Abstract
Aims
To characterize patient radiation doses from nuclear myocardial perfusion imaging (MPI) and the use of radiation-optimizing ‘best practices’ worldwide, and to evaluate the relationship between laboratory use of best practices and patient radiation dose.
Methods and results
We conducted an observational cross-sectional study of protocols used for all 7911 MPI studies performed in 308 nuclear cardiology laboratories in 65 countries for a single week in March–April 2013. Eight ‘best practices’ relating to radiation exposure were identified a priori by an expert committee, and a radiation-related quality index (QI) devised indicating the number of best practices used by a laboratory. Patient radiation effective dose (ED) ranged between 0.8 and 35.6 mSv (median 10.0 mSv). Average laboratory ED ranged from 2.2 to 24.4 mSv (median 10.4 mSv); only 91 (30%) laboratories achieved the median ED ≤ 9 mSv recommended by guidelines. Laboratory QIs ranged from 2 to 8 (median 5). Both ED and QI differed significantly between laboratories, countries, and world regions. The lowest median ED (8.0 mSv), in Europe, coincided with high best-practice adherence (mean laboratory QI 6.2). The highest doses (median 12.1 mSv) and low QI (4.9) occurred in Latin America. In hierarchical regression modelling, patients undergoing MPI at laboratories following more ‘best practices’ had lower EDs.
Conclusion
Marked worldwide variation exists in radiation safety practices pertaining to MPI, with targeted EDs currently achieved in a minority of laboratories. The significant relationship between best-practice implementation and lower doses indicates numerous opportunities to reduce radiation exposure from MPI globally.
Keywords: Nuclear cardiology, SPECT, PET, Radiation dose, Best practices, Quality of care
See page 1649 for the editorial comment on this article (doi:10.1093/eurheartj/ehv160)
Introduction
Nuclear myocardial perfusion imaging (MPI) is a non-invasive diagnostic test widely used to diagnose coronary artery disease,1 stratify risk,2 predict outcomes,3 guide patient management,4 and control costs.5 Reflecting these benefits, MPI volume has grown rapidly worldwide over the past two decades, to 15–20 million procedures annually6 and diffusion of technology and expertise has led to its continued adoption across the developing world. However, significant concerns have been raised over radiation-related cancer risk from cardiac imaging7–10 and, in particular, the radiation burden from MPI. While considerable worldwide variation exists in the frequency of MPI use,11 in some settings, such as the USA, it is the medical test with the highest per capita radiation dose.9,12,13 Estimation of risk from ionizing radiation is difficult, since no prospective trials focusing on adverse events of radiation with doses used in diagnostic procedures have ever been performed.28 A variety of protocols can be used to perform MPI14,15 on single-photon emission computed tomography (SPECT) and positron emission tomography (PET) cameras, and a variety of approaches and ‘best practices’ have been developed to lower radiation exposures to patients. While preliminary single-country data suggest that radiation safety technique is frequently suboptimal,16 the worldwide use of strategies that may reduce dose has never been characterized. A better understanding of current practice would offer opportunities to identify areas to improve quality of care and to reduce disparities, which in turn would decrease the global radiation burden from MPI. Thus, we undertook to characterize worldwide nuclear cardiology practice and its impact on radiation exposure to patients and populations, including variation in radiation doses and the use of ‘best practices’ and dose-lowering techniques.
Methods
Study design and survey conduct
A needs assessment expert meeting was organized by the International Atomic Energy Agency (IAEA) in 2012 and identified knowledge of worldwide MPI protocols and practices as an important priority. We conducted a cross-sectional study in centres performing MPI. We obtained contact details of nuclear cardiology laboratories and practitioners from databases provided by national and international organizations (see Supplementary material online, Methods), and from designated INCAPS regional coordinators. On 15 March 2013, the IAEA contacted potential sites and requested that they participate voluntarily in a study aimed at identifying what laboratories ‘around the world [are] doing in terms of tracer utilization, doses used and technology that is available’ based on a consecutive series of patients over 1 week, chosen by the respondent, between the weeks beginning 19 March and 22 April, inclusive. The study was approved by the Columbia University Institutional Review Board, which declared it exempt from the requirements of US federal regulations for the protection of human subjects (45 CFR 46) since the study collected no individually identifiable health information.
Data collection instrument
A standardized data collection instrument was emailed to all potential participants. A local investigator at each site provided information on laboratory demographics, as well as patient demographics and clinical characteristics for each MPI study completed during the selected week, including the patient's age, gender, and weight, radiopharmaceuticals used and injected activities, camera type, patient positioning, additional scanning (CT or nuclear) performed for attenuation correction, and hardware and software used that improves camera efficiency. Data were checked for omissions and errors, and sites contacted when clarification was required; all sites responded and successfully addressed these concerns.
Radiation dose estimation
Radiation exposure was quantified by the effective dose (ED), a whole-body measure reflecting the dose to each organ and its relative sensitivity to the deleterious effects of radiation. ED was calculated for each patient based on the radiopharmaceutical(s) administered and their activities (MBq), using the most recent dosimetry as specified by the International Commission on Radiological Protection.17,18 For rubidium-82, ED was calculated according to the approach of Senthamizhchelvan.19 Achievement of median ED ≤9 mSv, a target established in professional society recommendations,20 was evaluated for each laboratory.
