limitations, benefits, alternatives, and uncertainties; has considered his or her preferences as appropriate; has participated in decision making at a personally desirable level; and either makes a decision consistent with his or her preferences and values or elects to defer a decision to a later time” (Briss, Rimer, Reilley, Coates, Lee, Mullen, Corso, Hutchinson, Hiatt, Kerner, George, White, Gandhi, Saraiya, Breslow, Isham, Teutsch, Hinman, & Lawrence, 2004, p. 1214).
There are multiple patient (e.g., medical mistrust, fear, decreased self-efficacy) and physician-related (e.g., lack of medical knowledge, limited availability, and subpar interpersonal skills) barriers that hinder IDM between AAs and their doctors (Peek, Quinn, Gorawara-Bhat, Odoms-Young, Wilson, & Chin., 2009; Sanchez, Bowen, Hart, & Spigner, 2007; Woods, Montgomery, Herring, Gardner, & Stokols, 2006). One key facilitator of IDM is ensuring that the patient has an understanding about a disease and its implications (i.e. knowledge, health literacy) (Lovell, Lee, & Brotheridge, 2010, Peek et al., 2009). To prepare individuals of varying health literacy levels for participation in IDM, the Institute of Medicine recommends the use of effective, plain language, and culturally appropriate communication strategies (Institute of Medicine, Committee on Health Literacy, & Board of Neuroscience and Behavioral Health, 2004). Some strategies to prepare individuals for participation in IDM have included the use of paper-based decision aids but have been expanded in recent years to include interactive communication technologies (ICTs) (e.g., computers, kiosks), which can increase access to these decision aids/interventions (i.e. reach) and produce a more engaging experience for the user (Lisetti, Yasavur, De Leon, Amini, Rishe, & Visser, 2012; Ellison, Weinrich, Lou, Xu, Powellm & Baquet, 2008; Volk, Hawley, Kneuper, Holden, Stroud, Cooper, & Pavlik, 2007;). For instance, Lissetti (2012) reports that using computer-based interventions which include embodied conversational agents (i.e. avatars) could be a means for addressing low literacy, eliminating variability in intervention implementation, tailoring information based on individual users, and implementing race concordance by an matching avatar’s appearance to the race of the user.
Several research studies have recognized ICTs as effective and culturally appropriate mediums for disseminating plain language health content to diverse populations (Bernhardt, Mays, Eroğlu, & Daniel, 2009; Bernhardt, Mays, & Kreuter, 2011; Gielen et al., 2007; Porter, Cai, Gribbons, Goldmann, & Kohane, 2004; Thompson, Lozano, & Christakis, 2007) and serving as decision-making aids for the prevention and/or treatment of a number of chronic diseases including lung, colorectal, and prostate cancers (Allen, Mohllajee, Shelton, Drake, & Mars, 2009; Cupertino et al., 2010; Evans et al., 2010; Kassan et al., 2012; Lindblom, Gregory, Wilson, Flight, & Zajac, 2011; Miller et al., 2011; Schroy, Mylvaganam, & Davidson, 2011; Wakefield et al., 2011). Some outcomes that have been demonstrated through the use of ICTs for cancer in general include increasing health knowledge, influencing healthy behaviors, and assisting with decisions about screening (Bass, Gordon, Ruzek, Wolak, Ruggieri, Mora, Rovito, Britto, Parameswaran, Abedin, Ward, Paranjape, Lin, Meyer, & Pitts, 2012; Hassinger, Holubar, Pendlimari, Dozois, Larson, & Cima, 2010; Ryhänen, Siekkinen, Rankinen, Korvenranta, & Leino-Kilpi, 2010; Schroy et al., 2011). For PrCA specifically, there have been studies demonstrating the efficacy of using computer-based ICT’s to increase men’s knowledge about PrCA, enhance their IDM self-efficacy, and reduce decisional conflict regarding cancer screening and/or treatment (Frosch, Bhatnagar, Tally, Hamori, & Kaplan, 2008; Ilic, Egberts, McKenzie, Risbridger, & Green, 2008; Kassan et al., 2012; Krist, Woolf, Johnson, & Kerns, 2007). Few studies have examined the use of computer-based ICTs solely for facilitating informed PrCA screening decisions among AA men (Allen et al., 2009).
Technology Use and Health & Cancer Information Seeking among African Americans
When considering access to ICTs, over half of AAs own a desktop (45%) or laptop (51%) computer (Pew Internet & American Life Project, 2012b). As for broadband internet, AAs have less access than EAs (74% versus 64%) (Cohall, Nye, Moon-Howard, Kukafka, Dye, Vaughan, & Northridge, 2011; Pew Internet & American Life Project, 2013c), but AA’s adoption of mobile (93% of AAs versus 90% of EAs) and smart phones (64% of AAs versus 43% of EAs) has led to a modest narrowing of the digital divide (Pew Internet and American Life Project, 2013). Pew also reports that 74% of AAs seek health information online about a variety of topics, but most often search for disease-specific information (Pew Internet & American Life Project, 2013a). There have been few recent studies, that have assessed AAs’ cancer-specific information sources, including PrCA (Friedman, Thomas, Owens, & Hebert, 2012b; Ross, Dark, Orom, Underwood, Anderson-Lewis, Johnson, & Erwin, 2011). However, because of the burden of PrCA and the exponential growth in access to ICTs among AAs, further research on the use of ICTs for facilitating IDM among AA men is warranted (Pew Internet & American Life Project, 2012b, Pew Internet and American Life Project, 2013a–c).
In order to create the most effective future PrCA IDM intervention for AA men in South Carolina faith communities, formative research was conducted to determine AA men’s (1) current PrCA risk and screening knowledge, (2) decision-making processes for PrCA screening, and (3) usage of, attitudes toward, and access to ICTs (e.g., computers, ATMs, kiosks) (4) preferences toward a novel computer-based PrCA education intervention using avatars. The results from this formative research are intended to inform the appropriate PrCA content, interface (e.g., inclusion of an avatar), and functionality of a collaboratively developed, computer-based intervention.
