Abstract
Background
Catheter ablation (CA) for atrial fibrillation (AF) is now an important therapeutic modality for patients with AF. However, data regarding changes in left atrial (LA) function after CA have indicated conflicting results depending on the AF types, follow-up period, and the analytical imaging tools. The objective of this review was to analyze the effect of CA on the LA size and function for patients with AF.
Methods
We searched for studies regarding LA size and function pre- and post-ablation in PubMed, Embase, the Cochrane Library, and Web of Knowledge through May 2014. LA function was measured by LA ejective fraction (LAEF), LA active ejective fraction (LAAEF), or both. Total and subgroup analyses were implemented using Cochrane Review Manager Version 5.2. Weighted mean differences with 95% confidence intervals were used to express the results of continuous outcomes using fixed or random effect models. I2 was used to calculate heterogeneity. To assess publication bias, Egger’s test and Begg’s funnel plot were performed using Stata 12.0.
Results
Twenty-five studies (2040 enrolled patients) were selected for this meta-analysis. The LA diameter (LAD), maximum LA volume, and minimal LA volume were significantly decreased post-ablation, as compared with those at a pre-ablation visit. Compared with the pre-ablation outcomes, we found no significant differences in LAEF/LAAEF at a post-ablation follow-up. Decreases in LA volume and LAEF remained significant post-ablation for paroxysmal AF (PAF); however, the LAEF was insignificant changes in persistent AF (PeAF). Heterogeneity was significant in spite which individual study was excluded. A publication bias was not found. In a meta-regression analysis, we did not find any factor that contributed to the heterogeneity.
Conclusion
With CA, LA volumes and LAD were decreased significantly in patients with AF; LAEF was not significant changes in patients with PeAF but decreased in those with PAF.
Introduction
Atrial fibrillation (AF) is the most commonly sustained tachyarrhythmia in clinical practice. It is associated with an increase in disease-related hospitalizations; a reduction in quality of life; complications such as congestive heart failure (HF), thromboembolism, and stroke; and an increased mortality risk [1–4]. Catheter ablation (CA) is considered an efficient mainstream therapy and potentially curative treatment for drug-refractory symptomatic AF [5, 6]. After successful ablation, patients with AF would experience improved left atrial (LA) function because of a reduction in AF burden. Nevertheless, it is noted that extensive atrial scar tissue formation produced by CA may result in adverse reactions in atrial function in AF patients. Although Jeevanantham et al. [7] reported successful CA for AF patients does not appear to adversely impact LA function, recent studies that investigated the impact of CA on LA function reported inconsistent results. Therefore, the purpose of this study was to update evidence regarding the effect of CA on the LA size and function in patients with AF.
Methods
Search Strategy
We performed a search for articles pertaining to CA in AF patients using the key words “atrial fibrillation,” “catheter ablation,” “atrial size,” “left atrial function,” and “left atrium function.” We searched for all relevant studies, without any language limitations, in PubMed, Embase, the Cochrane Library, and Web of Knowledge through May 2014. Manual searches were also performed of the bibliographies.
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (1) randomized control trials (RCTs) or nonrandomized control trials were included; (2) follow-up imaging was performed no less than 3 months post-ablation; (3) primary outcome measurements changed regarding maximum LA volume (LAVmax), minimum LA volume (LAVmin), LA diameter (LAD), LA ejection fraction (LAEF; LAEF = [LAVmax − LAVmin]/LAVmax), LA active emptying fraction (LAAEF; LAAEF = {LA mid-diastolic volume just before atrial contraction [LAVmid]–LAVmin}/LAVmid), A wave velocity (A; defined as the peak velocities of late transmitral flow measured by pulsed-wave Doppler echocardiography [DE]), and the A' wave velocity (A'; defined as the velocities of the mitral annulus during atrial contraction as measured by pulsed-wave tissue Doppler echocardiography [TDE]) [8].
Exclusion criteria were as follows: (1) surgical ablation; (2) left ventricular ejection fraction (LVEF) of <50% or included HF patients in each enrolled study; (3) significant valvular disease including a stenotic valvular lesion or moderate-to-heavy regurgitation after valvular replacement; (4) heart dysfunction was caused by structural heart disease or another disease; (5) the LA parameters, as detailed previously, were not reported either pre- or post-ablation; and (6) median and inter-quartile range outcomes were reported.
Data Extraction and Quality Evaluation
Two reviewers (Xiong and Li) assessed the quality of each study and then independently extracted data from the included studies; another author (Wang) checked the data. The extracted information were: (1) basic information regarding those studies, including country and publication year; (2) the number of patients in the study; (3) patient characteristics; (4) type of catheter ablation performed for the treatment group; and (5) outcome measures, as previously defined. Any disagreement was resolved by discussion with a third party (Wang).
To evaluate the quality of the included studies, the following aspects had been performed, including (1) research design; (2) the representativeness of the enrolled patients; (3) the bias of loss to follow-up; and (4) other biases and limitations.
Statistical Analysis
Cochrane Review Manager Version 5.2 and Stata 12.0 were used to perform the statistical analysis. Weighted mean differences (WMDs) with 95% confidence intervals (CIs) were used for expressing continuous outcomes. Statistical heterogeneity was tested using the χ2 test and was quantified using the I2 statistic; significant heterogeneity was defined as a P of <0.10 or an I2 of >50%. Data were pooled using a fixed effect or random effect model, based on whether the absence of significant heterogeneity existed. If the absence of heterogeneity was significant, the fixed effect model was performed, but if not, the random effect model was performed. Publication bias was evaluated using Egger’s test and Begg’s funnel plot with Stata 12.0; statistical significance was defined as a P of <0.05.
Results
Study Characteristics
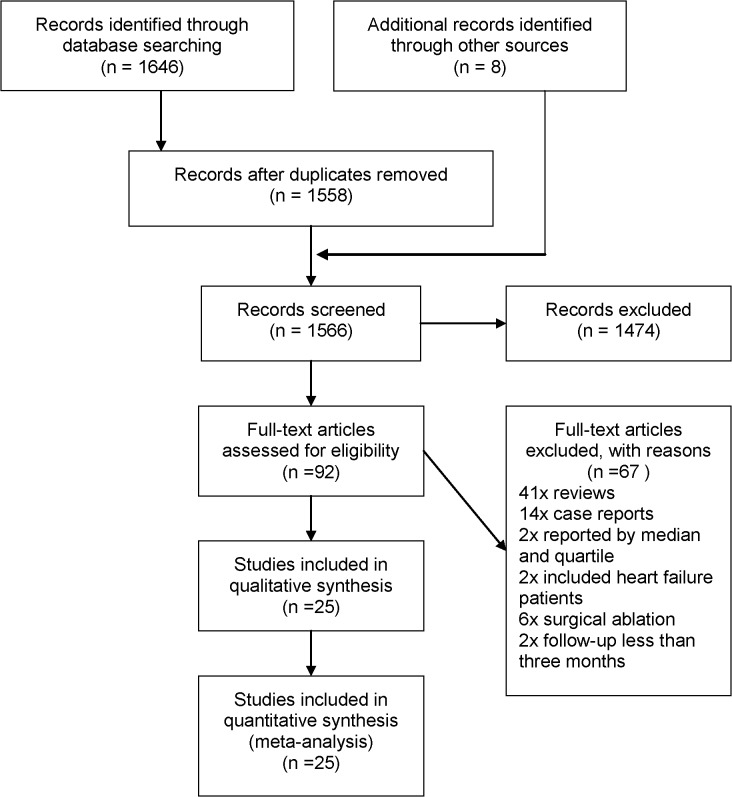
We identified 1566 references from electronic databases using the previously described strategy. According to the inclusion criteria, 92 citations were retrieved and required further evaluation after screening the title, abstract, or both. Forty-one reviews and 14 case reports were excluded. Two studies reported median and inter-quartile range outcomes; 6 studies included surgical ablation; 2 studies had a follow-up of <3 months; and 2 studies included HF patients. Finally, 25 studies (2040 enrolled patients) were selected for this meta-analysis [9–33]. The selection process is demonstrated in a flow chart (Fig 1). The characteristics of each included study are listed in Table 1. The primary results of each included study are shown in Table 2.
Fig 1. Flow chart of the literature search and study selection processes.