Best practices quality index
Acquired data were used to determine each laboratory's adherence to eight ‘best practices’ with bearing on radiation exposure, based on current clinical practice guidelines.14,15,21 These criteria (Table 1) were determined, prior to data analysis, by a committee of expert physicians and medical physicists convened by IAEA, charged with identifying the critical, measurable practices that impact and optimize radiation dose from MPI. The core elements identified by the panel included practices such as avoiding administering too much isotope, avoiding higher dose isotopes (viz. thallium-201), and using newer technologies that can lower radiation doses.
Table 1.
Definitions of the eight best practices
| 1. Avoid thallium stress: No thallium stress tests were performed in patients ≤70 years old. SPECT MPI performed with thallium-201 is associated with a considerably higher radiation dose to patients than when it is performed with technetium-99m.29 This excludes thallium rest-redistribution viability studies and stress-redistribution-reinjection stress-and-viability studies. |
| 2. Avoid dual isotope: No dual isotope (rest thallium and stress technetium) stress tests were performed in patients ≤70 years old. Dual isotope MPI is associated with the highest radiation dose of any protocol.29 |
| 3. Avoid too much technetium: No study was performed with administered activity >1332 MBq (36 mCi) for an injection of technetium, and mean total effective dose was <15 mSv for all studies using just technetium injections. 1332 MBq is the highest recommended activity in guidelines,15 and 15 mSv is a high radiation dose for a study using technetium-99m. |
| 4. Avoid too much thallium: For each nuclear stress test involving thallium, no more than 129.5 MBq (3.5 mCi) was administered at stress. The expert committee maintained that no more than this activity is needed for patients who are good candidates to receive thallium MPI. |
| 5. Perform stress-only imaging: The laboratory performed at least one stress-only study, in which rest imaging was omitted, or the laboratory only does PET-based stress tests. If stress images are completely normal, subsequent rest imaging can be avoided to reduce radiation dose by up 80%. PET MPI studies have low radiation dose, the dosimetric advantage of stress-only is less, and there is less evidence regarding stress-only PET MPI. |
| 6. Use camera-based dose-reduction strategies: The laboratory performed at least one study using at least one of the following: (i) attenuation correction (CT or line source), (ii) imaging patients in multiple positions, e.g. both supine and prone, (iii) high-technology software (e.g. incorporating iterative reconstruction, resolution recovery, and noise reduction), and (iv) high-technology hardware (e.g. PET, a high-efficiency solid-state SPECT camera, or a cardiac-focused collimator). Each of these approaches reduces the radiation dose needed or facilitates performance of stress-only imaging. |
| 7. Weight-based dosing for technetium: The laboratory had a statistically significant positive correlation between patient weight and administered activity (MBq), for injections of technetium. Tailoring the administered activity to the patient size offers an opportunity to reduce radiation dose. |
| 8. Avoid inappropriate dosing that can lead to ‘shine through’ artefact: The laboratory performed no SPECT MPI studies with technetium rest and stress injections on the same day, in which activity of the second injection was <3× that of the first injection. Shine through occurs in two injection, single-day technetium studies when residual radioactivity from the first injection interferes with interpretation of images for the second injection. To avoid shine through, it is recommended in guidelines that the activity (mCi or MBq) imaged for the second injection be at least three to four times that of the first injection; in some cases, this can be achieved with a second injection that has less than four times the activity by waiting for some of the technetium-99 m to decay. Reflecting guidelines, we considered a second injection of less than three times the activity of the first injection to constitute dosing that can lead to shine through.14,15,21,30 |
A committee of international experts convened at the IAEA, including physicians and medical physicists, developed these criteria to be applied to nuclear cardiology laboratories.
SPECT, single-photon emission computed tomography; MPI, myocardial perfusion imaging; MBq, megabecquerel; mCi, millicurie; PET, positron emission tomography; CT, computed tomography.
The panel also a priori devised a best practices quality index (QI), defined as the number (0–8) of best practices adhered to by a laboratory during the specified week; a QI score of ≥6 was pre-specified by the panel, prior to data analysis, as a desirable level.
Statistical methods
We calculated radiation dose (ED) for each patient and QI score for each laboratory as above. Continuous variables were described in terms of means (±standard deviation) and medians (interquartile range; IQR), and compared using analysis of variance and Kruskal–Wallis tests, respectively. Categorical variables were compared using χ2 tests. Comparisons were performed at the world regional level. World regions were defined as Africa, Asia, Europe, Latin America (including Mexico, Central and South America), North America (Canada and United States), and Oceania (Australia and New Zealand).
Hierarchical linear regression models were developed to determine if laboratory adherence to best practices was associated with patient ED, adjusting for patient clustering by laboratory and country. Model regression coefficients correspond to the expected change in ED associated with adherence to a specific best practice. The eight best practices were included as independent variables (fixed factors), and treated as dichotomous (laboratory adherence: yes/no). The intercept was defined as a random factor. The dependent variable was patient ED (mSv). We performed analyses with and without adjustment for patient age, gender, and weight. Additional linear regression models were developed to evaluate the impact of laboratory characteristics on QI. Independent variables included laboratory procedure volume (continuous variable), world region (categorical with Europe as reference category), and the laboratory's country's World Bank income level22 (low/low-middle (reference) vs. high-middle vs. high). Correlations between model variables were assessed using Pearson's φ. A two-tailed P < 0.05 was considered significant for all statistical tests. All analyses were performed using Stata/SE 13.1 (StataCorp, College Station, TX, USA).
