Abstract
We diagnosed postpartum eclampsia with posterior reversible encephalopathy syndrome (PRES) in a 35-year-old woman who began experiencing headaches after delivery. Cervical MR angiography (MRA) suggested concomitant vertebral artery (VA) dissection. Antiplatelet therapy was not indicated. Each episode resolved spontaneously. The patient subsequently developed sudden onset of thunderclap headache. She experienced a tonicoclonic seizure in the outpatient clinic. On the basis of clinical course and MRI, we diagnosed postpartum eclampsia with PRES. Antiplatelet therapy was not indicated, as there were no signs of stroke. Antiepileptic and antihypertensive medicines were used for a short term to control seizure and blood pressure. Subsequent MRI 17 days after discharge showed resolution of the abnormal signals, but the intramural heme signals became apparent on the dissecting segment of VA. Subsequent MRI after 3 months indicated resolution of arterial dissection. To the best of our knowledge, this represents the third report of postpartum cervicocephalic artery dissection with PRES in the literature.
Background
Headache is a common finding in the postpartum period. Stella et al1 reported causes of postpartum headache for 95 women >24 h after delivery. Posterior reversible encephalopathy syndrome (PRES) is one entity causing postpartum headache. According to that study, PRES accounts for about 4% of cases. The pathogenesis of PRES remains unclear, but appears related to disordered cerebral autoregulation and endothelial dysfunction.
However, cervicocephalic artery dissection (CAD) after childbirth is rare. No patients with CAD were found by Stella et al.1 Arnold et al2 reported that 6% of 102 women with CAD <50 years old were in a postpartum condition. In that study, patients with postpartum CAD had coexisting PRES more often than patients with non-postpartum CAD.2 Concomitant CAD and PRES after childbirth is rare. We present a case of postpartum headache with PRES and concomitant vertebral artery dissection in a 35-year-old woman.
Case presentation
A 35-year-old woman had a normal pregnancy and delivered her first baby without any complications. Blood pressure (BP) remained within the range of 100–110/70–80 mm Hg during the pregnancy. She began experiencing episodic headaches on postpartum day 5, with BP 150/90 mm Hg. Initially, the headaches were located in bioccipital areas and posterior neck with pressure qualities, resolving spontaneously after 7 h. On postpartum day 8, she developed sudden onset of a thunderclap headache, at which time CT of the head was performed and read as normal in the emergency room. The headaches persisted, with orthostatic qualities, and were worse when supine and relieved when upright. At this stage, she was referred to our medical outpatient clinic on postpartum day 11.
BP was 154/96 mm Hg, much higher than her usual pregnant outpatient BP. Axillary temperature was 37°C, heart rate was 72 bpm and respiratory rate was 15 breaths/min. Neurological examination showed no abnormalities.
Investigations
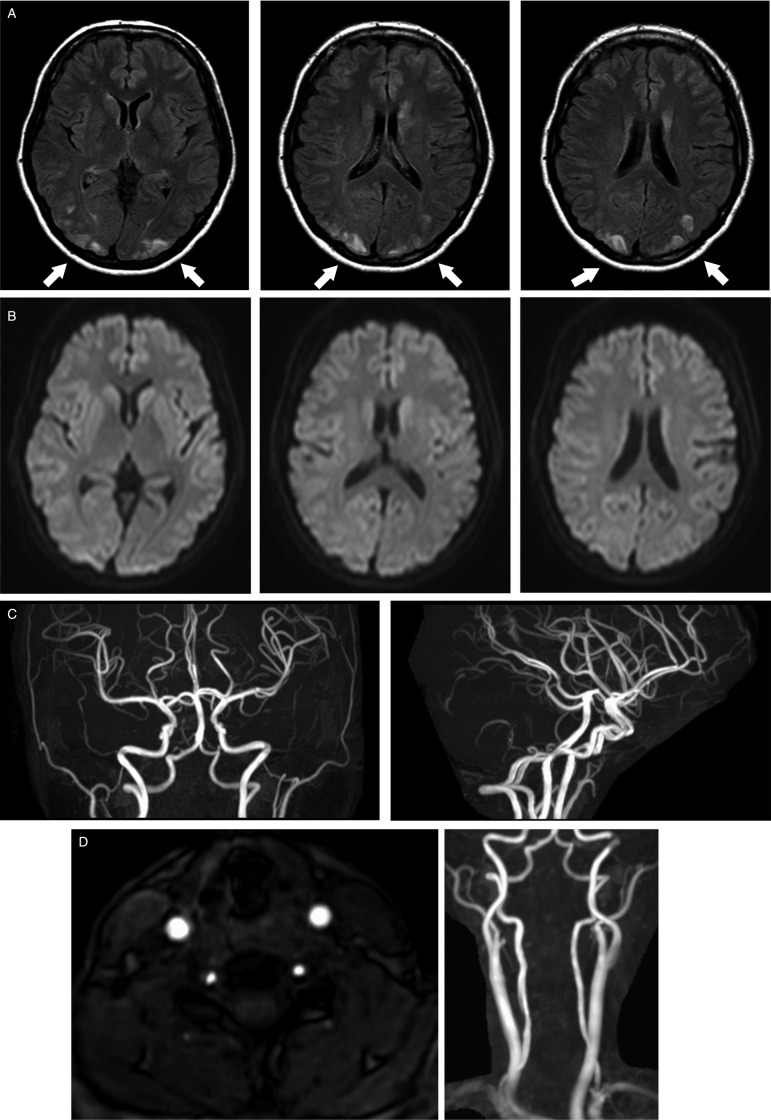
