Abstract
One day after molten aluminium had fallen into his right eye, a young man presented to our clinic with a vision of counting fingers at 1 m, conjunctival and corneal epithelial defects, and limbal involvement. He was diagnosed with grade 4 thermal burn and managed medically. Subsequently, the inflammation resolved, however, he developed pannus with conjunctivalisation and scarring of cornea suggestive of partial unilateral limbal stem cell deficiency. He was treated surgically with autologous simple limbal epithelial transplantation (SLET). Postoperatively, his vision improved along with corneal clarity. He achieved a best corrected vision of 20/50 at the last follow-up 27 months postsurgery, with maintenance of a healthy corneal epithelium. This case describes the different management strategies employed in two different stages of an ocular burn. It highlights the long-term success of SLET in a case of ocular surface thermal burn.
Background
A thermal burn of the eye is one among the true ocular emergencies. It can cause visual handicap if not managed in a timely and appropriate manner. Thermal burns are frequently associated with fireworks explosions, boiling water, steam or molten metal. Among molten metal burns, aluminium is most common.1 Acute presentation of an ocular surface burn can range from minor corneal epithelial defects to extensive corneal melt, loss of conjunctival epithelium and limbal ischaemia. The acute phase requires immediate medical management with or without surgical intervention. Subsequently, the possible sequelae that may ensue in the chronic phase of a thermal burn are symblepharon formation, secondary glaucoma, corneal perforation and limbal stem cell deficiency (LSCD).2 LSCD has varied manifestations in the form of recurrent corneal epithelial defects, superficial corneal vascularisation, conjunctivalisation of cornea and fibrovascular pannus formation.3 The definitive management of LSCD is replenishment of the destroyed limbal stem cell population through limbal stem cell transplantation (LSCT). Among the different techniques that have been used for LSCT, simple limbal epithelial transplantation (SLET) is a unique surgical technique in that it combines the benefits of conventional and cultivated LSCT.4
This report describes the successful management and long-term outcome using medical therapy and SLET in a case of unilateral molten metal ocular burn.
Case presentation
A 32-year-old man presented to our clinic in July 2010, with pain, redness and diminution of vision in his right eye 1 day after accidental injury with hot molten aluminium at his factory (figure 1A). He had received first aid in the form of immediate rinsing of the eye and was using a topical steroid, antibiotic, lubricant and cycloplegic eye drops. He had no problem with his left eye. On examination, his unaided visual acuity was counting fingers at 1 m in the right eye, with no further refinement on pin hole or refractive correction, and 20/20 in the left eye. Slit lamp examination of the right eye revealed lid oedema, conjunctival congestion, corneal stromal oedema with 20% conjunctival epithelial defect and a total corneal epithelial defect. There was limbal involvement of 9 clock hours (figure 1B). Digital ocular tension was normal. Thus the patient was diagnosed with grade 4 ocular surface burn (Dua's classification) following thermal injury.1 The left eye was normal.
Figure 1.
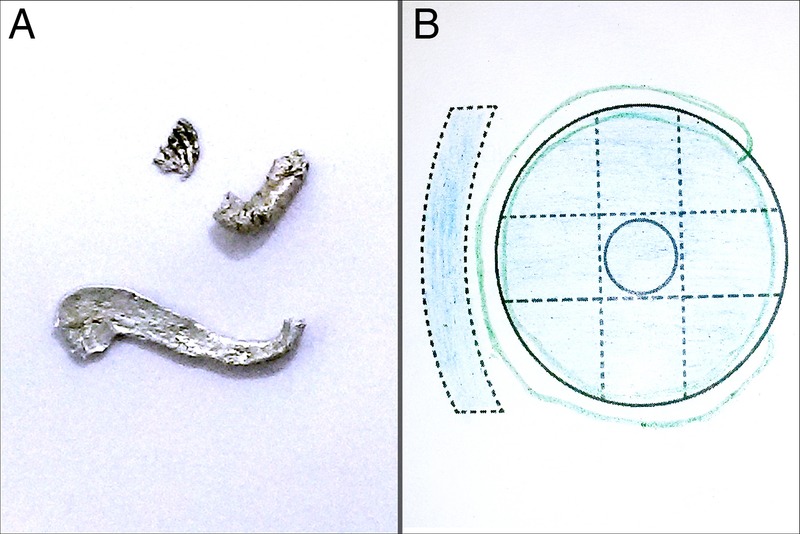
(A) Retrieved aluminium that had fallen into the patient's right eye. (B) Diagrammatic illustration of the right eye at presentation, showing a total corneal epithelial defect, stromal oedema and area of limbal involvement.
Investigations
B scan of the right eye was normal showing the presence of a lens echo, an echo-free vitreous cavity, a normal optic nerve shadow, attached retina and normal choroidal thickness.