Results
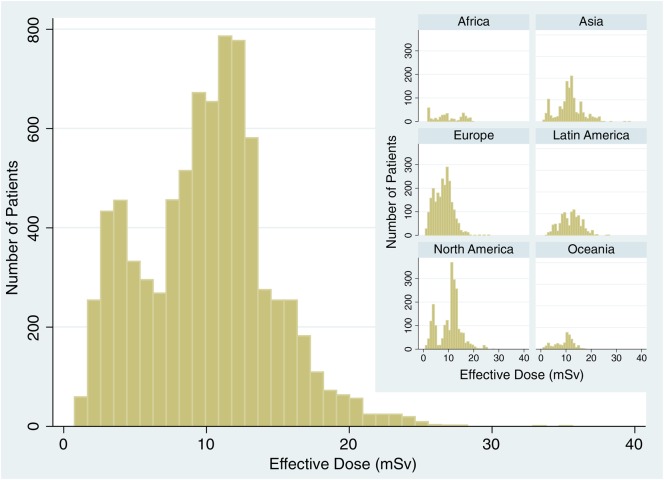
Data were collected on all 7911 patients undergoing MPI in 308 laboratories in 65 countries, during the specified 1-week period. Mean patient age was 64.1 ± 12.0 years, and 41% were female. Mean ED for all patients was 10.0 ± 4.5 mSv. The distribution of patient ED showed a slight positive skew, with 978 patients (12%) receiving an estimated ED of >15 mSv (Figure 1). Both mean and median ED differed between laboratories (see Supplementary material online, Table S1), countries (see Supplementary material online, Table S2), and world regions (P < 0.001 for each). Worldwide, only 30% of laboratories had median ED ≤9 mSv. Adherence to best practices (Table 2) varied markedly between laboratories (mean QI score 5.4 ± 1.3), countries (see Supplementary material online, Table S2), and world regions (Table 3). Only 46% of laboratories adhered to six or more best practices.
Figure 1.
Worldwide distribution of patient radiation effective doses from myocardial perfusion imaging. Inset displays the distribution of patient effective doses by region.
Table 2.
Best practice adherence by region
| Number (%) of laboratories adhering to best practice |
||||||||
|---|---|---|---|---|---|---|---|---|
| Africa | Asia | Europe | Latin America | North America | Oceania | Total | P-Value | |
| Laboratories | 12 | 69 | 102 | 36 | 55 | 34 | 308 | n/a |
| Best practices | ||||||||
| Avoid thallium stress | 12 (100) | 52 (75) | 97 (95) | 35 (97) | 55 (100) | 31 (91) | 282 (92) | <0.001 |
| Avoid dual isotope | 12 (100) | 64 (93) | 101 (99) | 34 (94) | 53 (96) | 34 (100) | 298 (97) | 0.2 |
| Avoid too much technetium | 11 (92) | 64 (93) | 101 (99) | 23 (64) | 33 (60) | 31 (91) | 263 (85) | <0.001 |
| Avoid too much thallium | 12 (100) | 68 (99) | 102 (100) | 35 (97) | 55 (100) | 34 (100) | 306 (99) | 0.48 |
| Perform stress-only imaging | 8 (67) | 16 (23) | 47 (46) | 7 (19) | 9 (16) | 6 (18) | 93 (30) | <0.001 |
| Use camera-based dose-reduction strategies | 8 (67) | 48 (70) | 71 (70) | 16 (44) | 33 (60) | 30 (88) | 206 (67) | 0.005 |
| Weight-based dosing for technetium | 6 (50) | 8 (12) | 48 (47) | 11 (31) | 10 (18) | 5 (15) | 88 (29) | <0.001 |
| Avoid ‘shine through’ | 7 (58) | 26 (38) | 66 (65) | 14 (39) | 8 (15) | 15 (44) | 136 (44) | <0.001 |
Table 3.
