Abstract
There are only three cases in the literature that describe development of neurosarcoidosis in a patient who is on tumour necrosis factor α inhibitors. We describe a case of a 33-year-old woman with a history of juvenile rheumatoid arthritis and refractory uveitis (with previous treatment trials of adalimumab, infliximab, mycophenolate, methotrexate) who had been stable for 2 years on etanercept. She was diagnosed with biopsy-proven systemic sarcoidosis with meningeal and parenchymal neurosarcoidosis. She was switched to infliximab and methotrexate, with clinical and imaging improvements. This is a case that demonstrates the difficulty of choosing tumour necrosis factor α (TNF-α) inhibitors when treating patients with multiple clinical autoimmune entities. It is also a case where a change in the mechanism of TNF-α inhibition pathway can still be used to treat refractory sarcoidoisis and rheumatoid arthritis. It is still unclear what the exact difference between the TNF-α blockers and their neurological complications is, and who the patients at risk of developing neurological complications are.
Background
Tumour necrosis factor α (TNF-α) inhibitors have been used as an effective treatment for moderate to severe active rheumatoid arthritis.1 They have also been used as effective combination therapy with methotrexate, which is often used as an adjunctive treatment to prevent immunogenicity.2 Etanercept is an antirheumatic, disease-modifying TNF-α receptor protein used to treat rheumatoid arthritis (RA), ankylosing spondylitis and psoriatic arthritis.3 It has also been used for off-label treatment of refractory sarcoidosis and uveitis.4 In cases of refractory neurosarcoidosis, infliximab, which is a monoclonal antibody against TNF-α, also has been used with success.5–8
According to the drug insert, the most common neurological side effects related to etanercept are headaches (17–19%), dizziness (7%) and fever (2–3%).9 There are also rare adverse events such as aseptic meningitis, demyelinating disorders, normal pressure hydrocephalus, seizure, stroke, lymphomas and sarcoidosis (<3%). It is paradoxical to note that a TNF-α inhibitor used to treat sarcoidosis has also been known to have the rare adverse effect of leading to sarcoidosis. There are three case studies in which development of neurosarcoidosis was reported following the use of TNF-α inhibitors for RA treatment.8 10–12 We present an unusual case of drug-induced neurosarcoidosis after treatment with etanercept, and its resolution with infliximab.
Case presentation
We describe a case of a 33-year-old woman with a history of chronic juvenile RA and refractory uveitis who, at various points, required monotherapy with adalimumab, infliximab, mycophenolate and methotrexate. She was clinically stable for 2 years after being transitioned to etanercept. Subsequently, she presented with an acute mental status change over 2 weeks, which was accompanied by fever (Tmax 39.8°C), daily headaches, joint pain, dizziness, night sweats and chills. A mental status examination showed deficits in attention span, recall and calculation, and difficulty following complex commands. She could not draw a clock.
Investigations
An initial lumbar puncture showed white cell count 28/mm3 (96% lymphocytes, 3% monocytes and 1% lymphocytes) with protein 48 mg/dL and glucose 49 mg/dL. After receiving unremarkable results for viral or bacterial meningitis, there was a high suspicion of aseptic meningitis. MRI of the brain at that time showed diffuse abnormal hyperintensities within the sulci of both cerebral hemispheres associated with abnormal leptomeningeal enhancement; these findings were consistent with meningitis. MRI also showed two small non-specific foci of fluid-attenuated inversion recovery hyper-intense signals in the right thalamus and lower pons (figure 1). The patient was diagnosed with aseptic meningitis, discharged on tramadol and instructed to stop etanercept.
Figure 1.
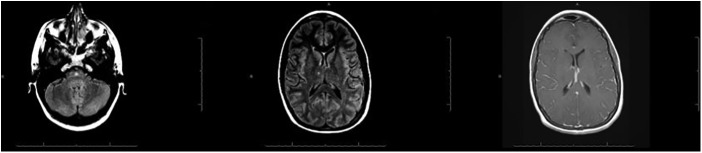
MRI of the brain at admission showing diffuse abnormal hyperintensities within the sulci of both cerebral hemispheres associated with abnormal leptomeningeal enhancement; these findings were consistent with meningitis. The MRI also showing two small, non-specific foci of fluid-attenuated inversion recovery hyperintense signals in the R thalamus and lower pons.
