Abstract
Background
Physician–nurse task shifting in primary care appeals greatly to health policymakers. It promises to address workforce shortages and demands of high-quality, affordable care in the healthcare systems of many countries. This systematic review was conducted to assess the evidence about physician–nurse task shifting in primary care in relation to the course of disease and nurses’ roles.
Methods
We searched MEDLINE, Embase, The Cochrane Library and CINAHL, up to August 2012, and the reference list of included studies and relevant reviews. All searches were updated in February 2014. We selected and critically appraised published randomized controlled trials (RCTs).
Results
Twelve RCTs comprising 22 617 randomized patients conducted mainly in Europe met the inclusion criteria. Nurse-led care was delivered mainly by nurse practitioners following structured protocols and validated instruments in most studies. Twenty-five unique disease-specific measures of the course of disease were reported in the 12 RCTs. While most (84 %) study estimates showed no significant differences between nurse-led care and physician-led care, nurses achieved better outcomes in the secondary prevention of heart disease and a greater positive effect in managing dyspepsia and at lowering cardiovascular risk in diabetic patients. The studies were generally small, of varying follow-up episodes and were at risk of biases. Descriptive details about roles, qualifications or interventions were also incomplete or not reported.
Conclusion
Trained nurses may have the ability to achieve outcome results that are at least similar to physicians’ for managing the course of disease, when following structured protocols and validated instruments. The evidence, however, is limited by a small number of studies reporting a broad range of disease-specific outcomes; low reporting standards of interventions, roles and clinicians’ characteristics, skills and qualifications; and the quality of studies. More rigorous studies using validated tools could clarify these findings.
Electronic supplementary material
The online version of this article (doi:10.1186/s12960-015-0049-8) contains supplementary material, which is available to authorized users.
Keywords: Systematic review, Physician–nurse substitution, Task shifting, Course of disease, Randomized controlled trials, Health policy
Resumen
Antecedentes
La transferencia de tareas del médico a profesionales de enfermería en atención primaria atrae enormemente a los legisladores de salud. Esta estrategia promete abordar la escasez de recursos humanos y demandas de atención asequible y de alta calidad en los sistemas de salud de muchos países. Realizamos una revisión sistemática para evaluar la evidencia sobre la transferencia de tareas médico-enfermería en atención primaria con relación al curso de la enfermedad y a las funciones de enfermería.
Métodos
Realizamos búsquedas en los registros de Medline, Embase, Cochrane Library y CINAHL, hasta Agosto del 2012; y en las listas de referencia de los estudios incluidos y de revisiones sistemáticas relevantes. Actualizamos las búsquedas en Febrero del 2014. Seleccionamos y realizamos una valoración crítica de los ensayos controlados aleatorios (ECA) ya publicados.
Resultados
Doce ECA realizados principalmente en Europa con 22 617 participantes asignados al azar reunieron los criterios de inclusión. Profesionales de enfermería, principalmente enfermeras médico, dieron el cuidado de atención, mayormente mediante el uso de protocolos estructurados e instrumentos validados. Se reportaron veinticinco medidas únicas del curso de la enfermedad. La mayoría (84 %) de éstas mostraron diferencias no significativas entre grupos, pero el profesional de enfermería consiguió tasas de pacientes significativamente mejores que el médico en la prevención secundaria de enfermedades cardiacas, un efecto positivo mayor en el manejo de dispepsia, y en la reducción del riesgo cardiovascular en pacientes diabéticos. Los estudios fueron generalmente pequeños, de seguimiento variado, y vulnerables a sesgos de selección, detección y deserción. Descripciones de las funciones, calificaciones e intervenciones no se reportan o son incompletas.
Conclusión
Profesionales de enfermería capacitados podrían obtener resultados de similitud al médico en el manejo del curso de la enfermedad, mediante el seguimiento de protocolos estructurados e instrumentos validados. La evidencia, sin embargo, se limita a un pequeño número de estudios que reportan una amplia gama de resultados de enfermedades específicas, y un bajo estándar en el reporte de intervenciones, características y funciones del profesional clínico, habilidades y calificaciones; y por la calidad de los estudios. Estudios con mejor calidad de métodos, que utilicen herramientas validadas podrían aclarar estos hallazgos.
Electronic supplementary material
The online version of this article (doi:10.1186/s12960-015-0049-8) contains supplementary material, which is available to authorized users.
Background
Chronic illness and disability are major contributing factors of morbidity and mortality worldwide. Long life spans and ageing populations are already imposing a major challenge for the infrastructures of healthcare systems [1]. These factors and patients’ expectations give rise to professional care-giving demands, consequently increasing the need for more activity in the community, ambulatory and primary care. There is currently a global shortage of 7.2 million physicians, nurses and midwives, however, and this number is estimated to increase to about 12.9 million by 2035 [2].
A popular approach to overcome this increasing shortage of human resources is task shifting, a process of delegation whereby tasks are moved to less specialized healthcare workers [3]. The strategy aims to efficiently and effectively reorganize the existing healthcare human resources to improve the distribution of workload, increase service capacity and reduce healthcare costs [4, 5]. Physician–nurse task shifting is carried out by transferring specific functions or tasks traditionally from the domain of physicians to nurses. Nurses are less costly to employ and train than physicians and are one of the largest groups of qualified healthcare providers [6]. In many countries, nurses are being granted more responsibilities and a wider range of clinical tasks [7]. This means that nurses might have a key role in medical areas where workforce shortages are a major health issue. Chronic conditions, for example, depend on resourceful caregiving, a long-term plan, continuous monitoring and adherence to disease management to achieve better health outcomes [8].
Two reviews suggested that nurses can provide same quality care and achieve as-good health outcomes as primary care physicians, but the volume and methodological quality of studies were insufficient [9, 10]. Measures of the course of disease such as symptoms, severity and complications were rarely reported. These measures help in monitoring the course of disease and treatment response and can have a major impact on patient outcomes; some may serve as surrogate measures of disease severity. We systematically reviewed the evidence on the effectiveness of physician–nurse task shifting in primary care in relation to measures of the course of disease and nurses’ roles.
Methods
The protocol of our review followed a population, intervention, comparison and outcome (PICO) approach [11] and the recommended guidelines [12] for the reporting of systematic reviews and meta-analyses (see Additional file 1).
Study identification
We searched MEDLINE (OVID), Embase (Elsevier), CINAHL (EBSCOHost) and The Cochrane Library of Systematic Reviews (Wiley) which includes the Cochrane Effective Practice and Organization of Care Group. The searches were not restricted by age, publication date or country and included a study design filter for randomized controlled trials (RCTs) and a combination of MeSH terms, text words, free text terms and synonyms for “primary care”, “skill mix”, “doctors”-“nurse” “substitution” (see Additional file 2). Additional publications were identified by manual searches of the reference lists of included studies and relevant reviews. All searches were carried out to cover publications from the inception of databases to August 2012 and were updated in February 2014.
Study inclusion and exclusion criteria
We included peer-reviewed RCTs published in English that examined task shifting from physicians to nurses in primary care (general practices, community or ambulatory care settings). Studies were eligible if care from family physicians, paediatricians and/or geriatricians was compared to care delivered by nurses (nurse-led care) in all roles under a task-shifting model of care and for patients of all ages and all conditions, and if studies reported outcome measures related to the course of disease including symptoms, severity and complications. We excluded measures of quality of life, satisfaction, mortality, hospital admissions, process of care or clinical parameters that were not surrogates of the course of disease.