Laboratory investigations were all within normal limits, including blood cell count, liver enzyme levels, renal function and electrolytes. Urinalysis revealed no proteinuria. Cerebrospinal fluid examination yielded normal results. Fluid-attenuated inversion recovery images of MRI revealed bilateral multiple hyperintense areas, predominantly in the subcortical white matter (figure 1A). Diffusion-weighted imaging demonstrated no evidence of ischaemic stroke (figure 1B). MR angiography (MRA) showed no segmental arterial narrowing or dilation in the cerebral vessels (figure 1C). However, the right vertebral artery at the cervical level showed stenosis (figure 1D). After MRI, the patient experienced a tonicoclonic seizure lasting for 1 min. Her level of consciousness gradually normalised postictally, without treatment. She was admitted to our intensive care unit.
Figure 1.
MRI and MR angiography (MRA) on the day of admission. (A) Fluid-attenuated inversion recovery images showing multiple high-intense areas in the bilateral occipital area (arrows). (B) Diffusion-weighted images showing no high-intense area, which suggests that there is no ischaemic stroke. (C) Cranial MRA. There is no segmental arterial narrowing, dilation or occlusion. (D) Right: cervical MRA, left: horizontal image of MRA at the level of fifth cervical vertebra. Cervical MRA showing stenosis at the right vertebral artery.
Differential diagnosis
A woman in the puerperal period who presents with thunderclap headaches and neurological symptoms may have PRES, reversible cerebral vasoconstriction syndrome (RCVS) or CAD. PRES may be reversible, but CAD is not, so these pathologies require differentiation. Identification of one entity causing headaches tends to make us overlook other causes. Variations in the quality of headaches over the clinical course may indicate dual entities as causes of headaches.
We reached a diagnosis of postpartum eclampsia with PRES, based on the clinical course and previously reported MRI findings.3 RCVS is usually diagnosed from the presence of arterial narrowing on angiography. However, MRA of our patient on the day of admission showed no arterial narrowing.
Treatment
The headaches resolved and further seizures were prevented by intravenous treatment with phenytoin and magnesium sulfate. Nicardipine was also administered to control BP. The patient was discharged without any neurological sequela.
Outcome and follow-up
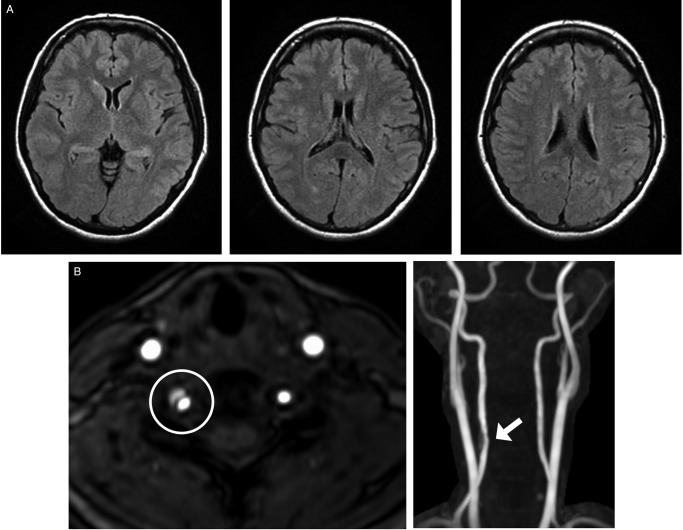
The clinical course was good until subsequent MRI 17 days after discharge was performed. The imaging showed resolution of the multiple abnormal signals in the white matter (figure 2A). However, MRA was suggestive of right vertebral artery dissection at the level of the fifth cervical vertebra, based on the presence of an intramural haematoma (figure 2B),4 which showed stenosis on the day of admission. So, dissection was considered. Antiplatelet therapy for prevention was not indicated, as there were no signs of stroke. All intramural heme signals had resolved by follow-up MRA 3 months later (figure 3).