Three weeks after discharge, the patient developed a new onset of transient left leg numbness, ataxia and worsening cognitive issues. A repeat MRI of the brain showed small hyper-intense lesions on her cortex, and an MRI of the cervical spine was also performed to look for a demyelinating process (figure 2). MRI was unremarkable, but there was an incidental finding of abnormal lymph nodes in the right upper mediastinum (figure 3). Thoracic, abdominal and pelvic CT scans showed hepatosplenomegaly and lymphadenopathy in the axillary, mediastinal, intra-abdominal, iliac chain and inguinal lymph nodes (figure 4). A PET scan did not show abnormal uptake. Subsequent fine-needle aspiration of the mediastinal lymph node and cerebrospinal fluid cytology was not revealing and did not show evidence of lymphoma. After 1 month, subsequent MRIs of the brain, and cervical and thoracic spine, were negative for any new demyelinating lesions. Another lumbar puncture was also negative for oligoclonal bands, JCV PCR, cytology and normal ACE level. A core biopsy of a left external iliac lymph node demonstrated non-caseating granulomatous lymphadenitis without evidence of lymphoma. Staining was negative for acid fast or fungal organisms. A lymph node biopsy confirmed a diagnosis of sarcoidosis (figure 5). The patient was ultimately diagnosed with probable neurosarcoidosis with meningeal and parenchymal involvement.
Figure 2.
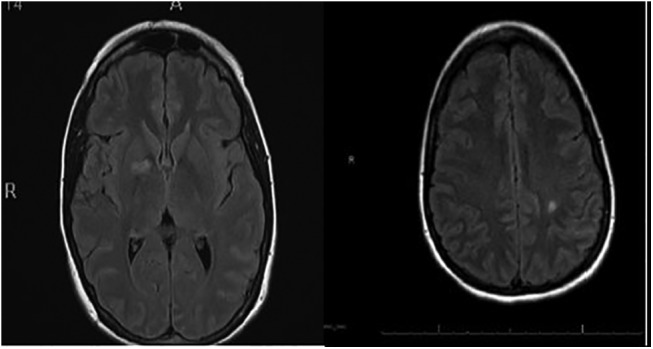
Repeat MRI of the brain showing small hyperintense lesions on the cortex 1 month later.
Figure 3.
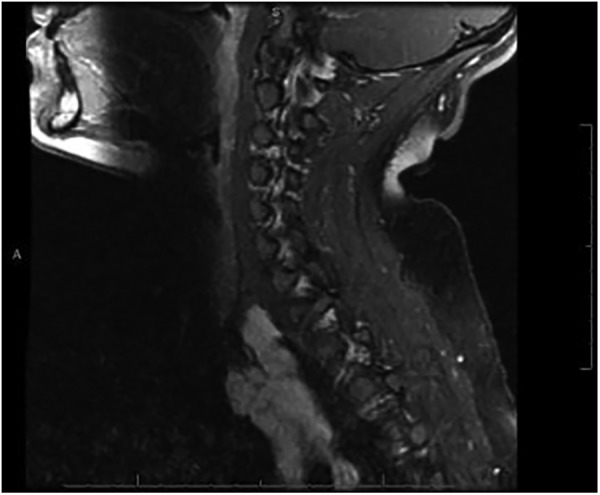
MRI of the c-spine showing an incidental finding of abnormal lymph nodes in the right upper mediastinum.
Figure 4.