We focused on a task-shifting approach by differentiating it from supplementation based on the framework from a Cochrane review [10]. Under task shifting, clearly delineated tasks or functions traditionally from the domain of physicians are transferred to nurses [3]. Nurses may receive specific or competency-based training to perform such tasks/functions and would deliver consultations with autonomous or delegated responsibility. Studies of task shifting thus compare the performance between nurses (as main figure of care) and physicians when both manage the same work or tasks in a similar capacity. In a supplementation approach, nurses complement the work of physicians or extend the range of services to improve the quality of care. Studies of supplementation compare nurses working alongside other clinicians (multi-professional service) with physicians working alone (uni-professional service). We excluded studies of supplementation.
Study selection and quality assessment
Two authors independently screened titles and abstracts and assessed the full text of eligible publications and the methodological features of included studies, resolving differences by consensus. Based on well-established guidelines [13], we assessed the methodological features of studies including core items of quality criteria that could influence the risk of bias (sequence and allocation concealment, blinding of participants, personnel and outcome assessors and intention to treat (ITT)). Following the debate about the validity of scores for the assessment of risk of bias [14, 15], we did not calculate a composite score. We describe the studies’ adequacy in each item with an overall judgement of the quality of evidence.
Data abstraction
Structured data collection forms were used independently by two authors to abstract the bibliographic details, population demographics, interventions (training competency, roles, type of care, clinical responsibility, use of guidelines, follow-up length) and outcome data (in all forms, for example, binary, continuous and/or semi-quantitative) including the length of consultations in minutes. Differences were resolved through consensus. Based on the studies’ description of interventions and competencies, we categorized nurses into the following: nurse practitioner (NP) or NP with additional degree/courses (NP+), for example, NP with Master degree; registered nurse (RN); or licensed nurse (LN). Outcomes were grouped according to disease area, for example, heart disease for heart failure and coronary heart disease. Data from a single study reported across various publications were extracted as one unit. Publications reporting more than one RCT were extracted as separate studies.
Data synthesis
Data were analysed based on the individual trial estimates. Using Review Manager (Version 5.1) [16], we calculated the unadjusted relative risks (RRs) or the weighted mean differences (WMDs) and 95 % confidence intervals (CI) of the absolute end points. There was mostly one study per outcome which precluded the ability to perform meta-analyses. We tabulated the effect sizes, and the results were synthesized narratively. We considered P < 0.05 to imply statistical significance. Following established techniques [17], standard deviations were estimated using the information from the studies’ statistical analyses.
Results
Study identification
Figure 1 shows the flow of study selection. Our literature searches identified 4 589 original records. Based on screening of titles and abstracts, 268 records were eligible for detailed examination of full-text publications; 44 of these were relevant for appraisal, but we excluded 27 for the reasons provided in Additional file 3. Twelve RCTs reported in 17 publications [18–34] met the inclusion criteria.
Fig. 1.
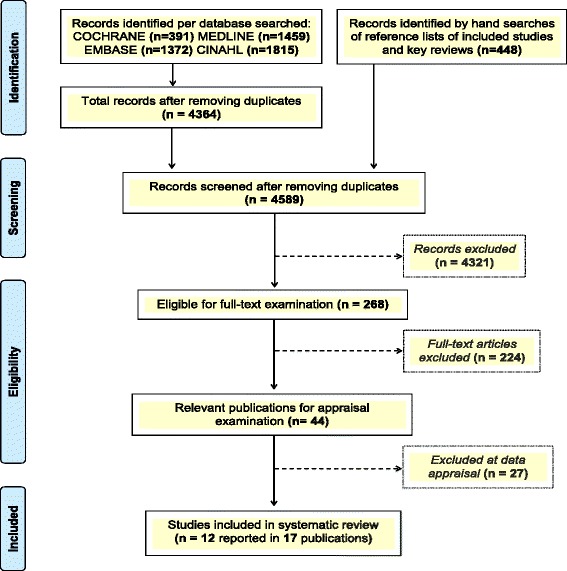
Illustration of the study selection process
Study and population characteristics
Table 1 provides the summary characteristics of studies in review including the study design, setting, population demographics and interventions (see Additional file 4 for a detailed description). The trials were conducted in the UK (n = 6), the Netherlands (n = 3), South Africa (n = 2) and Russia (n = 1). More than one follow-up episode was reported in a few cases; median of maximum follow-up was 6 (range: 0.5–48) months. The 12 trials comprised of 22 617 enrolled or randomized patients (range: 100–9 252); 4 had less than 200 patients (range: 100–175). Mean age in 10 trials and ranged from 35 (SD 9.63) to 69.5 (SD 10.6) years; median age was 27.6 (IQR: 9.0–44.9) in another trial, and patients’ age ranged from 0 to >75 years in another one, and 34.7 % of the population were male.
Table 1.
Summary characteristics of studies included in review
| Study | Setting | Population | Nurse group | Physician group | Intervention | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First author, publication (y) | Location | Design, perioda | Facilities, n | Diagnosis | Nurses (n) | Patients (N) | Mean age (SD), y | Male, % | Phys., (n) | Patients (N) | Mean age (SD), y | Male, % | By | FCA | GDL | 1st C | UV | OC | C, n | FUP, months |
| Fairall et al., 2012 [25] | ZA 2 | cRCT2, 2008–2010 | Nurse ART clinic, 31 | HIV/AIDS | 103 | 3029 | 38.0 (8.9) | 30 | nr | 3202 | 38.0 (9.6) | 27 | LN | n | y | n | n | y | >1 | 12–18 |
| Fairall et al., 2012 [25] | ZA 1 | cRCT1, 2008–2010 | Nurse ART clinic, 31 | HIV/AIDS | 103 | 5390 | 36.0 (9.6) | 33 | nr | 3862 | 35.0 (9.6) | 31 | LN | n | y | n | n | y | >1 | 12–18 |
| Houweling et al., 2011 [27] | NL 3 | RCT, period nr | Practice, 1 | DM2 | 2 | 116 | 67.1 (11.0) | 53 | 5 | 114 | 69.5 (10.6) | 42 | NP | y | y | n | n | y | >1 | 14 |
| Andryukhin et al., 2011 [18] | RU 1 | RCT, 2006–2009 | Medical centre practice, 1 | Heart failure with preserved ejection fraction | 10 | 50 | 66.5 (3.2) | 27 | 8 | 50 | 68.0 (4.3) | 34 | NP/LN | n | y | n | n | y | >1 | 6 |
| Dierick-van Daele et al., 2009 [24] | NL 2 | RCT, 2006 | Practice, 15, Reference, 5 | Common complaints | 12 | 817 | 42.8 (16.5) | 38 | 50 | 684 | 46.1 (16.6) | 40 | NP+ | n | y | y | n | n | 1 | 0.5 |
| Chan et al., 2009 [22] | UK 6 | RCT, 2002–2004 | Nurse clinic, 1 | GORD, moderate gastritis, dyspepsia after direct access gastroscopy | nr | 89 | 50.2 (13.9) | 49 | nr | 86 | 48.4 (12.8) | 49 | NP+ | n | y | n | n | y | >1 | 6 |
| Hesselink et al., 2004 [26] | NL 1 | RCT, 1998–2002 | Practice, 12 | Asthma and COPD | 2 | 139 | 49.9 (14.2) | 35 | 14 | 137 | 44.7 (13.6) | 28 | LN | n | y | n | n | y | >1 | 0.5, 12, 24 |