Conceptual Framework
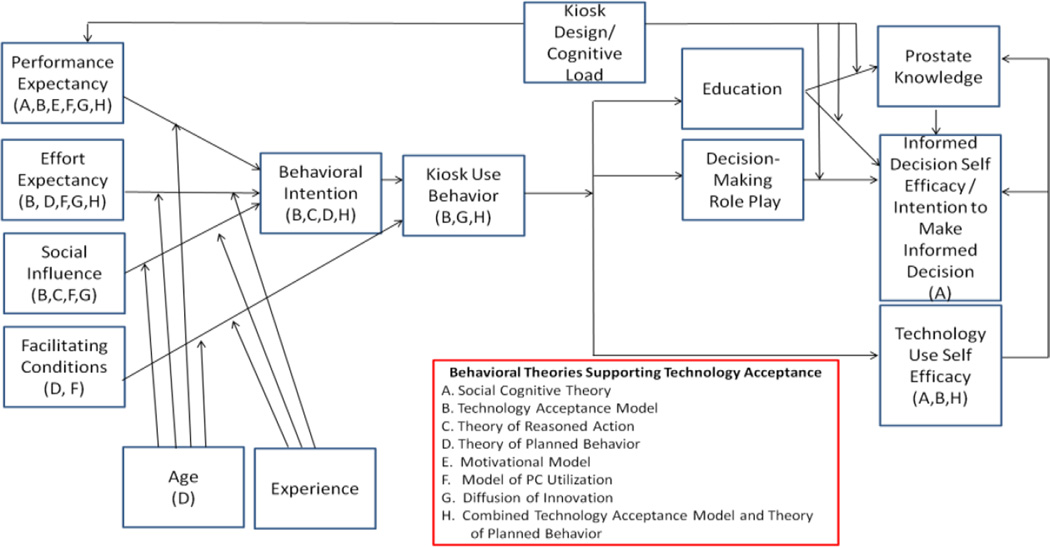
The conceptual framework guiding this study (See Figure 1) has been adapted from Venkatesh’s Unified Theory of Acceptance and Use of Technology (UTAUT) (Venkatesh, Morris, Davis, & Davis, 2003). The theory posits that four key constructs including performance expectancy (i.e. the degree to which a man believes that a computer/kiosk-based intervention that delivers education and a decision-making role play will lead to personal gains such as prostate knowledge), effort expectancy (i.e. the degree of ease associated with using the intervention to retrieve information), social influence (i.e. the degree to which an individual perceives the importance that his social network (e.g., friends and family) will place on the use of the decision aid) and facilitating conditions (i.e. degree to which an individual believes that an organizational and technical infrastructure exists to support use of a computer/kiosk intervention for IDM), moderated by factors such as age and experience, contribute to an individuals’ behavior intention (i.e. intention to use) and intervention use behavior (i.e. adoption of the computer/kiosk as a regular source of information) (Venkatesh et al., 2003). The theory is based on the consolidation of eight validated health behavior theories (e.g., Social Cognitive Theory) which contain several common tenets supporting the adoption of any technology (Ajzen, 1991; Bufford, 1986; Compeau & Higgins, 1995; Davis, Bagozzi, & Warshaw, 1992; Fishbein & Ajzen, 1979; Rogers, 2003; Taylor & Todd, 1995; Thompson, Higgins, & Howell, 1991).
Figure 1.
Conceptual Framework based on Venkatesh et al. (2003) and Mayer and Moreno (2003).
In order to develop a computer-based PrCA education intervention that will lead to our long-term targeted outcomes (i.e. improved prostate knowledge, greater informed decision self-efficacy/intention to make an informed decision, and increased technology use self-efficacy), it is important to be cognizant of principals relevant to interface design and its impact on an individual’s ability to process information disseminated by a computer. According to Mayer’s theory of cognitive multimedia learning (CMLT) (represented by the kiosk design/cognitive load in Figure 1), individuals process information through two channels that have limited capacity (i.e. cognitive load) (Mayer & Moreno, 2003). Mayer & Moreno have several recommendations for designing multimedia that can enhance a person’s capacity for processing information and enhance learning. Multimedia presentations, for example, should stress auditory, as opposed to visual, presentation of words in order to reduce the amount of attention that a person has to devote to processing text (Mayer & Moreno, 2003). CMLT has been used to design several computer-based media for adults (Paas & Sweller, 2012; Struve & Wandke, 2009; Van Gerven, Paas, & Tabbers, 2006; van Weert, van Noort, Bol, van Dijk, Tates, & Jansen, 2011; Wilson & Wolf, 2009; Xie, Yeh, Walsh, Watkins, & Huang, 2012). When used in conjunction, the UTAUT and CMLT not only offer a full perspective of the various ways in which technology can affect health outcomes, but also provide the appropriate framework to guide the formative research, development, and feasibility testing of a computer-based PrCA intervention.
Methods
Sampling Description and Procedures
The University of South Carolina Institutional Review Board approved the research prior to implementation. A purposive, (Patton, 1990) convenience sample of AA men ages 40+ years from AA churches in and in close proximity to Columbia, South Carolina were asked to participate in one of six focus groups. Recruitment efforts were guided by Vesey’s framework on recruitment and retention of minority groups that involves a series of strategies such as leveraging partnerships in the community to assist researchers throughout the planning and implementation process (Vesey, 2002). Purposeful recruitment strategies included the distribution of flyers to churches, barbershops, and community organizations; in-person announcements at churches; one-on-one meetings with pastors and community leaders; radio promotion on stations with a large number of AA listeners; messages on AA community organization, academic, and healthcare system websites/listservs; and participation in health-related activities (e.g., health fairs) at churches. Besides being 40+ years old (see results for one exception), eligible AA men had to: (1) speak and comprehend English, (2) have no personal history of PrCA, and (3) have no history of cognitive decline that will inhibit their participation.
Churches were selected as appropriate settings for the proposed research because prior studies have concluded that AAs’ spiritual needs (in addition to their socio-cultural and psychological needs) often influence their participation and trust in health research (Campbell et al., 2004; Holt et al., 2009; Huang & Coker, 2010; Resnicow et al., 2005; Rimer, Briss, Zeller, Chan, & Woolf, 2004; Vesey, 2002). A minimum of three and a maximum of ten men were included in each of the six focus groups. The sampling strategy for the focus groups in this study was based on the qualitative research principles of saturation and sufficiency (Glaser & Strauss, 1967; Morse & Field, 1995; Seidman, 1998; Strauss & Corbin, 1998). Based on prior research, it was predicted that saturation and sufficiency should be reached within five to six focus groups (Friedman et al., 2012a; Friedman et al., 2012b). Recruitment for and implementation of all focus groups took place between September and December 2012.
Data Collection Procedures
Descriptive surveys
One-half hour prior to each focus group, participants were provided with an informed consent document, which was explained on the telephone prior to the focus group and reviewed and signed in-person. After returning the signed consent document to the focus group facilitator, participants were also administered a short descriptive survey. The 18-item survey assessed participant’s: (1) use of technologies for receiving health information, (2) non-technology-related resources for health information, (3) most common and preferred sources of HI, (4) PrCA screening behaviors, and (5) PrCA IDM practices.
Focus groups
The 90-minute focus groups were held in the fellowship halls of churches around Columbia, SC and at a conference room on the campus of the University. During the focus group, participants were asked questions about their: (1) current PrCA knowledge including prostate anatomy, PrCA prevention symptoms, prostate screening and diagnosis, and risks and benefits of PrCA screening, (2) their decision-making process regarding whether or not to receive PrCA screening, and (3) types of, access to, and personal or health-related use of ICTs. Participants were also asked about social and physical barriers/facilitators of using ICTs and suggestions for alleviating these barriers. In addition, participants were asked about recommendations for a culturally appropriate computer-based intervention for promoting IDM for PrCA screening. Items for the focus group guide were created based on domains from our team’s previous research (Friedman et al., 2012a; Friedman et al., 2012b), but expanded to include general content about their technology use and performance expectancy (e.g., “How often do you use email to find health information?”) which are consistent with constructs in our conceptual framework. Each focus group was consistently moderated by one AA researcher and each group discussion was digitally recorded. All data were transcribed by a professional transcription service. Following transcription, the audio recording from each focus group was compared to its corresponding transcript to ensure quality. Each participant received a monetary honorarium of $10 for their involvement in the study.
Data analysis/analytic approach
Analyses of the data on the descriptive survey were calculated using SPSS® 20.0 (SPSS Inc., 2012). Data from focus group transcripts were managed using NVivo® 9 (QSR, 2010), a qualitative software program. Prior to downloading focus group transcript data into NVivo®, a preliminary draft codebook was developed through a grounded theory approach where the open coding of analogous transcripts by two researchers (including the focus group moderator) led to the conceptual organization of the data based on potential themes (Glaser & Strauss, 1967; Strauss & Corbin, 1998). After the codebook was finalized, NVivo® was used to facilitate the axial coding of all transcripts. Axial coding helped us identify any thematic relationships that existed between codes (Strauss & Corbin, 1998). Inter-rater reliability was calculated using a percent-agreement method in which the number of agreed codes are divided by the total number of items coded (i.e. agreements and disagreements) (Neuendorf, 2002). Throughout the analysis process, emergent themes were compared and contrasted between and within focus groups (Glaser & Strauss, 1967).