Treatment
The patient received eye drops containing prednisolone acetate 1%, chloramphenicol 0.5%, homatropine 2% and carboxy-methyl cellulose 0.5%; and hypromellose 2% eye gel and oral vitamin C 500 mg, which he used for 2 weeks. He was asked to come for review after a week, however, he came to us 2 months later. At this visit, his vision was counting fingers at 3 m in the right eye. There was conjunctivalisation of peripheral cornea involving 9 clock hours and superficial stromal scarring. A diagnosis of partial unilateral LSCD was made and the patient was continued on tapering doses of prednisolone acetate 1% eye drops.
Subsequently, at 10 months from presentation, the patient's vision remained poor at counting fingers 2 m in the right eye. There was formation of symblepharon and pannus that encroached onto the superotemporal quadrant of cornea, conjunctivalisation of the peripheral cornea in three quadrants and corneal scarring (figure 2A). Active inflammation had subsided in the eye. Surgical intervention was planned and the patient underwent autologous SLET in his right eye in June 2012, as per the technique described by us earlier in a pilot study of SLET.4 Donor tissue was harvested from superior limbus of the left eye. After pannus resection from the right eye, human amniotic membrane (hAM) with small pieces of donor limbal tissue was transplanted over the diseased cornea (figure 2B, C). Postoperatively, the patient received topical prednisolone acetate 1% eye drops in his right eye every 3 h, which was gradually tapered over 4 months.
Figure 2.
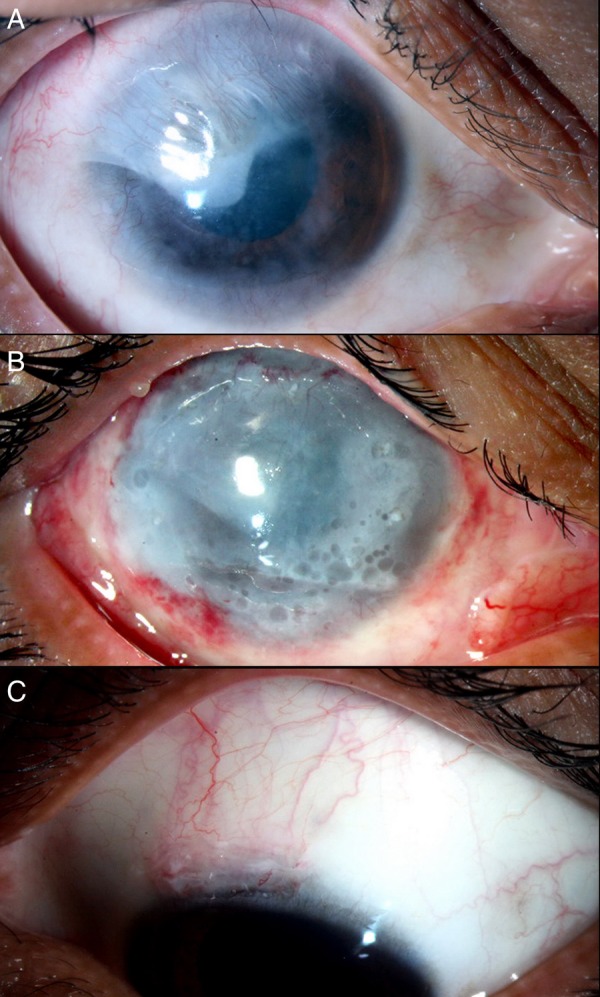
(A) Slit-lamp photograph of the right eye showing pannus on the superotemporal quadrant of cornea, conjunctivalisation of three quadrants of peripheral cornea sparing the nasal quadrant and corneal scarring. (B) Immediate postoperative photograph of the right eye after simple limbal epithelial transplantation (SLET) showing tiny limbal explants (arrows) and amniotic membrane in situ. (C) The donor limbal biopsy site in the left eye covered with adjoining conjunctiva.
Outcome and follow-up
The postoperative visual acuity on day 1 was counting fingers at 20 cm. At 5-month follow-up, the patient's unaided visual acuity was 20/200 with presence of a completely epithelialised and stable surface. This was maintained until his latest follow-up 27 months postsurgery, with further improvement in vision to 20/50, using a rigid gas permeable contact lens. There was gradual dissolution of the limbal biopsy explants, reduction in stromal scarring and improvement in corneal clarity (figure 3). The donor site was healthy in his left eye, and there was no evidence of donor site LSCD.
Figure 3.
