Abstract
Glycogen storage disease type IX (GSD IX) is caused by a defect in phosphorylase b kinase (PhK) that results from mutations in the PHKA2, PHKB, and PHKG2 genes. Patients usually manifest recurrent ketotic hypoglycemia with growth delay, but some may present simple hepatomegaly. Although GSD IX is one of the most common causes of GSDs, its biochemical and genetic diagnosis has been problematic due to its rarity, phenotypic overlap with other types of GSDs, and genetic heterogeneities. In our report, a 22-month-old boy with GSD IX is described. No other manifestations were evident except for hepatomegaly. His growth and development also have been proceeding normally. Diagnosed was made by histologic examination, an enzyme assay, and genetic testing with known c.3210_3212del (p.Arg1070del) mutation in PHKA2 gene.
Keywords: Glycogen storage disease, Glycogen storage disease type IX, Phosphorylase b kinase 2, Phosphorylase kinase, Hepatomegaly
INTRODUCTION
Glycogen storage disease (GSD) is a group of diseases caused by inborn errors of glycogen metabolism that affect the liver and/or muscle. It is characterized by the accumulation of glycogen in various tissues and is caused by deficiencies of enzymes or transporter proteins involved in glycogen metabolism [1]. GSD type IX (GSD IX) results from a deficiency of phosphorylase b kinase (PhK), which plays an essential role in regulating the breakdown of glycogen to glucose. Defects in PhK, corresponding to GSD IX, are responsible for 25% of all cases of GSD and occur with a frequency of 1 in 100,000 live births [2]. PhK activates glycogen phosphorylase, which catalyzes the glucosyl units from glycogen to release glucose 1-phosphate [3]. PhK is a holoenzyme consisting of four subunits (α, β, γ, and δ subunits). The α, β, and γ subunits are encoded by PHKA1 or PHKA2, PHKB, and PHKG2, respectively. PhK deficiency can be either hepatic or muscular. PHKA1 (Xq13.1) encodes the muscle form of the α subunit, whereas PHKA2 (Xp22.1) encodes the liver form. PHKA1 mutations cause GSD IXd (OMIM 300559), a muscle form of GSD, whereas PHKA2 mutations cause a liver form of GSD IXa (OMIM 306000). GSD IXa is the most common GSD IX, accounting for about 75% of all GSD IX cases [4,5]. Both GSD IXa and GSD IXd are inherited in an X-linked recessive manner. Deficiencies of the other two PhK subunits, β and γ subunits, cause two recessive forms, GSD IXb (OMIM 261750), from PHKB (16q12.1) mutations [3], and GSD IXc (OMIM 613027), from PHKG2 (16p11.2) mutations, respectively [4,5]. GSD IXb includes both liver and muscle PhK deficiencies, whereas GSD IXc is characterized by liver PhK deficiency.
Although GSD IX is a major subgroup of GSDs, its biochemical and genetic diagnosis has been problematic due to its rarity, phenotypic overlap with other types of GSDs, and genetic heterogeneities. To date, only one case of GSD IX has been reported in the Korean population [6]. Here, we describe another Korean patient with GSD IXa confirmed by biochemical and genetic testing.
CASE REPORT
A 22-month-old boy was transferred our hospital due to persistent hepatomegaly for 5 months. Except for hepatomegaly and abdominal distension, he had no specific symptom.
On physical examination, his abdomen was diffusely distended and the liver was palpable at three finger breadths below the right costal margin. He had no jaundice or splenomegaly. His neurologic exams were all normal. Mental state was alert, and muscle contracted normally full resistance. His height was 87 cm, a 0.24 standard deviation (SD) score of age- and sex-matched controls, and his body weight was 14.5 kg (1.46 SD score). No history of hypoglycemic episodes or hepatitis was present. There was no family history of liver disease.