Results
Demographic Survey
Descriptive Characteristics of Participants
The sample (see Table 1) included 39 AA male participants with a mean age of 53.6 (SD =7.2) years. One of the 39 participants did not meet the age criteria (he was age 37 at the time of the study), but was allowed to participate. Most participants either had some college or vocational school (33%, n=13) or had completed vocational school, bachelors, or higher degree (40%, n=16). Many of the participants were also married (61%, n=24), employed full-time (54%, n=21), and had some form (e.g. private, Medicare) of health insurance (92%, n=36). Household incomes were variable, but a quarter (26%, n=10) of participants reported earning between $20,000 and $39,999 annually.
Table 1.
Descriptive Statistics
| Variable | Frequency | Mean (SE) or % |
|---|---|---|
| Age | 39 | 53.6 (7.2) |
| Education | ||
| High School | 10 | 26.0 % |
| Some College or Vocational School | 13 | 33.0 % |
| Completed College or Vocational School | 7 | 18.0 % |
| Post Graduate School | 9 | 23.0 % |
| Marital Status | ||
| Single/Never Married | 7 | 18.0 % |
| Married | 24 | 61.0 % |
| Separated | 4 | 10.0 % |
| Divorced | 3 | 8.0 % |
| Other | 1 | 3.0 % |
| Income | ||
| <$19,999 | 7 | 18.0 % |
| $20,000–$39,999 | 10 | 26.0 % |
| $40,000–$59,999 | 2 | 5.0 % |
| $60,000–$79,999 | 7 | 18.0 % |
| $80,000–$99,999 | 4 | 10.0 % |
| ≥$100,000 | 6 | 15.0 % |
| Not Reported | 3 | 8.0 % |
| Employment | ||
| Full time | 21 | 54.0 % |
| Part time | 3 | 8.0 % |
| Retired | 4 | 10.0 % |
| Unemployed | 6 | 15.0 % |
| Not Reported | 5 | 13.0 % |
| Health Insurance (Type)* | ||
| Employer | 19 | 49.0 % |
| Private | 20 | 51.0 % |
| Medicare | 6 | 15.0 % |
| Medicaid | 2 | 5.0 % |
| Military Healthcare | 11 | 28.0 % |
| Prescription Drug Coverage | 5 | 13.0 % |
| Other | 1 | 3.0 % |
| No Coverage | 3 | 8.0 % |
Question allowed multiple responses to accommodate all options that applied so percentages will not equal to 100%
Findings: Focus Groups
Qualitative findings below have been divided into two main categories based on our original research questions and the pattern of the results. These categories are as follows: (1) PrCA knowledge and decision making, and (2) technology use and barriers (See Table 2).
Table 2.
Focus Group Themes
| FOCUS GROUP THEMES AND SUBTHEMES |
Summary | Explanatory/Representative Quotes |
|---|---|---|
| 1. Prostate Cancer Knowledge | ||
| Prostate Cancer Risks | Most participants were knowledgeable about
cancer risks including links to race, age, heredity, and diet. |
“As a black man…, we are
more susceptible to get it [PrCA] than Caucasians or any other race.” |
| Prostate Cancer Screening | Most participants were knowledgeable about two
types of PrCA screening with few misperceptions that were most often linked to confusion with a colonoscopy |
“They do a blood test, or do a
rectal inspection to see…..if the prostate is swollen…” |
| Prostate Cancer Symptoms | Participants had some but varied knowledge about
the symptoms of PrCA with some misperceptions. |
“I think having polyps over a
long period of time that aren’t removed. It turns into cancer.” (misperception) |
|
2. Prostate Screening
Decision Making |
||
| Participant’s healthcare provider
makes final decision |
Many participants received screening as advised by
a healthcare provider |
“The first thing she does is say
it’s that time a year again. She puts on the plastic glove. Drop your pants, and turn around.” |
| Participant’s job requires screening | Some participants (e.g., military) were required
to receive annual screening exams. |
“In the military it was forced
upon you…” |
| 3. Technology Use | ||
| Definitions, access, and purposes | Technology was defined by electronic items such as
cell phones, computers, tablets, television, radio, and internet. These items were used on a daily basis for a variety of professional and leisurely purposes. |
“Every day at work I’m on
the internet emailing.” |
| Health and cancer information | Participants report frequently using TV and internet
as frequent sources for heath and PrCA information |
“A lot of information I’ve been able
to gather, just not about cancer but just about any kind of different medical issue, has been on the internet.” |
| Technology usability/barriers | The lack of prior experience or education, and age
may affect a person’s ability to use a technology, but most participants suggested that technologies are effortless. |
“It’s not a matter of what we can do
to make it easier, other than education…Basically you have to have the willingness to learn” |
Prostate cancer knowledge and decision making
Prostate cancer knowledge: symptoms, risks, and screening
Overall, most participants had at least some knowledge about PrCA including the symptoms, risks, and screenings used for PrCA. However, participants’ knowledge about each of these areas varied. Participants knew the least about PrCA symptoms. The symptoms most commonly mentioned by participants were those related to difficulty urinating or frequent urination. The most common misperception among participants was that PrCA caused rectal bleeding. Most participants were particularly familiar with the most common risk factors for PrCA and most often reported race (e.g., AAs being at the highest risk), heredity, age, and diet as risks for the disease. The most common reasons why participants reported that AAs are at the highest risk for PrCA included their perceptions that AAs have unhealthy diets, lack regular visits to a doctor’s office, have inadequate health insurance, and/or lack of awareness about PrCA. In addition, most participants were knowledgeable about the two types of PrCA screening (i.e. PSA and digital rectal exam (DRE)) and the recommended age at which conversations about PrCA screening should take place (i.e. as early as 40 to 45 years for high-risk groups). There were also some misperceptions about PrCA screening such as confusion of a colon cancer screening (i.e. or colonoscopy) with screening for PrCA.
Prostate screening decision making
The majority of participants reported receiving either one or both screenings for PrCA and received their first screening at or near 40 years of age. PrCA screenings were often performed at a doctor’s offices upon recommendation of the participant’s doctor, as a requirement of a job, or as a personal decision prompted by knowledge about PrCA risks among AAs. In many instances, participants reported receiving PrCA screenings on an annual basis.
When asked about their role in the IDM process prior to screening, some participants sensed that doctors didn’t provide patients with a voice in the decision making process, but rather swayed participants towards receiving PrCA screening. Those who had no prior information about PrCA screening, were especially reliant on the information and screening advice provided by their doctors. While participant’s doctors commonly informed them about the benefits of PrCA screening, none of the participants reported being informed by their doctors about the risks and uncertainties of the PrCA screening.
Technology Use and Barriers
Technology use: definitions, access, and purposes
When asked about what types of items that come to mind when they hear the word technology, most participants associated the term with electronics such as cell phones, computers, tablets, television, radio, and internet. All participants reported having access to more than one of the aforementioned technologies. In addition, almost all participants reported using technology (particularly computers, mobile phones, and television) on a daily basis and for various purposes including those related to business, leisure, and receiving/seeking health and cancer information. For example, when asked about sources for health and cancer information, one participant responded “A lot of information I’ve been able to gather, just not about cancer but just about any kind of different medical issue, has been on the internet.” Although mentioned slightly less often, participants also reported receiving health and cancer information through radio and mobile phones.
