Abstract
OBJECTIVE:
The purpose of this study was to systematically review the research on volume and outcome relationships in critical care.
METHODS:
From January 1, 2001, to April 30, 2014, MEDLINE and EMBASE were searched for studies assessing the relationship between admission volume and clinical outcomes in critical illness. Bibliographies were reviewed to identify other articles of interest, and experts were contacted about missing or unpublished studies. Of 127 studies reviewed, 46 met inclusion criteria, covering seven clinical conditions. Two investigators independently reviewed each article using a standardized form to abstract information on key study characteristics and results.
RESULTS:
Overall, 29 of the studies (63%) reported a statistically significant association between higher admission volume and improved outcomes. The magnitude of the association (mortality OR between the lowest vs highest stratum of volume centers), as well as the thresholds used to characterize high volume, varied across clinical conditions. Critically ill patients with cardiovascular (n = 7, OR = 1.49 [1.11-2.00]), respiratory (n = 12, OR = 1.20 [1.04-1.38]), severe sepsis (n = 4, OR = 1.17 [1.03-1.33]), hepato-GI (n = 3, OR = 1.30 [1.08-1.78]), neurologic (n = 3, OR = 1.38 [1.22-1.57]), and postoperative admission diagnoses (n = 3, OR = 2.95 [1.05-8.30]) were more likely to benefit from admission to higher-volume centers compared with lower-volume centers. Studies that controlled for ICU or hospital organizational factors were less likely to find a significant volume-outcome relationship than studies that did not control for these factors.
CONCLUSIONS:
Critically ill patients generally benefit from care in high-volume centers, with more substantial benefits in selected high-risk conditions. This relationship may in part be mediated by specific ICU and hospital organizational factors.
Volume-outcome relationships are well established in many surgical conditions and high-risk procedures in health care.1 Under these relationships, higher numbers of procedures are thought to lead to better patient outcomes through the development of procedural skill.2 Such observations lend conceptual support to the development of regionalized systems of surgical care, in which patients are selectively referred to high-volume providers.3 Selective referral has substantially improved the quality of care for patients in need of these planned high-risk procedures, with improved outcomes over time due in large part to concentration of care.2
Given the current shortage of ICU physicians and the overall complexity of critical illness, critical care is also an attractive target for regionalization. However, unlike in many surgical conditions, the volume-outcome relationship in critical illness is still incompletely characterized.4 In the absence of a well-defined volume-outcome relationship, regionalization of critical care may increase costs while delaying definitive therapy for extremely sick patients in need of rapid diagnosis and treatment. Moreover, regionalization is only one potential strategy for region-wide organization of critical care.5 Without a greater understanding of the mechanism of the volume-outcome relationship, which may in part be determined by organizational factors that are correlated with volume, we may miss out on opportunities to improve outcomes for small-volume providers without large-scale reorganization of care.
The goal of this study was to perform a systematic review of literature to assess the volume-outcome relationship among critically ill adult patients. In addition to providing summary information, we sought to understand organizational factors that may be potential mechanisms for this effect by analyzing the differences between positive and negative studies.
Materials and Methods
We performed a systematic review of research studies examining the volume-outcome relationship in critical care. The complete review protocol was submitted to the PROSPERO registry of systematic reviews (CRD42011001265) prior to beginning the study search, study review, data extraction, and analyses.
Study Selection Criteria
Eligible studies were observational studies that assessed the association between critically ill admissions volume (at either the level of the hospital, ICU, ED, or physician) and patient mortality (within the ICU, hospital, or a fixed time period after admission). All observational studies including registries and retrospective observational analyses of existing clinical or administrative databases were eligible. We excluded studies on volume and outcome in trauma, neonatal critical care, and pediatric critical care as these service lines are already extensively regionalized. We also excluded studies when we either could not determine the proportion of patients who were admitted to an ICU or the proportion of patients in the ICU was < 50%.
Search Methods
To identify candidate studies we searched MEDLINE and EMBASE for English-language articles published between January 1, 2001, and April 30, 2014. Our search algorithm included medical subject heading terms and text words for both critical illness and clinical conditions that are likely to result in critical illness (e-Appendix 1 (149.2KB, pdf) , e-Table 1 (149.2KB, pdf) ). All searches were combined in a reference manager database (Resyweb). When articles separately analyzed distinct clinical conditions, we analyzed the data of each condition separately, treating the data as separate studies. We excluded studies published before 2001 because the practice of critical care and critical care outcomes has changed considerably since that time.6,7 We also searched several other sources: we reviewed the reference lists of selected studies, we contacted experts in the field to identify missed or unpublished studies, and we performed a manual examination of abstracts books from the main international meetings of critical care medicine (International Symposium on Intensive Care and Emergency Medicine, European Society Intensive Care Medicine Meeting, Society of Critical Care Medicine) between 2007 and 2014 to locate additional relevant titles. For studies published in abstract form, the primary author was contacted to identify manuscripts in progress.
Study Selection, Data Collection, and Analyses
Identifying Studies:
All retrieved records and reports were assessed independently by two authors. First, titles and abstracts were screened to identify obvious exclusions (ie, records that were found by our electronic searches but were clearly irrelevant to this review). Second, full-text reports were retrieved to determine whether they met the selection criteria. Any disagreements were resolved through discussion.
Data Extraction:
Data extraction was performed independently by two authors using a prespecified data extraction form. Information extracted included the following: study characteristics (study design, period, and setting); patient characteristics (inclusion and exclusion criteria); definition of volume (unit of measurement, continuous or categorical variable and, if categorical, thresholds); outcomes (mortality in the ED, ICU, hospital, or at a fixed time point, ICU, and hospital lengths of stay); statistical methods (multivariable modeling technique, adjustment for cluster effect, and list of adjustment variables); and structural characteristics of the ICU, hospital, and health system. We collected the effect size quantifying the strength of the association between volume and mortality. We collected all available estimates, regardless of the unit of measurement for volume, the method of operationalizing volume, the end point, and the type of statistical analysis, that is, according to the measurement unit of volume (at the hospital, unit, or care provider level), to the definition of the volume variable (continuous or categorical), to the end point (intensive care, in-hospital, or 30-day mortality), and according to the analysis (raw or adjusted estimates). For each study, two authors evaluated independently the risk of bias using a modification of a previously published approach to effectiveness reviews.8 This scale included attributes of risk adjustment, adjustment for correlated data, and adjustment for temporal trends.
Data Analysis
First, among selected studies, we checked the data used to exclude in the final analysis results from subpopulation of studies already included. For the synthesis, we initially planned to primarily focus on the volume treated as a continuous variable. However, the most frequently reported measure of the volume-outcome effect was the OR of death in patients treated in a low-volume center compared with patients treated in a high-volume center, so that an OR > 1 would indicate increased risk in low-volume compared with high-volume center. Because of considerable variability in the numbers of categories used (defined according to tertiles, quartiles, or quintiles) and in the thresholds used to define these categories, we focused on the effect comparing the lowest volume group with the highest volume group. For the synthesis, we used the adjusted ORs based on the multivariate model used in each study.