On history taking, the patient was born by normal vaginal delivery after 40 weeks of gestation and his birth weight was 4,020 g. The prenatal and postnatal periods were uneventful and his developmental milestones had been normal. Mild abdominal distension was noted at 12 months of age by his parents. At 17 months of age, he visited a local clinic because of vomiting, diarrhea, and poor oral intake. On physical examination, the abdomen was distended and the liver was palpable at three finger breaths below the right costal margin. Jaundice, lymphadenopathy, or splenomegaly was not noted. His hemoglobin, white blood cell counts, and platelet counts were 12.8 g/dL (normal range, 10.5-14.0 g/dL), 14.65×103/µL (6-15×103/µL), and 572×103/µL (150-450×103/µL), respectively. Serum aspartate aminotransferase (AST) was 53 IU/L (15-40 IU/L) and alanine aminotransferase (ALT) was 56 IU/L (10-40 IU/L). Serum total bilirubin was 0.5 mg/dL (0.2-1.2 mg/dL) and creatine kinase (CK) was 116 IU/L (32-294 IU/L). Serum ceruloplasmin was 36.1 mg/dL (15-44 mg/dL) and ferritin was 38.5 ng/mL (22-322 ng/mL).
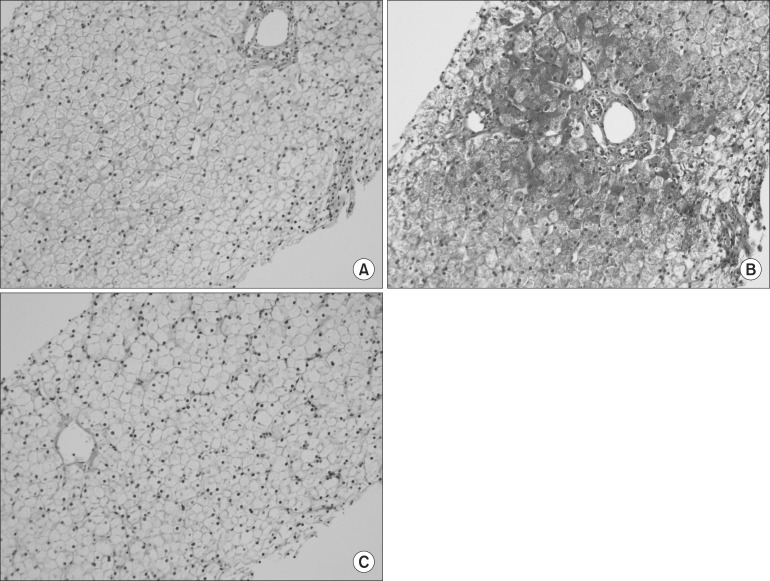
In our hospital, his AST, ALT, and bilirubin levels were 42 IU/L, 38 IU/L, and 0.7 mg/dL, respectively. His serum cholesterol, uric acid, glucose, lactic acid, CK, and albumin levels were all normal (Table 1). Serological tests revealed no evidence of infection such as hepatitis virus A, B, or C, Epstein-Barr virus, or cytomegalovirus. Plasma amino acid and urine organic acid profiles were also unremarkable. On sonographic examination, his liver was enlarged with slightly increased parenchymal echogenicity but the intrahepatic and extrahepatic biliary ducts were not dilated. The gallbladder and spleen were normal. A liver biopsy was performed and, on histological examination, the hepatocytes were filled with abundant glycogen particles in the cytoplasm with peripheral displacement of organelles (Fig. 1).
Table 1. Laboratory Findings in a Korean Patient with Glycogen Storage Disease Type IXa.