Table 1. Characteristics of the studies included in the current review.
| Study | Area | Number of Patients | Age (yrs) | Men | Paroxysmal AF Persistent AF Permanent AF | Follow-Up (mon) | Duration of AF | Comorbidities | Medications | Type of Ablation | Type of Imaging | LVEF (%) | Patients with Recurrence | Success Rate |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dagres [9] | Greece | 289 | 56±9 | 214 | 289 | 12 | 68±58mon | HTN (43%); | NA | PVCA | TTE | 62±10 | 123 | 166/289 |
| 2009 | (74%) | NA | DM (5%); | (57%) | ||||||||||
| NA | CAD (5%) | |||||||||||||
| Erdei [10] | Hungary | 36 | 57±9 | 26 | 36 | 12 | 6.7±7.3yrs | HTN (75%); | AAD | CCA | TTE | 63±5 | 21 | 15/36 |
| 2012 | (72%) | NA | IHD (11%); | (42%) | ||||||||||
| NA | OB (28%) | |||||||||||||
| Hof [11] | Netherlands | 206 | 57±10 | 165 | 114 | 16 | 7±6yrs | HTN (35%); | AAD | PVAI | CMR | NA | 37 | 169/206 |
| 2013 | (80%) | 92 | IHD (10%) | (Class I and III) | (82%) | |||||||||
| NA | ||||||||||||||
| Jahnke [12] | Germany | 41 | 57±10 | 28 | 25 | 12 | NA | HTN (66%); | NA | PVI | CMR | 58±5 | 10 | 31/41 |
| 2011 | (68%) | 16 | DM (5%); | (76%) | ||||||||||
| NA | CAD (20%); | |||||||||||||
| HLP (59%) | ||||||||||||||
| Machino- | Japan | 123 | 60±9 | 104 | NA | 18 | 5.2±4.3yrs | HTN (56%); | AAD | PVI | TTE | NA | 45 | 78/123 |
| Ohtsuka[13] | (85%) | 123 | DM (7%); | (63%) | ||||||||||
| 2013 | NA | CAD (6%) | ||||||||||||
| Masuda [14] | Japan | 115 | 62±10 | 82 | 92 | 3 | 44.6±51.9mon | HTN (50%); | AAD | PVCA | MDCT | 67±7 | 32 | 83/115 |
| 2012 | (71%) | 23 | DM (13%) | (72%) | ||||||||||
| NA | ||||||||||||||
| Montserrat | Spain | 158 | 53±11 | 120 | 77 | 6 | 52±34mon | HTN (44%) | AAD | RFCA | TTE | 59±9 | 82 | 76/158 |
| [15] 2011 | (76%) | 77 | (48%) | |||||||||||
| NA | ||||||||||||||
| Nori [16] | America | 29 | 54±11 | 18 | 16 | 3 | 4.1±3.4yrs* | HTN (48%); | NA | PVAI | CMR | 63±11* | NA | NA |
| 2009 | (62%) | 13 | 2.0±1.0yrs# | DM (17%); | 60±10# | |||||||||
| NA | CAD (38%); | |||||||||||||
| HLP (55%) | ||||||||||||||
| Rodrigues | Brazil | 28 | 53±13 | 22 | 28 | 8 | 6 yrs | HTN (39%) | Amiodarone; | PVCA | TTE | NA | 11 | 17/28 |
| [17] 2009 | (79%) | NA | (3mon-20yrs) | Propafenone; | (61%) | |||||||||
| NA | β-blocker | |||||||||||||
| Teh [18] | Australia | 11 | 59±8 | 8 | 7 | 10 | 5.6±4.8yrs | NA | NA | RFCA | TTE | 60±7 | NA | NA |
| 2012 | (73%) | 4 | ||||||||||||
| NA | ||||||||||||||
| Tops [19] | Netherlands | 148 | 54±9 | 117 | 112 | 13 | 5.3±4.5yrs | HTN (42%); | AAD; | PVI | TTE | 57±7 | 49 | 99/148 |
| 2011 | (79%) | 36 | CAD (6%) | ACEI (49%) | (67%) | |||||||||
| NA | ||||||||||||||
| Yoshida [20] | Japan | 67 | 64±8 | 58 | 34 | 6 | NA | NA | NA | PVI | TTE | NA | 11 | 56/67 |
| 2013 | (87%) | 33 | (84%) | |||||||||||
| NA | ||||||||||||||
| Reant [24] | France | 48 | 53±9* | 40 | 37 | 11 | 6±5yrs* | NA | β-blocker (29%); | PVI | TTE | 62±5* | 13 | 35/48 |
| 2005 | 55±11& | (83%) | NA | 12±9yrs& | Amiodarone(2%); | 53±8& | (73%) | |||||||
| 11& | Flecainide (14%) | |||||||||||||
| Delgado | Spain | 34 | 53±13 | 24 | 23 | 6 | 90±72mon | HTN (24%) | AAD | CPVA | 3D-TTE | NA | 13 | 21/34 |
| [29] 2008 | (70%) | 6 | (62%) | |||||||||||
| 5 | ||||||||||||||
| Verma [27] | America | 67 | 56±10 | 49 | 40 | 6 | 5.8±5.1yrs | HTN (31%); | AAD | PVAI | TTE, | 50±13 | NA | NA |
| 2006 | (73%) | 27 | DM (9%); | CT | ||||||||||
| NA | CAD (19%); | |||||||||||||
| VHD (15%) | ||||||||||||||
| Lemola [23] | America | 36 | 55±11 | 24 | 27 | 5 | 5±4yrs | CAD (9%) | NA | LACA | CT | 56±5 | NA | NA |
| 2005 | (67%) | NA | ||||||||||||
| 9& | ||||||||||||||
| Perea [33] | Spain | 55 | 52±11 | 44 | 41 | 12 | 8.4±8yrs | HTN (22%); | AAD | CPVA | CMR | 60±9 | 17 | 38/55 |
| 2008 | (80%) | 14 | SHD (16%) | (69%) | ||||||||||
| NA | ||||||||||||||
| Muller [32] | Switzerland | 91 | 59±8 | 79 | 72 | 6 | 6.4±5.8yrs | HTN (33%); | ACEI and/or ARB(30%); | PVI | TTE | NA | 21 | 70/91 |
| 2008 | (87%) | 11 | IHD (7%) | Diuretic (15%); | (77%) | |||||||||
| 8 | Amiodarone (24%); | |||||||||||||
| Sotalol (12%); | ||||||||||||||
| Ic (31%); | ||||||||||||||
| β-blocker (43%) | ||||||||||||||
| Marsan [31] | Netherlands | 57 | 56±9 | 44 | 43 | 8 | 4.6±4.1yrs | HTN (44%); | Amiodarone; | RFCA | 3D-TTE | 57±9 | 19 | 38/57 |
| 2008 | (77%) | 14 | DM (11%); | Propafenone; | (67%) | |||||||||
| NA | CAD (5%) | Flecainide; | ||||||||||||
| Sotalol; | ||||||||||||||
| ACEI and/or ARBs(46%) | ||||||||||||||
| Beukema | Netherlands | 105 | 53±10 | 88 | 52 | 15 | 6±5.1yrs* | HTN (26%); | AAD | PVI | TTE | 54±4 | 34 | 71/105 |
| [22] 2005 | (84%) | 53 | 7.6±6yrs# | DM (5%) | (68%) | |||||||||
| NA | ||||||||||||||
| Choi [28] | Korea | 33 | 56±10 | 27 | 21 | 3 | 63±47mon | HTN (21%); | ACEI or ARB (24%); | RFCA | TTE | 53±6 | NA | NA |
| 2008 | (82%) | 12 | DM (6%); | CCB (30%); | ||||||||||
| NA | CAD (6%) | β-blocker (15%); | ||||||||||||
| Amiodarone (30%); | ||||||||||||||
| Propafenone (30%); | ||||||||||||||
| Flecainide (6%) | ||||||||||||||
| Liu [30] | China | 120 | 60±9 | 80 | 120 | 12 | 2.6±1.4yrs | NA | Amiodarone; | CPVA | TTE | 67±3 | 42 | 78/120 |
| 2008 | (83%) | NA | Losartan | SPVI | (65%) | |||||||||
| NA | ||||||||||||||
| Tops [26] | Netherlands | 57 | 53±8 | 45 | 35 | 3 | 6±5yrs | HTN (30%); | AAD | RFCA | TTE | 55±7 | 18 | 39/57 |
| 2006 | (79%) | 18 | CAD (7%); | (68%) | ||||||||||
| 4 | VHD (11%) | |||||||||||||
| Lemola [21] | America | 41 | 54±12 | 33 | 25 | 4 | 5±3yrs | HTN (21%); | NA | LACA | CT | 55±8 | 8 | 33/41 |
| 2004 | (80%) | NA | SHD (41%) | (80%) | ||||||||||
| 16 | ||||||||||||||
| Tsao [25] | China | 45 | 60±13 | 36 | 45 | 21 | NA | NA | AAD | PVI | CMR | NA | 10 | 35/45 |
| 2005 | Taiwan | (80%) | NA | (77%) | ||||||||||
| NA |
* Paroxysmal Atrial Fibrillation
# Persistent Atrial Fibrillation
& Chronic Atrial Fibrillation
NA = Not Available; mon = months; yrs = years
HTN = Hypertension; DM = Diabetes Mellitus; CAD = Coronary Artery Disease; OB = Obesity; IHD = Ischemic Heart Disease; HLP = Hyperlipidemia; VHD = Valvular Heart Disease; SHD = Structural heart disease.