Separate meta-analyses were performed to combine the study estimates for each of the presenting problems in critical illness (respiratory, cardiovascular, neurologic, hepato-GI or renal diagnosis, sepsis, postoperative conditions, or any indications). Studies that lacked sufficient data to calculate an OR were excluded from the meta-analyses. Their results were analyzed qualitatively and are reported separately. Because some studies published in 2001 and later contained data from earlier time periods, we performed a sensitivity analysis in which we excluded all studies containing data earlier than 2001.
Higgins’ I2 statistics and between-study variance τ2 were calculated to assess the amount of heterogeneity across studies. The effect sizes were combined using a random-effects meta-analysis model because we expected a substantial heterogeneity due to diversity of design across studies. All reported P values were two-sided. Analyses were performed using Stata statistical software release 11 (StataCorp LP).
To assess potential mechanisms underlying the volume-outcome effect, we used a conceptual framework in which the ICU volume-outcome relationship could be attributed to three factors: acquisition of clinical skill at high-volume centers (“practice-makes-perfect”), selective referral to high-volume centers, and the presence of specific organizational factors that are associated with outcome and may be more common at high-volume centers.9 This last category includes structural factors that might be associated with high volume and high quality. At the ICU level, these might include ICU type,10 ICU size, ICU level, intensivist physician staffing,11 nurse-to-bed ratio,12 and intensivist-to-bed ratio. At the hospital level, these might include geographic position, hospital size, teaching status,13 technology capacity, trauma center designation,14 hospital, and ED level. This third factor is analogous to unmeasured confounding, since to the degree that these factors mediate the volume-outcome relationship, controlling for them would attenuate the observed effect. Therefore, to determine the role of organizational factors as a mechanism for the volume-outcome relationship, we qualitatively compared studies that did and did not control for these factors. To the degree that the results of volume-outcome studies depend on controlling for these factors, the volume-outcome relationship may be due to correlation between high-volume and ICU organizational best practices. To the degree that the results of volume-outcome studies do not depend on controlling for these factors, the volume-outcome relationship may be due to clinical skill and selective referral.
Results
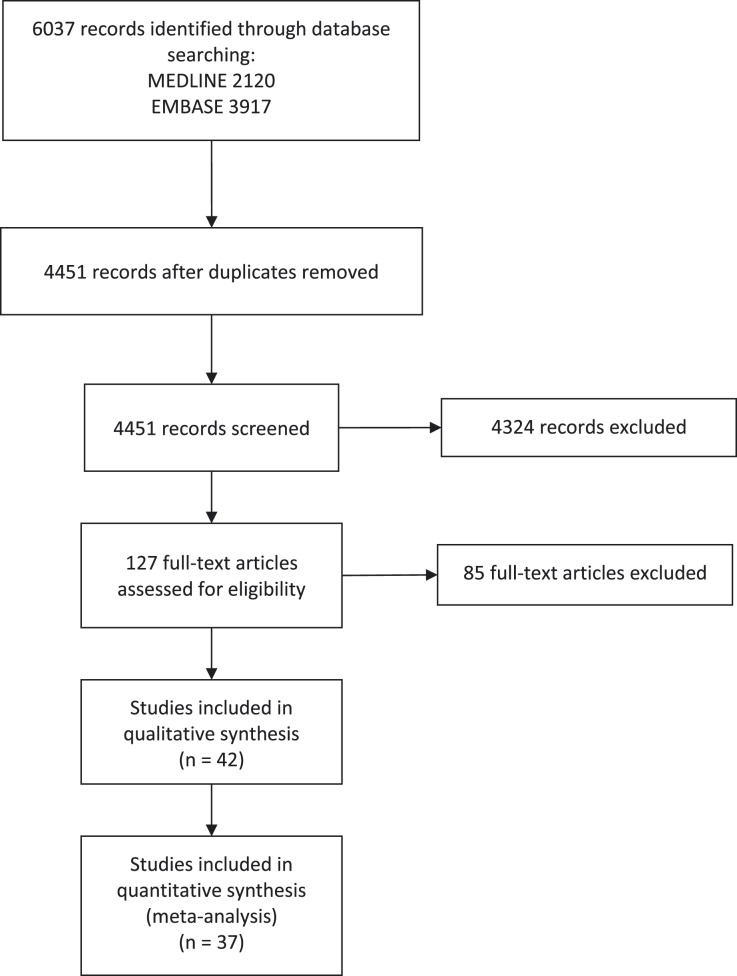
Of 6,037 potentially relevant references, we reviewed 127 publications fulfilling our search criteria, of which 42 references (33%) met all criteria for inclusion (Fig 1). One study reported three different patient subsets and was analyzed as three distinct studies.15 One study reported two different patient subsets and was analyzed as two distinct studies.16 One study reported the volume-outcome relationship in two different health-care systems; we analyzed the data as two different studies.17 We did not retrieve any reference from abstract books of the main international meetings of critical care medicine. This resulted in 46 distinct studies for analysis.
Figure 1 –
Flow diagram of study selection. The main reasons for exclusion of full-text articles were absence of details regarding ICU or hospital mortality or majority of population not including critically ill patients.
Study Characteristics
General study characteristics are shown in Table 1.18‐56 The majority of included studies were from North America (n = 25, 54%) and included data after 2001 (n = 35, 76%). Three studies included all ICU admissions.16,18,19 Seven clinical conditions were covered: respiratory diagnoses including mechanical ventilation, acute respiratory failure, and pneumonia (13 studies)15,16,20‐30; cardiovascular diagnoses including cardiac arrest and cardiogenic shock (eight studies)31‐38; sepsis (six studies)39‐44; neurologic diagnoses (three studies)15,45,46; hepato-GI diagnoses (three studies)15,47,48; renal diagnoses (three studies)17,49; and postoperative conditions including pancreatectomy, hepatectomy, esophagectomy, major vascular surgery (seven studies).50‐56 The majority of studies (n = 24, 52%) used clinical databases rather than administrative databases. The most common unit of analysis used was hospital volume (n = 25, 54%), followed by ICU volume (n = 14, 30%), ED volume (n = 4, 9%), and then intensivist volume (n = 1, 2%). The threshold used to differentiate low-volume and high-volume institutions varied greatly within and across clinical conditions. For 38 studies (83%), the primary outcome was hospital mortality, followed by 30-day mortality (n = 4, 9%), ICU mortality (n = 4, 8%), survival to admission from the ED (n = 2, 4%), perioperative death (n = 1, 2%), and early hospital mortality (n = 1, 2%). Only 10 studies (21%) reported ICU or hospital lengths of stay as secondary outcomes.