| Denver et al., 2003 [23] | UK 5 | RCT, 2000–2001 | Nurse hospital-based hypertension clinic, n = nr | DM2,hypertension, under blood pressure lowering treatment | nr | 60 | 58.1 (13.8) | 57 | nr | 60 | 62.4 (9.1) | 70 | NP+ | n | y | n | n | y | >1 | 6 |
| Kernick et al., 2000 [28] | UK 4 | RCT, period nr | Health centre, 1 | Psoriasis and eczema | 1 | 55 | 47.4 (18.4) | 39 | nr | 54 | 51.7 (15.8) | 48 | NP+ | n | y | n | n | y | >1 | 4 |
| Kinnersley et al., 2000 [34] | UK 3 | RCT, period nr | Practice, 10 | Diverse conditions | 12 | 1465b | range: 0–>75 | 39 | 10 | 1465b | range: 0–>75 | 42 | NP | n | nr | y | y | n | 1 | 0.5 |
| Shum et al., 2000 [32] | UK 2 | RCT, 1998–1999 | Practice, 5 | Acute minor illnesses | 5 | 900 | IQR:26.0 (9.0–41.7) | 40 | 19 | 915 | IQR:29.1 (9.7–44.9) | 40 | NP | n | nr | y | y | n | ≥1 | 0.5 |
| Campbell et al., 1998 [19–21, 29–31, 33] | UK 1 | RCT, 1995–1996 | Practice, 19 | CHD secondary prevention | 28 | 673 | 65.9 (7.9) | 58 | nr | 670 | 66.3 (8.3) | 58 | NP | n | y | n | n | y | >1 | 12, 48 |
Studies are listed by year (y) of publication, in decreasing order
Phys. (n): number of physicians; Nurses (n): number of nurses; Patients (N): number of patients enrolled (Fairall et al. 2012 [25]) or randomized; SD: standard deviation; UK: United Kingdom; NL: The Netherlands; ZA: South Africa; RU: Russia; RCT: randomized controlled trial; cRCT: cluster randomized controlled trial; Facilities n: number of facilities; DM (2): diabetes mellitus (type 2); GORD: gastro-esophageal reflux disease; COPD: chronic obstructive pulmonary disease; CHD: coronary heart disease; IQR: interquartile ranges; NP: nurse practitioner; NP+: nurse practitioner with additional degrees/courses; LN: licensed nurse; FCA: full clinical autonomy; GDL: guideline/(semi-structured)protocol-based interventions; 1stC.: 1st contact; UV: urgent visits; OC: ongoing care; C (n): number of consultations; FUP: length of follow-up; y: yes; n: no; nr: not reported
aStart and end year when studies were conducted
bNumber of randomized patients per group not reported
Task shifting was carried out in general practices, nurse clinics and healthcare centres, for a wide range of possible diagnoses (diverse, minor acute, common or specific, for example, hypertension) in patients requiring single-contact care, single-contact and urgent care and/or ongoing care. The tasks varied widely from assessment, history taking, preparation, diagnostic, monitoring and prescription to decisions on eligibility for and initiation of treatment, referral, follow-up and secondary prevention. Description of nurses’ competencies and training components often lacked enough detail. The number of participating nurses and physicians was reported in 10 and 6 trials; the median number was 11 (range: 1–103) and 12 (range: 5–50), respectively. Nurses performed roles of NPs in eight trials, LNs in three trials and LNs and NPs in one trial. Nurses’ and physicians’ experience was reported in four (range: 1–12 years) and one (16 years) trials, respectively. Three trials stated the nurses’ educational degree: a Masters in Advanced Nursing, a diploma in general practice and a special degree in patient education. Nurses delivered independent interventions in all trials but required support from physicians in 11 trials and assumed full responsibility in 1 trial. All but two trials reported the use of clinical guidelines or protocols.
Risk of bias in individual studies
The methodological assessment per quality item for each trial is reported on Table 2. Ten trials individually assigned patients to intervention groups and two randomized 31 clinics with 103 nurses. No trial fulfilled all the quality criteria assessed. Ten trials reported patient inclusion and exclusion criteria and seven measured the intervention by definition of a primary outcome. The trials were at risk of selection bias since only six had adequate random sequence generation and allocation concealment. No trial reported blinding of patients and providers, and three performed blinded assessment of outcomes, making trials vulnerable to performance and detection biases. Eleven trials reported to have calculated sample sizes, eight had at least 20 % attrition (overall range: %: 24–59) and seven reported the use of intention-to-treat techniques to deal with missing data. Nine trials reported the funding sources; one was industry funded.
Table 2.
Methodological features of included studies
| Study | Inclusion and exclusion criteria | Outcome | Sequence generation | Allocation concealment | Blinding | Sample | Attrition, % | Funding | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| First author | Location | 1ry | 2ry | calc. | size | ||||||
| Fairall et al., 2012 [25] | ZA 2 | ✓ | ✓ | ✓ | A | A | d | ✓e | ≥200 | <20 | G |
| Fairall et al., 2012 [25] | ZA 1 | ✓ | ✓ | ✓ | A | A | d | ✓e | ≥200 | ≥20 | G |
| Houweling et al., 2011 [27] | NL 3 | ✓ | ✓ | ✓ | I | A | NP | ✓ | ≥200 | <20 | G |
| Andryukhin et al., 2011 [18] | RU 1 | ✓ | U | I | c | ✓e | <200 | ≥20 | None | ||
| Dierick-van Daele et al., 2009 [24] | NL 2 | ✓ | A | A | NP | ≥200 | ≥20 | G | |||
| Chan et al., 2009 [22] | UK 6 | ✓ | A | A | b | ✓ | <200 | <20 | nr | ||
| Hesselink et al., 2004 [26] | NL 1 | a | ✓ | ✓ | U | U | b | ✓ | ≥200 | ≥20 | nr |
| Denver et al., 2003 [23] | UK 5 | a | ✓ | ✓ | I | I | NP | ✓e | <200 | <20 | nr |
| Kernick et al., 2000 [28] | UK 4 | ✓ | ✓ | A | U | U | ✓e | <200 | ≥20 | Ind. | |
| Kinnersley et al., 2000 [34] | UK 3 | ✓ | ✓ | ✓ | A | A | NP | ✓e | ≥200 | ≥20 | G |
| Shum et al., 2000 [32] | UK 2 | ✓ | A | A | NP | ✓e | ≥200 | ≥20 | G | ||
| Campbell et al., 1998 [19–21, 29–31, 33] | UK 1 | ✓ | A | I | b | ✓ | ≥200 | ≥20 | G | ||
Studies are listed by year (y) of publication, in decreasing order. A tick indicates the specific criteria fulfilled
Blinding: whether patients, care providers and/or outcome assessors were blinded; UK: United Kingdom; NL: the Netherlands; ZA: South Africa; RU: Russia. I: inadequate; A: adequate; U: unclear; NP: not performed; G: government; Ind.: industry; P: private; nr: not reported
aInclusion criteria only
bBlinding of outcome assessors
cSingle blinding
dData analysts partly blinded
eIntention to treat strategies to deal with missing data
Outcomes
Twenty-five different measures of the course of disease were reported for a wide range of conditions (Table 3). All but three [24, 26] of the measures were taken using validated methods, and the follow-up time span varied widely.