ACEI = Angiotensin Converting Enzyme Inhibitors; ARB = Angiotensin Receptor Blocker; CCB = Calcium-channel Blocker; AAD = Anti-Arrhythmic Drugs.
RFCA = Radiofrequency Catheter Ablation; CCA = Cryoballoon Catheter Ablation; PVI = Pulmonary vein isolation; PVAI = Pulmonary Vein Antrum Isolation; CPVA/PVCA = Circumferential Pulmonary Vein Catheter Ablation; SPVI = Segmental Pulmonary Vein Isolation; LACA = Radiofrequency Left Atrial Circumferential Ablation. CMR = Cardiac Magnetic Resonance Imaging; TTE = Transthoracic Echocardiography; TEE = Transesophageal Echocardiography; MDCT = Multidetector Computed Tomography.
Atrial fibrillation recurrence is defined as documented by body surface 12-lead electrocardiogram (ECG) or 24-hour Holter ECG lasting 30 seconds, despite being symptomatic or not, at any time from 3 months after catheter ablation.
Table 2. Primary outcome variables before and after ablation.
| Study | LAD | LAD | LAVmax | LAVmax | LAVmin | LAVmin | LAEF | LAEF | LAAEF | LAAEF | A Wave | A Wave | A' Wave | A' Wave | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-ablation | Post-ablation | Pre-ablation | Post-ablation | Pre-ablation | Post-ablation | Pre-ablation | Post-ablation | Pre-ablation | Post-ablation | Pre-ablation | Post-ablation | Pre-ablation | Post-ablation | ||
| Dagres [9] | 42±6* | 41±5* | NA | NA | NA | NA | NA | NA | NA | NA | 59±23* | 53±12* | NA | NA | |
| 2009 | |||||||||||||||
| Erdei [10] | 54±6(NR) * | 56±5(NR) * | 67±20(NR) * | 69±15(NR) * | 30±12(NR) * | 32±11(NR) * | 55±8(NR) * | 55±9(NR) * | NA | NA | NA | NA | 10.7±2.7(NR) * | 10.8±3.1(NR) * | |
| 2012 | 55±5(R) * | 59±6(R) * | 73±23(R) * | 81±24(R) * | 38±19(R) * | 44±20(R) * | 48±11(R) * | 47±11(R) * | 9.8±2.1(R) * | 10.2±2.7(R) * | |||||
| Hof [11] | NA | NA | 116.6±27.7* | 104.1±25.3* | 62.8±20* | 57.9±18.9* | 43.8±9.3 | 41.2±9.6 | 27.9±9.5 | 25.4±9.5 | NA | NA | NA | NA | |
| 2013 | 135.6±35.9# | 121.5±34.8# | 80.2±32.1# | 73.8±27.1# | |||||||||||
| Jahnke | NA | NA | 98±18(NR) | 83.7±19.3(NR) | 68.2±23.7(NR) | 50.4±18.4(NR) | 31.4±17.3(NR) | 40.7±13.2(NR) | NA | NA | NA | NA | NA | NA | |
| [12] 2011 | 116.7±20.3(R) | 108±19.8(R) | 80.2±24.9(R) | 71.3±23.8(R) | 31.8±15.2(R) | 34.9±13.9(R) | |||||||||
| Machino- | NA | NA | 48±25(NR) # | 34±16(NR) # | 40±19(NR) # | 23±12(NR) # | 24±17(NR) # | 36±14 NR) # | NA | NA | 54±12# | 63±19# | NA | NA | |
| Ohtsuka | 57±23(R) # | 59±22(R) # | 47±16(R) # | 49±20(R) # | 21±16(R) # | 17±14(R) # | |||||||||
| [13] 2013 | |||||||||||||||
| Masuda | NA | NA | 57.3±17.7* | 53.2±14.9* | NA | NA | 47.4±11.8* | 44.9±10.6* | NA | NA | NA | NA | NA | NA | |
| [14] 2012 | 65.8±28.4# | 53.4±22.8# | 32.7±11.4# | 39.1±11.5# | |||||||||||
| Montserrat | 42±6* | 41±6* | 53±16* | 47±15* | 30±12* | 28±11* | 44±16* | 40±13* | 37±23* | 44±25* | NA | NA | NA | NA | |
| [15] 2011 | 44±6# | 43±5# | 64±20# | 56±18# | 46±18# | 39±16# | 28±16# | 31±17# | |||||||
| Nori [16] | NA | NA | 37±6.4* | 28.5±5.9* | 19.7±5.7* | 16.3±5.9* | 47.3±10.1* | 42.7±9.4* | 33.4±8.3* | 26.2±7.9* | NA | NA | NA | NA | |
| 2009 | 41.4±8.7# | 36.7±10# | 31.7±9.3# | 24±8.8# | 24.1±11.8# | 34.8±10.2# | |||||||||
| Rodrigues | 41±7* | 40±6* | 56±21(NR)* | 58±20(NR)* | 30±15* | 34±15* | 47±8* | 43±8* | NA | NA | 55±15* | 58±19* | 7.9±2.3* | 8.1±2.8* | |
| [17] 2009 | 53±14(R)* | 57±20(R)* | |||||||||||||
| Teh [18] | 45±7 | 42±6 | 76±30 | 63±23 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| 2012 | |||||||||||||||
| Tops [19] | 43±4 | 40±4 | 31±7 | 21±6 | 19±6 | 12±5 | 41±14 | 46±11 | NA | NA | NA | NA | NA | NA | |
| 2011 | |||||||||||||||
| Yoshida | 38±7* | 40±8* | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| [20] 2013 | 41±6# | 40±8# | |||||||||||||
| Reant [24] | 59.7±7.3* | 53.19±7.7* | NA | NA | NA | NA | NA | NA | 30.9±13.5* | 34±11.3* | NA | NA | NA | NA | |
| 2005 | 68.4±8.1& | 60.68±6.5& | 5.4±3.6& | 21.8±11& | |||||||||||
| Delgado | 40±6(NR) | 39±6(NR) | 50±11(NR) | 45±10(NR) | 26±13(NR) | 24±8(NR) | 49±19(NR) | 48±18(NR) | 25±21(NR) | 26±21(NR) | 31±27(NR) | 30±26(NR) | NA | NA | |
| [29] 2008 | 42±7(R) | 43±9(R) | 64±19(R) | 53±22(R) | 32±12(R) | 30±15(R) | 49±14(R) | 43±13(R) | 23±19(R) | 18±12(R) | 22±36(R) | 42±16(R) | |||
| Verma [27] | 45.9±10.2 | 44.4±4.5 | 94.5±28.1 | 85.8±18.2 | 78.6±23.8 | 66.8±13.9 | 16.7±5.8 | 22.1±5.4 | NA | NA | 42.8±20.9 | 61.9±17.3 | NA | NA | |
| 2006 | |||||||||||||||
| Lemola | NA | NA | 121±40* | 95±30* | 87±39* | 78±27* | 32±13* | 21±8* | NA | NA | NA | NA | NA | NA | |
| [23] 2005 | |||||||||||||||
| Perea [33] | NA | NA | 98±19.9(NR) | 84.9±17.1(NR) | 58.6±16.1(NR) | 52.2±12.1(NR) | 40.2±11.5(NR) | 38.1±9.8(NR) | NA | NA | NA | NA | NA | NA | |
| 2008 | 126.2±32.8(R) | 103.5±28.1(R) | 78.4±22.2(R) | 75.8±24.3(R) | 37.4±10.1(R) | 26.9±10.2(R) | |||||||||
| Muller [32] | 56±8 | 53±7 | 59.6±21.3 | 51±15.5 | NA | NA | NA | NA | NA | NA | 59.7±20.4 | 59±16.1 | 8.9±2.9 | 9.8±3.4 | |
| 2008 | |||||||||||||||
| Marsan | NA | NA | 26±8(NR) | 23±7(NR) | 13±5(NR) | 10±4(NR) | 52±10(NR) | 58±10(NR) | 22±8(NR) | 33±9(NR) | NA | NA | NA | NA | |
| [31] 2008 | 31±8(R) | 32±8(R) | 16±7(R) | 18±6(R) | 47±13(R) | 42±11(R) | 24±7(R) | 15±9(R) | |||||||
| Beukema | 40.5±4.4(NR) * | 37.5±3.5(NR) * | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| [22] 2005 | 44±5.8(NR) # | 40±4.5(NR) # | |||||||||||||
| 45±6.5(R) # | 49±5.4(R) # | ||||||||||||||
| Choi [28] | 41±5.4 | 39±6.4 | 63.4±20.7 | 50.7±16.6 | 43.8±18.2 | 35.1±12.9 | 31.8±12.8 | 30.9±10 | NA | NA | 60.7±22.7 | 44.8±16.7 | 9.7±1.9 | 7.6±1.6 | |
| 2008 | |||||||||||||||
| Liu | CPVA | 33.8±3.6(NR) * | 32.2±2.5(NR) * | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| [30] | 34.9±2.8(R) * | 34.1±1.9(R) * | |||||||||||||
| 2008 | SPVI | 34.8±2.8(NR) * | 35±2.4(NR) * | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 35.4±2.7(R) * | 38.4±2.8(R) * | ||||||||||||||
| Tops [26] | 45±3(NR) | 42±3(NR) | 59±12(NR) | 50±11(NR) | 37±9(NR) | 31±7(NR) | NA | NA | NA | NA | NA | NA | NA | NA | |
| 2006 | 45±3(R) | 48±3(R) | 63±7(R) | 68±8(R) | 43±7(R) | 47±7(R) | |||||||||
| Lemola | NA | NA | 115±39(NR) | 97±35(NR) | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| [21] 2004 | 128±80(R) | 135±70(R) | |||||||||||||
| Tsao [25] | 33.5±5.9(NR) * | 32.5±6.9(NR) * | 61.5±19.1(NR) * | 56.6±17.1(NR) * | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| 2005 | 34.1±6.6(R) * | 36.2±6.4(R) * | 61.1±17.5(R) * | 78.7±25.3(R) * | |||||||||||
* Paroxysmal Atrial Fibrillation
# Persistent Atrial Fibrillation
& Chronic Atrial Fibrillation
NR = Not Recurrence; R = Recurrence; NA = Not Available
LAD = left atrial diameter; LAVmax = maximum left atrial volume; LAVmin = minimum left atrial volume; LAEF = left atrial ejective fraction; LAAEf = left atrial active ejective fraction; A wave = A wave velocity; A' wave = A' wave velocity
Other abbreviations and AF Recurrence defined as previously detailed.