TABLE 1 ] .
General Characteristics of Included Studies
| Study/Year | Population | Country | Study Period | Type of Database | Unit of Analysis | Centers | Patients | Outcomes |
| Ananthakrishnan et al48/2008 | Medical (acute liver failure) and surgical (liver transplant) | USA | 2001-2004 | Administrative | Hospital | Unknown | 25,907 | In-hospital mortality |
| Callaway et al31/2010 | Medical (cardiac arrest) | USA and Canada | 2005-2007 | Clinical | Hospital | 254 | 4,087 | In-hospital mortality |
| Carr et al32/2009 | Medical (cardiac arrest) | USA | 2002-2005 | Clinical | Hospital | 39 | 4,674 | In-hospital mortality |
| Chen et al33/2003 | Medical (intraaortic balloon pump) | USA | 1994-1998 | Clinical | Hospital | 750 | 12,730 | In-hospital mortality |
| Cha et al34/2012 | Medical (cardiac arrest) | South Korea | 2006-2008 | Administrative | ED | 679 | 27,662 | In-hospital mortality |
| Cooke et al20/2012 | Medical (mechanical ventilation) | USA | 2009 | Administrative | Hospital | 119 | 5,131 | 30-d mortality |
| Cross et al45/2003 | Medical and surgical (subarachnoid hemorrhage) | USA | 1998-2000 | Administrative | Hospital | 1,546 | 16,399 | In-hospital mortality |
| Cudnik et al35/2012 | Medical (cardiac arrest) | USA | 2009 | Clinical | Hospital | 155 | 4,125 | In-hospital mortality |
| Darmon et al21/2011 | Medical (mechanical ventilation) | France | 2004-2005 | Administrative | Hospital | 294 | 179,197 | In-hospital mortality |
| Dimick et al51/2002 | Surgical (hepatic resection) | USA | 1994-1998 | Clinical | Hospital | 52 | 569 | In-hospital mortality |
| Dimick et al50/2003 | Surgical (esophageal resection) | USA | 1994-1998 | Administrative | Hospital and surgeon | 35 | 366 | In-hospital mortality |
| Durairaj et al15/2005 | Medical (respiratory) | USA | 1991-1997 | Clinical | Hospital | 29 | 16,949 | In-hospital mortality |
| Durairaj et al15/2005 | Medical (neurologic) | USA | 1991-1997 | Clinical | Hospital | 29 | 13,805 | In-hospital mortality |
| Durairaj et al15/2005 | Medical (GI) | USA | 1991-1997 | Clinical | Hospital | 29 | 12,881 | In-hospital mortality |
| Giles et al52/2009 | Surgical (ruptured aortic abdominal aneurysm) | USA | 2000-2005 | Administrative | Hospital | Unknown | 28,429 | In-hospital mortality |
| Glance et al18/2006 | Medical and surgical | USA | 2001-2003 | Clinical | ICU | 92 | 70,757 | In-hospital mortality |
| Gopal et al22/2011 | Medical (mechanical ventilation) | England | 1996-2006 | Clinical | Hospital | 12 | 17,132 | ICU mortality |
| Joseph et al53/2009 | Surgical (pancreatic resection) | USA | 2005 | Administrative | Hospital | 434 | Unknown | Perioperative death |
| Kahn et al23/2006 | Medical (mechanical ventilation) | USA | 2002-2003 | Clinical | Hospital | 37 | 20,241 | In-hospital mortality/ICU mortality |
| Kahn et al24/2009 | Medical (mechanical ventilation) | USA | 2004-2006 | Administrative | Hospital | 169 | 30,677 | 30-d mortality |
| Knipp et al54/2007 | Surgical (aortic dissection) | USA | 1995-2003 | Administrative | Hospital | Unknown | 3,013 | In-hospital mortality |
| Kuo et al55/2001 | Surgical (esophageal resection) | USA | 1992-1999 | Administrative | Hospital | 64 | 1,193 | In-hospital mortality |
| Lecuyer et al25/2008 | Medical (acute respiratory failure) | France | 1997-2004 | Clinical | ICU | 28 | 1,753 | ICU mortality |
| Lin et al26/2008 | Medical (pneumonia) | Taiwan | 2002-2004 | Administrative | Physician | Unknown | 87,479 | 30-d mortality |
| Macomber et al56/2012 | Liver transplantation | USA | 2009-2010 | Administrative | Hospital | 63 | 5,130 | In-hospital mortality |
| Metnitz et al19/2009 | Medical and surgical | Austria | 1998-2005 | Clinical | ICU | 40 | 83,259 | In-hospital mortality |
| Moran et al28/2008 | Medical and surgical (mechanical ventilation) | Australia and New Zealand | 1995-2009 | Clinical | ICU | 136 | 208,810 | In-hospital mortality |
| Needham et al27/2006 | Medical and surgical (mechanical ventilation) | Canada | 1998-2000 | Administrative | Hospital | 95 (surgical); 126 (medical) | 20,219 | 30-d mortality |
| Nguyen et al17/2011 | Medical (renal failure) | France | 1997-2004 | Clinical | ICU | 32 | 9,449 | In-hospital mortality |
| Nguyen et al17/2011 | Medical (renal failure) | USA | 1997-2004 | Clinical | ICU | 76 | 3,498 | In-hospital mortality |
| Nuño et al46/2012 | Medical and surgical (subarachnoid hemorrhage) | USA | 2002-2007 | Administrative | Hospital | Unknown | 47,114 | In-hospital mortality |
| Peelen et al40/2007 | Medical (sepsis) | The Netherlands | 2003-2005 | Clinical | ICU | 28 | 4,605 | In-hospital mortality |
| Powell et al39/2010 | Medical (sepsis) | USA | 2007 | Administrative | ED | 551 | 87,166 | In-hospital mortality and early hospital mortality |
| Shahin et al41/2012 | Medical (sepsis) | UK | 2008-2009 | Clinical | ICU | 170 | 30,727 | In-hospital mortality |
| Shin et al36/2011 | Medical (cardiac arrest) | South Korea | 2006-2007 | Clinical | ED | 410 | 20,457 | Survival to admission |
| Stub et al37/2011 | Medical (cardiac arrest) | Australia | 2003-2010 | Clinical | Hospital | 70 | 2,706 | In-hospital mortality |
| Ro et al38/2012 | Medical (cardiac arrest) | South Korea | 2006-2008 | Clinical | ED | 410 | 10,425 | Survival to admission and in-hospital mortality |
| Vaara et al49/2012 | Medical (renal failure) | Finland | 2007-2008 | Administrative | ICU | 23 | 1,558 | In-hospital mortality |
| Zuber et al42/2012 | Medical and surgical (sepsis) | France | 1997-2008 | Clinical | ICU | 41 | 3,437 | In-hospital mortality |
| Banta et al43/2012 | Medical and surgical (sepsis) | USA | 2005-2010 | Administrative | Hospital | Unknown | 1,213,219 | In-hospital mortality |
| Shen et al47/2012 | Medical (acute pancreatitis) | Taiwan | 2000-2009 | Administrative | Hospital | 806 | 22,551 | In-hospital mortality |
| Dres et al29/2013 | Medical (acute respiratory failure) | France | 1998-2001 | Clinical | ICU | 31 | 14,440 | In-hospital mortality, ICU mortality |
| Fernández et al16/2013 | Medical and surgical | Spain | 2008 | Clinical | ICU | 29 | 4,001 | In-hospital mortality |
| Fernández et al16/2013 | Medical and surgical (mechanical ventilation) | Spain | 2008 | Clinical | ICU | 29 | 1,923 | In-hospital mortality |
| Shahin et al30/2014 | Medical and surgical (mechanical ventilation) | UK | 2008-2010 | Administrative | ICU | 193 | 104,844 | In-hospital mortality |
| Walkey and Wiener44/2014 | Medical and surgical (sepsis) | USA | 2011 | Clinical | ICU | 124 | 56,997 | Hospital mortality index |
UK = United Kingdom; USA = United States of America.