Technology usability/barriers
Though most of the participants reported being comfortable using technology, they were typically not able to communicate what elements of the actual interface or features/functions of various technologies made them easy to use. Participants simply referred to the accessibility of the technology. When asked what would make it hard for others to use the technologies aforementioned, some participants reported that the lack of prior experience, lack of technology education, and age may affect a person’s ability to use any technology, but overall participants suggested that the technologies they use require little effort.
Recommendations for a computer-based PrCA education intervention
Content
When asked about the content that should be included in a computer-based intervention to help a man make an informed decision with his doctor about PrCA screening, all participants reported that the intervention should focus on a number of topics including: prostate location, disease prevalence, signs and symptoms of PrCA, age at which men should begin discussions about screening, disease prevention, and treatment options. Many participants stressed that this information should be simple enough for any lay person to use, especially those who are older or have lower literacy levels.
Intervention Features/User Interest
There were several features that were recommended for a computer-based intervention to make it easy to use by AA men with varying levels of computer literacy and to attract users. General features recommended by participants included: large text and buttons, an audio option for individuals who did not prefer reading, an index for navigating to specific information without having to sit for the entire presentation, a touch screen, an interactive interface, a question and answer exercise, and AA presenters. All participants stressed that the intervention should not exceed 5 to 10 minutes in duration, be as simple as possible, and protect their privacy (i.e. information provided and received).
Participants also were asked to give their thoughts on an avatar being featured in the intervention. While most were open to the idea, two participants from a single focus group expressed concerns. Participants who were open to the avatar most frequently reported that the avatar should be: (1) male (2) AA (3) aged similar to the target population and (4) as human-like as possible. The key concern voiced by the two participants who were slightly skeptical about the inclusion of an avatar was the age-appropriateness of using an avatar. Because avatars are commonly associated with games and play, some participants wondered whether older men would use the intervention if it featured an avatar. For example, one participant reported “Because I’m in my 50’s right now …I would watch it. But you may have some that are older, that will say, I don’t have time for this.”
In addition to general features of the computer-based intervention, participants also were asked what specific features should be included to promote user interest. The most commonly mentioned features were the inclusion of (1) sports-related videos or (2) images of attractive women. In a discussion about what will attract an AA man to use a computer-based PrCA intervention, one participant suggested “you need something that is going to draw them over; fishing, football….or something like that just to catch the eye.” Another participant stated “For some folks, an attractive female would be right on.” Other commonly mentioned features to promote interest in the use of the intervention included moving graphics or text that can catch an individual’s attention and offering an incentive such as a coupon or promotional item for using the intervention.
Location
Though the focus group guide did not aim to assess a location for the intervention, participants had multiple suggestions for future locations where the intervention could be placed. Suggested locations most often included high-traffic areas such as service businesses (e.g., barber/beauty shops), convenient/grocery stores, and churches. For example, one participant stated “you have to put it at some gas joint where people go and hang out. Because a lot of them [men] don’t go to church.”
Discussion
Our research has provided insight regarding AA participants’ PrCA screening knowledge and decision making. It also has provided us with a deeper understanding of their use of, attitudes toward, and access to technologies. In addition, the study provided insight on AA men’s perceptions and preferences regarding a novel computer-based PrCA education intervention. These findings have multiple implications for using technology as a vehicle to promote IDM for PrCA screening.
Prostate Knowledge
Overall, most participants were knowledgeable about PrCA including the symptoms, screenings, and risk factors. Participants knew the least about the types of PrCA symptoms. While participants most commonly referred to urinary issues (e.g., frequent urination) when asked about symptoms for PrCA, there are several other common symptoms (e.g., pain in the back or pelvis, blood in the semen, painful ejaculation, and swelling in the legs) which can occur. In addition, there were few participants who reported that PrCA can produce no symptoms. Though many early stage PrCAs do not produce symptoms, it is important for men to have knowledge about the symptoms in case they are experiencing similar symptoms at the time of the discussion with their doctor. Furthermore, it is noteworthy that the most common misperception regarding PrCA screening was rectal bleeding. The prostate is located in front of the bladder and below the rectum and blood has been known to be present in the urine or semen of men with PrCA, but blood from the rectum is not typically associated with PrCA. Bleeding in the rectum has however been periodically associated with prostate biopsies and treatment (American Cancer Society, 2013a). Although there have been few studies that have identified a disparity between AA men’s knowledge about PrCA symptoms in comparison to men of other races, there have been no recent studies that have provided evidence that AA men have less knowledge of PrCA symptoms (Barber, Shaw, Folts, Taylor, Ryan, Hughes, Scott, & Abbott, 1998).
Most participants were familiar with both the DRE and PSA screening tests and seldom confused these screenings other exams such as the colonoscopy. Men in prior studies commonly confused PrCA screening with colorectal cancer screening (Bastani, Gallardo, & Maxwell, 2001; Beeker, Kraft, Southwell, & Jorgensen, 2000; Kilbridge, Fraser, Krahn, Nelson, Conaway, Bashore, Wolf, Barry, Gong, Nease, & Connors, 2009; Palmer, Midgette, & Dankwa, 2008). In addition to the anatomical proximities of the two exams, both may be administered on a routine basis (though routine screening for PrCA is becoming less common, based on the current recommendations). For example, according to many of the participants, PrCA screening is being recommended to them by their doctors on an annual basis beginning at ages ranging from 40 to 50. It also is recommended by ACS that men and women receive a flexible sigmoidoscopy every 5 years and a colonoscopy every 10 years beginning at 50 years of age (American Cancer Society, 2013a). Therefore, It is not uncommon to find men who confuse the PrCA and colorectal cancer screenings, including the age, type of tests, and time frame at which each should take place (Carter, Tippett, Anderson, & Tameru, 2010; Friedman, Corwin, Rose, & Dominick, 2009).
Most participants also were considerably knowledgeable about the main risk factors for PrCA. They most commonly reported race, heredity, and diet as factors for PrCA. Age also was mentioned, (but less often), despite the fact that it is the most significant risk factor for PrCA (American Cancer Society, 2013a). According to the ACS, over two-thirds of men who develop PrCA are over 65 years of age (American Cancer Society, 2013a). Race and heredity also are common risk factors for PrCA (American Cancer Society, 2013a). AA men are twice as likely as EA men to develop and die from PrCA (Siegel et al., 2012). Men who have a father or other male family member with a history of PrCA are also at a greater risk for PrCA (American Cancer Society, 2013a). One of the solutions recommended for reducing the likelihood of PrCA is the adoption of a healthy lifestyle (e.g., reducing the intake of fatty-foods) (American Cancer Society, 2013a). Therefore, a high-fat diet can be considered a risk factor for PrCA.