All patients had underwent CA, one study [15] had repeated ablation. The majority of studies performed radiofrequency catheter ablation (RFCA), only one study [10] implemented cryoablation. Twelve studies [10, 12, 13, 17, 21, 22, 25, 26, 29–31, 33] had reported changes in LAD, LA volumes, or function on the basis of AF recurrence (AF recurrence defined as documented by body surface 12-lead electrocardiogram (ECG) or 24-hour Holter ECG lasting 30 seconds, despite being symptomatic or not, at any time from 3 months after CA [34]). Liu et al. [30] had compared two different treatment strategies [circumferential pulmonary vein ablation (CPVA) vs. segmental pulmonary vein isolation (SPVI)] on left atrial size in patients with lone paroxysmal AF (PAF). Nineteen studies [11, 12, 14–16, 18–24, 26–29, 31–33] had included patients with paroxysmal or non-paroxysmal AF, five studies [9, 10, 17, 25, 30] only included patients with PAF, one study [13] only included patients with persistent AF (PeAF), six studies [21, 23, 24, 26, 29, 32] included patients with permanent AF (only 49 enrolled patients). There were some co-morbidities including hypertension (HTN), diabetes mellitus (DM), and coronary artery disease (CAD) et al. in the majority of enrolled patients.
Quantitative Data Synthesis
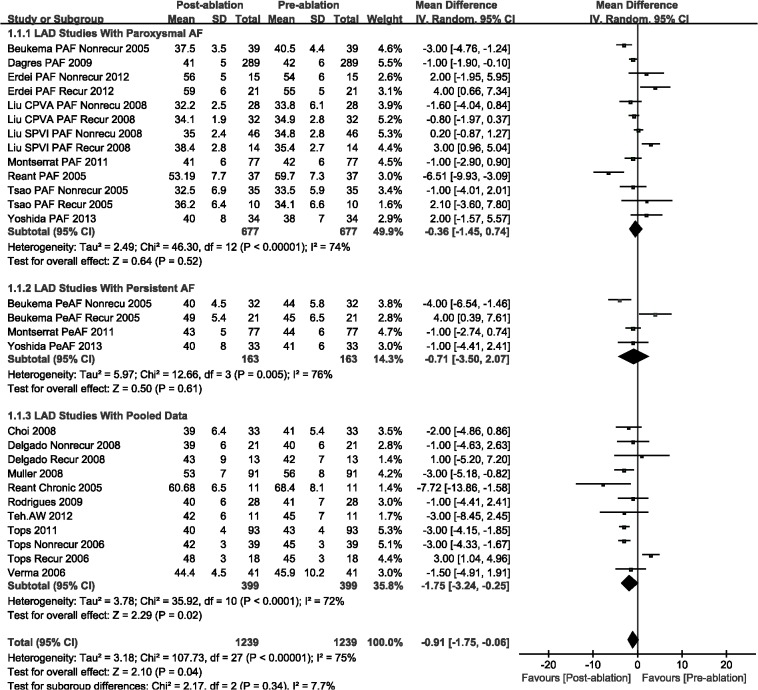
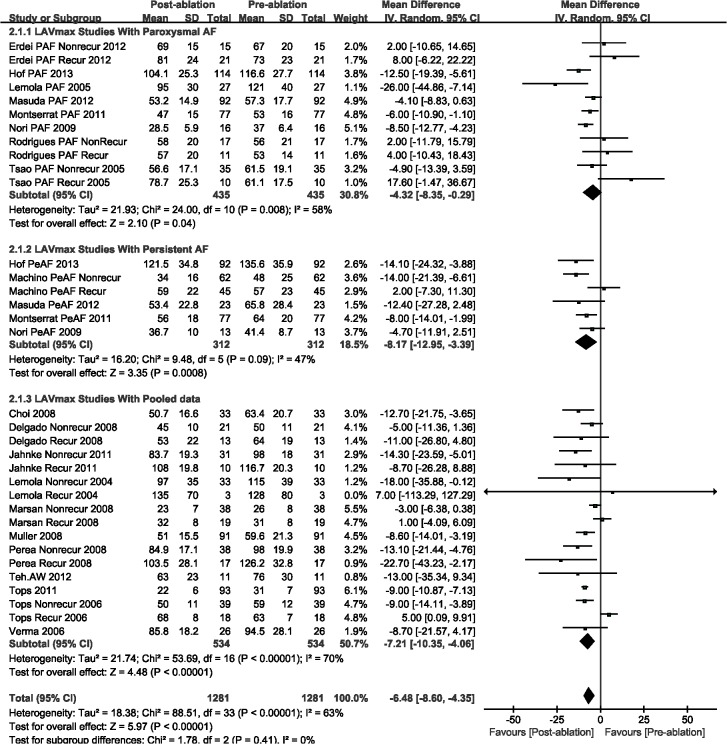
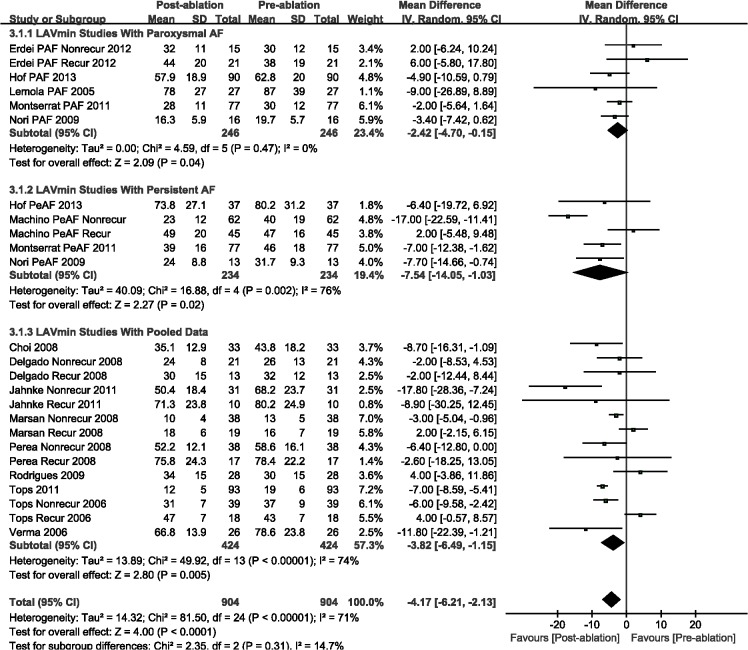
The LAD (WMD, -0.91 mm; 95%CI, from -1.75 mm to -0.06 mm, P = 0.04; Fig 2), LAVmax (WMD, -6.48 mL; 95%CI, from -8.60 mL to -4.35 mL, P < 0.00001; Fig 3), and LAVmin (WMD, -4.17 mL; 95%CI, from -6.21 mL to -2.13 mL, P < 0.0001; Fig 4) were significantly decreased post-ablation, as compared with those pre-ablation. Nevertheless, a subgroup analysis was performed that was based on AF type; there were significant decreases in LA volumes (including LAVmax and LAVmin) for the AF patients. The LAD result indicated insignificant changes for patients with either paroxysmal or persistent AF (Figs 2–4).