Demographics, radiation burden, and adherence to best practices by world region
| Africa | Asia | Europe | Latin America | North America | Oceania | Total | P-Value | |
|---|---|---|---|---|---|---|---|---|
| Countries | 6 | 18 | 27 | 10 | 2 | 2 | 65 | n/a |
| Laboratories | 12 | 69 | 102 | 36 | 55 | 34 | 308 | n/a |
| Patients/lab, mean (SD) | 29.0 (23.7) | 21.3 (23.9) | 23.3 (32.8) | 31.6 (37.7) | 38.9 (38.8) | 12.9 (9.8) | 25.7 (31.6) | 0.002 |
| Patients/lab, median (IQR) | 19 (10–48) | 15 (6–29) | 15 (8–28) | 12 (8–42) | 31 (14–46) | 9.5 (6–17) | 16 (8–33) | <0.001 |
| Average ED (mSv), mean (SD) | 9.3 (3.9) | 11.7 (4.1) | 8.7 (3.1) | 13.0 (2.8) | 12.0 (3.6) | 10.3 (2.4) | 10.7 (3.7) | <0.001 |
| Average ED (mSv), median | 9.4 | 11.4 | 8.8 | 12.8 | 12.1 | 11.4 | 10.9 | <0.001 |
| Average ED (mSv), IQR | 6.3–13.6 | 9.7–13.0 | 6.3–10.8 | 11.3–14.9 | 9.5–13.3 | 9.4–11.7 | 8.4–12.9 | n/a |
| Average ED (mSv), range | 3.5–15.2 | 2.2–21.5 | 3.1–18.0 | 7.8–18.6 | 3.7–24.4 | 3.1–14.3 | 2.2–24.4 | n/a |
| Number with median ED ≤9 mSv | 5 (42%) | 12 (17%) | 52 (51%) | 4 (11%) | 11 (20%) | 7 (21%) | 91 (30%) | <0.001 |
| QI score, mean (SD) | 6.3 (1.2) | 5.0 (1.1) | 6.2 (1.2) | 4.9 (1.0) | 4.7 (1.2) | 5.5 (0.7) | 5.4 (1.3) | 0.02 |
| QI score, median (IQR) | 6.5 (5.5–7) | 5 (4–6) | 6 (5–7) | 5 (4–5) | 5 (4–6) | 6 (5–6) | 5 (5–6) | <0.001 |
| QI score | ||||||||
| 2 | 0 | 0 | 0 | 1 (3%) | 1 (2%) | 0 | 2 (1%) | |
| 3 | 0 | 4 (6%) | 0 | 0 | 11 (20%) | 0 | 15 (5%) | |
| 4 | 1 (8%) | 18 (26%) | 10 (10%) | 12 (33%) | 12 (22%) | 3 (9%) | 56 (18%) | |
| 5 | 2 (17%) | 29 (42%) | 20 (20%) | 15 (42%) | 14 (25%) | 13 (38%) | 93 (30%) | |
| 6 | 3 (25%) | 12 (17%) | 28 (27%) | 6 (17%) | 16 (29%) | 17 (50%) | 82 (27%) | |
| 7 | 4 (33%) | 3 (4%) | 27 (26%) | 2 (5%) | 1 (2%) | 1 (3%) | 38 (12%) | |
| 8 | 2 (17%) | 3 (4%) | 17 (17%) | 0 | 0 | 0 | 22 (7%) | |
| Number with ≥6 best practices | 9 (75%) | 18 (25%) | 72 (71%) | 8 (22%) | 17 (31%) | 18 (53%) | 142 (46%) | <0.001 |
| Patients | 348 | 1469 | 2381 | 1139 | 2135 | 439 | 7911 | n/a |
| Female | 135 (39%) | 559 (38%) | 949 (40%) | 492 (43%) | 921 (43%) | 198 (45%) | 3254 (41%) | 0.005 |
| Age, mean (SD) | 60.2 (11.0) | 61.8 (12.5) | 65.3 (11.1) | 62.4 (11.5) | 65.8 (12.3) | 65.4 (12.6) | 64.1 (12.0) | <0.001 |
| Weight (kg), mean (SD) | 81.2 (15.8) | 71.6 (15.7) | 80.0 (16.7) | 77.8 (16.0) | 87.2 (21.5) | 83.0 (20.1) | 80.2 (18.7) | <0.001 |
| ED (mSv), mean (SD) | 9.7 (5.5) | 11.4 (4.8) | 7.9 (3.5) | 11.8 (4.1) | 10.5 (4.5) | 9.3 (3.7) | 10.0 (4.5) | <0.001 |
| ED (mSv), median | 9.1 | 11.4 | 8.0 | 12.1 | 11.4 | 10.1 | 10.2 | <0.001 |
| ED (mSv), IQR | 5.1–15.6 | 9.2–13.5 | 5.1–10.1 | 8.4–14.6 | 8.0–12.9 | 6.5–11.7 | 6.7–12.7 | n/a |
| ED (mSv), range | 1.8–20.0 | 1.0–35.6 | 0.8–25.9 | 2.2–27.1 | 0.9–28.1 | 0.9–17.9 | 0.8–35.6 | n/a |
| Number with ED ≤9 mSv | 173 (50%) | 358 (24%) | 1420 (60%) | 304 (27%) | 649 (30%) | 161 (37%) | 3065 (39%) | <0.001 |
| Stress-only tests | 109 (31%) | 272 (19%) | 461 (19%) | 54 (4.7%) | 54 (2.5%) | 55 (13%) | 1005 (13%) | <0.001 |
Quality index (QI) is the number of best practices adhered to by a laboratory. Mean and median QI values are based on laboratory scores in each region. Effective dose (ED) mean and median estimates are based on patient estimates in each region.
NC, nuclear cardiology; SD, standard deviation; IQR, interquartile range.