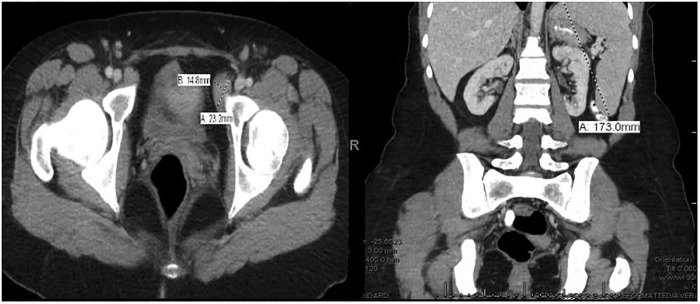
CT of the pelvis with contrast demonstrating lymphadenopathy. Coronal view CT scan with splenomegaly.
Figure 5.
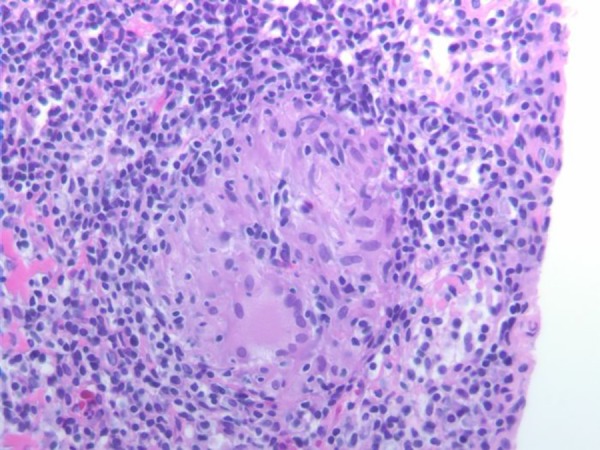
Core biopsy of the left external iliac lymph node showing non-caseating granulomatous lymphadenitis without evidence of lymphoma.
Differential diagnosis
The major differential diagnoses that could explain the patient's neurological symptoms were possible lymphoma, demyelinating process, or systemic sarcoidosis.
Treatment
The patient was treated with pulse steroids, followed by oral taper steroids in addition to methotrexate 25 mg intramuscularly weekly and infliximab 400 mg (5 mg/kg) intravenously every 8 weeks.
Outcome and follow-up
As the patient's therapy was maintained with infliximab and methotrexate, she showed clinical and imaging improvements (figure 6).
Figure 6.
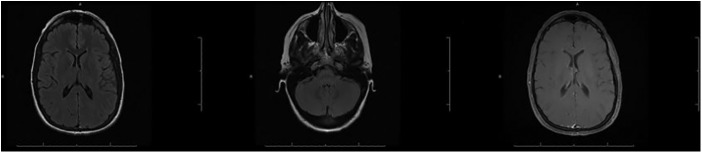
As the patient's therapy was maintained with infliximab and methotrexate, the patient showed clinical and imaging improvement. MRI of the brain 2 years post-therapy.
Discussion
Sarcoidosis is a complex systemic disease, the pathophysiology of which involves helper T1 immune response. This response reportedly activates cytokines, including TNF-α, which in turn form granuloma.1 Neurogenic sarcoidosis is uncommon; it is prevalent in approximately 5% of patients with sarcoidosis, and its cause is not known.13 The concern is that corticosteroids may not be successful in treating neurosarcoidosis, which makes it crucial to consider alternative treatment such as immunotherapy, given that the deficits and manifestations of neurosarcoidosis can be quite devastating. One of the immunotherapies involves TNF-α inhibitors such as etanercept, which is a soluble p75 TNF receptor fusion protein that binds to immunoglobulin G. Infliximab, which is a chimeric monoclonal antibody directly against TNF-α, is another immunotherapy that can be used.14
There have been cases in the rheumatology literature that describe paradoxical events in which sarcoid-like granulomatosis developed with the utilisation of TNF-α blockers in inflammatory conditions. One example is RA, in which tuberculous granulomas occurred with monoclonal anti-TNF antibodies, as well as sarcoid-like granulomatosis with TNF soluble receptor and monoclonal anti-TNF antibodies.15 It is thought that an anti-TNF-α blockade can potentially lead to sarcoidosis by enhancing the infectious antigens or by affecting cytokines.13 Our case demonstrates a rare example in which treatment with one TNF-α inhibitor (etanercept) was associated with the development of neurosarcoidosis, while transitioning to an alternate TNF-α inhibitor (infliximab) led to resolution. Only three cases of neurosarcoidosis have been reported with the use of TNF-α blockers, and among these only one case was associated with etanercept.8 10–12 This leads to the question of why one TNF-α inhibitor resolves symptoms while another induces them. Since we did not obtain histological confirmation, this case is probable, and not definite, neurosarcoidosis, based on Zajicek et al16's criteria for diagnosis of neurosarcoidosis. In the literature, it