Fig 2. A forest plot of comparison: changes in left atrial diameter (LAD) pre-ablation and post-ablation.
Fig 3. A forest plot of comparison: changes in maximum left atrial volume (LAVmax) pre-ablation and post-ablation.
Fig 4. A forest plot of comparison: changes in minimum left atrial volume (LAVmin) pre-ablation and post-ablation.
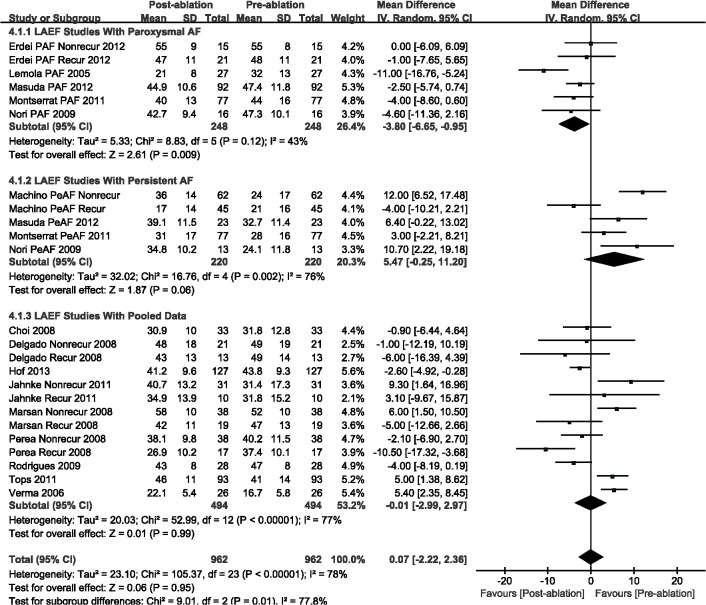
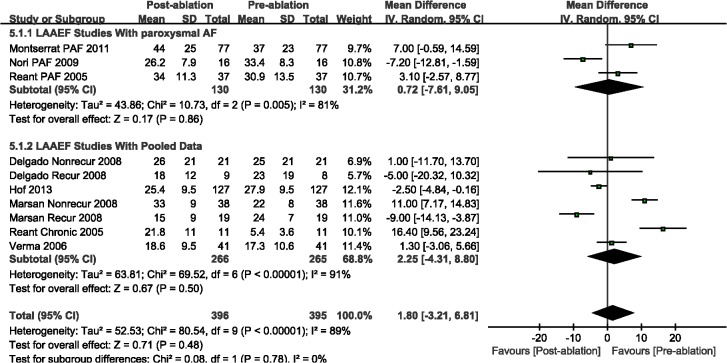
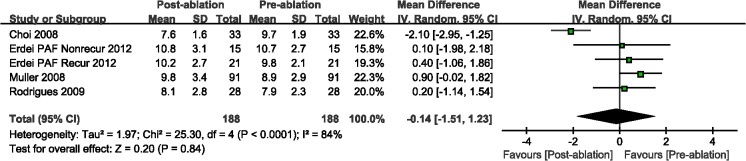
Compared with the pre-ablation outcomes, we found no significant differences in LAEF (WMD, 0.07%; 95%CI, from -2.22% to 2.36%, P = 0.95; Fig 5) and LAAEF (WMD, -1.86%; 95%CI, from -3.92% to 7.63%, P = 0.48; Fig 6). Subsequently, we performed a subgroup analysis based on the AF type, and there were insignificant differences among those studies with either PAF or PeAF, except for LAEF with PAF (WMD, -3.80%; 95%CI, from -6.65% to -0.95%, P = 0.009; Fig 5). Finally, we analyzed the A wave velocity (A) and A' wave velocity (A'), and there were insignificant differences during follow-up imaging for CA treatment, as compared with pre-ablation (Figs 7 and 8).
Fig 5. A forest plot of comparison: changes in left atrial ejective fraction (LAEF) pre-ablation and post-ablation.
Fig 6. A forest plot of comparison: changes in left atrial active ejective fraction (LAAEF) pre-ablation and post-ablation.
Fig 7. A forest plot of comparison: changes in A wave velocity pre-ablation and post-ablation.
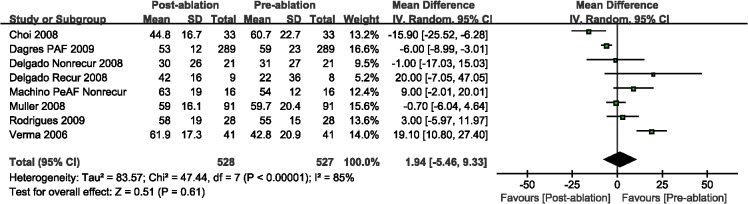
Fig 8. A forest plot of comparison: changes in A´ wave velocity pre-ablation and post-ablation.
Subsequently, we implemented a subgroup analysis on the basis of AF recurrence. There were significant decreased in LAD (WMD, -1.63 mm; 95%CI, from -3.01 mm to -0.24 mm, P = 0.02, S1 Fig), LAVmax (WMD, -7.53 mL; 95%CI, from -11.09 mL to -3.97 mL, P < 0.0001, S2 Fig), and LAVmin (WMD, -6.73 mL; 95%CI, from -11.07 mL to -2.39 mL, P = 0.002, S3 Fig) with no recurrence AF during post-ablation follow-up, but not those with AF recurrence, except for LAD with AF recurrence (WMD, 2.25 mm; 95%CI, from 0.29 mm to 4.21 mm, P = 0.02, S1 Fig). The LAEF (WMD, -4.60%; 95%CI, from -7.91% to -1.29%, P = 0.006, S4 Fig) and LAAEF (WMD, -8.60%; 95%CI, from -13.46% to -3.74%, P = 0.0005, S5 Fig) were decreased significantly in patients with recurrence AF after CA during follow-up, however, there were insignificant changes between those with no recurrence AF.
Heterogeneity Analysis
After performing a heterogeneity test, the existence of heterogeneity among those studies should not be ignored. To demonstrate the origin of the heterogeneity, a meta-regression analysis and sensitivity analysis were performed. Heterogeneity was significant in spite which individual study was excluded. As previously illustrated, a subgroup analysis was performed; each outcome was analyzed based on the AF type (PAF or PeAF). A random effects model was used to combine the effect size because significant heterogeneity was shown as an all-total consequence.
Subsequently, a sensitivity analysis that was on the basis of image modalities, the LAVmax (WMD, -9.31 mL; 95%CI, from -12.45 mL to -6.16 mL, P < 0.00001, S7 Fig) and LAVmin (WMD, -6.07 mL; 95%CI, from -8.49 mL to -3.65 mL, P < 0.00001, S8 Fig) remained significant decreased at post-ablation which detected by cardiac magnetic resonance imaging (CMR) and/or Computed Tomography (CT). However, the LAD (WMD, -0.77 mm; 95%CI, from -2.87 mm to 1.33 mm, P = 0.47, S6 Fig), LAEF (WMD, -0.28%; 95%CI, from -3.91% to 3.35%, P = 0.88, S9 Fig) and LAAEF (WMD, -2.47%; 95%CI, from -6.30% to 1.36%, P = 0.21, S10 Fig) were not significant change during follow-up after catheter ablation treatment. And then, we found that the LAVmax (WMD, -7.08 mL; 95%CI, from -12.52 mL to -1.64 mL, P = 0.01, S7 Fig), LAVmin (WMD, -4.07 mL; 95%CI, from -7.29 mL to -0.84 mL, P = 0.01, S8 Fig) and LAEF (WMD, -5.72%; 95%CI, from -11.02% to -0.42%, P = 0.03, S9 Fig) were significant decrease in PAF; the LAV (LAVmax: WMD, -8.90 mL; 95%CI, from -15.28 mL to -2.53 mL, P = 0.006, S7 Fig; LAVmin: WMD, -7.42 mL; 95%CI, from -13.59 mL to -1.25 mL, P = 0.02, S8 Fig) were decreased significantly in PeAF, however, the LAEF (WMD, 8.03%; 95%CI, from 2.81% to 13.24%, P = 0.003, S9 Fig) was increased significantly in PeAF.
According to a sensitivity analysis that was based on a follow-up of >6 months, there were significant decreases in only LAV after catheter ablation therapy, including LAVmax (WMD, -6.07 mL; 95%CI, from -8.76 mL to -3.38 mL, P < 0.00001, S12 Fig) and LAVmin (WMD, -3.91 mL; 95%CI, from -6.62 mL to -1.20 mL, P = 0.005; S13 Fig). However, the LAD, LAEF, and LAAEF did not significantly change during follow-up after ablation treatment (WMD, -0.81 mm; 95%CI, from -1.68 mm to 0.06 mm, P = 0.07; WMD, 0.05%; 95%CI, from -2.67% to 2.77%, P = 0.97; WMD, 2.89%; 95%CI, from -2.42% to 8.20%, P = 0.29; respectively, S11, S14 and S15 Figs).