Prostate Screening Decision Making
Based on their knowledge of PrCA risk factors, symptoms, and screenings, participants are somewhat informed, but they are not participating in PrCA screening IDM with their doctors as recommended by ACS. Most participants reported that they were told about the risks of not receiving PrCA screening and were often encouraged by their doctor to receive screening. It is important, however, that men know about the risks of PrCA screening which include the chances that the PSA can lead to false-negatives, false-positives, and over-diagnosis (American Cancer Society, 2013b), resulting in a variety of negative outcomes. A false negative can cause a man to feel secure about not having PrCA when in fact the cancer is present. A PSA score can be falsely lowered by extraneous factors (e.g., medications) when cancer is actually present (American Cancer Society, 2013b). A false positive can take place when the PSA is elevated by something other than cancer (e.g., rigorous physical activity, benign prostatic hypertrophy) (American Cancer Society, 2013b). The over-diagnosing of cancers is disadvantageous because it can lead men to undergo unnecessary surgeries or receive other treatments for indolent forms of PrCA (Welch & Albertsen, 2009). Men who would likely have not succumbed to their cancer, may be exposed to the many risks associated with PrCA treatment. These risks include, but are not limited to, incontinence and impotence (American Cancer Society, 2013b; Welch & Albertsen, 2009). It is because of these uncertainties about the effectiveness of PrCA screening, that men need to be well informed and share the decision about screening with their doctor.
Technology Use
Consistent with prior research on middle aged to older adults, many participants use various technologies (particularly internet and cell phones) on a frequent basis for a number of purposes (e.g., health information seeking) (Bundorf, Wagner, Singer, & Baker, 2006; Pew Internet & American Life Project, 2012a, 2013c; Pew Internet and American Life Project, 2009a,b; Rains, 2007). Most participants reported that the technologies they used were effortless and reported high levels of fluency with completing computer, email, and web-related tasks (e.g., sending an email). Some participants suggested that these technologies also would be easy for any individual with prior experience using similar technologies (e.g., participants who used internet on their job expressed being more comfortable using the internet outside the job). In addition, some participants also felt that a man’s age could contribute to his technology use and perception of how difficult it is to use a specific technology. Based on the portion of our conceptual framework guided by Venkatesh et al (2003), both age and experience have the potential to moderate other factors (e.g., effort expectancy) to affect technology use. According to our formative research, not solely age-related disabilities (e.g., poor eye sight) could make technologies more difficult to use for older AA men. The correlation between age and perceived technology-use difficulty may be dependent on prior experience, making age an indirect moderator between technology use factors (e.g., performance expectancy) and ultimate technology adoption. For example, since older men might be less likely to use technology for the purposes of a job, they may be less inclined to use similar technologies outside the job. When older, inexperienced men are required to use a new technology, it is exceedingly more difficult. To overcome the perceived difficulty, some participants suggested that some older men may need instructions or education to use new technologies. These findings regarding the diverse ages and levels of computer fluency among anticipated users and other salient suggestions introduced through the focus groups will be considered for the future development of a computer-based, PrCA education intervention. Specifically, we will use information from the focus groups on aspects related to each theoretical tenet of our conceptual framework (e.g., effort expectancy: a touch screen can facilitate ease of use) to develop a user-friendly interface with plain-language content that is appropriate for any user.
Intervention Features/User Interest
The recommendations for a computer-based intervention to facilitate IDM regarding PrCA screening were consistent with technologies used by many individuals on a daily basis. For example, many mobile (i.e. cellphones, tablets) and service kiosks (e.g., Redbox, ATM, Self-checkout) have similar features (e.g., touchscreen, interactive, audio, index) mentioned by participants. By creating a system that is congruent with existing, commonly used technologies, and by customizing these features to accommodate older users, the system can be easy to use for people with varying ages and computer literacy levels. Some participants also recommended that a question and answer exercise be included. The exercise could be helpful to increase knowledge of the participant because it will allow the participant to recall the information learned, respond, and potentially hear the information repeated. In regards to the participant’s concerns about privacy, many studies have concluded that AA men have a mistrust of the medical system and this wariness stems from prior unethical practices of the medical and research communities (Braunstein, Sherber, Schulman, Ding, & Powe, 2008; Moore, Knafl, Hamilton, Godley, Carpenter et al., 2013). Also, though most participants were open to using an avatar if it was realistic and race-concordant, some participants were skeptical about the use of an avatar in the computer-based PrCA education intervention. With the paucity of educational tools that use avatars outside the context of a game, it is not surprising that some participants associate the avatar solely with games. Furthermore, there are several locations which participants reported as being appropriate for placing the final intervention, but future research should be conducted to determine which location will provide the greatest access to the intervention.
Study Limitations
The participant sample was well educated, with no men completing less than high school and a great majority having had at least some college. Despite this limitation, this study provided valuable information that can be used to contribute to the future development of culturally appropriate, plain-language tools for helping AA men make informed decisions about their prostate health.
Conclusion and Implications
The research presented indicates that AA men are knowledgeable about PrCA, but knowledge on some relevant topics is limited. Therefore, it would be advantageous for future interventions to provide basic information about PrCA prevalence, anatomy, risks, symptoms, and screening and also emphasize the role of healthy lifestyle, and knowing the risks, benefits, and uncertainties of PrCA screening. Based on the ACS’s PrCA screening guidelines, the information included in the intervention also needs to stress the importance of men actively participating in the PrCA screening decision process with their doctor. In addition, because of the growing access and acceptability of various technologies within AA communities, these technologies should be considered for use in the widespread dissemination of PrCA information and preparing men for making informed PrCA screening decisions with their doctor. Furthermore, establishing community partnerships that contribute to the formative research process can be exceedingly beneficial when assessing the cultural appropriateness of an intervention platform (i.e. technology) and the design that will lead to optimal impact.
These findings also have important implications for future research. Our study included a small sample of AA men. It is documented in the literature that AA men rely on relatives/friends (particularly AA women) to find health information and in some cases will involve these individuals in their healthcare decisions (Friedman et al., 2012c; Levinson et al., 2005), but women were not included in this study. Future studies should focus on assessing AA women’s PrCA knowledge, technology use, and role in men of faith communities’ PrCA screening decisions. Since most men in our study had a history of PrCA screening, their PrCA knowledge and opinions about the computer-based intervention could be different from men who have not received prior PrCA screenings. Future studies also should include men who have not been screened for PrCA and those with varying education levels as they may have a different perspective on the intervention design. Further research is also warranted on the role of the doctor in men’s IDM processes since participant’s report the doctor as their most common and preferred source for health information.
Acknowledgements
Funded by the University of South Carolina’s (USC) Institute of African American Research, USC’s Science and Health Communication Research Group, USC’s Office of Vice President for Research and the National Cancer Institute (NCI) Community Networks Program U54 CA153461 (PI: Hébert; Project Leader: Friedman). Partially supported by an Established Investigator Award in Cancer Prevention and Control from the Cancer Training Branch of the NCI to J.R. Hébert (K05 CA136975). We also acknowledge the study participants. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Ajzen I. The Theory of Planned Behavior. Organizational Behavior and Human Decision Processes. 1991;50(2):179–211. [Google Scholar]
- Allen JD, Mohllajee AP, Shelton RC, Drake BF, Mars DR. A computer-tailored intervention to promote informed decision making for prostate cancer screening among African American men. American Journal of Mens Health. 2009;3(4):340–351. doi: 10.1177/1557988308325460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Cancer Society. Cancer Facts and Figures For African Americans. Atlanta, GA: 2011. [Google Scholar]
- American Cancer Society. [Retrieved June 6, 2013];American Cancer Society Guidelines for the Early Detection of Cancer. 2013a from http://www.cancer.org/healthy/findcancerearly/cancerscreeningguidelines/american-cancer-society-guidelines-for-the-early-detection-of-cancer.
