Lung cancer screening using low-dose computed tomography is recommended for high-risk individuals by professional associations including the US Preventive Services Task Force (USPSTF).1 The implications of the USPSTF screening criteria were investigated in a retrospective study of a well-defined population to demonstrate trends in the proportion of lung cancer patients meeting the criteria over 28 years.
METHODS
The cohort contained all Olmsted County (Minnesota) residents aged over 20 years from 1984 through 2011, 2 comprising approximately 140,000 people, of whom 83% are non-Hispanic white and socioeconomically similar to the Mid-Western US population.2 All pathology-confirmed incident cases of primary lung cancer in the cohort were identified using the Rochester Epidemiology Project database, which has maintained a comprehensive medical records linkage system for over 60 years;3 based on using the Hospital Adaptation of International Classification of Diseases Adaptation (HICDA) and the International Statistical Classification of Diseases, ninth revision (ICD-9) codes.3,4 Patient characteristics were extracted with minimal missing data or loss to follow up.3 This study was approved by the institutional review boards with a waiver of informed consent due to no patient contact.
Trends in incidence rates of primary lung cancer were determined based on decennial census data adjusted for the age and sex distribution of the US population in 2000. Cases were grouped into 4 calendar-year intervals (7 years each) when assessing secular trends to minimize the annual rate fluctuations. Assuming a Poisson distribution, 95% confidence intervals (CIs) for incidence rates were calculated with generalized linear models using the Poisson error structure and a log link function.4,5
The proportion of cases meeting USPSTF screening criteria - asymptomatic adults aged 55 to 80 years with a 30 pack-year smoking history and currently smoking or having quit within the past 15 years1 - were identified. The Cochran-Armitage trend test was used for comparing proportions. Two-sided P <0.05 was considered statistically significant. Analyses were performed using SAS, v.9.3 (SAS Institute Inc.).
RESULTS
There were 1351 patients with incident primary lung cancer between 1984 and 2011. The mean (SD) age was 68.1 (11.3) years, with 54.9% male. The age- and sex-adjusted incidence rate decreased from 52.3 per 100,000 person-years in 1984–1990 to 44.1in 2005–2011 (P<0.001; Table). Trend analyses showed a decline in men but not women. Although the proportion of lung cancer patients who smoked more than 30 pack-years declined, the proportion of former smokers, especially those who quit smoking more than 15 years, increased.
Table.
Changing characteristics of Olmsted County Residents Diagnosed with Primary Lung Cancer, 1984–2011
| 1984–1990 (n=257) | 1991–1997 (n=301) | 1998–2004 (n=400) | 2005–2011 (n=393) | Total (n=1351) | P valuea | |
|---|---|---|---|---|---|---|
| Age-adjusted incidence rate(95%CI)b | ||||||
| Overall | 52.3 (45.8–58.7) | 50.8 (45.0–56.6) | 55.8 (50.3–61.3) | 44.1 (39.7–48.5) | 49.8 (47.1–52.5) | <0.001 |
| Men | 75.4 (62.9–87.9) | 69.8 (59.2–80.3) | 70.6 (61.0–80.2) | 49.4 (42.4–56.3) | 63.8 (59.1–68.5) | 0.007 |
| Women | 36.7 (29.7–43.7) | 37.0 (30.4–43.5) | 45.9 (39.3–52.6) | 40.1 (34.4–45.8) | 40.0 (36.8–43.2) | 0.14 |
| Age at diagnosis, No. (%) | ||||||
| <55 y | 31(12.1) | 49(16.3) | 44(11.0) | 53(13.5) | 177(13.1) | 0.85 |
| 55–80 y | 198(77.0) | 216(71.8) | 300(75.0) | 292(74.3) | 1006(74.5) | 0.75 |
| >80 y | 28(10.9) | 36(11.9) | 56(14.0) | 48(12.2) | 168(12.4) | 0.54 |
| Male sex, No. (%) | 150 (58.4) | 177 (58.8) | 216 (54.0) | 199 (50.6) | 742(54.9) | 0.02 |
| Cigarette smoking status at diagnosis, No. (%)c | ||||||
| Never smoker | 25 (9.7) | 26 (8.6) | 40 (10.0) | 34 (8.7) | 125(9.3) | 0.83 |
| Former smoker | 98 (38.1) | 126 (41.9) | 205 (51.2) | 190 (48.3) | 619(45.8) | 0.002 |
| Current smoker | 134 (52.2) | 149 (49.5) | 155 (38.8) | 169 (43.0) | 607(44.9) | 0.003 |
| Smoking amount of ever smokers, No. (%)d | (n=232) | (n=275) | (n=360) | (n=359) | (n=1226) | |
| <30 pack-years | 31 (13.4) | 44 (16.0) | 82 (22.8) | 82 (22.8) | 239(19.5) | <0.001 |
| ≥30 pack-years | 201 (86.6) | 231 (84.0) | 278 (77.2) | 277 (77.2) | 987(80.5) | <0.001 |
| Smoking cessation of former smokers, No. (%) | (n=98) | (n=126) | (n=205) | (n=190) | (n=619) | |
| <15 quit-years | 68 (69.4) | 92 (73.0) | 119 (58.0) | 103 (54.2) | 382(61.7) | <0.001 |
| ≥15 quit-years | 30 (30.6) | 34 (27.0) | 86 (42.0) | 87 (45.8) | 237(38.3) | <0.001 |
| Tumor Staging | ||||||
| NSCLC, No. (%) | (n=212) | (n=261) | (n=346) | (n=339) | (n=1158) | |
| I–II | 77(36.3) | 105(40.2) | 135(39.0) | 138(40.7) | 455(39.3) | 0.42 |
| III–IV | 135(63.7) | 156(59.8) | 211(61.0) | 201(59.3) | 703(60.7) | 0.42 |
| SCLC, No. (%) | (n=44) | (n=40) | (n=53) | (n=52) | (n=189) | |
| Limited | 21 (47.7) | 9 (22.5) | 19 (35.8) | 17 (32.7) | 66(34.9) | 0.34 |
| Extensive | 23 (52.3) | 31 (77.5) | 34 (64.2) | 35 (67.3) | 123(65.1) | 0.34 |
Abbreviation: NSCLC, non-small cell lung cancer; SCLC: small cell lung cancer.