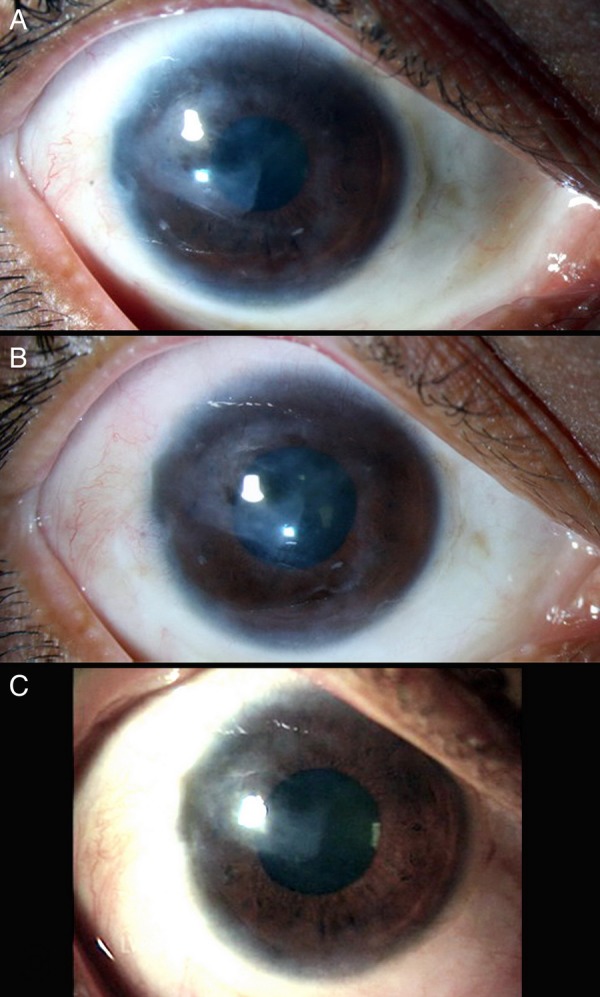
Serial slit lamp photographs of the right eye at (A) 5 months, (B) 10 months and (C) 27 months (last follow-up) postoperatively, showing gradual dissolution of limbal explants, reduction in peripheral corneal vascularisation and increased clarity of cornea with maintenance of a healthy epithelium.
Discussion
This case of a molten metal thermal burn was treated successfully using medical therapy and SLET, with maintenance of a healthy cornea and good visual acuity for over 2 years.
Management of ocular surface burns depends on the stage of presentation. If the patient presents immediately after the insult, management of this acute stage is aimed at promotion of surface epithelialisation, and healing, reduction of inflammation, prevention of infection and maintenance of a normal intraocular pressure. Preservative-free artificial tears for promotion of re-epithelisation, topical steroids to limit the inflammation and topical antibiotics for antimicrobial prophylaxis are indicated. Oral or topical ascorbate and topical citrate aid in epithelial healing, and in prevention of stromal necrosis. If there is extensive damage and necrosis, a surgical approach along with medical therapy may be chosen involving debridement of necrotic tissue followed by amniotic membrane transplantation (AMT) to promote epithelialisation while suppressing the perilimbal inflammation.2 Tamhane et al, in a randomised controlled clinical trial, compared medical therapy alone versus medical therapy with AMT, and concluded that AMT helps in reduction of pain and promotion of early re-epithelialisation in moderate burns only (grades 2 and 3 of Roper-Hall classification). However, it has no definite advantage over medical therapy in terms of improvement of visual acuity, corneal vascularisation or symblepharon formation on short-term follow-up.5 In our case, the patient was managed medically with attainment of a completely epithelialised surface and resolution of inflammation. However, he subsequently developed partial LSCD in the chronic stage of the thermal insult in the form of conjunctivalisation of cornea and pannus formation.
Among the various ocular surface injuries that can cause LSCD, a thermal burn is one of the most severe causes.6 Definitive treatment for LSCD is LSCT, which can be performed through several techniques. An autologous transplantation technique in which the donor tissue is harvested from the same or opposite eye of the patient helps avoid the pitfalls of allogenic transplantation, which include the risk of graft rejection as well as need for prolonged immunosuppression.7 Autologous LSCT can be performed either by a direct grafting of limbal epithelial cells (LECs) or grafting of LECs after cultivating them in vitro on a biological membrane. Techniques of direct limbal tissue grafting have evolved from conjunctivolimbal autograft, which involves harvesting a large portion of donor limbus to SLET in which a very small portion of donor tissue is required.4 The technique of grafting cultivated LECs, known as cultivated limbal epithelial transplantation, was first described by Pellegrini et al8 in 1997, and it is a predecessor of SLET.