- American Cancer Society. Cancer Facts and Figures 2014. Atlanta, GA: 2014. [Google Scholar]
- American Cancer Society. Prostate Cancer: Early Detection. Atlanta, GA: 2013b. [Google Scholar]
- Andriole GL, Crawford ED, Grubb RL, Buys SS, Chia D, Church TR, et al. Mortality results from a randomized prostate-cancer screening trial. New England Journal of Medicine. 2009;360(13):1310–1319. doi: 10.1056/NEJMoa0810696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber KR, Shaw R, Folts M, Taylor DK, Ryan A, Hughes M, et al. Differences between African American and Caucasian men participating in a community-based prostate cancer screening program. Journal of Community Health. 1998;23(6):441–451. doi: 10.1023/a:1018758124614. [DOI] [PubMed] [Google Scholar]
- Barry MJ. Screening for prostate cancer - the controversy that refuses to die. New England Journal of Medicine. 2009;360(13):1351–1354. doi: 10.1056/NEJMe0901166. [DOI] [PubMed] [Google Scholar]
- Bass SB, Gordon TF, Ruzek SB, Wolak C, Ruggieri D, Mora G, et al. Developing a computer touch-screen interactive colorectal screening decision aid for a low-literacy African American population: lessons learned. Health Promotion Practice. 2012;14(4):589–598. doi: 10.1177/1524839912463394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastani R, Gallardo NV, Maxwell AE. Barriers to colorectal cancer screening among ethnically diverse high- and average-risk individuals. Journal of Psychosocial Oncology. 2001;19(3–4):65–84. [Google Scholar]
- Beeker C, Kraft JM, Southwell BG, Jorgensen CM. Colorectal cancer screening in older men and women: qualitative research findings and implications for intervention. Journal of Community Health. 2000;25(3):263–278. doi: 10.1023/a:1005104406934. [DOI] [PubMed] [Google Scholar]
- Bernhardt JM, Mays D, Eroğlu D, Daniel KL. New communication channels: changing the nature of customer engagement. Social Marketing Quarterly. 2009;15(1 suppl):7–15. [Google Scholar]
- Bernhardt JM, Mays D, Kreuter MW. Dissemination 2.0: closing the gap between knowledge and practice with new media and marketing. Journal of Health Communication. 2011;16(sup 1):32–44. doi: 10.1080/10810730.2011.593608. [DOI] [PubMed] [Google Scholar]
- Braunstein JB, Sherber NS, Schulman SP, Ding EL, Powe NR. Race, medical researcher distrust, perceived harm, and willingness to participate in cardiovascular prevention trials. Medicine. 2008;87(1):1–9. doi: 10.1097/MD.0b013e3181625d78. [DOI] [PubMed] [Google Scholar]
- Briss P, Rimer B, Reilley B, Coates RC, Lee NC, Mullen P, et al. Promoting informed decisions about cancer screening in communities and healthcare systems. American Journal of Preventive Medicine. 2004;26(1):67–80. doi: 10.1016/j.amepre.2003.09.012. [DOI] [PubMed] [Google Scholar]
- Bufford RK. Social foundations of thought and action: a social cognitive theory - Bandura, A. Journal of Psychology and Theology. 1986;14(4):341–342. [Google Scholar]
- Bundorf MK, Wagner TH, Singer SJ, Baker LC. Who searches the internet for health information? Health Services Research. 2006;41(3p1):819–836. doi: 10.1111/j.1475-6773.2006.00510.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell MK, James A, Hudson MA, Carr C, Jackson E, Oakes V, et al. Improving multiple behaviors for colorectal cancer prevention among African American church members. Health Psychology. 2004;23(5):492–502. doi: 10.1037/0278-6133.23.5.492. [DOI] [PubMed] [Google Scholar]
- Carter VL, Tippett F, Anderson DL, Tameru B. Increasing prostate cancer screening among African American men. Journal of Health Care for the Poor and Underserved. 2010;21(3):91–106. doi: 10.1353/hpu.0.0366. [DOI] [PubMed] [Google Scholar]
- Cohall AT, Nye A, Moon-Howard J, Kukafka R, Dye B, Vaughan RD, et al. Computer use, internet access, and online health searching among harlem adults. American Journal of Health Promotion. 2011;25(5):325–333. doi: 10.4278/ajhp.090325-QUAN-121. [DOI] [PubMed] [Google Scholar]
- Compeau D, Higgins C. Computer self-efficacy: development of a measure and initial test. Management Information Systems Quarterly. 1995;19(2):189–211. [Google Scholar]
- Cupertino AP, Richter K, Cox LS, Garrett S, Ramirez R, Mujica F, et al. Feasibility of a Spanish/English computerized decision aid to facilitate smoking cessation efforts in underserved communities. Journal of Health Care for the Poor and Underserved. 2010;21(2):504–517. doi: 10.1353/hpu.0.0307. [DOI] [PubMed] [Google Scholar]
- Davis FD, Bagozzi RP, Warshaw PR. Extrinsic and intrinsic motivation to use computers in the workplace. Journal of Applied Social Psychology. 1992;22(14):1111–1132. [Google Scholar]
- Ellison GL, Weinrich SP, Lou M, Xu H, Powell IJ, Baquet CR. A randomized trial comparing web-based decision aids on prostate cancer knowledge for African-American men. Journal of the National Medical Association. 2008;100(10):1139. doi: 10.1016/s0027-9684(15)31481-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans R, Joseph-Williams N, Edwards A, Newcombe RG, Wright P, Kinnersley P, et al. Supporting informed decision making for prostate specific antigen (PSA) testing on the web: an online randomized controlled trial. Journal of Medical Internet Research. 2010;12(3):e27. doi: 10.2196/jmir.1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbein M, Ajzen I. [Retrieved on June 4, 2012];Belief, attitude, intention, and behavior: An introduction to theory and research. 1979 from http://people.umass.edu/aizen/f&a1975.html.