Trend for incidence rates was tested by fitting a Poisson regression model where age, sex, and diagnosis year as the independent predictors; trend for proportions was tested by the Cochran-Armitage test.
Incidence is per 100,000 person-years.
Never smokers: smoking <100 cigarettes during lifetime; Former smokers: quit smoking ≥1 years before diagnosis.
Pack-year: packs smoked daily × years.
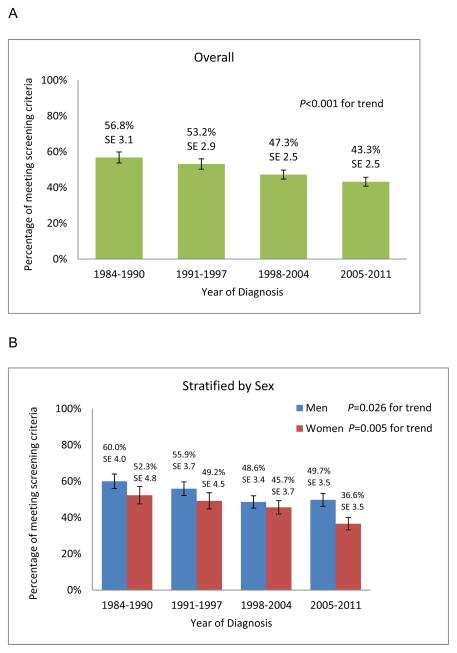
We observed a decline in the relative proportion of lung cancer patients meeting the USPSTF criteria overall, from 56.8% (95% CI, 50.8%–62.9%) in 1984–1990 to 43.43 % (95% CI, 38.4%–48.2%) in 2005–2011 (P<.001; Figure). The proportion of patients who would have been eligible under the USPSTF screening criteria decreased in women from 52.3% (95%CI, 42.9%–61.8%) to 36.6% (95%CI, 29.8%–43.4%; P=0.005) and in men from 60.0% (95%CI, 52.2%–67.8%) to 49.7% (95%CI, 42.8%–56.7%; P=0.026).
Figure.
Temporal Pattern of Coverage Proportion by USPSTF Screening Criteria in Olmsted County (Minnesota), 1984–2011
A. Overall B. Stratified by Sex
DISCUSSION
The proportion of lung cancer patients in Olmsted County meeting the USPSTF screening criteria decreased significantly between 1984 and 2011: 37% of female and 50% of male patients would have been eligible for screening in the most recent time interval. Our findings may reflect a temporal change in smoking patterns where the proportion of adults with a 30 pack-year smoking history and quit within 15 years declined. The secular trends of lung cancer incidence rates in Olmsted County are comparable to the US Surveillance, Epidemiology and End Results registry data,6 although they may not be generalizable to the entire US population. The decline in the proportion of patients meeting USPSTF “high risk” criteria for lung cancer screening indicates that an increasing number of lung cancer patients would not have been candidates for screening. Our data raises concerns that if the demonstrated trends continue, fewer patients who actually get lung cancer would be eligible for screening, which could ultimately decrease the disease-specific mortality. Therefore, more sensitive criteria may need to be amended, e.g. reevaluating those smoked <30 pack-year and quit >15 years.
Acknowledgments
Funding/Support: This study is supported by grants R03 CA77118, R01 CA80127 and R01 CA84354 from the National Institutes of Health; R01 AG034676 from the National Institute on Aging; and Mayo Clinic Foundation.
We thank Barbara A Abbott, Jennifer L St. Sauver, PhD, Walter A Rocca, MD(Department of Health Sciences Research, Mayo Clinic), and Barbara P Yawn, MD (Department of Research, Olmsted Medical Center), for their assistance in preparing the manuscript. The authors appreciate Khadija Idiris for her technical assistance with the manuscript. No compensation was received by any of these individuals.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Role of the Sponsor: The National Institutes of Health, National Institute on Aging, and Mayo Clinic Foundation had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author Contributions: Drs. Yang and Wang had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Yang, Wang, Midthun.
Acquisition, analysis, or interpretation of data: Yang, Wang, Wampfler.
Drafting of the manuscript: Wang, Midthun, Yang.
Critical manuscript revision for important intellectual content: Midthun, Yang, Wang.
Statistical analysis: Wang, Wampfler, Yang.
Obtained funding: Yang.
Administrative, technical, or material support: Wang, Wampfler, Zhang, Deng, Stoddard, Yang.
Study supervision: Yang.
References
- 1.Moyer VA U.S. Preventive Services Task Force. Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160(5):330–338. doi: 10.7326/M13-2771. [DOI] [PubMed] [Google Scholar]
- 2.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87(2):151–160. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCullagh P, Nelder JA. Generalized Linear Models. London: Chapman and Hall; 1983. [Google Scholar]
- 4.Bergstralh EJ, Offord KP, Chu CP, Beard CM, O’Fallon WM, Melton LJ., 3rd . Technical Report Series No. 49. Department of Health Science Research, Mayo Clinic; Rochester, Minnesota: Apr, 1992. Calculating Incidence, Prevalence, and Mortality Rates for Olmsted County, Minnesota: An Update. [Google Scholar]
- 5.Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64(1):9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]