Figure 2.
Subsequent MRI and MR angiography (MRA) 17 days after discharge. (A) Fluid-attenuated inversion recovery images showing that multiple high-intense areas in the bilateral occipital area, which were observed on the day of admission, disappeared. (B) Right: cervical MRA, left: horizontal image of MRA at the level of fifth cervical vertebra. Cervical MRA showing intramural heme signals at the level of fifth cervical vertebra (arrow and circle).
Figure 3.
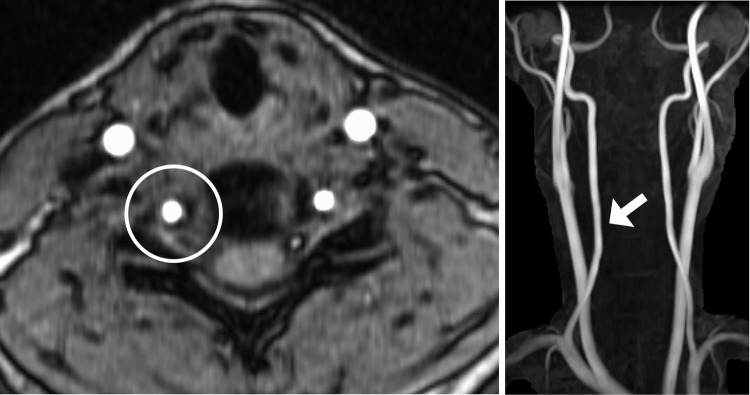
MR angiography (MRA) 3 months after discharge. Cervical MRA showing the resolution of dissecting segment (arrow and circle).
Discussion
Headaches are a frequent symptom in the postpartum period. In the majority of cases, such headaches represent either migraines or tension-type headaches, which are both easily treated.5 Rarely, headaches in the postpartum patient signal a life-threatening condition. Our patient initially reported of a bioccipital headache without neurological deficit 5 days after delivery. This condition was self-limited. However, she developed sudden onset of a thunderclap headache 8 days after delivery. She also experienced a tonicoclonic seizure 11 days after delivery. The quality of the headache, which varied over the clinical course, suggested dual entities as their causes.
PRES is characterised by headaches, seizures and visual changes.3 Characteristic imaging features often include focal regions of symmetric oedema in the posterior brain parenchyma, as well as in other brain regions.3 The pathogenesis is hypothesised to involve disorders of cerebral autoregulation and/or endothelial dysfunction with increased permeability of the blood–brain barrier.3 PRES generally develops in the setting of preeclampsia/eclampsia, but may also develop in the puerperium and as a presenting feature of late eclampsia.3 Most patients with PRES do well if the seizures and hypertension are appropriately managed. Unfortunately, some more severe cases can result in lasting neurological morbidity or even mortality due to ischaemic stroke or haemorrhage.
RCVS and PRES are said to have a shared pathophysiology.5 RCVS should be diagnosed based on the presence of vasoconstriction on MRA. We could not diagnose RCVS in this case due to the absence of narrowed blood vessels on MRA.
CAD is a rare postpartum complication only previously described in case reports and one small case series involving a total of six patients.2 6–10 A recent registry database identified that 2.4% of cases of spontaneous CAD occurred in the postpartum period.2 Postpartum CAD remains poorly understood. According to the case series of six cases with postpartum CAD, four had vertebral artery dissection and two had PRES.2
Stella et al1 reported causes of postpartum headache for 95 women >24 h after delivery. According to that study, PRES accounts for about 4% of cases. However, no patients with CAD were identified in that study. Arnold et al2 reported that a postpartum condition accounted for 6% among 102 women <50 years old with CAD. In that study, patients with postpartum CAD had coexisting PRES more often (2 of 6 patients) than patients with non-postpartum CAD (1 of 96 patients; p=0.009).2 We were unable to find any studies showing how many patients with PRES show concomitant CAD.