SLET, first reported by us in 2012, dispenses the need for a large donor graft and does not require support of a stem cell laboratory setup. In this simple technique, the expansion of limbal epithelial stem cells occurs from multiple pieces of limbal biopsy explants on the host corneal surface directly, as in our case.4 This technique was performed in our patient after a gap of about 1 year following injury, by which time the inflammation had subsided, and this resulted in a successful outcome with complete replenishment of corneal epithelium. In our earlier study, we reported the attainment of a completely epithelialised, avascular and stable corneal surface in all recipient eyes by 6 weeks of SLET, and this was maintained at a mean follow-up of 9.2±1.9 months.7 After this technique was first reported in 2012, there have been a couple of reports on the successful outcome of SLET for LSCD following ocular burns with maintenance of corneal surface stability for more than a year.9 10 The stability of corneal surface was maintained for over 2 years in our case. A best corrected visual acuity of 20/50 was attained in our patient at his latest follow-up, which was a substantial improvement compared to his vision at presentation. Medical management after SLET involves a slow taper of steroids and frequent follow-up to check the health of the corneal epithelium and to look for any recurrence of LSCD. In our case, the corneal epithelium remained healthy and there was no recurrence of LSCD.
This case features a successful outcome of SLET in a case of an ocular thermal burn caused by molten metal, with maintenance of a healthy corneal surface for over 2 years of follow-up. To the best of our knowledge, this is the longest follow-up reported in the literature to date (PubMed search) for a case of ocular thermal burn managed with SLET. This case also emphasises on the options and goals of management of different stages of an ocular surface burn, acute versus chronic. A suitable approach to such cases can result in an excellent outcome.
Learning points.
Thermal ocular burns require timely management for promotion of healing and restoration of vision.
Knowledge regarding the goals and available options for management of different stages of ocular surface burns is essential.
Autologous simple limbal epithelial transplantation (SLET) is an ideal option for treatment of unilateral limbal stem cell deficiency (LSCD) occurring after thermal burns and can give an excellent outcome with maintenance of a stable corneal epithelium over a long period of time.
Reporting the utilisation of SLET technique and its long-term outcomes is necessary to lay strong foundations for acceptance of this technique in the treatment of LSCD.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Dua HS, King AJ, Joseph A. A new classification of ocular surface burns. Br J Ophthalmol 2001;85:1379–83. 10.1136/bjo.85.11.1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fish R, Davidson RS. Management of ocular thermal and chemical injuries, including amniotic membrane therapy. Curr Opin Ophthalmol 2010;21:317–21. 10.1097/ICU.0b013e32833a8da2 [DOI] [PubMed] [Google Scholar]
- 3.Fernandes M, Sangwan VS, Rao SK et al. Limbal stem cell transplantation. Indian J Ophthalmol 2004;52:5–22. [PubMed] [Google Scholar]
- 4.Sangwan VS, Basu S, MacNeil S et al. Simple limbal epithelial transplantation (SLET): a novel surgical technique for the treatment of unilateral limbal stem cell deficiency. Br J Ophthalmol 2012;96:931–4. 10.1136/bjophthalmol-2011-301164 [DOI] [PubMed] [Google Scholar]
- 5.Tamhane A, Vajpayee RB, Biswas NR et al. Evaluation of amniotic membrane transplantation as an adjunct to medical therapy as compared with medical therapy alone in acute ocular burns. Ophthalmology 2005;112:1963–9. 10.1016/j.ophtha.2005.05.022 [DOI] [PubMed] [Google Scholar]
- 6.Shimazaki J, Konomi K, Shimmura S et al. Ocular surface reconstruction for thermal burns caused by fireworks. Cornea 2006;25:139–45. 10.1097/01.ico.0000180083.59244.8f [DOI] [PubMed] [Google Scholar]
- 7.Bhalekar S, Basu S, Sangwan VS. Successful management of immunological rejection following allogeneic simple limbal epithelial transplantation (SLET) for bilateral ocular burns. BMJ Case Rep 2013;2013:pii: bcr2013009051 10.1136/bcr-2013-009051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pellegrini G, Traverso CE, Franzi AT et al. Long-term restoration of damaged corneal surfaces with autologous cultivated corneal epithelium. Lancet 1997;349:990–3. 10.1016/S0140-6736(96)11188-0 [DOI] [PubMed] [Google Scholar]
- 9.Lal I, Panchal BU, Sangwan VS. In-vivo expansion of autologous limbal stem cell using simple limbal epithelial transplantation for treatment of limbal stem cell deficiency. BMJ Case Rep 2013;2013:pii: bcr2013009247 10.1136/bcr-2013-009247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhalekar S, Basu S, Lal I et al. Successful autologous simple limbal epithelial transplantation (SLET) in previously failed paediatric limbal transplantation for ocular surface burns. BMJ Case Rep 2013;2013:pii: bcr2013009888 10.1136/bcr-2013-009888 [DOI] [PMC free article] [PubMed] [Google Scholar]