Table 3.
Effect estimates of studies in review
| Study | Nurses’ role | Population diagnosis | Outcome | Measurement method/scale | FUP, months | Nurse group | Physician group | Effect estimate | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| First author, y | Location | ||||||||||
| Binary data | n | N | n | N | RR (95 % CI) | ||||||
| Heart disease | |||||||||||
| Andryukhin et al., 2011 [18] | RU 1 | NP/LN | Heart failure PEF | Positiveb changes in class HF | NYHA | 6 | 18 | 40 | 8 | 35 | 1.97 (0.98 to 3.96) |
| Campbell et al., 1998 [19–21, 29–31, 33] | UK 1 | NP | CHD secondary prevention | Chest pain | ATyPeS/SF36a | 12 | 232 | 508 | 250 | 498 | 0.91 (0.80 to 1.04) |
| Campbell et al., 1998 [19–21, 29–31, 33] | UK 1 | NP | CHD secondary prevention | Chest pain | ATyPeS/SF36 | 48 | 147 | 430 | 129 | 385 | 1.02 (0.84 to 1.24) |
| Campbell et al., 1998 [19–21, 29–31, 33] | UK 1 | NP | CHD secondary prevention | Worsening chest pain | ATyPeS/SF36 | 12 | 37 | 519 | 54 | 500 | 0.66 (0.44 to 0.98) |
| Campbell et al., 1998 [19–21, 29–31, 33] | UK 1 | NP | CHD secondary prevention | Worsening chest pain | ATyPeS/SF36 | 48 | 44 | 439 | 35 | 395 | 1.13 (0.74 to 1.73) |
| Lung disease | |||||||||||
| Hesselink et al., 2004 [26] | NL 1 | LN | Asthma/COPD | No chronic cough and phlegm production or an improvement | Present/absent | 12 | 43 | 108 | 39 | 85 | 0.87 (0.63 to 1.20) |
| Hesselink et al., 2004 [26] | NL 1 | LN | Asthma/COPD | No chronic cough and phlegm production or an improvement | Present/absent | 24 | 41 | 93 | 33 | 79 | 1.06 (0.75 to 1.49) |
| Hesselink et al., 2004 [26] | NL 1 | LN | Asthma/COPD | No wheezing or an improvement in frequency | Never, ever, most days and night | 12 | 68 | 106 | 51 | 85 | 1.07 (0.85 to 1.34) |
| Hesselink et al., 2004 [26] | NL 1 | LN | Asthma/COPD | No wheezing or an improvement in frequency | Never, ever, most days and night | 24 | 53 | 93 | 37 | 79 | 1.22 (0.91 to 1.63) |
| Infectious disease | |||||||||||
| Fairall et al., 2012 [25] | ZA 2 | LN | HIV/AIDS | Suppressed viral load in patients receiving ARTd | Viral load | 12–18 | 2156 | 3029 | 2230 | 3202 | 1.02 (0.99 to 1.06) |
| Fairall et al., 2012 [25] | ZA 1 | LN | HIV/AIDS | Suppressed viral load in patients starting ARTd | Viral load | 12–18 | 1706 | 2375 | 1062 | 1449 | 0.98 (0.94 to 1.02) |
| Diverse, acute and minor conditions | |||||||||||
| Shum et al., 2000 [32] | UK 2 | NP | Acute and minor | Same, improved or cured self-reported health status | Murphy | 0.5 | 650 | 672 | 646 | 661 | 0.99 (0.97 to 1.01) |
| Kinnersley et al., 2000 [34] | UK 3 | NP | Diverse conditions | Same or improved symptoms (much better, better or unchanged) | Likert-type and single reminders | 0.5 | 472 | 484 | 515 | 529 | 1.00 (0.98 to 1.02) |
| Continuous data | Mean (SD) | N | Mean (SD) | N | WMD (95 % CI) | ||||||
| Lung disease | |||||||||||
| Hesselink et al., 2004 [26] | NL 1 | LN | Asthma/COPD | Mean change score in dyspnea | MRCQTc | 12 | 0.00 (1.3) | 115 | 0.10 (1.3) | 94 | −0.10 (−0.45 to 0.25) |
| Hesselink et al., 2004 [26] | NL 1 | LN | Asthma/COPD | Mean change score in dyspnea | MRCQTc | 24 | 0.20 (1.4) | 96 | 0.30 (1.3) | 80 | −0.10 (−0.50 to 0.30) |
| Metabolic disease | |||||||||||
| Denver et al., 2003 [23] | UK 5 | NP+ | DM2 with hypertension, under BPLT | Mean fall in 10-year CHD risk | Framingham CHD risk score | 6 | −2.33 (3.87) | 59 | −0.33 (2.16) | 56 | −2.00 (−3.14 to −0.86) |
| Denver et al., 2003 [23] | UK 5 | NP+ | DM2 with hypertension, under BPLT | Mean fall in 10-year stroke risk | Framingham stroke risk score | 6 | −4.33 (6.0) | 59 | −1.80 (3.53) | 56 | −2.53 (−4.32 to −0.74) |
| Digestive disease | |||||||||||
| Chan et al., 2009 [22] | UK 6 | NP+ | GORD, moderate gastritis | Mean score, dyspepsia severity | GDSS (Gladys) scoreg | 6 | 4.90 (2.9) | 89 | 7.20 (3.1) | 86 | −2.30 (−3.19 to −1.41) |
| Skin disease | |||||||||||
| Kernick et al., 2000 [28] | UK 4 | NP+ | Psoriasis/eczema | Mean score for symptoms and severity of skin condition | Self-evaluation clinical scoree | 4 | 7.60 (3.3) | 35 | 8.1 (3.3) | 46 | −0.50 (−1.95 to 0.95) |
| Common complaints | |||||||||||
| Dierick-van Daele et al., 2009 [24] | NL 2 | NP+ | Common complaints | Mean difference in the degree of burden of illness | LikertQTf | 0.5 | −1.77 (3.18) | 473 | −1.50 (2.63) | 451 | −0.27 (−0.65 to 0.11) |
| Dierick-van Daele et al., 2009 [24] | NL 2 | NP+ | Common complaints | Mean difference in the concerns about illness | LikertQTf | 0.5 | −1.51 (3.20) | 476 | −1.40 (2.97) | 450 | −0.11 (−0.51 to 0.29) |
| Qualitative data | |||||||||||
| Metabolic disease | |||||||||||
| Houweling et al., 2011 [27] | NL 3 | NP | DM2 | Perceived burden of DM symptoms and rating of symptom troublesomeness | Type 2 Diabetes Symptom Checklisth | 14 | “significant differences at follow-up for some of the Diabetes Symptom Score dimensions (data not shown). After 14 months, the mean sub-dimension scores for DM symptoms ‘fatigue’ and ‘cognitive distress’ and the total scores were lower in each group, although no difference was observed between the groups.” | ||||
| Lung disease | |||||||||||
| Hesselink et al., 2004 [26] | NL 1 | LN | Asthma/COPD | Respiratory complaints within two weeks after intervention | Disturbance (present/absent) for >1 day or night | 0.5 | “no significant group differences in the number of days or nights disturbed, OR 0.96 (95 % CI 0.56 to 1.61)” | ||||
| Common complaints | |||||||||||
| Dierick-van Daele et al., 2009 [24] | NL 2 | NP+ | Common complaints | Complications due to illness | Mean number of days of work absence | 0.5 | “1.11 days (nurse, SD 0.32; physician, SD 0.31) of work absence in average” | ||||
| Dierick-van Daele et al., 2009 [24] | NL 2 | NP+ | Common complaints | Complications due illness | Mean number of days of inability for daily activities | 0.5 | “no statistically significant differences between groups; mean days unable for daily activities: nurse-led care 2.53 (SD 2.89), physician-led care 2.69 (SD 2.90)” | ||||
Studies are listed in order of increasing length of follow-up, within each category of outcomes
UK: United Kingdom; NL: the Netherlands; ZA: South Africa; RU: Russia; n: number of patients or number of events; N: total number of patients per group; SD: standard deviation; RR: relative risk; WMD: weighted mean difference; CI: confidence intervals; DM(2): diabetes mellitus (type 2); GORD: gastro-esophageal reflux disease; COPD: chronic obstructive pulmonary disease; CHD: coronary heart disease; BPLT: blood pressure lowering treatment; PEF: preserved ejection fraction; MRCQT: Medical Research Council Questionnaire; LikertQT: Likert-type questionnaire; GDSS: Glasgow Dyspepsia Severity Score (Gladys); NYHA: New York Heart Association Functional Classification; ATyPeS: Angina TyPe specification scale
aATyPeS is designed to use with the SF36 questionnaire to assess the presence, frequency and course of chest pain
bPositive changes mean regression of class or stay within class I of NYHA
cMRCQT ranking from 0 (no dyspnea) to 4 (very serious); positive mean values in each group indicate improvement; mean differences with negative values mean a reduction or improvement