Summary of Findings of Included Studies
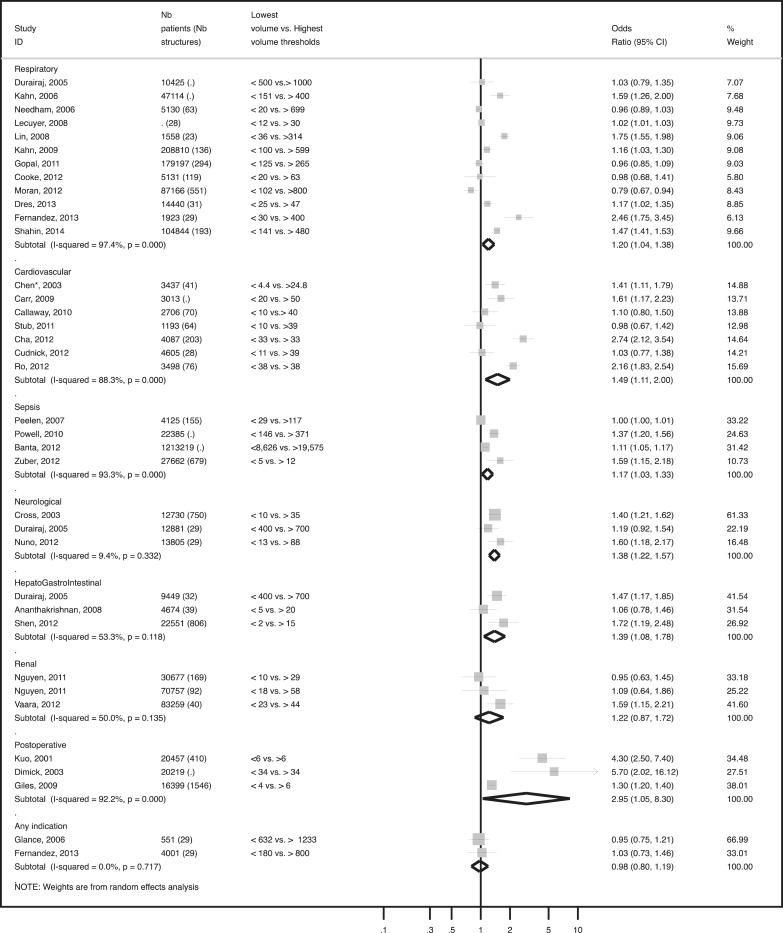
Figure 2 shows the meta-analyses of adjusted ORs comparing the lowest-volume group with the highest-volume group in seven conditions separately. Eight studies could not be included in the final analyses because they had insufficient data to calculate OR.19,21,41,44,51,53,54,56 The results of these studies are presented in Table 2. Among the remaining studies (n = 37), the consistency of the relationship varied considerably across diagnoses. All studies including patients with sepsis (n = 4) or patients with postoperative diagnosis (n = 3) found a positive association between volume and outcome. In studies looking at the subset of patients with respiratory (n = 7), cardiovascular (n = 4), hepato-GI (n = 2), and neurologic (n = 2) diagnoses, there was on average a positive association between higher volume and better outcomes. However, there was substantial heterogeneity, especially in subsets of patients with respiratory, cardiovascular, sepsis, and postoperative diagnoses (I2 = 97.4%, 88.3%, 98%, 92.2% respectively). Conversely, in studies looking at a subset of patients with renal diagnosis (n = 3), the meta-analyses did not demonstrate a significant association and there was also considerable between-trial heterogeneity (I2 = 50%). One study in patients with respiratory diagnoses documented a statistically significant association between higher volume and poorer outcomes.28
Figure 2 –
Forrest plots of comparisons between lowest and highest volume institutions for seven clinical conditions. Nb = number.
TABLE 2 ] .
Summary of Studies Not Included in the Meta-analysis
| Clinical Condition | Positive Association | No Association |
| Respiratory | Darmon et al21/2011 | … |
| Sepsis | Walkey and Wiener44/2014 | Shahin et al41/2012 |
| Neurologic | … | … |
| Hepato-GI | … | … |
| Renal | … | … |
| Postoperative | Dimick et al51/2002 | Joseph et al53/2009 |
| Knipp et al54/2007 | … | |
| Macomber et al56/2012 | … | |
| Any indication | Metnitz et al19/2009 | … |
Between categories of medical conditions (respiratory, cardiovascular, neurologic, liver-GI, postoperative, and sepsis) high-volume to low-volume thresholds varied greatly. For respiratory diagnoses, the highest volume quartile > 699 showed a nonsignificant relationship between volume and outcome, whereas studies on cardiac arrest with 50 cases per year were more likely to show a significant relationship.
The highest absolute hospital mortality differences between high-volume and low-volume institutions were found for hematologic patients with acute respiratory failure (36%), cardiac arrest (22%), cardiogenic shock and intraaortic balloon pump (14.8%), endovascular repair of ruptured abdominal aortic aneurysm (22%), and postesophagectomy (12.9%). These diagnoses shared the characteristic of being associated with the highest mortality rates within their diagnosis category.
Sensitivity Analysis
Figure 3 shows the meta-analyses of adjusted ORs comparing the lowest-volume group with the highest-volume group in seven conditions, after exclusion of eight studies with the majority of data from before 2001 (studies of Durairaj et al,15 Needham et al,27 Chen et al,33 Cross et al,45 Dimick et al,50 Kuo et al55). The volume-outcome association remained unchanged after exclusion of these studies.