has been observed that the use of infliximab in pulmonary sarcoidosis was helpful in improving symptoms, whereas the use of etanercept was not as successful. It was noted that this contradiction among TNF-α inhibitors was likely associated with the differences within the mechanisms of TNF-α blockade.16 Our case demonstrates a fascinating point in which changing one TNF-α blocker to another in combination with methotrexate therapy led to resolution of neurosarcoidosis. It is known that TNF-α receptor proteins and anti-TNF monoclonal antibodies are both associated with development of sarcoidosis. However, the TNF-α receptor proteins had the highest frequency of development of sarcoidosis compared to the anti-TNF monoclonal antibodies.11 As our case demonstrates, there is a concern that the TNF-α receptor protein has a greater risk of granuloma formation. One of the known reasons for this enhanced risk is the reduction of INF-γ by infliximab due to the lysis of CD4 and CD8 cells versus production of INF-γ by etanercept, causing sarcoidosis.11 Moreover, the p75 mediated TNF-α receptor function in etanercept is known to cause granuloma, whereas the complete inhibition of both p55-mediated and p75-mediated action in infliximab decreases the risk of development.11 Furthermore, the respective administration and clearance of TNF-α receptor proteins and anti-TNF monoclonal antibodies are known to cause different peak concentrations, and steady-state drug levels. In particular, there is especially higher concentration and drug levels in infliximab, which cause greater and more prolonged TNF-α suppression.17
In conclusion, it is crucial to consider changing TNF-α inhibitors if one type of therapy induces sarcoidosis. Ours is a case that demonstrates the difficulty of choosing a TNF-α inhibitor for treating patients with multiple clinical autoimmune entities. A change in the mechanism of TNF-α inhibition pathways can still be used to treat refractory sarcoidosis and rheumatoid arthritis. It is still unclear what the exact differences between the TNF-α inhibitors and their neurological complications are, and also as to which patients are at risk of developing neurological complications. The above case has proven our hypothesis that the use of different mechanisms of various TNF-α inhibitors may be useful to treat a specific individual's secondary autoimmunity that is mediated by possible genetic susceptibility and related to drug-dependent, not class-dependent, action. We have successfully treated our patient using infliximab despite rare reports associating this drug with development of neurosarcoidosis.18 Physicians should be aware of this potential risk due to adverse autoimmune effects when treating patients with TNF-α blockers.
Learning points.
This is a case that demonstrates the difficulty of choosing a tumour necrosis factor α (TNF-α) inhibitor for treating patients with multiple clinical autoimmune entities.
Use of different mechanisms of various TNF-α inhibitors may be useful to treat a specific individual's secondary autoimmunity that is mediated by possible genetic susceptibility and related to drug-dependent, not class-dependent, action.