dZA1 trial: patients starting ART whose results were available for at least 6 months. ZA2 trial: 76 % and 78 % of the patients in the intervention and control group, respectively, had been receiving ART for at least 2 years at the time of viral load measurements
eThree out of eight possible symptoms, each ranked from 1 (mild) to 5 (very severe). The sum score gave a clinical score from 3 (best state) to 15 (worst)
fLikert-type questionnaire ranking from 0 (excellent) to 10 (poor/worse); mean differences with negative values mean a reduction or improvement
gGDSS (Gladys) ranking from 0 (no symptoms) to 20 (symptoms)
h34-item scale based on yes/no questionnaires for perceived burden of symptoms including hyperglycemic, hypoglycemic, cardiac, neuropathic, psychological and vision-related. Summary responses ranked from 1 (symptom not occurred or not perceived as troublesome) to 5 (symptom extremely troublesome) on Likert-type scale
Heart disease
In one trial, NPs delivered care techniques to facilitate behavioural change following clinical guidelines to perform secondary prevention of coronary heart disease (CHD) [20]. In a time span of 12 or 48 months, nurse-led care showed no significant differences to physician-led care in the number of patients with chest pain, reflected on the Angina TyPe specification scale and the SF-36 questionnaire. In a time span of 12 months, however, nurse-led care showed significantly fewer patients (7.1 %), compared to physician-led care (10.8 %), who reported worsening (little or much worse) chest pain (RR 0.66, 95 % CI 0.44 to 0.98). This difference levelled off at 48 months.
In another trial, LNs and/or NPs delivered patient education, treatment, exercise and training information and counselling following clinical guidelines to manage heart failure with preserved ejection fraction [18]. In a time span of 6 months, nurse-led care showed no significant differences to physician-led care in the number of patients with positive changes in heart failure class, reflected on the New York Heart Association Functional Classification tool: positive changes meant regression of class or stay within class I.
Lung disease
In one trial, LNs delivered patient education and followed structured protocols to manage asthma and chronic obstructive pulmonary disease [26]. In a time span of 12 and 24 months, both nurse-led care and physician-led care showed a small (mean change) improvement in dyspnea scores, but the differences were not significant, reflected on the Medical Research Council Questionnaire. The trial also showed no significant differences between groups in the number of patients in whom chronic cough, phlegm production and wheezing were absent or improved and in the number of days or nights disturbed.
Metabolic disease
In one trial, NPs+ followed clinical guidelines to manage hypertension in patients with type 2 diabetes mellitus (DM2); no other details about the interventions delivered were reported [23]. In a time span of 6 months, nurse-led care compared to physician-led care showed that the differences in mean fall from baseline were significantly lower for stroke risk (WMD −2.53, 95 % CI −4.32 to −0.74) and CHD risk (WMD −2.00, 95 % CI −3.14 to −0.86), reflected on the Framingham 10-year stroke risk and the 10-year CHD risk scores.
In another trial, NPs followed clinical guidelines to manage patients with DM2; no other details about the interventions delivered were reported [27]. The trial stated that in a time span of 14 months significant differences with nurse-led care were observed for some of the DM2-related symptom score dimensions, reflected on the revised version of DM2 Symptom Checklist. The mean sub-dimension scores for fatigue, cognitive distress and the total scores were stated to be lower in each group.
Digestive disease
In one trial, NPs+ ran a follow-up clinic and managed gastroscopy and dyspepsia according to guidelines; no other details about the interventions delivered were reported [22]. In a time span of 6 months, nurse-led care significantly improved (maintained or reduced) dyspepsia, compared to physician-led care, reflected in the Glasgow Dyspepsia Severity Score (Gladys) (WMD −2.30, 95 % CI −3.19 to −1.41).
Skin disease
In one trial, NPs+ managed and prescribed medications for the management of psoriasis and eczema following a dermatology manual; no other details about the interventions delivered were reported [28]. In a time span of 4 months, nurse-led care showed no significant differences to physician-led care in the severity of skin condition and symptoms for psoriasis and eczema, reflected in a summary clinical score for self-evaluation of symptoms.
Infectious disease
In one trial, LN assessed eligibility and prepared patients for antiretroviral therapy (ART); monitored, prescribed and initiated ART therapy; and referred patients to physicians for ART initiation and re-prescriptions and followed clinical guidelines for the management of HIV [25]. In a time span of 12–18 months, nurse-led care compared to physician-led care showed no significant differences in the number of patients for whom suppressed viral load was maintained while they were under ART; 77 % of the patients had ART for at least 2 years. In another trial, nurses delivered the same interventions for HIV patients whose viral load results were available for at least 6 months [25]. In a time span of 12–18 months, there were no significant differences between groups in the number of patients for whom suppressed viral load was maintained after starting ART.
Diverse, acute, minor or common complaints
In one trial, NPs performed history taking and physical examinations, gave advice and prescribed treatment and referrals, for the management of acute and minor illness [32]. In another trial, NPs performed same-day consultations for diverse conditions; no other details about the interventions delivered were reported [34]. Both trials included children (Table 1). None of the trials reported whether nurses followed clinical guidelines to deliver interventions. In a time span of half a month, the two trials showed no significant differences between groups in the number of patients who reported their health status as same, improved or cured, reflected on the Murphy scale [32] and a Likert-type scale [34].
In another trial, NPs+ assessed symptoms, performed clinical examinations and diagnosis, planned further treatment, prescribed and performed referrals to primary or secondary care, ordered clinical tests and examinations and followed clinical guidelines for the management of common complaints [24]. In a time span of half a month, nurse-led care compared to physician-led care showed no significant (mean) differences (before and 2 weeks after consultation) in the degree of burden of illness and in the concerns about illness, reflected on a Likert-type questionnaire. The trial also stated no significant differences between groups in the mean number of days for which patients reported being unable to perform daily activities due to illness. The stated average number of days that patients missed their job due to illness was 1.11 days.