A sensitivity analysis was performed based on a follow-up of >12 months. After ablation therapy, the LAVmax (WMD, -7.83 mL; 95%CI, from -11.65 mL to -4.01 mL, P < 0.0001, S17 Fig) and LAVmin (WMD, -5.90 mL; 95%CI, from -9.77 mL to -2.03 mL, P = 0.003, S18 Fig) were significantly decreased; however, the LAD and LAEF did not significantly change (WMD, -0.36 mm; 95%CI, from -1.53 mm to 0.81 mm, P = 0.55; WMD, 0.80%; 95%CI, from -3.03% to 4.63%, P = 0.68; respectively, S16 and S19 Figs).
Subsequently, a meta-regression analysis was performed to determine the heterogeneity origin. However, we did not find any factors that contributed to the heterogeneity.
Publication Bias Analysis
Egger’s test and Begg’s funnel plot were used to evaluate publication bias. There were no significant risks of publication bias according to an analysis using Stata 12.0 (the P value for each test was >0.05; Table 3). The funnel plot was generally symmetrical, and it indicated that the publication bias for the studies was controlled.
Table 3. Assessment of publication bias with Stata 12.0 for each primary outcome.
| Primary Outcome | Begg’s Test (P value) | Egger’s Test (P value) |
|---|---|---|
| LAD | 0.921 | 0.636 |
| LAVmax | 0.767 | 0.832 |
| LAVmin | 0.726 | 0.670 |
| LAEF | 0.785 | 0.948 |
| LAAEF | 1.000 | 0.605 |
| A Wave | 0.536 | 0.205 |
| A' Wave | 0.086 | 0.117 |
Abbreviations as previously detailed.
Discussion
In the present review, we found that the LA volumes and LAD were significantly decreased after CA therapy during follow-up imaging. Nonetheless, we did not find any significant changes in LA function (included LAEF and LAAEF) after ablation treatment during follow-up imaging. Furthermore, there were significant decreases in the LA volumes and LAEF with paroxysmal AF after CA treatment. However, we did not find any significant changes in outcomes, as previously detailed, for persistent AF after ablation therapy, except for LA volumes.
CA is a therapeutic method for terminating the underlying electrophysiological mechanism of AF. The substrate and trigger foci are isolated by freezing (cryoablation) or radiofrequency energy and then terminate the electrical conduction from the pulmonary vein (PV) to LA. Currently, CA is approved by the Food and Drug Administration (FDA) for managing paroxysmal AF. Although this practical strategy is also used for managing non-paroxysmal AF, unfortunately, it is not yet approved by the FDA [2, 35]. The resumption of a sinus rhythm with CA is a perfect consequence, but the amount of LA scarring produced by CA could influence LA structural and functional remodeling, especially with repeated ablation. Structural remodeling includes increasing LA size and a change in LA strain. Several studies [10, 18, 19] reported that the enlargement could be reversed after successful ablation therapy that is defined as the maintenance of a sinus rhythm during follow-up [34]. Thus, LA reverse remodeling may become a robust sign of successful CA for patients with AF. Further studies should be conducted to evaluate the effects on LA function for patients with AF after a repeat ablation treatment.
There was a significant decrease in LAEF after CA treatment in studies with paroxysmal AF; however, we did not find similar outcomes in studies with persistent AF. Rodrigues et al. [17] reported a degradation in LAEF after CA for patients with paroxysmal AF at a follow-up duration of about 8 months after performing transthoracic echocardiography (TTE). Hof et al. [11] found a similar outcome using three-dimensional computed tomography (CT). However, Erdei et al. [10] and Machino-Ohtsuka et al. [13] described that the LAEF was preserved and even increased in patients without an AF recurrence at a follow-up of >12 months; however, it had decreased in AF recurrence patients after TTE and CMR. Why did this phenomenon occur in these studies? Several reasons for this variance should be considered, including the follow-up duration after CA therapy; the chronicity of AF; the different clinical outcomes; and the different degrees of tissue damage related to the different ablation strategies, tools, or both.
More consideration should be given to the follow-up duration regarding studying LA function and size. Studies with a long follow-up (not less than 12 months) [12, 13, 19] have illustrated significant increases in LAEF after ablation treatment in AF patients; however, insignificant changes in LAEF with paroxysmal AF in 3 months follow-up [14, 16]. Further, a sensitivity analysis based on the follow-up duration was not persuasive because of a lack of detailed individual patient data. McGann et al. [36] reported that the quantification and detection of left atrial wall scarring would be applicable 3 months after CA in patients with AF. As we known, there is a phenomenon of atrial “stunning” during in 1 month follow-up after catheter ablation therapy, and either the LA size or the LA function is unstable change. After the “blanking period” (about 3 months), which the rate of recurrence AF is highest [37], the quantification and detection of LA size and function is more credible and accurate. Therefore, it is important that a longer follow-up duration should be performed for evaluating LA function. Moreover, because the LA function was assessed using only the sinus rhythm (SR), it is difficult to evaluate LA function in permanent AF patients.
In addition, the imaging technique is another important factor. Many different methods were performed in the studies, including TTE [9, 10, 13–15, 17–20, 22, 24, 26–32], CMR [11, 12, 16, 25, 33], and CT [14, 21, 23, 27]. As an established method in cardiac imaging modalities, TTE can identify the size of each chamber, as well as the ejection fraction of the LA and left ventricle (LV). However, a limitation occurs if patients are obese and have serious obstructive pulmonary disease with poor acoustic windows [38]. Multidetector Computed Tomography (MDCT) has a prominent temporal and spatial resolution for measuring LA volumes. CMR can concurrently discover pre-ablation fibrosis and post-ablation scar tissue and measure PV anatomy in patients who undergo CA therapy [39]. As we known, different analytical methods or image tools would obtain different results. Compare to TTE, using CMR and CT have a prominent temporal and spatial resolution for measuring LA volumes and EF, the results of CMR or CT should be more accurate than that of TEE. Due to this important issue, we performed subgroup analysis based on the variant methods of image. Subsequently, after excluding studies using TTE, only 9 studies (enrolled 635 patients) [11, 12, 14, 16, 21, 23, 25, 27, 33] were included in the subgroup analysis on the basis of detecting by CMR and/or CT. The LA volumes significantly decreased, LAEF/LAAEF insignificant changed. The explanations for this phenomenon as follow. First, CMR and CT/MDCT are more accuracy and improve reproducibility in measurement of LA volumes and functions compare to TTE. Second, the numbers of included studies were decreased, and then it may influence the pooled data. Therefore, compared with MDCT and CMR, TTE may underestimate the true LA size and function.
Nonetheless, there is no gold standard for measuring LA function. In the present review, the LAEF was used to define LA function in 15 studies [10–17, 19, 23, 27–29, 31, 33], and only 6 studies used LAAEF to define LA function [11, 15, 16, 24, 29, 31]. Furthermore, A wave velocity [9, 13, 17, 27–29, 32] and A' wave velocity [10, 17, 28, 32] were used to define LA contractile function. The A wave velocity involves the peak velocities of the late transmitral flow, as measured by pulsed-wave DE, reflecting LA systolic function from hemodynamics, but it is not sensitive because it can be affected by the LV diastolic function and preload. However, compared with the A wave velocity, the A' wave velocity, as detailed previously, is an easy and effective means to assess LA systolic function from tissue motion because it is correlated with changes in the LA systolic area and volume [8]. Therefore, further studies should be conducted to assess this method for evaluating LA function.
Beyond these, the treatment strategy and energy of catheter ablation are another factor. In this meta-analysis, the majority of included studies were used RFCA, only one study [10] performed cryoablation. As we known, different treatment strategies, such as SPVI and PVAI, lead to different outcomes, and diverse ablation temperature and power resulted in different damages for atrium. The included studies used RFCA were set at a similar value of the ablation temperature and power, and therefore, the results have consistency and comparability. After excluding the study performed cryoablation, there were similar pooled data compare to previous detailed. Due to there was no more available data, further studies should be focused on evaluating the effects on LA function and size for patients with AF after cryoablation treatment.
Heterogeneity is an important issue for explaining the outcomes of this review, and significant heterogeneity was found in this meta-analysis. Subsequently, sensitivity analyses were performed, and heterogeneity was significant in spite which individual study was excluded. We did not find any contributing factor for the heterogeneity with a meta-regression. The quality of the included articles may be the origin of heterogeneity.