- Friedman DB, Corwin SJ, Rose ID, Dominick GM. Prostate cancer communication strategies recommended by older African-American men in south carolina: A qualitative analysis. Journal of Cancer Education. 2009;24(3):204–209. doi: 10.1080/08858190902876536. [DOI] [PubMed] [Google Scholar]
- Friedman DB, Johnson KM, Owens O, Thomas T, Dawkins D, Gansauer L, et al. Developing partnerships and recruiting dyads for a prostate cancer informed decision making program: lessons learned from a community-academic-clinical team. Journal of Cancer Education. 2012a;27(2):243–249. doi: 10.1007/s13187-012-0353-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman DB, Thomas T, Owens O, Hebert JR. It takes two to talk about prostate cancer: a qualitative assessment of African American men's and women's cancer communication practices and recommendations. American Journal of Mens Health. 2012b;6(6):472–484. doi: 10.1177/1557988312453478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frosch DL, Bhatnagar V, Tally S, Hamori CJ, Kaplan RM. Internet patient decision support: a randomized controlled trial comparing alternative approaches for men considering prostate cancer screening. Archives of Internal Medicine. 2008;168(4):363–369. doi: 10.1001/archinternmed.2007.111. [DOI] [PubMed] [Google Scholar]
- Gielen A, Mckenzie L, Mcdonald E, Shields W, Wang M, Cheng Y, et al. Using a computer kiosk to promote child safety: results of a randomized, controlled trial in an urban pediatric emergency department. Pediatrics. 2007;120(2):330–339. doi: 10.1542/peds.2006-2703. [DOI] [PubMed] [Google Scholar]
- Glaser BG, Strauss A. The Discovery of Grounded Theory: Strategies for Qualitative Research. New York: Aldine de Gruyter; 1967. [Google Scholar]
- Hassinger JP, Holubar SD, Pendlimari R, Dozois EJ, Larson DW, Cima RR. Effectiveness of a multimedia-based educational intervention for improving colon cancer literacy in ccreening colonoscopy patients. Diseases of the Colon and Rectum. 2010;53(9):1301–1307. doi: 10.1007/DCR.0b013e3181e291c0. [DOI] [PubMed] [Google Scholar]
- Holt CL, Wynn TA, Litaker MS, Southward P, Jeames S, Schulz E. A comparison of a spiritually based and non-spiritually based educational intervention for informed decision making for prostate cancer screening among church-attending African-American men. Urologic Nursing. 2009;29(4):249–258. [PMC free article] [PubMed] [Google Scholar]
- Huang H, Coker AD. Examining issues affecting African American participation in research studies. Journal of Black Studies. 2010;40(4):619–636. [Google Scholar]
- Ilic D, Egberts K, Mckenzie JE, Risbridger G, Green S. Informing men about prostate cancer screening: a randomized controlled trial of patient education materials. Journal of General Internal Medicine. 2008;23(4):466–471. doi: 10.1007/s11606-007-0466-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Informed Medical Decisions Foundation. Informed Medical Decisions Foundation: Advancing Shared Decision Making. 2012 [Google Scholar]
- Institute of Medicine, Committee on Health Literacy, & Board of Neuroscience and Behavioral Health. Health Literacy: A Prescription to End Confusion. Washington, District of Columbia: The National Academies Press; 2004. [Google Scholar]
- Kassan EC, Williams RM, Kelly SP, Barry SA, Penek S, Fishman MB, et al. Men's use of an internet-based decision aid for prostate cancer screening. Journal of Health Communication. 2012;17(6):677–697. doi: 10.1080/10810730.2011.579688. [DOI] [PubMed] [Google Scholar]
- Kilbridge KL, Fraser G, Krahn M, Nelson EM, Conaway M, Bashore R, et al. Lack of comprehension of common prostate cancer terms in an underserved population. Journal of Clinical Oncology. 2009;27(12):2015–2021. doi: 10.1200/JCO.2008.17.3468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krist AH, Woolf SH, Johnson RE, Kerns JW. Patient education on prostate cancer screening and involvement in decision making. Annals of Family Medicine. 2007;5(2):112–119. doi: 10.1370/afm.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindblom K, Gregory T, Wilson C, Flight IHK, Zajac I. The impact of computer self-efficacy, computer anxiety, and perceived usability and acceptability on the efficacy of a decision support tool for colorectal cancer screening. Journal of the American Medical Informatics Association. 2011;19(3):407–412. doi: 10.1136/amiajnl-2011-000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisetti C. 10 advantages of using avatars in patient-centered computer-based interventions for behavior change. ACM SIGHIT Record. 2012;2(1):28. [Google Scholar]
- Lisetti C, Yasavur U, De Leon C, Amini R, Rishe N, Visser U. Building an on-demand avatar-based health intervention for behavior change; Paper presented at the Proceedings of the 25th International FLAIRS Conference; Marco Island, USA. 2012. [Google Scholar]
- Lovell BL, Lee RT, Brotheridge CM. Physician communication: barriers to achieving shared understanding and shared decision making with patients. Journal of Participation in Medicine. 2010;2:e12. [Google Scholar]
- Mayer RE, Moreno R. Nine ways to reduce cognitive load in multimedia learning. Educational Psychologist. 2003;38(1):43–52. [Google Scholar]
- Miller DP, Spangler JG, Case LD, Goff DC, Jr, Singh S, Pignone MP. Effectiveness of a web-based colorectal cancer screening patient decision aid: a randomized controlled trial in a mixed-literacy population. American Journal of Preventive Medicine. 2011;40(6):608–615. doi: 10.1016/j.amepre.2011.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitka M. Urology group: prostate screening should be offered beginning at age 40. Journal of the American Medical Association. 2009;301(24):2538–2539. doi: 10.1001/jama.2009.868. [DOI] [PubMed] [Google Scholar]
- Moore AD, Knafl GJ, Hamilton JB, Godley PA, Carpenter WR, Bensen JT, Mishel M. The influence of mistrust, racism, religious participation, and access to care on patient satisfaction for African-American men: The North Carolina-Louisiana Prostate Project (PCaP) Journal of the National Medical Association. 2013;105(1):59. doi: 10.1016/s0027-9684(15)30086-9. [DOI] [PubMed] [Google Scholar]
- Morse J, Field PA. Qualitative research methods for health professionals. 2nd edn. Thousand Oaks, CA: Sage; 1995. [Google Scholar]
- National Medical Association. [Retrieved March 21, 2012];Statement on Prostate Specific Antigen: National Medical Association’s Urology Section’s Experts. 2011 from http://www.prlog.org/11725950-statement-on-prostate-specific-antigen-national-medical-associations-urology-sections-experts.html.
- Neuendorf KA. The Content Analysis Guidebook: SAGE Publications. 2002 [Google Scholar]
- Paas F, Sweller J. An Evolutionary upgrade of cognitive load theory: using the human motor system and collaboration to support the learning of complex cognitive tasks. Educational Psychology Review. 2012;24(1):27–45. [Google Scholar]
- Palmer RC, Midgette LA, Dankwa I. Colorectal cancer screening and African Americans: findings from a qualitative study. Cancer Control. 2008;15(1):72–79. doi: 10.1177/107327480801500109. [DOI] [PubMed] [Google Scholar]
- Patton MQ. Qualitative Evaluation and Research Methods. Newbury Park, CA: Sage Publications; 1990. [Google Scholar]
- Peek ME, Wilson SC, Gorawara-Bhat R, Odoms-Young A, Quinn MT, Chin MH. Barriers and facilitators to shared decision-making among African-Americans with diabetes. Journal of general internal medicine. 2009;24(10):1135–1139. doi: 10.1007/s11606-009-1047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Internet & American Life Project. [Retrieved December 28, 2012];Cell Phone Activities 2012. 2012a from http://pewinternet.org/~/media//Files/Reports/2012/PIP_CellActivities_11.25.pdf.
- Pew Internet & American Life Project. [Retrieved July 5, 2012];A Closer Look at Gadget Ownership. 2012b from http://www.pewinternet.org/2012/06/28/a-closer-look-at-gadget-ownership/
- Pew Internet and American Life Project. [Retrieved October 23, 2013];Mobile. 2013a from http://www.pewinternet.org/Commentary/2012/February/Pew-Internet-Mobile.aspx.
- Pew Internet & American Life Project. [Retrieved January 12, 2013];Health Online 2013. 2013b from http://pewinternet.org/~/media//Files/Reports/2013/Pew%20Internet%20Health%20Online%20report.pdf.
- Pew Internet & American Life Project. [Retrieved Septermber 25, 2013];Home Broadband 2013. 2013c from http://www.pewinternet.org/2013/08/26/home-broadband-2013/
- Pew Internet and American Life Project. [Retrieved February 11, 2011];Americans' pursuit of health takes place within a widening network of both online and offline sources. 2009a from http://pewinternet.org/Reports/2009/8-The-Social-Life-of-Health-Information.aspx.
- Pew Internet and American Life Project. [Retrieved February 11, 2011];Generations Online in 2009. 2009b from http://pewinternet.org/Reports/2009/8-The-Social-Life-of-Health-Information.aspx.