Length of consultations
Four trials [24, 27, 32, 34] reported the length of consultations; all showed longer consultations by nurses than by physicians (WMD range: 1.90–3.80 min; 95 % CI: 1.32 to 4.26).
The quality of studies was mixed, and sample sizes were generally small. The three trials [20, 22, 23] in which the intervention effects favoured nurse-led care were of lower methodological quality (small study (N < 200), lack/unclear random generation and allocation concealment and/or blinding and/or ≥20 % attrition). Among these, only one [22] was superior in quality but used a small patient population. A trial [25] of somehow higher quality (N > 3000, better random generation and allocation concealment, <20 % attrition, some blinding) also showed no significant differences between groups. Of the remaining trials, four [24, 25, 32, 34] had larger patient populations and better random generation and allocation concealment, but did not fulfil blinding and/or attrition criteria.
Discussion
In this systematic review, we identified 12 trials aiming to compare physician-led care with nurse-led care under a task-shifting model in primary care. Nurse-led care was provided mainly by nurse practitioners whose scope expanded to a wide range of clinical domains and patient populations. Nurses performed various tasks with different degrees of clinical responsibility. They used clinical guidelines and validated tools in most studies to deliver care and monitor and identify disease-specific changes of the course of disease. The volume of literature continues to be low, however, and belongs mostly to European high-income countries, mainly the UK and the Netherlands. The evidence represents a wide range of disease-specific measurements of disease progression, is at risk of biases and consists of variable follow-up episodes. Nevertheless, we found that nurse-led care was statistically not significantly different to physician-led care in 84 % of the patient outcomes reported. The remaining 16 % significantly favoured nurse-led care compared to physician-led care. Nurses may thus have the ability to meet the needs of healthcare systems with an increasing shortage of physicians, in keeping with reports calling for nurses to be used more and to perform greater roles [7, 9, 10, 35].
The use of structured protocols that combine non-pharmacological interventions with pharmacological therapy and the use of validated tools in 75–84 % of the studies might have resulted in better or similar care by nurses than by physicians. It has been shown [36, 37] that through delivering interventions that include education, counselling and advice, nurses may encourage more life changes and retain more patients in treatment resulting in greater medication compliance, improve prevention and better symptom control. Interventions that include the provision of information about causes of illness and patients’ disease, for example, in the trial of patients with dyspepsia, may have also added benefits to nurse-led care resulting in more motivated patients and more effective (self-care) interventions in general. Research has shown that patients generally want more information than they routinely receive from healthcare professionals and that they like greater involvement in the process of making decisions about their treatment [38]. Good communication skills can also increase adherence to treatment and outcome effectiveness [39, 40] and may have led to more patients being involved in their own care and treatment decisions.
The use of disease-specific protocols may have also guided nurse-led care interventions to at least similar effectiveness as physicians-led care in the management of stroke and CHD risk in diabetic patients. Disease-specific protocols that include intensified non-pharmacological programmes have indeed been associated with improved cardiovascular risk factors but also with patient self-efficacy and patient safety [41–43]. Using these protocols may have also led nurses to successfully perform therapy techniques that require safe (for example, inhalation) and continuous management for conditions such as COPD and asthma control. In addition, appropriate identification and monitoring of disease changes have been recommended to successfully engage and retain patients in care [44, 45]. Following like-guidelines, nurses might have appropriately quantified and monitored viral load, for example, resulting in similar effectiveness to physician-led care at maintaining suppressed viral load. In all, nurses might have followed protocols more strictly resulting in outcome improvements [46].
The long-term nature of chronic disease necessitates a programme with an appropriate time span. It is unclear, however, if the length of follow-up was adequate to identify a true effect; the studies do not report details about the monitoring length needed to reflect a change. For most of the studies, the time span was short, 6 months or less. Disease complexity may have also resulted in longer consultations by nurses than by physicians. In all studies, nurses were trained and/or took courses for delivering the studies’ interventions. Further, nurses were supported by physicians in most of the studies, suggesting of the potential benefits of collaborative teams in the improvement of patient outcomes, for example, reducing modifiable risk factors [47, 48]. In a broader context, by participating in these studies, nurse-led care patients may have become more aware of their condition and were thus more receptive to care resulting in better outcomes.
It is uncertain to what extent nurses’ educational preparation and type of nurses’ roles influenced the outcome effects. The three trials that reported the nurses’ educational degree showed no significant differences. Although nurses were in NP roles in 16 % (4/25) of the outcomes that favoured nurse-led care, the studies were of lower methodological quality somehow (lack/unclear random generation and/or allocation concealment and/or ≥20 % attrition and/or small study). Furthermore, nurses were NPs and/or LNs in 84 % (21/25) of the outcomes which showed no significant differences. Although these studies were of variable quality, one trial of somehow higher quality also had a bigger sample (N > 3000).
Future research could benefit from a more rigorous methodology and better study reporting. Change in health status over a time interval can occur due to the natural course of disease and/or as a result of the care provided. Future studies should therefore report about the regularity of disease monitoring needed to obtain an improved outcome, consist of longer follow-up episodes and continue using validated instruments. This could lead to increased safety, effectiveness and improved compliance to medication [36, 37]. Self-report scales should be considered more carefully since these may not be able to accurately detect the causes for the changes in the course of disease. In order to understand how nurses’ competencies and qualifications influence patient outcomes and quality of care, future studies should map all available nurses’ roles and consistently report the educational qualifications and clinical responsibilities, training and clinicians’ characteristics (for example, nurse–physician–patient ratios and years of experience). Reporting of intervention components as recently recommended [49] could help to identify the benefits of this strategy. The implementation of non-pharmacological strategies should be further considered to improve disease management and quality outcomes [50, 51].
Strengths and limitations of this systematic review
This is, to our knowledge, the first task-shifting systematic review with a focus on the study of measurements of the course of disease. Although many measures were reported, most were unique to each study precluding the incorporation of meta-analyses. Where data were available, however, we report the trial estimates. Although observational studies if well implemented could provide important information, we only included RCTs because these are at a lower risk of bias and allow the estimation of causal effects. A small number of studies met the inclusion criteria, possibly because the number of studies in this area is increasing slowly. We did not search for grey literature, and we excluded publications reported in languages other than English. We used thorough electronic and manual searches, however, and screened relevant reviews (some in foreign languages) to identify all relevant publications. It was difficult to understand the level of nurses’ autonomy since nurses were supported by physicians in most studies. In most cases, the interventions are not described in detail, and we could not make clear judgments about nurses’ educational degree.
Conclusion
Trained nurses, mostly NPs, appeared to achieve outcomes of at least similar effects as physicians for the management of disease progression in a wide range of patient populations. Structured protocols and validated tools might be some of the main boosters of outcome improvement. The implementation of non-pharmacological and patient-centred care approaches may also lead to successful nurse-led care interventions. A clear definition of roles, qualifications, skills and experience, essential for an effective and safe transfer of tasks and functions, is only reported in low standards. It is therefore unclear to what extent nurses should be involved in task shifting from physicians. The evidence is also limited by the mixed methodological quality of the trials, although a few of the trials have larger patient populations. More good quality studies using validated tools and larger samples from many countries should improve the reporting standards and consistency of nurses’ roles, qualifications and interventions.