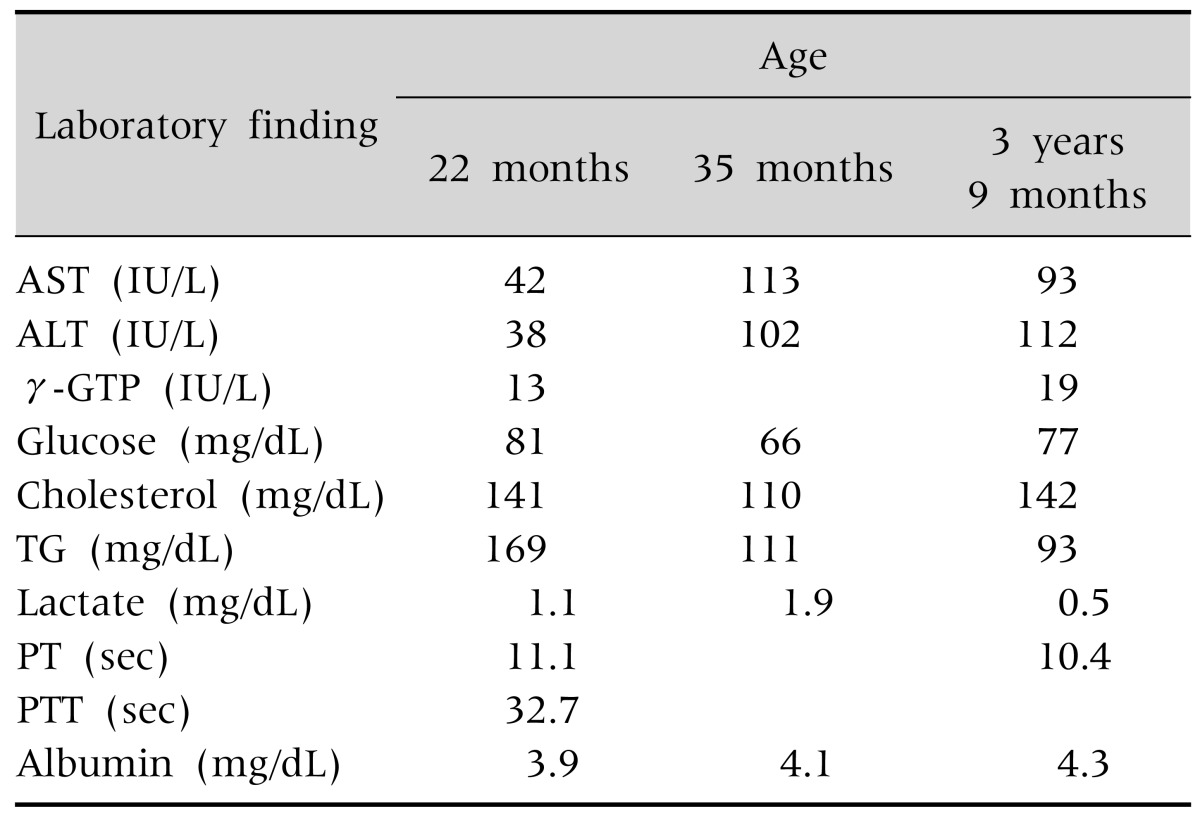
AST: aspartate aminotransferase, ALT: alanine transaminase, γ-GTP: gamma-glutamyl transpeptidase, TG: triglyceride, PT: prothrombin time, PTT: partial thromboplastin time.
Fig. 1. Pathologic findings. (A) Hepatocytes were filled with abundant glycogen particles in the cytoplasmonroutine transmission electron microscopy (×200). (B) Hepatocyte cytoplasmic material was positive byperiodic acid-Schiff staining (×200). (C) Hepatocyte cytoplasmic material was digested by diastase-treatment (×200).