Moreover, our review had some limitations. First, we did not consider any randomized control trial in this meta-analysis; the sample sizes of the included studies were small, and most were single center and either a prospective or retrospective study that may have added potential biases to such studies. Second, it is difficult to draw decisive conclusions regarding LA functional change after ablation therapy, because of inconsistencies regarding individual patient data, the imaging method, and the follow-up duration. Third, although publication bias was not significant after performing an Egger’s test and a Begg’s funnel plot, the influence of bias in this article could not be thoroughly excluded, as only studies published in English were included. Forth, we have tried addressing an issue but indirectly regarding the effectiveness of CA for AF by looking at LA size and function, however, it is a pooled data and it has its own set of issues which precludes us from providing any more clarity. Moreover, another limitation is the lack of a gold standard to measure LA function among these involved studies. Currently, MDCT and CMR are considered relatively accurate methods for measuring LA function and size. Finally, although several studies reported that the LA volumes and sizes are predictors of AF recurrence after CA therapy [40–42], our review did not perform an analysis based on AF recurrence in different types of AF. Therefore, we do not know the relationship between AF recurrence and LA function/size among different types of AF.
In conclusion, With CA, LA volumes and LAD were decreased significantly in patients with AF; LAEF was not significant changes in patients with PeAF but decreased in those with PAF.
Supporting Information
(DOC)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
Acknowledgments
We would like to thank everyone who contributed to this research. This study was not supported by any fund.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors have no support or funding to report. Li Su, Male, MD, Doctor of Department of Cardiology, The Second Affiliate Hospital of Chongqing Medical University, was without any source of funds. Bin Xiong, Male, a graduate student study at graduate college, Chongqing Medical University, was without any source of money. Dan Li, Female, a graduate student study at graduate college, Chongqing Medical University, was without any source of money. Jianling Wang, Male, a graduate student study at graduate college, Chongqing Medical University, was without any source of money. Laxman Gyawali, Male, a graduate student study at graduate college, Chongqing Medical University, was without any source of money. Jinjin Jing, Female, a graduate student study at graduate college, Chongqing Medical University, was without any source of money.
References
- 1. Arbelo E, Brugada J, Hindricks G, Maggioni A, Tavazzi L, Vardas P, et al. ESC-EURObservational Research Programme: the Atrial Fibrillation Ablation Pilot Study, conducted by the European Heart Rhythm Association. Europace: European pacing, arrhythmias, and cardiac electrophysiology: journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2012;14(8):1094–103. Epub 2012/05/26. 10.1093/europace/eus153 . [DOI] [PubMed] [Google Scholar]
- 2. Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). European heart journal. 2010;31(19):2369–429. Epub 2010/08/31. 10.1093/eurheartj/ehq278 . [DOI] [PubMed] [Google Scholar]
- 3. Miyasaka Y, Barnes ME, Bailey KR, Cha SS, Gersh BJ, Seward JB, et al. Mortality trends in patients diagnosed with first atrial fibrillation: a 21-year community-based study. Journal of the American College of Cardiology. 2007;49(9):986–92. Epub 2007/03/06. 10.1016/j.jacc.2006.10.062 . [DOI] [PubMed] [Google Scholar]
- 4. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke; a journal of cerebral circulation. 1991;22(8):983–8. Epub 1991/08/01. . [DOI] [PubMed] [Google Scholar]
- 5. Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, et al. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114(7):e257–354. Epub 2006/08/16. 10.1161/circulationaha.106.177292 . [DOI] [PubMed] [Google Scholar]
- 6.January CT, Wann LS, Alpert JS, Calkins H, Cleveland JC Jr, Cigarroa JE, et al. 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation. 2014. Epub 2014/04/01. 10.1161/cir.0000000000000040 . [DOI] [PubMed]
- 7. Jeevanantham V, Ntim W, Navaneethan SD, Shah S, Johnson AC, Hall B, et al. Meta-analysis of the effect of radiofrequency catheter ablation on left atrial size, volumes and function in patients with atrial fibrillation. The American journal of cardiology. 2010;105(9):1317–26. 10.1016/j.amjcard.2009.12.046 . [DOI] [PubMed] [Google Scholar]
- 8. Hesse B, Schuele SU, Thamilasaran M, Thomas J, Rodriguez L. A rapid method to quantify left atrial contractile function: Doppler tissue imaging of the mitral annulus during atrial systole. European journal of echocardiography: the journal of the Working Group on Echocardiography of the European Society of Cardiology. 2004;5(1):86–92. Epub 2004/04/29. . [DOI] [PubMed] [Google Scholar]
- 9. Dagres N, Hindricks G, Kottkamp H, Varounis C, Bode K, Arya A, et al. Effect of atrial fibrillation ablation on left atrial contractile function in patients with paroxysmal atrial fibrillation and a relatively well preserved atrial function. Acta Cardiologica. 2009;64(2):167–9. 10.2143/ac.64.2.2035339 [DOI] [PubMed] [Google Scholar]
- 10. Erdei T, Denes M, Kardos A, Mihalcz A, Foldesi C, Temesvari A, et al. Could successful cryoballoon ablation of paroxysmal atrial fibrillation prevent progressive left atrial remodeling? Cardiovascular ultrasound. 2012;10:11 10.1186/1476-7120-10-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hof IE, Vonken EJ, Velthuis BK, Wittkampf FH, van der Heijden JF, Neven KG, et al. Impact of pulmonary vein antrum isolation on left atrial size and function in patients with atrial fibrillation. Journal of interventional cardiac electrophysiology: an international journal of arrhythmias and pacing. 2013. 10.1007/s10840-013-9860-0 . [DOI] [PubMed]
- 12. Jahnke C, Fischer J, Gerds-Li JH, Gebker R, Manka R, Fleck E, et al. Serial monitoring of reverse left-atrial remodeling after pulmonary vein isolation in patients with atrial fibrillation: a magnetic resonance imaging study. International journal of cardiology. 2011;153(1):42–6. 10.1016/j.ijcard.2010.08.034 . [DOI] [PubMed] [Google Scholar]
- 13. Machino-Ohtsuka T, Seo Y, Ishizu T, Yanaka S, Nakajima H, Atsumi A, et al. Significant Improvement of Left Atrial and Left Atrial Appendage Function After Catheter Ablation for Persistent Atrial Fibrillation. Circulation Journal. 2013;77(7):1695–704. 10.1253/circj.CJ-12-1518 [DOI] [PubMed] [Google Scholar]
- 14. Masuda M, Inoue K, Iwakura K, Okamura A, Koyama Y, Kimura R, et al. The impact of atrial fibrillation ablation on left atrial function: association with baseline left atrial function. Pacing and clinical electrophysiology: PACE. 2012;35(3):327–34. 10.1111/j.1540-8159.2011.03284.x . [DOI] [PubMed] [Google Scholar]
- 15. Montserrat S, Sitges M, Calvo N, Silva E, Tamborero D, Vidal B, et al. Effect of repeated radiofrequency catheter ablation on left atrial function for the treatment of atrial fibrillation. The American journal of cardiology. 2011;108(12):1741–6. 10.1016/j.amjcard.2011.07.041 . [DOI] [PubMed] [Google Scholar]
- 16. Nori D, Raff G, Gupta V, Gentry R, Boura J, Haines DE. Cardiac magnetic resonance imaging assessment of regional and global left atrial function before and after catheter ablation for atrial fibrillation. Journal of interventional cardiac electrophysiology: an international journal of arrhythmias and pacing. 2009;26(2):109–17. 10.1007/s10840-009-9409-4 . [DOI] [PubMed] [Google Scholar]
- 17. Rodrigues AC, Scannavacca MI, Caldas MA, Hotta VT, Pisani C, Sosa EA, et al. Left atrial function after ablation for paroxysmal atrial fibrillation. The American journal of cardiology. 2009;103(3):395–8. 10.1016/j.amjcard.2008.09.094 . [DOI] [PubMed] [Google Scholar]
- 18. Teh AW, Kistler PM, Lee G, Medi C, Heck PM, Spence SJ, et al. Long-term effects of catheter ablation for lone atrial fibrillation: progressive atrial electroanatomic substrate remodeling despite successful ablation. Heart rhythm: the official journal of the Heart Rhythm Society. 2012;9(4):473–80. 10.1016/j.hrthm.2011.11.013 . [DOI] [PubMed] [Google Scholar]