Regional variation
The burden of radiation to patients undergoing MPI differed between world regions (Figure 1). Europe had both the lowest mean (7.9 mSv) and median (8.0 mSv) ED, and the highest proportion of patients with ED ≤9 mSv (60%). Latin America and Asia had the highest doses (mean of 11.8 and 11.4 mSv, respectively) and the second lowest proportion of patients with ED ≤9 mSv (27% and 24%, respectively). Europe was also among the highest in adherence to best practices with a mean laboratory QI of 6.2; ∼71% of laboratories adhered to six or more best practices (Table 3). North America had the lowest mean laboratory QI score (4.7), and was among the lowest in proportion of laboratories with ≥6 best practices (31%).
Laboratory radiation burden and adherence to best practices
Based on the regression analysis, undergoing a procedure at a laboratory that adhered to each of the best practices was associated with significantly lower patient ED. The only exceptions were laboratory adherence to avoiding ‘too much thallium’ and avoiding inappropriate dosing that can lead to ‘shine through’ (i.e. best practices 4 and 8 in Table 1, respectively). This relationship was maintained even after adjustment for patient age, gender, and weight. Laboratory avoidance of dual isotope use in patients under 70 years old was associated with the largest reduction in ED (5.4 mSv). The results of the hierarchical regression model adjusted for age, gender, and weight are presented in Table 4. Pairwise correlations between QIs were low; |φ| was <0.1 for most correlations and no more than 0.35 for any pair.
Table 4.
Relationship between laboratory best-practice adherence and predicted patient effective dose of radiation
| Best practice/factor | Reduction in predicted effective dose (mSv) | 95% confidence interval | Standard error | P-Value |
|---|---|---|---|---|
| Avoid thallium stress | 2.54 | 1.39 to 3.69 | 0.58 | <0.001 |
| Avoid dual isotope | 5.42 | 3.77 to 7.06 | 0.84 | <0.001 |
| Avoid too much technetium | 3.12 | 2.19 to 4.06 | 0.48 | <0.001 |
| Avoid too much thallium | 1.05 | −2.81 to 4.91 | 1.97 | 0.595 |
| Perform stress-only imaging | 2.28 | 1.57 to 2.98 | 0.36 | <0.001 |
| Use camera-based dose-reduction strategies | 1.23 | 0.58 to 1.88 | 0.33 | <0.001 |
| Weight-based dosing for technetium | 0.84 | 0.13 to 1.57 | 0.37 | 0.021 |
| Avoid ‘shine through’ | −1.03 | −1.66 to −0.39 | 0.32 | 0.002 |
| Age (years) | −0.004 | −0.009 to 0.001 | 0.003 | 0.142 |
| Female | 0.30 | 0.18 to 0.43 | 0.06 | <0.001 |
| Weight (kg) | −0.04 | −0.04 to −0.03 | 0.002 | <0.001 |
| Intercept (predicted effective dose, mSv) | 20.5 | 16.5 to 24.5 | 2.05 | <0.001 |
Results of the final hierarchical regression model.
A univariable regression model showed that World Bank income level was not associated with laboratory QI score, and thus it was not included in the multivariable model. Laboratory volume, while statistically significant, showed an extremely small effect in relation to QI (i.e. increase of 0.07 in QI for every 10 patients; P < 0.001). Relative to Europe, each of the regions except Africa was a significant predictor of a lower laboratory QI score (P < 0.01). However, these predictors together explained <30% of the variance in laboratory QI score (R2 = 0.28).
Discussion
The IAEA-sponsored INCAPS study found that while the worldwide median laboratory radiation dose from MPI was 10.9 mSv, equivalent to over 4 years of natural background radiation,5 this ranged over an order of magnitude (2.2–24.4 mSv) depending on the laboratory, and fewer than a third of laboratories achieved a median ED ≤9 mSv as recommended in professional society guidelines. Moreover, adherence to radiation safety best practices was incomplete among the laboratories observed. Only three of the eight best practices were adopted by at least 90% of laboratories, and only 7% of laboratories adhered to all eight best practices. Thus, almost all laboratories have the potential to increase the number of best practices used. Each best practice can be easily adopted, at least in some form, with no additional resource requirements, and some may even reduce resources required, e.g. the amount of radiopharmaceutical used as well as staff and scanner time in the case of stress-only studies.
Of the individual best practices, performing stress-only studies where possible and using weight-based dosing for Tc-99m studies, were the two areas with lowest adherence worldwide and thus the greatest potential for improvement among laboratories. Stress-only technetium imaging has gained particular emphasis in recent professional guidelines, and can be performed with no special requirements in terms of technology or isotopes. It entails performing stress imaging first and then omitting the higher dose rest images in a patient with completely normal stress images. This reduces radiation dose by up to 80% while maintaining diagnostic utility, and has been validated in clinical studies involving over 20 000 patients.23 We observed stress-only imaging, to be performed in only 30% of laboratories worldwide, and only 13% of MPI studies, despite its having the potential to impact ED for the majority of patients with low-risk MPI findings. We noted a similarly low proportion of laboratories performing weight-based dosing, i.e. adjusting administered Tc-99m activity to reflect patient weight.