Figure 3 –
Sensitivity analysis: Forrest plots of comparisons between lowest and highest volume institutions for seven clinical conditions after exclusion of studies with data older than 2001. See Figure 2 legend for expansion of abbreviation.
Relationship Between Organizational Factors and Primary Study Results:
Eighteen studies (39%) did not adjust their results to any ICU or hospital-level factor (Table 3). Studies that did not find a statistically significant association between higher patient volume and better outcomes were more likely to have adjusted their results for ICU-level factors (such as ICU type, ICU level, intensivist staffing model, nurse-to-bed ratio) and hospital-level factors (such as geographical position, teaching status, technological capacity, trauma center designation, or hospital level), compared with studies that did find a statistically significant association (Table 3).
TABLE 3 ] .
Relationship Between Methodologic Characteristics, ICU, and Hospital-Level Confounders and Primary Study Results
| Study Characteristics | Positive Studies (n = 29, 63%) | Negative Studies (n = 17, 37%) |
| Unit of volume measure, No. (%) | ||
| Hospital | 15 (58) | 11 (42) |
| ICU | 8 (57) | 6 (43) |
| ED | 2 (100) | 0 (0) |
| Intensivist | 4 (100) | 0 (0) |
| Sample size, No. (%) | ||
| < 10,000 | 9 (53) | 8 (47) |
| 10,000-50,000 | 14 (70) | 6 (30) |
| > 50,000 | 6 (75) | 2 (25) |
| Unknown | … | 1 (100) |
| Location, No. (%) | ||
| North America | 15 (58) | 11 (42) |
| Europe | 9 (69) | 4 (31) |
| Other | 5 (71) | 2 (29) |
| Risk of adjustment | ||
| Clinical | 15 (52) | 14 (48) |
| Administrative data with clinical adjustment | 13 (87) | 2 (13) |
| Administrative | 1 (50) | 1 (50) |
| ICU-level factors, No. (%) | ||
| ICU type | 1 (25) | 3 (75) |
| ICU size | 1 (100) | 0 (0) |
| ICU level | 0 (0) | 1 (100) |
| Intensivist staffing model | 2 (50) | 2 (50) |
| Nurse-to-bed ratio | 1 (50) | 1 (50) |
| Intensivist-to-bed ratio | 1 (100) | 0 (0) |
| Hospital-level factors, No. (%) | ||
| Hospital size | 7 (88) | 1 (12) |
| Teaching status | 7 (47) | 8 (53) |
| Technological capacity | 2 (40) | 3 (60) |
| Trauma center designation | 0 (0) | 2 (100) |
| Hospital level | 0 (0) | 1 (100) |
| ED level | 2 (100) | 0 (0) |
ICU level (defined by the US Department of Veterans Affairs national bed control database): level 1 and 2 ICUs are where most subspecialty care and intervention are available. Level 3 and 4 ICUs provide more limited subspecialty care and intervention. Hospital level (defined in the Australian and New Zealand Intensive Care Society database): rural, metropolitan, tertiary, private. ED level (defined by the Korean government): level 1 and 2 are covered by emergency physicians 24/24; level 3 is basically equipped and usually served by general physicians.
All studies performed some risk adjustment (Table 4). Two studies (4%) used risk adjustment based on administrative data alone, 15 (33%) used risk adjustment based on a combination of administrative and some clinical data, and 30 (65%) used risk adjustment based on clinical models with historically good calibration and discrimination. Most adjusted for demographic characteristics such as age (n = 45, 98%) and sex (n = 36, 78%). Around one-half of studies (n = 22, 48%) adjusted for patient comorbidities; 34 studies (74%) adjusted for severity of illness using a physiologic measure. Eighteen (39%) adjusted for admission source. Thirteen (28%) adjusted for the diagnosis at admission. Other patient adjustments included insurance status (n = 5, 11%), race (n = 7, 15%), functional status (n = 2, 4%), ICU pre-length of stay (n = 3, 7%), life support measures (n = 6, 13%), the type of malignancy (n = 2, 4%), and the known prognostic for cardiac arrest (n = 6, 13%).
TABLE 4 ] .
Quality of Included Studies
| Study/Year | Attributes of Risk Adjustment | Adjustment for Correlated Data | Adjustment for Temporal Trendsa |
| Ananthakrishnan et al48/2008 | Clinical | No | No |
| Callaway et al31/2010 | Clinical | No | No |
| Carr et al32/2009 | Clinical | Yes | No |
| Chen et al33/2003 | Clinical | No | No |
| Cha et al34/2012 | Administrative with clinical risk adjustment | Yes | No |
| Cooke et al20/2012 | Administrative with clinical risk adjustment | Yes | … |
| Cross et al45/2003 | Administrative with clinical risk adjustment | Yes | Yes |
| Cudnik et al35/2012 | Clinical | Yes | … |
| Darmon et al21/2011 | Clinical | No | No |
| Dimick et al51/2002 | Clinical | Yes | No |
| Dimick et al50/2003 | Clinical | No | No |
| Durairaj et al15/2005 | Clinical | Yes | No |
| Durairaj et al15/2005 | Clinical | Yes | No |
| Durairaj et al15/2005 | Clinical | Yes | No |
| Giles et al52/2009 | Administrative | No | Yes |
| Glance et al18/2006 | Clinical | Yes | No |
| Gopal et al22/2011 | Clinical | Yes | Yes |
| Joseph et al53/2009 | Administrative | No | … |
| Kahn et al23/2006 | Clinical | Yes | … |
| Kahn et al24/2009 | Administrative with clinical risk adjustment | Yes | … |
| Knipp et al54/2007 | Administrative with clinical risk adjustment | No | No |
| Kuo et al55/2001 | Administrative with clinical risk adjustment | Yes | Yes |
| Lecuyer et al25/2008 | Clinical | Yes | No |
| Lin et al26/2008 | Administrative with clinical risk adjustment | Yes | No |
| Macomber et al56/2012 | Administrative with clinical risk adjustment | Yes | Yes |
| Metnitz et al19/2009 | Clinical | Yes | Yes |
| Moran et al28/2008 | Clinical | Yes | Yes |
| Needham et al27/2006 | Administrative with clinical risk adjustment | Yes | No |
| Nguyen et al17/2011 | Clinical | Yes | No |
| Nguyen et al17/2011 | Clinical | Yes | No |
| Nuño et al46/2012 | Administrative with clinical risk adjustment | Yes | No |
| Peelen et al40/2007 | Clinical | Yes | No |
| Powell et al39/2010 | Administrative with clinical risk adjustment | Yes | … |
| Shahin et al41/2012 | Clinical | … | … |
| Shin et al36/2011 | Clinical | Yes | … |
| Stub et al37/2011 | Clinical | No | No |
| Ro et al38/2012 | Clinical | Yes | No |
| Vaara et al49/2012 | Administrative with clinical risk adjustment | Yes | … |
| Zuber et al42/2012 | Clinical | No | Yes |
| Banta et al43/2012 | Administrative with clinical risk adjustment | Yes | Yes |
| Shen et al47/2012 | Administrative with clinical risk adjustment | Yes | No |
| Dres et al29/2013 | Clinical | Yes | Yes |
| Fernández et al16/2013 | Clinical | Yes | … |
| Fernández et al16/2013 | Clinical | Yes | … |
| Shahin et al30/2014 | Administrative with clinical risk adjustment | Yes | … |
| Walkey and Wiener44/2014 | Clinical | Yes | … |
For studies longer than 2 y.