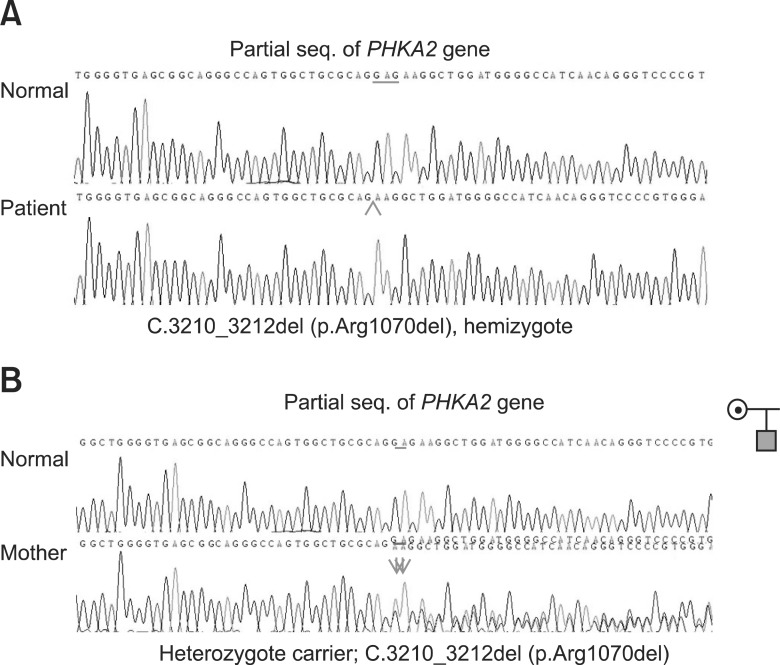
With a high suspicion of GSD, genetic testing was performed to rule out GSD III (the AGL gene) and GSD VI (the PYGL gene). Genomic DNA was isolated from peripheral leukocytes of the patient with a PureGene blood kit (Qiagen, Hilden, Germany). All exons and their intronic boundaries of AGL and PYGL were amplified and sequenced using a BigDye Terminator V3.1 Cycle Sequencing Ready Reaction kit (Applied Biosystems, Foster City, CA, USA). He had normal sequences in the coding regions of the AGL and PYGL genes. We then checked PhK activity in the red blood cells, which was 15 µmol/min/g Hb (normal range, 100-300 µmol/min/g Hb). With a suspicion of GSD IXa, the PHKA2 gene was tested. Thirty-three exons and their intronic boundaries were investigated, revealing a previously reported mutation, c.3210_3212del (p.Arg1070del) (Fig. 2A) [7]. His mother carried the mutation as a heterozygote (Fig. 2B). However, there was no family history of liver disease on his maternal side.
Fig. 2. Partial genomic sequences of the PHAK2 gene. (A) The patient is a homozygotefor the c.3210_3212del (p.Arg1070del) mutation. (B) His mother is a heterozygote for this mutation.
We educated his parents on preventing hypoglycemia via frequent meals high in complex carbohydrates and protein, as well as cornstarch supplements. In particular, we advised that cornstarch should be fed to the patient before bed to maintain an adequate glucose level throughout the night. We recommended liver ultrasonography every 6months. At the latest evaluation at 4.2 years of age, his height was 100 cm (-0.4 SD score) and his weight was 19.8 kg (1.32 SD score). He had not experienced any hypoglycemic episodes. Hepatic dysfunction was unchanged except for elevated AST and ALT.
DISCUSSION
Our patient had no symptomatic presentation of liver-type GSD, such as hypoglycemia, delayed development, or growth retardation, and had only hepatosplenomegaly with hepatic enzyme elevation. GSD I is the most common liver type in Korea [8], but GSD I usually manifests in the neonatal period with severe and recurrent hypoglycemia. Patients with GSD III and GSD IV usually present mild fasting hypoglycemia, as in GSD IX. Most patients have both liver and muscle involvement in GSD III, which shows hypotonia, weakness, wasting of skeletal muscle, and heart involvement. Osteopenia and fractures are associated with GSD III and GSD IV [9]. GSD IV typically presents in early infancy with hepatosplenomegaly and growth failure. The disorder is rapidly progressive, leading to liver failure without transplantation [10,11]. Otherwise, there is no evidence of viral hepatitis and autoimmune hepatitis. Liver and/or muscle cells are affected in GSD IX and when liver cells are affected in this disorder the signs and symptoms appear in early childhood [4,5]. Liver enlargement and slow growth are the initial features. The height of affected children is usually below the average of age- and sex-matched controls. During prolonged fasting periods, hypoglycemia or increasing levels of ketones are one of the signs of being affected, although ketotic hypoglycemia is not always noted in GSD IXa. In addition, patients may have delayed achievement of motor skills, and some have mild muscle weakness. These signs and symptoms usually improve with age. However, some patients may have a fibrosis in the liver tissue, which can in rare cases progress to irreversible liver cirrhosis in childhood [12,13,14]. Therefore, it is very important to make an early diagnosis of GSD IX and to undertake surveillance for hepatic dysfunction on a regular basis in these patients. Patients with muscle-type GSD IX may experience myopathy such as fatigue, cramps, and muscle pain, especially during exercise. Muscle-type GSD IX is a rare form, and most patients are diagnosed between 15 and 36 years of age [15]. Hypercholesterolemia and hyper triglyceridemia are common. CK levels are sometimes increased in muscle-type GSD IX. In myopathic variants, less frequent presentations include cardiac problems [10].