Physicians should be aware of this potential risk due to adverse autoimmune effects when treating patients with TNF-α inhibitors.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Gerske AK, Hunninghake G. The immunology of sarcoidosis. Clin Chest Med 2008;29:379–90. 10.1016/j.ccm.2008.03.014 [DOI] [PubMed] [Google Scholar]
- 2.Breedveld FC, Weisman MH, Kavanaugh AF et al. . The PREMIER study: a multicenter, randomized, double-blind clinical trial of combination therapy with adalimumab plus methotrexate versus methotrexate alone or adalimumab alone in patients with early, aggressive rheumatoid arthritis who had not had previous methotrexate treatment. Arthritis Rheum 2006;54:26–37. 10.1002/art.21519 [DOI] [PubMed] [Google Scholar]
- 3.Enbrel (etacercept) food and drug administration highlights of prescribing information. Food and drug administration; 1998. http://www.accessdata.fda.gov/drugsatfda_docs/label/2003/etanimm060503LB.pdf [Google Scholar]
- 4.Saurenmann RK, Levin AV, Rose JB et al. . Tumor necrosis factor alpha inhibitors in the treatment of childhood uveitis. Rheumatology (Oxford) 2006;45:982–9. 10.1093/rheumatology/kel030 [DOI] [PubMed] [Google Scholar]
- 5.Pereira J, Anderson NE, McAuley D et al. . Medically refractory neurosarcoidosis treated with infliximab. Intern Med J 2011;41:354–7. 10.1111/j.1445-5994.2011.02457.x [DOI] [PubMed] [Google Scholar]
- 6.Chintamaneni S, Patel AM, Pegram SB et al. . Dramatic response to infliximab in refractory neurosarcoidosis. Ann Indian Acad Neurol 2010;13:207–10. 10.4103/0972-2327.70874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Santos E, Shaunak S, Renowden S et al. . Treatment of refractory neurosarcoidosis with infliximab. J Neurol Neurosurg Psychiatry 2010;81:241–6. 10.1136/jnnp.2008.149989 [DOI] [PubMed] [Google Scholar]
- 8.Sturfelt G, Christensson B, Bynke G et al. . Neurosarcoidosis in a patient with rheumatoid arthritis during treatment with infliximab. J Rheumatol 2007;34:2313–14. [PubMed] [Google Scholar]
- 9.Etanercept: Drug information Lexicomp 2014 uptodate. Copyright 1978–2014 Lexicomp, Inc.
- 10.Durel CA, Feurer E, Pialat JB et al. . Etanercept may induce neurosarcoidosis in a patient treated for rheumatoid arthritis. BMC Neurol 2013;13:212 10.1186/1471-2377-13-212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tong D, Manolios N, Howe G et al. . New onset sarcoid-like granulomatosis developing during anti-TNF therapy: an under-recognised complication. Intern Med J 2012;42:89–94. 10.1111/j.1445-5994.2011.02612.x [DOI] [PubMed] [Google Scholar]
- 12.Mao-Draayer Y, Cash T. Neurosarcoidosis in a patient treated with tumor necrosis factor alpha inhibitors. J Neurol 2013;13:651–3. 10.1007/s00415-012-6726-9 [DOI] [PubMed] [Google Scholar]
- 13.Krumbolz A, Stern BJ. Neurologic manifestations of sarcoidosis. Handb Clin Neurol 2014;119:305–33. 10.1016/B978-0-7020-4086-3.00021-7 [DOI] [PubMed] [Google Scholar]
- 14.Stone JH, Furst DH, Romain PL. Overview of biological agents in the rheumatic diseases. Uptodate.com, August 29 2012. http://www.uptodate.com/contents/overview-of-biologic-agentsin-the-rheumatic-diseases?source=see_link.
- 15.Daien Cl, Monnier A, Claudepierre P et al. . Sarcoid-like granulomatosis in patients treated with tumor necrosis factor blockers: 10 cases. Rheumatology 2009;48:883–6. 10.1093/rheumatology/kep046 [DOI] [PubMed] [Google Scholar]
- 16.Zajicek JP, Scolding NJ, Foster O et al. . Central nervous system sarcoidosis–diagnosis and management. QJM Mon J Assoc Physicians 1999;13:103–17. 10.1093/qjmed/92.2.103 [DOI] [PubMed] [Google Scholar]
- 17.Verschueren K, Van Essche E, Verschueren P et al. . Development of sarcoidosis in etanercept-treated rheumatoid arthritis patients. Clin Rheumatol 2007;26:1969–71. 10.1007/s10067-007-0594-1 [DOI] [PubMed] [Google Scholar]
- 18.Denys BG, Bogaerts Y, Coenegrachts KL et al. . Steroid-resistant sarcoidosis: is antagonism of TNF-alpha the answer? Clin Sci (Lond) 2007;112:281–9. 10.1042/CS20060094 [DOI] [PubMed] [Google Scholar]