Discussion
We evaluated 40 studies on the volume-outcome relationship in broadly defined critically ill patients. The majority of studies found that patients admitted in high-volume structures had better outcomes, although the consistency and magnitude of the relationship, as well as the thresholds used to differentiate low-volume and high-volume centers, varied across clinical conditions. Studies showing no volume-outcome relationship were more likely to have adjusted their results for key ICU or hospital-level organizational factors.
Our results extend those of a prior systematic review in two ways.4 First, we include many more studies (46 vs 13, several of which were published recently). Second, we specifically examine the characteristics of positive vs negative studies, providing new insight into the potential mechanism of the volume-outcome relationship not addressed in the prior review.
Within diagnosis categories, those with the highest risk of death are most likely to benefit from admission to a high-volume center. This variation of the volume-outcome relationship may be related to the complexity of diagnosis and management in these conditions. Durairaj et al15 found that in comparison with a nonselected population of patients who were mechanically ventilated, only the most severe (ie, with an APACHE [Acute Physiology and Chronic Health Evaluation] III score > 57) benefited from high-volume hospitals. Glance et al18 showed that only critically ill patients with a Simplified Acute Physiology Score (SAPS) 2 ≥ 30 benefited from a high-volume center. Darmon et al21 found that in comparison with patients with ARDS who were mechanically ventilated, those with toxic coma did not benefit from mechanical ventilation admissions volume. Lecuyer et al25 and Zuber et al42 both looked at the subset of hematologic patients with acute respiratory failure or severe sepsis, finding large benefits from high-volume ICUs (OR = 0.63 [0.46-0.87]).
Only one study documented a statistically significant association between higher volume and worse outcomes.28 The underlying reason for this result may be related to either the total workload or overall capacity strain in high-volume centers, which may be related to poor outcomes.57 For one clinical condition category (patients undergoing renal support therapy), we were not able to find any association between volume and outcome.17 Among the plausible explanations may be use of patients receiving dialysis as the unit of measurement (rather than the number of dialysis sessions performed, which may be more directly related to clinical experience) or the lack of inclusion of other relevant outcomes besides mortality (ie, renal function recovery). Additionally, renal support therapy is guided by an uncertain evidence base with regard to timing, the use continuous vs intermittent dialysis, and the dose of dialysis. Thus, clinical experience may not translate into higher outcomes for this condition.
We observed large differences among the thresholds used to differentiate low-volume and high-volume centers between and within clinical condition categories. These differences mainly related to the prevalence of the diagnoses, and may be partly explained by variation in ICU bed availability across industrialized countries and the median size of acute care hospitals.58 Countries with a large number of ICU beds are more likely to have a less restricted ICU admission policy and may admit less severe patients.59 Our review highlights that the shape of the volume-outcome relationship varies within and across clinical condition categories. Consequently, our results do not support recommendations of minimal ICU volumes for diagnosis categories.
Adjustments for ICU or hospital-level factors seem to be a major determinant of the volume-outcome relationship. Within studies looking at the volume-outcome relationship among postoperative patients admitted in the ICU, those of Joseph et al53 and Dimick et al50 were not able to find any association. One explanation might be related to the adjustments of their results to managerial factors known to be associated with better outcomes (such as ICU staffing and the presence of a daily round by an intensivist) or to the technology capacity of their structures (such as the presence of an interventional radiology service). Similarly, the two studies on cardiac arrest that found negative results are those where the authors (Callaway et al31 and Stub et al37) adjusted their results for organizational factors known to be associated with improved outcomes (ie, trauma center, cardiac center, 24-h cardiac interventional services). Again, these results emphasize the idea that the volume affected may be mediated in part by organizational factors that have a major impact on patient outcomes. To the degree that the volume outcome is in part mediated by organizational factors, increasing the size of low-volume centers or systematically transferring patients from low-volume to high-volume centers may not be the most efficient way to improve outcomes. Instead of conjunction, it may be beneficial to “export” organizational best practices to small-volume ICUs to improve their quality without systematically transferring patients.
Our study has several limitations. First, our systematic review may suffer from publication bias. Due to public health implications, studies showing no volume-outcome relationship might have more difficulties being published. Second, the majority of studies did not adjust their results to organizational factors and none directly adjusted for processes of care used. Thus, we had only a limited ability to assess for the mechanism of the volume-outcome relationship. Third, all studies used mortality as the primary outcome, though other patient outcomes such as discharge location, quality of life, and cognitive status are also patient-centered and outcomes of interest. Fourth, due to variation in the way that studies categorized volume and the lack of studies looking precisely at the volume-outcome relationship as a continuous variable, we could not directly assess for a “dose-response” effect. Fifth, our study may suffer from reporting bias. We may have excluded studies from critical care surgical literature that do not explicitly report ICU use.
In summary, critically ill patients appear to benefit from care in high-volume hospitals, though there is not complete consistency in this relationship. Variability may be partly explained by case mix, diagnosis complexity, and the type of adjustments. Our results highlight the major role of organizational factors on patient outcomes and that specific management and care practices may allow low-volume centers to provide a high quality of care.
Supplementary Material
Online Supplement
Acknowledgments
Author contributions: B. G. is the guarantor of the entire manuscript. Y.-L. N. and D. J. W. contributed to drafting the manuscript; Y.-L. N., D. J. W., Y. Y., L. T., and J. B. contributed to statistical analyses; Y.-L. N., D. J. W., Y. Y., L. T., D. C. A., J. M. K., P. R., and B. G. contributed to the critical revision of the manuscript for important intellectual content; and all authors read and approved the final manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts of interest: Dr Kahn receives in-kind research support from the Cerner Corporation. Drs Nguyen, Wallace, Yordanov, Trinquart, Angus, Ravaud, and Guidet and Ms Blomkvist have reported that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Additional information: The e-Appendix and e-Table can be found in the Supplemental Materials section of the online article.