In the liver biopsy sample, we found glycogen particles in hepatocytes, indicative of GSD. After GSD III (the AGL gene) and GSD VI (the PYGL gene) were ruled out by genetic testing, we evaluated PhK activity to confirm a diagnosis of GSD IX and identified the c.3210_3212del (p.Arg1070del) mutation in the PHKA2 gene. This mutation was reported previously in a Finnish boy who also only had hepatomegaly with no growth retardation or hypoglycemic episodes [7]. As an in-frame deletion, the mutant protein might have residual function, which could be evaluated by assessing the RNA and protein expression of the mutant PHKA2.
Given the X-linked inheritance of GSD, we recommended genetic testing of the mother and sisters of our patient. His mother is a heterozygote for the same mutation of PHAK2. The testing has not yet been performed in his sisters. The screening of the carrier state of female members is important because some female carriers can manifest mild hepatomegaly with hepatic dysfunction and growth retardation and the severity can differ according to the degree of the skewed inactivation of the X chromosome. In addition, GSD IX can progress with age in some carriers [16]. Thus, regular surveillance of hepatic function should be performed for female carriers with GSD IXa. Another reason for the importance of family screening is that the inheritance from a female carrier to her son is 50% and the risks to future offspring should be carefully discussed.
Our current patient is the second reported Korean case of GSD IXa to date. Unlike the previous Korean case, however, our current patient had no specific symptoms such as ready fatigability or hypoglycemic events. Moreover, his growth was not significantly retarded and there was no familial history of liver disease. On the other hand, the first reported Korean case, a 5-year-old boy, presented with mild hypoglycemic symptoms, easy fatigability, and hepatomegaly since the age of two [6].
There is no specific treatment for GSD IX, but complex carbohydrates and protein-rich foods can prevent hypoglycemia. Night-time cornstarch consumption can stave off a hypoglycemic attack during sleep. Patients should be monitored for hepatic dysfunction on a regular basis. Though rare, some affected patients have fibrosis in the liver, which can progress to liver cirrhosis. In addition, echocardiography should be performed every 5 years to survey cardiac involvement in muscle-type GSD IX. Growth retardation is a common symptom of GSD IX but almost all patients achieve complete catch-up in growth.
In conclusion, our experience with the present case indicates the importance of screening for GSD IXa in male patients who are suspected of having GSD but manifest unusual presentations, such as those owe have here described. More Korean cases should be identified considering the prevalence of this GSD subgroup. Early identification and management is important for patient prognosis.