Of the eight best practices, two were not associated with lower patient ED in the multivariable model. Only two laboratories did not adhere to avoidance of ‘too much thallium,’ and thus our study was not powered to reveal its effect. Avoidance of inappropriate dosing that can lead to ‘shine through’ artefact was shown to increase patient ED. While this serves as a best practice impacting on ED, the expert panel included it despite a priori not expecting it be associated with lower dose. To avoid shine through, which compromises MPI image interpretation, guidelines recommend that activity for the second injection be sufficiently high to minimize the impact of residual counts on images (Table 1). Accordingly, while avoidance of shine through is an important dose-related best practice, its implementation in fact entails administration of a higher activity and hence higher dose.
INCAPS found lower ED among patients who underwent MPI in laboratories adhering to more of the specified best practices, thereby providing validation of these practices. This relationship also suggests the importance of developing, validating, and implementing strategies that increase adherence to best practices. Potential approaches include educational interventions targeting laboratory-specific deficiencies in best practices, linking their use to reimbursement and laboratory accreditation, public reporting of QIs, and the use of checklists.24 Such strategies can be realized by laboratories working in partnership with organizations such as the IAEA, professional societies, and regulatory agencies.
We observed significant differences in both ED and QI between countries and world regions. World regions where average patient EDs were lowest also showed the highest rates of laboratory adherence to best practices. For example, the lowest median ED (8.0 mSv) and highest proportion of laboratories with median ED ≤9 mSv occurred in Europe, which had the second highest regional best practice adherence (mean laboratory QI 6.2) and was home to more than three quarters of all laboratories observed worldwide with perfect QI scores of 8. The highest median radiation dose (12.1 mSv) and lowest proportion of laboratories with median ED ≤9 mSv (11%) occurred in Latin America, which also had the lowest proportion of laboratories with QI score of at least 6. North American laboratories also performed poorly in terms of mean ED and QIs.
Regional differences in utilization of some best practices contributed in part to the marked regional differences in MPI radiation dose. For example, the use of stress-only imaging was performed in 67% of the limited number (12) of African laboratories and in 46% of European laboratories, but only in 16–23% of laboratories in the other world regions. Camera-based dose-reduction strategies were used in 88% of laboratories in Oceania, and 60–70% of laboratories in other world regions, except for Latin American, where usage was only 44%. These comprise a variety of practices (Table 1), including the use of recent technological approaches which can maintain image quality while reducing ED to a fraction of that with standard protocols, but may be too costly for many laboratories. They also include combined prone and supine imaging, which can be performed with virtually any standard SPECT camera, and attenuation correction; both facilitate performance of stress-only imaging. Interestingly, the use of camera-based dose-reduction strategies was by far the highest in Oceania, where additional reimbursement is provided for CT-based attenuation correction. The impact of economic factors on best-practice utilization and on ED requires further study.
As the global burden of cardiovascular disease grows and redistributes to the developing world,25 increased utilization of cardiovascular procedures involving ionizing radiation, such as MPI, can dramatically influence radiation exposure to populations and hence potentially influence cancer morbidity and mortality. The significant geographical variation observed here in radiation doses and best practice use points to numerous opportunities, tailored to the laboratory and population of interest, to reduce the global burden of ionizing radiation from MPI and its associated cancer risk. For example, although radiation doses in Oceania were lower than the world average, utilization of stress-only imaging and weight-based dosing was very low. Future efforts in this population could focus on these best practices.
Our study is not without limitations. First, the extent to which participating INCAPS laboratories are representative of all nuclear cardiology laboratories worldwide is unknown. Since the data collection instrument was distributed through multiple channels with overlapping constituencies, and no reliable statistics exist regarding the number of nuclear cardiology laboratories worldwide, it was not possible for us to identify the response rate to our request for data. Respondents to a request for data from the IAEA may well represent a subset of laboratories with a better distribution of best practice use than that of all laboratories worldwide. In some parts of the world, for example in Russia, despite substantial efforts we had difficulty obtaining laboratory participation, and country-level ED and QI estimates may be more prone to sampling error when few laboratories were surveyed. Nevertheless, we believe that IAEA's extensive worldwide network, and our intensive outreach efforts, led to the broadest possible worldwide participation in INCAPS, thus making our findings widely generalizable. Secondly, our analysis is based on data collected over a limited timeframe that may not be completely representative of laboratories' practice. Thirdly, there are rare clinical scenarios where non-adherence to some of the best practices identified by our expert panel is warranted. For example, the lifetime probability of radiation-attributable cancer from MPI is exceedingly small in patients with low life expectancy,26 and the use of higher doses may be warranted in such patients. Even so, we believe that the components of the QI are generally valid and that, notwithstanding such exceptions, a laboratory paying careful attention to radiation safety practices will invariably have a high QI score. Nevertheless, caution should be exercised in interpreting a QI score in terms of predicted radiation dose, since in calculating the QI, its components are not weighted in terms of impact on radiation dose, and thus an identical score may have different implications in terms of ED depending on the particular best practices used. Fourthly, our study focused by design on radiation dose optimization, not on justification or appropriateness of MPI examinations performed; avoiding inappropriate examinations is a complementary approach to minimizing population radiation burdens.27 Finally, INCAPS did not assess image quality and thus the relationships between radiation best practices and radiation dose, and MPI image quality, could not be evaluated.