Footnotes
FUNDING/SUPPORT: The authors have reported to CHEST that no funding was received for this study.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137(6):511-520. [DOI] [PubMed] [Google Scholar]
- 2.Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364(22):2128-2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128-1137. [DOI] [PubMed] [Google Scholar]
- 4.Kanhere MH, Kanhere HA, Cameron A, Maddern GJ. Does patient volume affect clinical outcomes in adult intensive care units? Intensive Care Med. 2012;38(5):741-751. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen YL, Kahn JM, Angus DC. Reorganizing adult critical care delivery: the role of regionalization, telemedicine, and community outreach. Am J Respir Crit Care Med. 2010;181(11):1164-1169. [DOI] [PubMed] [Google Scholar]
- 6.The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301-1308. [DOI] [PubMed] [Google Scholar]
- 7.Esteban A, Anzueto A, Frutos F, et al. ; Mechanical Ventilation International Study Group. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002;287(3):345-355. [DOI] [PubMed] [Google Scholar]
- 8.Methods Guide for Effectiveness and Comparative Effectiveness Reviews. Rockville, MD: Agency for HealthCare Research and Quality; 2014. AHRQ Publication No. 10(14)-EHC063-RF. [PubMed] [Google Scholar]
- 9.Luft HS, Bunker JP, Enthoven AC. Should operations be regionalized? The empirical relation between surgical volume and mortality. N Engl J Med. 1979;301(25):1364-1369. [DOI] [PubMed] [Google Scholar]
- 10.Lott JP, Iwashyna TJ, Christie JD, Asch DA, Kramer AA, Kahn JM. Critical illness outcomes in specialty versus general intensive care units. Am J Respir Crit Care Med. 2009;179(8):676-683. [DOI] [PubMed] [Google Scholar]
- 11.Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288(17):2151-2162. [DOI] [PubMed] [Google Scholar]
- 12.Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, Harris M. Nurse staffing and inpatient hospital mortality. N Engl J Med. 2011;364(11):1037-1045. [DOI] [PubMed] [Google Scholar]
- 13.Hartz AJ, Krakauer H, Kuhn EM, et al. Hospital characteristics and mortality rates. N Engl J Med. 1989;321(25):1720-1725. [DOI] [PubMed] [Google Scholar]
- 14.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366-378. [DOI] [PubMed] [Google Scholar]
- 15.Durairaj L, Torner JC, Chrischilles EA, Vaughan Sarrazin MS, Yankey J, Rosenthal GE. Hospital volume-outcome relationships among medical admissions to ICUs. Chest. 2005;128(3):1682-1689. [DOI] [PubMed] [Google Scholar]
- 16.Fernández R, Altaba S, Cabre L, et al. ; Sabadell Score Group. Relationship between volume and survival in closed intensive care units is weak and apparent only in mechanically ventilated patients. Anesthesiology. 2013;119(4):871-879. [DOI] [PubMed] [Google Scholar]
- 17.Nguyen YL, Milbrandt EB, Weissfeld LA, et al. Intensive care unit renal support therapy volume is not associated with patient outcome. Crit Care Med. 2011;39(11):2470-2477. [DOI] [PubMed] [Google Scholar]
- 18.Glance LG, Li Y, Osler TM, Dick A, Mukamel DB. Impact of patient volume on the mortality rate of adult intensive care unit patients. Crit Care Med. 2006;34(7):1925-1934. [DOI] [PubMed] [Google Scholar]
- 19.Metnitz B, Metnitz PG, Bauer P, Valentin A; ASDI Study Group. Patient volume affects outcome in critically ill patients. Wien Klin Wochenschr. 2009;121(1-2):34-40. [DOI] [PubMed] [Google Scholar]
- 20.Cooke CR, Kennedy EH, Wiitala WL, Almenoff PL, Sales AE, Iwashyna TJ. Despite variation in volume, Veterans Affairs hospitals show consistent outcomes among patients with non-postoperative mechanical ventilation. Crit Care Med. 2012;40(9):2569-2575. [DOI] [PubMed] [Google Scholar]
- 21.Darmon M, Azoulay E, Fulgencio JP, et al. Procedure volume is one determinant of centre effect in mechanically ventilated patients. Eur Respir J. 2011;37(2):364-370. [DOI] [PubMed] [Google Scholar]
- 22.Gopal S, O’Brien R, Pooni J. The relationship between hospital volume and mortality following mechanical ventilation in the intensive care unit. Minerva Anestesiol. 2011;77(1):26-32. [PubMed] [Google Scholar]
- 23.Kahn JM, Goss CH, Heagerty PJ, Kramer AA, O’Brien CR, Rubenfeld GD. Hospital volume and the outcomes of mechanical ventilation. N Engl J Med. 2006;355(1):41-50. [DOI] [PubMed] [Google Scholar]
- 24.Kahn JM, Ten Have TR, Iwashyna TJ. The relationship between hospital volume and mortality in mechanical ventilation: an instrumental variable analysis. Health Serv Res. 2009;44(3):862-879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lecuyer L, Chevret S, Guidet B, et al. Case volume and mortality in haematological patients with acute respiratory failure. Eur Respir J. 2008;32(3):748-754. [DOI] [PubMed] [Google Scholar]
- 26.Lin HC, Xirasagar S, Chen CH, Hwang YT. Physician’s case volume of intensive care unit pneumonia admissions and in-hospital mortality. Am J Respir Crit Care Med. 2008;177(9):989-994. [DOI] [PubMed] [Google Scholar]
- 27.Needham DM, Bronskill SE, Rothwell DM, et al. Hospital volume and mortality for mechanical ventilation of medical and surgical patients: a population-based analysis using administrative data. Crit Care Med. 2006;34(9):2349-2354. [DOI] [PubMed] [Google Scholar]
- 28.Moran JL, Bristow P, Solomon PJ, George C, Hart GK; Australian and New Zealand Intensive Care Society Database Management Committee (ADMC). Mortality and length-of-stay outcomes, 1993-2003, in the binational Australian and New Zealand intensive care adult patient database. Crit Care Med. 2008;36(1):46-61. [DOI] [PubMed] [Google Scholar]
- 29.Dres M, Tran TC, Aegerter P, et al. ; CUB-REA Group. Influence of ICU case-volume on the management and hospital outcomes of acute exacerbations of chronic obstructive pulmonary disease. Crit Care Med. 2013;41(8):1884-1892. [DOI] [PubMed] [Google Scholar]
- 30.Shahin J, Harrison DA, Rowan KM. Is the volume of mechanically ventilated admissions to UK critical care units associated with improved outcomes? Intensive Care Med. 2014;40(3):353-360. [DOI] [PubMed] [Google Scholar]
- 31.Callaway CW, Schmicker R, Kampmeyer M, et al. ; Resuscitation Outcomes Consortium (ROC) Investigators. Receiving hospital characteristics associated with survival after out-of-hospital cardiac arrest. Resuscitation. 2010;81(5):524-529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carr BG, Kahn JM, Merchant RM, Kramer AA, Neumar RW. Inter-hospital variability in post-cardiac arrest mortality. Resuscitation. 2009;80(1):30-34. [DOI] [PubMed] [Google Scholar]