References
- 1.Lau CK, Hui J, Fong FN, To KF, Fok TF, Tang NL, et al. Novel mutations in PHKA2 gene in glycogen storage disease type IX patients from Hong Kong, China. Mol Genet Metab. 2011;102:222–225. doi: 10.1016/j.ymgme.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 2.Maichele AJ, Burwinkel B, Maire I, Søvik O, Kilimann MW. Mutations in the testis/liver isoform of the phosphorylase kinase gamma subunit (PHKG2) cause autosomal liver glycogenosis in the gsd rat and in humans. Nat Genet. 1996;14:337–340. doi: 10.1038/ng1196-337. [DOI] [PubMed] [Google Scholar]
- 3.Newgard CB, Hwang PK, Fletterick RJ. The family of glycogen phosphorylases: structure and function. Crit Rev Biochem Mol Biol. 1989;24:69–99. doi: 10.3109/10409238909082552. [DOI] [PubMed] [Google Scholar]
- 4.Tsilianidis LA, Fiske LM, Siegel S, Lumpkin C, Hoyt K, Wasserstein M, et al. Aggressive therapy improves cirrhosis in glycogen storage disease type IX. Mol Genet Metab. 2013;109:179–182. doi: 10.1016/j.ymgme.2013.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bali DS, Goldstein JL, Fredrickson K, Rehder C, Boney A, Austin S, et al. Variability of disease spectrum in children with liver phosphorylase kinase deficiency caused by mutations in the PHKG2 gene. Mol Genet Metab. 2014;111:309–313. doi: 10.1016/j.ymgme.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park KJ, Park HD, Lee SY, Ki CS, Choe YH. A novel PHKA2 gross deletion mutation in a Korean patient with X-linked liver glycogenosis type I. Ann Clin Lab Sci. 2011;41:197–200. [PubMed] [Google Scholar]
- 7.Crushell E, Treacy EP, Dawe J, Durkie M, Beauchamp NJ. Glycogen storage disease type III in the Irish population. J Inherit Metab Dis. 2010;33(Suppl 3):S215–S218. doi: 10.1007/s10545-010-9096-4. [DOI] [PubMed] [Google Scholar]
- 8.Choi J, Ko JM, Kim GH, Yoo HW. Clinical manifestation and effect of corn starch on height growth in Korean patients with glycogen storage disease type Ia. J Korean Soc Pediatr Endocrinol. 2007;12:35–40. [Google Scholar]
- 9.Beauchamp NJ, Taybert J, Champion MP, Layet V, Heinz-Erian P, Dalton A, et al. High frequency of missense mutations in glycogen storage disease type VI. J Inherit Metab Dis. 2007;30:722–734. doi: 10.1007/s10545-007-0499-9. [DOI] [PubMed] [Google Scholar]
- 10.Moses SW, Parvari R. The variable presentations of glycogen storage disease type IV: a review of clinical, enzymatic and molecular studies. Curr Mol Med. 2002;2:177–188. doi: 10.2174/1566524024605815. [DOI] [PubMed] [Google Scholar]
- 11.Ban HR, Kim KM, Jang JY, Kim GH, You HW, Kim K, et al. Living donor liver transplantation in a Korean child with glycogen storage disease type IV and a GBE1 mutation. Gut Liver. 2009;3:60–63. doi: 10.5009/gnl.2009.3.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brushia RJ, Walsh DA. Phosphorylase kinase: the complexity of its regulation is reflected in the complexity of its structure. Front Biosci. 1999;4:D618–D641. doi: 10.2741/brushia. [DOI] [PubMed] [Google Scholar]
- 13.Rudolfová J, Slovácková R, Trbusek M, Pesková K, St'astná S, Kozák L. Identification of three novel mutations in the PHKA2 gene in Czech patients with X-linked liver glycogenosis. J Inherit Metab Dis. 2001;24:85–87. doi: 10.1023/a:1005635629149. [DOI] [PubMed] [Google Scholar]
- 14.Hidaka F, Sawada H, Matsuyama M, Nunoi H. A novel mutation of the PHKA2 gene in a patient with X-linked liver glycogenosis type 1. Pediatr Int. 2005;47:687–690. doi: 10.1111/j.1442-200x.2005.02131.x. [DOI] [PubMed] [Google Scholar]
- 15.Bak H, Cordato D, Carey WF, Milder D. Adult-onset exercise intolerance due to phosphorylase b kinase deficiency. J Clin Neurosci. 2001;8:286–287. doi: 10.1054/jocn.1999.0230. [DOI] [PubMed] [Google Scholar]
- 16.Morava E, Wortmann SB, van Essen HZ, Liebrand van Sambeek R, Wevers R, van Diggelen OP. Biochemical characteristics and increased tetraglucoside excretion in patients with phosphorylase kinase deficiency. J Inherit Metab Dis. 2005;28:703–706. doi: 10.1007/s10545-005-0095-9. [DOI] [PubMed] [Google Scholar]