Acknowledgements
We are grateful to Martina Gosteli for her assistance with the search strategy, Fran Mikulicic for his support with search strategies, Stefan Markun for his support with consensus of data and Oliver Senn for his help with statistics.
Funding
This study was funded by the Health Services Research Fund (Bangerter foundation) from the Swiss Academy of Medical Sciences (SAMS) and by the Swiss Association of Family Physicians (Hausärzte Schweiz). The funder had no role in the content or preparation of the manuscript or in the decision to publish.
Additional files
PRISMA checklist.
Search strategy in Ovid MEDLINE. Note: Similar search strategies were performed and run in Embase, The Cochrane Library of Systematic Reviews and CINAHL and include specific search filters for RCTs.
Studies excluded based on appraisal of full-text articles.
Population and interventions in the included studies. Note: Studies are listed by year (y) of publication, in decreasing order. UK, United Kingdom; NL, The Netherlands; ZA, South Africa; RU, Russia; RCT, randomized controlled trial; cRCT, cluster randomized controlled trial; m, months; n/r, not reported; ART, antiretroviral therapy; HbA1c, haemoglobin; CD4, T-cell surface glycoprotein CD4.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
NAMG led the design and analysis of the study and wrote and revised the manuscript. NAMG, RT, SD and TR conceived and designed the experiments. NAMG and SD performed the experiments. RT provided input on eligibility of studies and with extraction of data. TR supervised the development and methodology of the review and manuscript revision. All authors read and approved the final manuscript.
Contributor Information
Nahara A. Martínez-González, Email: Nahara.Martinez@usz.ch
Ryan Tandjung, Email: Ryan.Tandjung@usz.ch.
Sima Djalali, Email: Sima.Djalali@usz.ch.
Thomas Rosemann, Email: Thomas.Rosemann@usz.ch.
References
- 1.United Nations Department of Economic and Social Affairs Population Division . World population ageing 2013. New York: United Nations; 2013. [Google Scholar]
- 2.Global Health Workforce Alliance and World Health Organization . A universal truth: no health without a workforce. Geneva: World Health Organization; 2013. [Google Scholar]
- 3.World Health Organization . Task shifting: rational redistribution of tasks among health workforce teams. Global recommendations and guidelines. Geneva: World Health Organization; 2008. [Google Scholar]
- 4.Laurant M, Harmsen M, Wollersheim H, Grol R, Faber M, Sibbald B. The impact of nonphysician clinicians: do they improve the quality and cost-effectiveness of health care services? Med Care Res Rev. 2009;66:36S–89. doi: 10.1177/1077558709346277. [DOI] [PubMed] [Google Scholar]
- 5.Cooper RA. New directions for nurse practitioners and physician assistants in the era of physician shortages. Acad Med. 2007;82:827–8. doi: 10.1097/ACM.0b013e31812f7939. [DOI] [PubMed] [Google Scholar]
- 6.Buchan J, Calman L. An overview of issues and actions. Geneva, Switzerland: International Council of Nurses; 2006. Summary: the global shortage of registered nurses. [Google Scholar]
- 7.Delamaire M, Lafortune G. Nurses in advanced roles: a description and evaluation of experiences in 12 developed countries. France: OECD Publishing; 2010. [Google Scholar]
- 8.World Health Organization. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003.
- 9.Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ. 2002;324:819–23. doi: 10.1136/bmj.324.7341.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laurant M, Reeves D, Hermens R, Braspenning J, Grol R, Sibbald B. Substitution of doctors by nurses in primary care. Cochrane Database Syst Rev. 2005;2:CD001271. doi: 10.1002/14651858.CD001271.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Egger M, Smith GD, Altman DG. Systematic reviews in health care. Hoboken: BMJ Publishing Group; 2008. Principles of and procedures for systematic reviews; pp. 23–42. [Google Scholar]
- 12.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Juni P, Witschi A, Bloch R, Egger M. The hazards of scoring the quality of clinical trials for meta-analysis. JAMA. 1999;282:1054–60. doi: 10.1001/jama.282.11.1054. [DOI] [PubMed] [Google Scholar]
- 15.da Costa BR, Hilfiker R, Egger M. PEDro’s bias: summary quality scores should not be used in meta-analysis. J Clin Epidemiol. 2013;66:75–7. doi: 10.1016/j.jclinepi.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 16.Review Manager (RevMan) [Computer Program] Version 5.2.4 edition for Windows. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 657 2012.
- 17.Higgins JPT GS, (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated September 2011]. The Cochrane Collaboration, 2011. Available from http://handbook.cochrane.org/.
- 18.Andryukhin A, Frolova E, Vaes B, Degryse J. The impact of a nurse-led care programme on events and physical and psychosocial parameters in patients with heart failure with preserved ejection fraction: a randomized clinical trial in primary care in Russia. Eur J Gen Pract. 2010;16:205–14. doi: 10.3109/13814788.2010.527938. [DOI] [PubMed] [Google Scholar]
- 19.Campbell NC, Ritchie LD, Thain J, Deans HG, Rawles JM, Squair JL. Secondary prevention in coronary heart disease: a randomised trial of nurse led clinics in primary care. Heart. 1998;80:447–52. doi: 10.1136/hrt.80.5.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Campbell NC, Thain J, Deans HG, Ritchie LD, Rawles JM. Secondary prevention in coronary heart disease: baseline survey of provision in general practice. BMJ. 1998;316:1430–4. doi: 10.1136/bmj.316.7142.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Campbell NC, Thain J, Deans HG, Ritchie LD, Rawles JM, Squair JL. Secondary prevention clinics for coronary heart disease: randomised trial of effect on health. BMJ. 1998;316:1434–7. doi: 10.1136/bmj.316.7142.1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan D, Harris S, Roderick P, Brown D, Patel P. A randomised controlled trial of structured nurse-led outpatient clinic follow-up for dyspeptic patients after direct access gastroscopy. BMC Gastroenterol. 2009;9:12. doi: 10.1186/1471-230X-9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Denver EA, Barnard M, Woolfson RG, Earle KA. Management of uncontrolled hypertension in a nurse-led clinic compared with conventional care for patients with type 2 diabetes. Diabetes Care. 2003;26:2256–60. doi: 10.2337/diacare.26.8.2256. [DOI] [PubMed] [Google Scholar]
- 24.Dierick-Van Daele ATM, Metsemakers JFM, Derckx EWCC, Spreeuwenberg C, Vrijhoef HJM. Nurse practitioners substituting for general practitioners: randomized controlled trial. J Adv Nurs. 2009;65:391–401. doi: 10.1111/j.1365-2648.2008.04888.x. [DOI] [PubMed] [Google Scholar]