While MPI conveys numerous benefits, it exposes patients to ionizing radiation.7,10,28 In the INCAPS study of worldwide nuclear cardiology practices, only a minority of laboratories achieved targeted radiation dose levels. Adherence to radiation safety best practices varied significantly between laboratories and world regions, however, patients undergoing procedures at laboratories adhering to best practices received significantly lower radiation doses. This relationship offers numerous opportunities to improve best practice use and thereby reduce radiation exposure from MPI across the globe.
Supplementary material
Supplementary material is available at European Heart Journal online.
Funding
This work was supported by the International Atomic Energy Agency, the Margaret Q. Landenberger Research Foundation, and the Irving Scholars Program (A.J.E.). Funding to pay the Open Access publication charges for this article was provided by the International Atomic Energy Agency.
Conflict of interest: Dr A.J.E. has received research grants for other investigator-initiated studies from GE Healthcare, Philips Healthcare, and Spectrum Dynamics. Dr P.A.K. receives an institutional research contract from GE Healthcare.
Acknowledgements
The authors thank the members of the INCAPS Investigators Group (see Supplementary material online, Appendix), and their institutions, for efforts in collecting data, and the cooperating professional societies, including the American Society of Nuclear Cardiology, Asian Regional Cooperative Council for Nuclear Medicine, Australian and New Zealand Society of Nuclear Medicine, British Nuclear Medicine Society/British Nuclear Cardiology Society, Comissão Nacional de Energia Nuclear, European Association of Nuclear Medicine, European Council of Nuclear Cardiology, IAEA, and Intersocietal Accreditation Commission.
References
- 1.Jaarsma C, Leiner T, Bekkers SC, Crijns HJ, Wildberger JE, Nagel E, Nelemans PJ, Schalla S. Diagnostic performance of noninvasive myocardial perfusion imaging using single-photon emission computed tomography, cardiac magnetic resonance, and positron emission tomography imaging for the detection of obstructive coronary artery disease: a meta-analysis. J Am Coll Cardiol 2012;59:1719–1728. [DOI] [PubMed] [Google Scholar]
- 2.Metz LD, Beattie M, Hom R, Redberg RF, Grady D, Fleischmann KE. The prognostic value of normal exercise myocardial perfusion imaging and exercise echocardiography: a meta-analysis. J Am Coll Cardiol 2007;49:227–237. [DOI] [PubMed] [Google Scholar]
- 3.Abraham A, Nichol G, Williams KA, Guo A, deKemp RA, Garrard L, Davies RA, Duchesne L, Haddad H, Chow B, DaSilva J, Beanlands RS. 18F-FDG PET imaging of myocardial viability in an experienced center with access to 18F-FDG and integration with clinical management teams: the Ottawa-FIVE substudy of the PARR 2 trial. J Nucl Med 2010;51:567–574. [DOI] [PubMed] [Google Scholar]
- 4.Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2003;107:2900–2907. [DOI] [PubMed] [Google Scholar]
- 5. International Atomic Energy Agency. Nuclear Cardiology: Its Role in Cost Effective Care. IAEA Human Health Series No. 18. Vienna: International Atomic Energy Agency; 2012. [Google Scholar]
- 6.Einstein AJ. Multiple opportunities to reduce radiation dose from myocardial perfusion imaging. Eur J Nucl Med Mol Imaging 2013;40:649–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Einstein AJ, Knuuti J. Cardiac imaging: does radiation matter? Eur Heart J 2012;33:573–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hausleiter J, Meyer T, Hermann F, Hadamitzky M, Krebs M, Gerber TC, McCollough C, Martinoff S, Kastrati A, Schomig A, Achenbach S. Estimated radiation dose associated with cardiac CT angiography. JAMA 2009;301:500–507. [DOI] [PubMed] [Google Scholar]
- 9.Fazel R, Krumholz HM, Wang Y, Ross JS, Chen J, Ting HH, Shah ND, Nasir K, Einstein AJ, Nallamothu BK. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 2009;361:849–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Picano E, Vañó E, Rehani MM, Cuocolo A, Mont L, Bodi V, Bar O, Maccia C, Pierard L, Sicari R, Plein S, Mahrholdt H, Lancellotti P, Knuuti J, Heidbuchel H, Di Mario C, Badano LP. The appropriate and justified use of medical radiation in cardiovascular imaging: a position document of the ESC Associations of Cardiovascular Imaging, Percutaneous Cardiovascular Interventions and Electrophysiology. Eur Heart J 2014;35:665–672. [DOI] [PubMed] [Google Scholar]
- 11.Vitola JV, Shaw LJ, Allam AH, Orellana P, Peix A, Ellmann A, Allman KC, Lee BN, Siritara C, Keng FY, Sambuceti G, Kiess MC, Giubbini R, Bouyoucef SE, He ZX, Thomas GS, Mut F, Dondi M. Assessing the need for nuclear cardiology and other advanced cardiac imaging modalities in the developing world. J Nucl Cardiol 2009;16:956–961. [DOI] [PubMed] [Google Scholar]