- 19. Tops LF, Delgado V, Bertini M, Marsan NA, Den Uijl DW, Trines SA, et al. Left atrial strain predicts reverse remodeling after catheter ablation for atrial fibrillation. Journal of the American College of Cardiology. 2011;57(3):324–31. 10.1016/j.jacc.2010.05.063 . [DOI] [PubMed] [Google Scholar]
- 20. Yoshida N, Okamoto M, Hirao H, Suenari K, Nanba K, Kinoshita H, et al. Efficacy of pulmonary vein isolation on left atrial function in paroxysmal and persistent atrial fibrillation and the dependency on its baseline function. Echocardiography. 2013;30(7):744–50. 10.1111/echo.12143 . [DOI] [PubMed] [Google Scholar]
- 21. Lemola K, Sneider M, Desjardins B, Case I, Chugh A, Hall B, et al. Effects of left atrial ablation of atrial fibrillation on size of the left atrium and pulmonary veins. Heart rhythm: the official journal of the Heart Rhythm Society. 2004;1(5):576–81. 10.1016/j.hrthm.2004.07.020 . [DOI] [PubMed] [Google Scholar]
- 22. Beukema WP, Elvan A, Sie HT, Misier AR, Wellens HJ. Successful radiofrequency ablation in patients with previous atrial fibrillation results in a significant decrease in left atrial size. Circulation. 2005;112(14):2089–95. 10.1161/CIRCULATIONAHA.104.484766 . [DOI] [PubMed] [Google Scholar]
- 23. Lemola K, Desjardins B, Sneider M, Case I, Chugh A, Good E, et al. Effect of left atrial circumferential ablation for atrial fibrillation on left atrial transport function. Heart rhythm: the official journal of the Heart Rhythm Society. 2005;2(9):923–8. 10.1016/j.hrthm.2005.06.026 . [DOI] [PubMed] [Google Scholar]
- 24. Reant P, Lafitte S, Jais P, Serri K, Weerasooriya R, Hocini M, et al. Reverse remodeling of the left cardiac chambers after catheter ablation after 1 year in a series of patients with isolated atrial fibrillation. Circulation. 2005;112(19):2896–903. 10.1161/CIRCULATIONAHA.104.523928 . [DOI] [PubMed] [Google Scholar]
- 25. Tsao HM, Wu MH, Huang BH, Lee SH, Lee KT, Tai CT, et al. Morphologic remodeling of pulmonary veins and left atrium after catheter ablation of atrial fibrillation: insight from long-term follow-up of three-dimensional magnetic resonance imaging. Journal of cardiovascular electrophysiology. 2005;16(1):7–12. 10.1046/j.1540-8167.2005.04407.x . [DOI] [PubMed] [Google Scholar]
- 26. Tops LF, Bax JJ, Zeppenfeld K, Jongbloed MR, van der Wall EE, Schalij MJ. Effect of radiofrequency catheter ablation for atrial fibrillation on left atrial cavity size. The American journal of cardiology. 2006;97(8):1220–2. 10.1016/j.amjcard.2005.11.043 . [DOI] [PubMed] [Google Scholar]
- 27. Verma A, Kilicaslan F, Adams JR, Hao S, Beheiry S, Minor S, et al. Extensive ablation during pulmonary vein antrum isolation has no adverse impact on left atrial function: an echocardiography and cine computed tomography analysis. Journal of cardiovascular electrophysiology. 2006;17(7):741–6. 10.1111/j.1540-8167.2006.00488.x . [DOI] [PubMed] [Google Scholar]
- 28. Choi JI, Park SM, Park JS, Hong SJ, Pak HN, Lim do S, et al. Changes in left atrial structure and function after catheter ablation and electrical cardioversion for atrial fibrillation. Circulation journal: official journal of the Japanese Circulation Society. 2008;72(12):2051–7. . [DOI] [PubMed] [Google Scholar]
- 29. Delgado V, Vidal B, Sitges M, Tamborero D, Mont L, Berruezo A, et al. Fate of left atrial function as determined by real-time three-dimensional echocardiography study after radiofrequency catheter ablation for the treatment of atrial fibrillation. The American journal of cardiology. 2008;101(9):1285–90. 10.1016/j.amjcard.2007.12.028 . [DOI] [PubMed] [Google Scholar]
- 30. Liu Z, Ling Z, Su L, Wu J, Lan X, Chen Y, et al. The effect of different treatment strategies on left atrial size in patients with lone paroxysmal atrial fibrillation-a prospective cohort study. Journal of interventional cardiac electrophysiology: an international journal of arrhythmias and pacing. 2008;23(3):167–73. 10.1007/s10840-008-9301-7 . [DOI] [PubMed] [Google Scholar]
- 31. Marsan NA, Tops LF, Holman ER, Van de Veire NR, Zeppenfeld K, Boersma E, et al. Comparison of left atrial volumes and function by real-time three-dimensional echocardiography in patients having catheter ablation for atrial fibrillation with persistence of sinus rhythm versus recurrent atrial fibrillation three months later. The American journal of cardiology. 2008;102(7):847–53. 10.1016/j.amjcard.2008.05.048 . [DOI] [PubMed] [Google Scholar]
- 32. Muller H, Noble S, Keller PF, Sigaud P, Gentil P, Lerch R, et al. Biatrial anatomical reverse remodelling after radiofrequency catheter ablation for atrial fibrillation: evidence from real-time three-dimensional echocardiography. Europace: European pacing, arrhythmias, and cardiac electrophysiology: journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2008;10(9):1073–8. 10.1093/europace/eun187 . [DOI] [PubMed] [Google Scholar]
- 33. Perea RJ, Tamborero D, Mont L, De Caralt TM, Ortiz JT, Berruezo A, et al. Left atrial contractility is preserved after successful circumferential pulmonary vein ablation in patients with atrial fibrillation. Journal of cardiovascular electrophysiology. 2008;19(4):374–9. 10.1111/j.1540-8167.2007.01086.x . [DOI] [PubMed] [Google Scholar]
- 34. Calkins H, Brugada J, Packer DL, Cappato R, Chen SA, Crijns HJ, et al. HRS/EHRA/ECAS expert Consensus Statement on catheter and surgical ablation of atrial fibrillation: recommendations for personnel, policy, procedures and follow-up. A report of the Heart Rhythm Society (HRS) Task Force on catheter and surgical ablation of atrial fibrillation. Heart rhythm: the official journal of the Heart Rhythm Society. 2007;4(6):816–61. Epub 2007/06/09. 10.1016/j.hrthm.2007.04.005 . [DOI] [PubMed] [Google Scholar]
- 35. Wazni O, Wilkoff B, Saliba W. Catheter ablation for atrial fibrillation. The New England journal of medicine. 2011;365(24):2296–304. Epub 2011/12/16. 10.1056/NEJMct1109977 . [DOI] [PubMed] [Google Scholar]
- 36. McGann CJ, Kholmovski EG, Oakes RS, Blauer JJ, Daccarett M, Segerson N, et al. New magnetic resonance imaging-based method for defining the extent of left atrial wall injury after the ablation of atrial fibrillation. Journal of the American College of Cardiology. 2008;52(15):1263–71. Epub 2008/10/18. 10.1016/j.jacc.2008.05.062 . [DOI] [PubMed] [Google Scholar]
- 37. Uchiyama T, Miyazaki S, Taniguchi H, Komatsu Y, Kusa S, Nakamura H, et al. Six-Year Follow-up of Catheter Ablation in Paroxysmal Atrial Fibrillation. Circulation Journal. 2013;77(11):2722–7. 10.1253/circj.CJ-13-0468 [DOI] [PubMed] [Google Scholar]
- 38. Cheitlin MD, Armstrong WF, Aurigemma GP, Beller GA, Bierman FZ, Davis JL, et al. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography—summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Journal of the American College of Cardiology. 2003;42(5):954–70. Epub 2003/09/06. . [DOI] [PubMed] [Google Scholar]
- 39. Tops LF, van der Wall EE, Schalij MJ, Bax JJ. Multi-modality imaging to assess left atrial size, anatomy and function. Heart (British Cardiac Society). 2007;93(11):1461–70. Epub 2007/10/16. 10.1136/hrt.2007.116467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sohns C, Sohns JM, Vollmann D, Luthje L, Bergau L, Dorenkamp M, et al. Left atrial volumetry from routine diagnostic work up prior to pulmonary vein ablation is a good predictor of freedom from atrial fibrillation. European heart journal cardiovascular Imaging. 2013;14(7):684–91. Epub 2013/02/26. 10.1093/ehjci/jet017 . [DOI] [PubMed] [Google Scholar]
- 41. Miyazaki S, Kuwahara T, Kobori A, Takahashi Y, Takei A, Sato A, et al. Preprocedural predictors of atrial fibrillation recurrence following pulmonary vein antrum isolation in patients with paroxysmal atrial fibrillation: long-term follow-up results. Journal of cardiovascular electrophysiology. 2011;22(6):621–5. Epub 2011/01/18. 10.1111/j.1540-8167.2010.01984.x . [DOI] [PubMed] [Google Scholar]
- 42. Shin SH, Park MY, Oh WJ, Hong SJ, Pak HN, Song WH, et al. Left atrial volume is a predictor of atrial fibrillation recurrence after catheter ablation. Journal of the American Society of Echocardiography: official publication of the American Society of Echocardiography. 2008;21(6):697–702. Epub 2008/01/12. 10.1016/j.echo.2007.10.022 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.