- Porter SC, Cai Z, Gribbons W, Goldmann DA, Kohane IS. The asthma kiosk: A patient-centered technology for collaborative decision support in the emergency department. Journal of the American Medical Informatics Association. 2004;11(6):458–467. doi: 10.1197/jamia.M1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qsr. NVivo 9. Version 9th. Melbourne, AU: Qualitative Solutions and Research Pty Ltd; 2010. [Google Scholar]
- Rains SA. Perceptions of traditional information sources and use of the world wide web to seek healthinformation: findings from the health information national trends survey. Journal of Health Communication. 2007;12(7):667–680. doi: 10.1080/10810730701619992. [DOI] [PubMed] [Google Scholar]
- Resnicow K, Jackson A, Blissett D, Wang T, Mccarty F, Rahotep S, et al. Results of the healthy body healthy spirit trial. Health Psychology. 2005;24(4):339–348. doi: 10.1037/0278-6133.24.4.339. [DOI] [PubMed] [Google Scholar]
- Rimer BK, Briss PA, Zeller PK, Chan ECY, Woolf SH. Informed decision making: what is its role in cancer screening? Cancer. 2004;101(S5):1214–1228. doi: 10.1002/cncr.20512. [DOI] [PubMed] [Google Scholar]
- Rogers E. Diffusion of Innovations. 5th Edition. Free Press; 2003. [Google Scholar]
- Ross L, Dark T, Orom H, Underwood W, Anderson-Lewis C, Iii, Johnson J, et al. Patterns of information behavior and prostate cancer knowledge among African-American men. Journal of Cancer Education. 2011;26(4):708–716. doi: 10.1007/s13187-011-0241-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryhänen AM, Siekkinen M, Rankinen S, Korvenranta H, Leino-Kilpi H. The effects of Internet or interactive computer-based patient education in the field of breast cancer: A systematic literature review. Patient Education and Counseling. 2010;79(1):5–13. doi: 10.1016/j.pec.2009.08.005. [DOI] [PubMed] [Google Scholar]
- Sanchez MA, Bowen DJ, Hart A, Spigner C. Factors influencing prostate cancer screening decisions among African American men. Ethnicity and Disease. 2007;17(2):374. [PubMed] [Google Scholar]
- Schroder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V, et al. Screening and prostate-cancer mortality in a randomized European study. New England Journal of Medicine. 2009;360(13):1320–1328. doi: 10.1056/NEJMoa0810084. [DOI] [PubMed] [Google Scholar]
- Schroy PC, Mylvaganam S, Davidson P. Provider perspectives on the utility of a colorectal cancer screening decision aid for facilitating shared decision making. Health Expectations. 2011 doi: 10.1111/j.1369-7625.2011.00730.x. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulman D, Bickmore T, Sidner C. An intelligent conversational agent for promoting long-term health behavior change using motivational interviewing; Paper presented at the AAAI Spring Symposium on AI and Health Communication.2011. [Google Scholar]
- Seidman I. Interviewing as qualitative research: a guide for researchers in education and the social sciences. New York, NY: Teachers College Press; 1998. [Google Scholar]
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA: A Cancer Journal for Clinicians. 2012;62(1):10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- Smith RA, Cokkinides V, Brawley OW. Cancer screening in the United States, 2012: A review of current American Cancer Society guidelines and current issues in cancer screening. CA: A Cancer Journal for Clinicians. 2012;62:129–142. doi: 10.3322/caac.20143. [DOI] [PubMed] [Google Scholar]
- Spss Inc. SPSS (Version 20) Chicago, IL: 2012. [Google Scholar]
- Strauss A, Corbin J. Basics of qualitative research: techniques and procedures for developing grounded theory. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- Struve D, Wandke H. Video modeling for training older adults to use new technologies. Association for Computing Machiery: Transactions on Accessible Computing. 2009;2(1):1–24. [Google Scholar]
- Taylor S, Todd PA. Understanding information technology usage: A test of competing models. Information Systems Research. 1995;6(2):144. [Google Scholar]
- Thompson DA, Lozano P, Christakis DA. Parent use of touchscreen computer kiosks for child health promotion in community settings. Pediatrics. 2007;119(3):427–434. doi: 10.1542/peds.2006-2669. [DOI] [PubMed] [Google Scholar]
- Thompson RL, Higgins CA, Howell JM. Personal computing: toward a conceptual model of utilization. Management Information Systems Quarterly. 1991;15(1):125–143. [Google Scholar]
- U.S. Cancer Statistics Working Group. United States Cancer Statistics (USCS) Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and National Cancer Institute; 2013. [Google Scholar]
- U.S. Preventive Services Task Force. [Retrieved September 23rd, 2012];Screening for Prostate Cancer: U.S. Preventive Services Task Force Recommendation Statement. 2011 from http://www.uspreventiveservicestaskforce.org/prostatecancerscreening.htm.
- Us Too International. [Retrieved March 22, 2012];Us TOO International Prostate Cancer Education & Support: Special News for African American Men. 2011 from http://www.ustoo.org/Special_News.asp.
- Van Gerven P, Paas F, Tabbers H. Cognitive aging and computer-based instructional design: where do we go from here? Educational Psychology Review. 2006;18(2):141–157. [Google Scholar]
- Van Weert JCM, Van Noort G, Bol N, Van Dijk L, Tates K, Jansen J. Tailored information for cancer patients on the Internet: effects of visual cues and language complexity on information recall and satisfaction. Patient Education and Counseling. 2011;84(3):368–378. doi: 10.1016/j.pec.2011.04.006. [DOI] [PubMed] [Google Scholar]
- Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. Management Information Systems Quarterly. 2003;27(3):425–478. [Google Scholar]
- Vesey GA. A successful strategy for recruitment and retention of Black elders in applied research. Journal of Aging and Health. 2002;16(5):9S–17S. doi: 10.1177/0898264304268146. [DOI] [PubMed] [Google Scholar]
- Volk RJ, Hawley ST, Kneuper S, Holden EW, Stroud LA, Cooper CP, Pavlik VN. Trials of decision aids for prostate cancer screening: a systematic review. American journal of preventive medicine. 2007;33(5):428–434. doi: 10.1016/j.amepre.2007.07.030. [DOI] [PubMed] [Google Scholar]
- Wakefield CE, Watts KJ, Meiser B, Sansom-Daly U, Barratt A, Mann GJ, et al. Development and pilot testing of an online screening decision aid for men with a family history of prostate cancer. Patient Education and Counseling. 2011;83(1):64–72. doi: 10.1016/j.pec.2010.05.025. [DOI] [PubMed] [Google Scholar]
- Welch HG, Albertsen PC. Prostate cancer diagnosis and treatment after the introduction of prostate-specific antigen screening: 1986–2005. Journal of the National Cancer Institute. 2009;101(19):1325–1329. doi: 10.1093/jnci/djp278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson EA, Wolf MS. Working memory and the design of health materials: A cognitive factors perspective. Patient Education and Counseling. 2009;74(3):318–322. doi: 10.1016/j.pec.2008.11.005. [DOI] [PubMed] [Google Scholar]
- Woods VD, Montgomery SB, Herring RP, Gardner RW, Stokols D. Social ecological predictors of prostate-specific antigen blood test and digital rectal examination in black American men. Journal of the National Medical Association. 2006;98(4):492. [PMC free article] [PubMed] [Google Scholar]
- Xie B, Yeh T, Walsh G, Watkins I, Huang M. Co-designing an e-health tutorial for older adults; Paper presented at the Proceedings of the 2012 iConference; Toronto, Ontario, Canada: 2012. [Google Scholar]