Since the dissection segment does not necessarily show the intramural haematoma at the acute stage, the stenosis on MRA on admission at the level of the fifth cervical vertebra was considered for dissection in this case. Therefore, careful observation of clinical symptoms for arterial dissection was made. The prognosis of CAD is related to the severity of associated ischaemic stroke or subarachnoid haemorrhage. Morbidity and mortality of acute CAD depend on the specific arteries involved and location of the dissection. Complete or excellent recovery occurs in 70–85% of patients with CAD, with major deficits in 10–25%, and death in 5–10% of cases.11 The optimal strategy for prevention of stroke in patients with CAD is controversial.
We used the key words “postpartum cervicocephalic artery dissection” and “posterior reversible encephalopathy syndrome” or “PRES” in the PubMed search. No other case reports of postpartum CAD with concomitant PRES were found. To the best of our knowledge, the present case represents only the third to be described in the literature.
Learning points.
Imaging studies are crucial when a patient in the puerperal period experiences headache with neurological symptoms or thunderclap characteristics.
The possibility of multiple entities causing headache must be considered when the quality of the headache varies over the clinical course.
Footnotes
Contributors: KK identified the patient in the outpatient department. MN, EH and KK managed the patient in the ward after admission. MN wrote the draft of this case report. EH, KK and HA reviewed and revised this case report. MN is the guarantor.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Stella CL, Jodicke CD, How HY et al. Postpartum headache: is your work-up complete? Am J Obstet Gynecol 2007;196:318.e1–7. 10.1016/j.ajog.2007.01.034 [DOI] [PubMed] [Google Scholar]
- 2.Arnold M, Camus-Jacqmin M, Stapf C et al. Postpartum cervicocephalic artery dissection. Stroke 2008;39:2377–9. 10.1161/STROKEAHA.107.510107 [DOI] [PubMed] [Google Scholar]
- 3.Hosley CM, McCullough LD. Acute neurological issues in pregnancy and the peripartum. Neurohospitalist 2011;1:104–16. 10.1177/1941875211399126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahn SS, Kim BM, Suh SH et al. Spontaneous symptomatic intracranial vertebrobasilar dissection: initial and follow-up imaging findings. Radiology 2012;264:196–202. 10.1148/radiol.12112331 [DOI] [PubMed] [Google Scholar]
- 5.Singhal AB. Postpartum angiopathy with reversible posterior leukoencephalopathy. Arch Neurol 2004;61:411–16. 10.1001/archneur.61.3.411 [DOI] [PubMed] [Google Scholar]
- 6.Abisaab J, Nevadunsky N, Flomenbaum N. Emergency department presentation of bilateral carotid artery dissections in a postpartum patient. Ann Emerg Med 2004;44:484–9. 10.1016/j.annemergmed.2004.03.031 [DOI] [PubMed] [Google Scholar]
- 7.Inoue T, Nishimura S, Hayashi N et al. Postpartum dissecting aneurysm of the posterior cerebral artery. J Clin Neurosci 2007;14:576–81. 10.1016/j.jocn.2006.04.005 [DOI] [PubMed] [Google Scholar]
- 8.Soltanolkotabi M, Ansari SA, Shaibani A et al. Spontaneous post-partum cervical carotid artery dissection in a patient with reversible cerebral vasoconstriction syndrome. Interv Neuroradiol 2011;17:486–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van de Kelft E, Kunnen J, Truyen L et al. Postpartum dissecting aneurysm of the basilar artery. Stroke 1992;23:114–16. 10.1161/01.STR.23.1.114 [DOI] [PubMed] [Google Scholar]
- 10.Waidelich JM, Bullough AS, Mhyre JM. Internal carotid artery dissection: an unusual cause of postpartum headache. Int J Obstet Anesth 2008;17:61–5. 10.1016/j.ijoa.2007.04.003 [DOI] [PubMed] [Google Scholar]
- 11.Arnold M, Bousser MG, Fahrni G et al. Vertebral artery dissection: presenting findings and predictors of outcome. Stroke 2006;37:2499–503. 10.1161/01.STR.0000240493.88473.39 [DOI] [PubMed] [Google Scholar]