- 25.Fairall L, Bachmann MO, Lombard C, Timmerman V, Uebel K, Zwarenstein M, et al. Task shifting of antiretroviral treatment from doctors to primary-care nurses in South Africa (STRETCH): a pragmatic, parallel, cluster-randomised trial. Lancet. 2012;380(9845):889–98. doi: 10.1016/S0140-6736(12)60730-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hesselink AE, Penninx BW, van der Windt DA, van Duin BJ, de Vries P, Twisk JW, et al. Effectiveness of an education programme by a general practice assistant for asthma and COPD patients: results from a randomised controlled trial. Patient Educ Couns. 2004;55:121–8. doi: 10.1016/j.pec.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 27.Houweling ST, Kleefstra N, van Hateren KJ, Groenier KH, Meyboom-de Jong B, Bilo HJG. Can diabetes management be safely transferred to practice nurses in a primary care setting? A randomised controlled trial. J Clin Nurs. 2011;20:1264–72. doi: 10.1111/j.1365-2702.2010.03562.x. [DOI] [PubMed] [Google Scholar]
- 28.Kernick D, Cox A, Powell R, Reinhold D, Sawkins J, Warin A. A cost consequence study of the impact of a dermatology-trained practice nurse on the quality of life of primary care patients with eczema and psoriasis. Br J Gen Pract. 2000;50:555–8. [PMC free article] [PubMed] [Google Scholar]
- 29.Murchie P, Campbell NC, Ritchie LD, Deans HG, Thain J. Effects of secondary prevention clinics on health status in patients with coronary heart disease: 4 year follow-up of a randomized trial in primary care. Fam Pract. 2004;21:567–74. doi: 10.1093/fampra/cmh514. [DOI] [PubMed] [Google Scholar]
- 30.Murchie P, Campbell NC, Ritchie LD, Simpson JA, Thain J. Secondary prevention clinics for coronary heart disease: four year follow up of a randomised controlled trial in primary care. BMJ. 2003;326:84. doi: 10.1136/bmj.326.7380.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raftery JP, Yao GL, Murchie P, Campbell NC, Ritchie LD. Cost effectiveness of nurse led secondary prevention clinics for coronary heart disease in primary care: follow up of a randomised controlled trial. BMJ. 2005;330:707. doi: 10.1136/bmj.38342.665417.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shum C, Humphreys A, Wheeler D, Cochrane MA, Skoda S, Clement S. Nurse management of patients with minor illnesses in general practice: multicentre, randomised controlled trial. BMJ. 2000;320:1038–43. doi: 10.1136/bmj.320.7241.1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Delaney EK, Murchie P, Lee AJ, Ritchie LD, Campbell NC. Secondary prevention clinics for coronary heart disease: a 10-year follow-up of a randomised controlled trial in primary care. Heart. 2008;94:1419–23. doi: 10.1136/hrt.2007.126144. [DOI] [PubMed] [Google Scholar]
- 34.Kinnersley P, Anderson E, Parry K, Clement J, Archard L, Turton P, et al. Randomised controlled trial of nurse practitioner versus general practitioner care for patients requesting “same day” consultations in primary care. BMJ. 2000;320:1043–8. doi: 10.1136/bmj.320.7241.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De Geest S, Moons P, Callens B, Gut C, Lindpaintner L, Spirig R. Introducing advanced practice nurses/nurse practitioners in health care systems: a framework for reflection and analysis. Swiss Med Wkly. 2008;138:621–8. doi: 10.4414/smw.2008.12293. [DOI] [PubMed] [Google Scholar]
- 36.Van Camp YP, Van Rompaey B, Elseviers MM. Nurse-led interventions to enhance adherence to chronic medication: systematic review and meta-analysis of randomised controlled trials. Eur J Clin Pharmacol. 2013;69:761–70. doi: 10.1007/s00228-012-1419-y. [DOI] [PubMed] [Google Scholar]
- 37.Van der Wal MH, Jaarsma T. Adherence in heart failure in the elderly: problem and possible solutions. Int J Cardiol. 2008;125:203–8. doi: 10.1016/j.ijcard.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 38.Grol R, Wensing M, Mainz J, Jung HP, Ferreira P, Hearnshaw H, et al. Patients in Europe evaluate general practice care: an international comparison. Br J Gen Pract. 2000;50:882–7. [PMC free article] [PubMed] [Google Scholar]
- 39.Bieber C, Muller KG, Blumenstiel K, Schneider A, Richter A, Wilke S, et al. Long-term effects of a shared decision-making intervention on physician-patient interaction and outcome in fibromyalgia. A qualitative and quantitative 1 year follow-up of a randomized controlled trial. Patient Educ Couns. 2006;63:357–66. doi: 10.1016/j.pec.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 40.Fellowes D, Wilkinson S, Moore P. Communication skills training for health care professionals working with cancer patients, their families and/or carers. Cochrane Database Syst Rev. 2004;2:CD003751. doi: 10.1002/14651858.CD003751.pub2. [DOI] [PubMed] [Google Scholar]
- 41.Tregunno D. Organizational climate and culture. In: McGillis HL, editor. Quality work environments for nurse and patient safety. Sudbery, MA: Jones & Bartlett; 2005. [Google Scholar]
- 42.Duffield M, Roche M, O’Brien-Pallas L, Diers D, Aisbett C, King M, et al. Glueing it together: nurses, their work environment and patient safety. Sydney, Australia: University of Technology Sydney: Centre for Health Services Management; 2007.
- 43.Woodward A, Wallymahmed M, Wilding J, Gill G. Successful cardiovascular risk reduction in Type 2 diabetes by nurse-led care using an open clinical algorithm. Diabet Med. 2006;23:780–7. doi: 10.1111/j.1464-5491.2006.01889.x. [DOI] [PubMed] [Google Scholar]
- 44.Bangsberg DR, Perry S, Charlebois ED, Clark RA, Roberston M, Zolopa AR, et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15:1181–3. doi: 10.1097/00002030-200106150-00015. [DOI] [PubMed] [Google Scholar]
- 45.Estill J, Egger M, Johnson LF, Gsponer T, Wandeler G, Davies MA, et al. Monitoring of antiretroviral therapy and mortality in HIV programmes in Malawi, South Africa and Zambia: mathematical modelling study. PLoS One. 2013;8:e57611. doi: 10.1371/journal.pone.0057611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lugtenberg M, Burgers JS, Westert GP. Effects of evidence-based clinical practice guidelines on quality of care: a systematic review. Qual Saf Health Care. 2009;18:385–92. doi: 10.1136/qshc.2008.028043. [DOI] [PubMed] [Google Scholar]
- 47.Katon WJ, Lin EH, Von Korff M, Ciechanowski P, Ludman EJ, Young B, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363:2611–20. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Leventhal ME, Denhaerynck K, Brunner-La Rocca HP, Burnand B, Conca-Zeller A, Bernasconi AT, et al. Swiss Interdisciplinary Management Programme for Heart Failure (SWIM-HF): a randomised controlled trial study of an outpatient inter-professional management programme for heart failure patients in Switzerland. Swiss Med Wkly. 2011;141:w13171. doi: 10.4414/smw.2011.13171. [DOI] [PubMed] [Google Scholar]
- 49.Mohler R, Bartoszek G, Meyer G. Quality of reporting of complex healthcare interventions and applicability of the CReDECI list - a survey of publications indexed in PubMed. BMC Med Res Methodol. 2013;13:125. doi: 10.1186/1471-2288-13-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Borosund E, Ruland CM, Moore S, Ekstedt M. Nurses’ experiences of using an interactive tailored patient assessment tool one year past implementation. Int J Med Inform. 2013;83(7):e23–34. doi: 10.1016/j.ijmedinf.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 51.Hibbard JH, Greene J, Overton V. Patients with lower activation associated with higher costs; delivery systems should know their patients’ ‘scores’. Health Aff (Millwood) 2013;32:216–22. doi: 10.1377/hlthaff.2012.1064. [DOI] [PubMed] [Google Scholar]