- 12.Einstein AJ, Weiner SD, Bernheim A, Kulon M, Bokhari S, Johnson LL, Moses JW, Balter S. Multiple testing, cumulative radiation dose, and clinical indications in patients undergoing myocardial perfusion imaging. JAMA 2010;304:2137–2144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berrington de Gonzalez A, Kim KP, Smith-Bindman R, McAreavey D. Myocardial perfusion scans: projected population cancer risks from current levels of use in the United States. Circulation 2010;122:2403–2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hesse B, Tagil K, Cuocolo A, Anagnostopoulos C, Bardies M, Bax J, Bengel F, Busemann Sokole E, Davies G, Dondi M, Edenbrandt L, Franken P, Kjaer A, Knuuti J, Lassmann M, Ljungberg M, Marcassa C, Marie PY, McKiddie F, O'Connor M, Prvulovich E, Underwood R, van Eck-Smit B. EANM/ESC procedural guidelines for myocardial perfusion imaging in nuclear cardiology. Eur J Nucl Med Mol Imaging 2005;32:855–897. [DOI] [PubMed] [Google Scholar]
- 15.Henzlova MJ, Cerqueira MD, Mahmarian JJ, Yao SS. Stress protocols and tracers. J Nucl Cardiol 2006;13:e80–e90. [DOI] [PubMed] [Google Scholar]
- 16.Einstein AJ, Tilkemeier P, Fazel R, Rakotoarivelo H, Shaw LJ, American Society of Nuclear Cardiology. Radiation safety in nuclear cardiology-current knowledge and practice: results from the 2011 American Society of Nuclear Cardiology member survey. JAMA Int Med 2013;173:1021–1023. [DOI] [PubMed] [Google Scholar]
- 17. Radiological protection in cardiology. ICRP Publication 120. Ann ICRP 2013;42:1–125. [DOI] [PubMed] [Google Scholar]
- 18. Radiation dose to patients from radiopharmaceuticals: A fourth addendum to ICRP Publication 53. http://www.icrp.org/docs/Radiation%20Dose%20to%20Patients%20from%20Radiopharmaceuticals%20-%20A%20fourth%20addendum%20to%20ICRP%20Publication%2053.pdf. (25 November 2014).
- 19.Senthamizhchelvan S, Bravo PE, Esaias C, Lodge MA, Merrill J, Hobbs RF, Sgouros G, Bengel FM. Human biodistribution and radiation dosimetry of 82Rb. J Nucl Med 2010;51:1592–1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cerqueira MD, Allman KC, Ficaro EP, Hansen CL, Nichols KJ, Thompson RC, Van Decker WA, Yakovlevitch M. Recommendations for reducing radiation exposure in myocardial perfusion imaging. J Nucl Cardiol 2010;17:709–718. [DOI] [PubMed] [Google Scholar]
- 21. International Atomic Energy Agency. Nuclear Cardiology: Guidance and Recommendations for Implementation in Developing Countries. IAEA Human Health Series No. 23 Vienna: International Atomic Energy Agency; 2012. [Google Scholar]
- 22. World Bank. How we classify countries (2014 version) http://data.worldbank.org/about/country-classifications. (16 June 2014).
- 23.Chang SM, Nabi F, Xu J, Raza U, Mahmarian JJ. Normal stress-only versus standard stress/rest myocardial perfusion imaging: similar patient mortality with reduced radiation exposure. J Am Coll Cardiol 2010;55:221–230. [DOI] [PubMed] [Google Scholar]
- 24.Winters BD, Gurses AP, Lehmann H, Sexton JB, Rampersad CJ, Pronovost PJ. Clinical review: checklists—translating evidence into practice. Crit Care 2009;13:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moran AE, Forouzanfar MH, Roth GA, Mensah GA, Ezzati M, Murray CJ, Naghavi M. Temporal trends in ischemic heart disease mortality in 21 world regions, 1980 to 2010: the global burden of disease 2010 study. Circulation 2014;129:1483–1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brenner DJ, Shuryak I, Einstein AJ. Impact of reduced patient life expectancy on potential cancer risks from radiologic imaging. Radiology 2011;261:193–198. [DOI] [PubMed] [Google Scholar]
- 27.Einstein AJ. Radiation protection of patients undergoing cardiac computed tomographic angiography. JAMA 2009;301:545–547. [DOI] [PubMed] [Google Scholar]
- 28.Knuuti J, Bengel F, Bax JJ, Kaufmann PA, Le Guludec D, Perrone Filardi P, Marcassa C, Ajmone Marsan N, Achenbach S, Kitsiou A, Flotats A, Eeckhout E, Minn H, Hesse B. Risks and benefits of cardiac imaging: an analysis of risks related to imaging for coronary artery disease. Eur Heart J 2014;35:633–638. [DOI] [PubMed] [Google Scholar]
- 29.Einstein AJ, Moser KW, Thompson RC, Cerqueira MD, Henzlova MJ. Radiation dose to patients from cardiac diagnostic imaging. Circulation 2007;116:1290–1305. [DOI] [PubMed] [Google Scholar]
- 30.Depuey EG, Mahmarian JJ, Miller TD, Einstein AJ, Hansen CL, Holly TA, Miller EJ, Polk DM, Wann SL. Patient-centered imaging. J Nucl Cardiol 2012;19:185–215. [DOI] [PubMed] [Google Scholar]