- 33.Chen EW, Canto JG, Parsons LS, et al. ; Investigators in the National Registry of Myocardial Infarction 2. Relation between hospital intra-aortic balloon counterpulsation volume and mortality in acute myocardial infarction complicated by cardiogenic shock. Circulation. 2003;108(8):951-957. [DOI] [PubMed] [Google Scholar]
- 34.Cha WC, Lee SC, Shin SD, Song KJ, Sung AJ, Hwang SS. Regionalisation of out-of-hospital cardiac arrest care for patients without prehospital return of spontaneous circulation. Resuscitation. 2012;83(11):1338-1342. [DOI] [PubMed] [Google Scholar]
- 35.Cudnik MT, Sasson C, Rea TD, et al. Increasing hospital volume is not associated with improved survival in out of hospital cardiac arrest of cardiac etiology. Resuscitation. 2012;83(7):862-868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shin SD, Suh GJ, Ahn KO, Song KJ. Cardiopulmonary resuscitation outcome of out-of-hospital cardiac arrest in low-volume versus high-volume emergency departments: An observational study and propensity score matching analysis. Resuscitation. 2011;82(1):32-39. [DOI] [PubMed] [Google Scholar]
- 37.Stub D, Smith K, Bray JE, Bernard S, Duffy SJ, Kaye DM. Hospital characteristics are associated with patient outcomes following out-of-hospital cardiac arrest. Heart. 2011;97(18):1489-1494. [DOI] [PubMed] [Google Scholar]
- 38.Ro YS, Shin SD, Song KJ, et al. A comparison of outcomes of out-of-hospital cardiac arrest with non-cardiac etiology between emergency departments with low- and high-resuscitation case volume. Resuscitation. 2012;83(7):855-861. [DOI] [PubMed] [Google Scholar]
- 39.Powell ES, Khare RK, Courtney DM, Feinglass J. Volume of emergency department admissions for sepsis is related to inpatient mortality: results of a nationwide cross-sectional analysis. Crit Care Med. 2010;38(11):2161-2168. [DOI] [PubMed] [Google Scholar]
- 40.Peelen L, de Keizer NF, Peek N, Scheffer GJ, van der Voort PH, de Jonge E. The influence of volume and intensive care unit organization on hospital mortality in patients admitted with severe sepsis: a retrospective multicentre cohort study. Crit Care. 2007;11(2):R40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shahin J, Harrison DA, Rowan KM. Relation between volume and outcome for patients with severe sepsis in United Kingdom: retrospective cohort study. BMJ. 2012;344:e3394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zuber B, Tran T-C, Aegerter P, et al. ; CUB-Réa Network. Impact of case volume on survival of septic shock in patients with malignancies. Crit Care Med. 2012;40(1):55-62. [DOI] [PubMed] [Google Scholar]
- 43.Banta JE, Joshi KP, Beeson L, Nguyen HB. Patient and hospital characteristics associated with inpatient severe sepsis mortality in California, 2005-2010. Crit Care Med. 2012;40(11):2960-2966. [DOI] [PubMed] [Google Scholar]
- 44.Walkey AJ, Wiener RS. Hospital case volume and outcomes among patients hospitalized with severe sepsis. Am J Respir Crit Care Med. 2014;189(5):548-555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cross DT, III, Tirschwell DL, Clark MA, et al. Mortality rates after subarachnoid hemorrhage: variations according to hospital case volume in 18 states. J Neurosurg. 2003;99(5):810-817. [DOI] [PubMed] [Google Scholar]
- 46.Nuño M, Patil CG, Lyden P, Drazin D. The effect of transfer and hospital volume in subarachnoid hemorrhage patients. Neurocrit Care. 2012;17(3):312-323. [DOI] [PubMed] [Google Scholar]
- 47.Shen HN, Lu CL, Li CY. The effect of hospital volume on patient outcomes in severe acute pancreatitis. BMC Gastroenterol. 2012;12:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ananthakrishnan AN, McGinley EL, Saeian K. Effect of hospital volume and teaching status on outcomes of acute liver failure. Liver Transpl. 2008;14(9):1347-1356. [DOI] [PubMed] [Google Scholar]
- 49.Vaara ST, Reinikainen M, Kaukonen KM, Pettilä V; Finnish Intensive Care Consortium. Association of ICU size and annual case volume of renal replacement therapy patients with mortality. Acta Anaesthesiol Scand. 2012;56(9):1175-1182. [DOI] [PubMed] [Google Scholar]
- 50.Dimick JB, Pronovost PJ, Cowan JA, Lipsett PA. Surgical volume and quality of care for esophageal resection: do high-volume hospitals have fewer complications? Ann Thorac Surg. 2003;75(2):337-341. [DOI] [PubMed] [Google Scholar]
- 51.Dimick JB, Pronovost PJ, Lipsett PA. The effect of ICU physician staffing and hospital volume on outcomes after hepatic resection. J Intensive Care Med. 2002;17(1):41-47. [Google Scholar]
- 52.Giles KA, Hamdan AD, Pomposelli FB, Wyers MC, Dahlberg SE, Schermerhorn ML. Population-based outcomes following endovascular and open repair of ruptured abdominal aortic aneurysms. J Endovasc Ther. 2009;16(5):554-564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Joseph B, Morton JM, Hernandez-Boussard T, Rubinfeld I, Faraj C, Velanovich V. Relationship between hospital volume, system clinical resources, and mortality in pancreatic resection. J Am Coll Surg. 2009;208(4):520-527. [DOI] [PubMed] [Google Scholar]
- 54.Knipp BS, Deeb GM, Prager RL, Williams CY, Upchurch GR, Jr, Patel HJ. A contemporary analysis of outcomes for operative repair of type A aortic dissection in the United States. Surgery. 2007;142(4):524-528. [DOI] [PubMed] [Google Scholar]
- 55.Kuo EY, Chang Y, Wright CD. Impact of hospital volume on clinical and economic outcomes for esophagectomy. Ann Thorac Surg. 2001;72(4):1118-1124. [DOI] [PubMed] [Google Scholar]
- 56.Macomber CW, Shaw JJ, Santry H, et al. Centre volume and resource consumption in liver transplantation. HPB (Oxford). 2012;14(8):554-559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gabler NB, Ratcliffe SJ, Wagner J, et al. Mortality among patients admitted to strained intensive care units. Am J Respir Crit Care Med. 2013;188(7):800-806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wunsch H, Angus DC, Harrison DA, et al. Variation in critical care services across North America and Western Europe. Crit Care Med. 2008;36(10):2787-2793. [DOI] [PubMed] [Google Scholar]
- 59.Wunsch H, Linde-Zwirble WT, Harrison DA, Barnato AE, Rowan KM, Angus DC. Use of intensive care services during terminal hospitalizations in England and the United States. Am J Respir Crit Care Med. 2009;180(9):875-880. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Supplement