Abstract
The Public Bodies (Joint Working) (Scotland) Act 2014 puts in place the framework for the Integration of health and social care in Scotland. Newly formed health and social care partnerships (HSCP), which will serve as the joint responsibility of NHS boards and local authorities, will work in partnership with the third sector, users, carers and other key stakeholders, including the independent sector. This paper details the underpinning features of the legislation which aims to put ‘personal’ outcomes at the centre, in order for everyone to be able to live longer and healthier lives at home or in a homely setting. Much activity is being undertaken in what is one of the single biggest changes to care services in Scotland.
Background and challenges
The challenge for all Western societies in how best to cope with ageing populations is at its most acute in Scotland where, over the next 10 years, there will be a 25% increase in those aged over 75 – the highest users of health and social care services. Although problems of frailty relate to ageing, in Scotland multi-morbidity is also seen at younger ages in areas of deprivation, and health inequalities remain a key factor in Scotland's public health record. A raft of measures including the Scottish Patient Safety Programme and a ban on smoking in public places have improved health and care, but it is increasingly recognised that a wholesystem approach is now required to deliver care for the future. In particular, barriers at the current interfaces between primary and secondary care and health and social care need to be re-thought and re-modelled. The pressure of austerity measures since 2009/10 as well as a fall in Scottish public expenditure in real terms, add impetus to the need for efficient and sustainable health and care services.1
Development of policy
The Scottish Parliament, created by the 1998 Scotland Act, has powers to make laws across a range of policy areas. Although some issues – mainly with a UK-wide or international impact (reserved matters) – remain the responsibility of the UK Parliament, health and social care are devolved matters and policy and legislation relating to these are the responsibility of the Scottish government. In response to the key challenges of changing demographics, our public health record and severe financial pressures, the Scottish government, Confederation of Scottish Local Authorities (COSLA) and NHS established, in 2009 the ‘Reshaping Care for Older People’ programme with the aim to engage all interested parties in reshaping care and support services in a sustainable manner.2 A further response, the Christie Commission on the Future of Public Services, followed in 2010.3,4 The Christie Commission noted that a radical change in the design and delivery of public services was necessary and proposed four pillars of reform: a ‘person-centred approach’ empowering individuals and communities; ‘partnership’ working and integrating services to provide seamless care; ‘prevention’ to minimise negative outcomes; and finally, services whose ‘performance’ and effectiveness are measured and monitored. These themes were further developed in the Scottish government's 2020 Vision (Box 1).
Box 1. Our 20:20 Vision.
Our vision is that by 2020 everyone is able to live longer healthier lives at home, or in a homely setting.
We will have a healthcare system where we have integrated health and social care.
Integration of health and social care
Moving these ideas forward, the Scottish government's manifesto pledge of 2011 stated it would deliver a ‘single integrated system of health and social care across Scotland’. In December 2011, the Scottish Health Secretary set out the Scottish government's plan to integrate adult health and social care. Under the new system, community health partnerships (CHPs) will be replaced by health and social care partnerships (HSCP), which will be the joint responsibility of the NHS boards and the local authority (joint integration authorities).
Primary legislation, the Public Bodies (Joint Working) (Scotland) Act 2014,5 received Royal Assent in April 2014. This puts in place the framework for integrating health and social care in Scotland. Following consultation, broader statutory guidance is being developed to further support implementation of service.6
Health and social care integration requires health boards and local authorities to work in partnership with the third sector, users, carers and other key stakeholders, including the independent sector. Currently (statutory) health care is delivered by 14 territorial NHS health boards and social work and social care are provided by 32 local authorities; 31 shadow health and social care partnerships have been established prior to 1 April 2015 implementation.4–6
The Public Bodies Act describes two models of integrating health and social care:
Option 1: Body Corporate. The health board and local authority delegate the responsibility for planning and resourcing service provision for adult health and social care services to an integration joint board.
Option 2: Lead Agency. The health board or the local authority takes the lead responsibility for planning, resourcing and delivering integrated adult health and social care services.
The chosen model, best suited for local need, is agreed by the health board and local authorities. Information suggests that most health boards and local authorities favour Option 1 – the body corporate model.
Distinctive features of the Scottish Integration models
Key features of the Public Body (Joint Working) (Scotland) Act 2014 are outlined in Box 2.
Box 2. Key features: Public Bodies (Joint Working) (Scotland) Act 2014.
Principles for integrated health and social care.
Nationally agreed outcomes for health and well-being.
Integrated governance arrangements for health and social care: delegation to a body corporate or lead agency.
Integrated budgets for health and social care.
Integrated oversight of delivery.
Strategic planning.
Locality planning.
Outcomes
A distinctive feature of the legislation is the importance of ‘personal outcomes’ and ‘outcomes-focused approaches’. National health and well-being outcomes (Box 3) will form a key part of the monitoring of performance of the joint integration boards. There is a recognition in the primary legislation that different models will be put in place across Scotland, and therefore its focus will be on impact rather than input. There is ongoing work on the measurables associated with the outcomes.
Box 3. The National Health and Wellbeing Outcomes (Public Bodies (Joint Working) (Scotland) Act 2014).
People are able to look after and improve their own health and well-being and live in good health for longer.
People, including those with disabilities or long-term conditions or who are frail, are able to live, as far as reasonably practicable, independently and at home or in a homely setting in their community.
People who use health and social care services have positive experiences of those services, and have their dignity respected.
Health and social care services are centred on helping to maintain or improve the quality of life of people who use those services.
Health and social care services contribute to reducing health inequalities.
People who provide unpaid care are supported to look after their own health and well-being, including to reduce any negative impact of their caring role on their own health and well-being.
People using health and social care services are safe from harm.
People who work in health and social care services feel engaged with the work they do and are supported to continuously improve the information, support, care and treatment they provide.
Resources are used effectively and efficiently in the provision of health and social care services.
Localities
Localities, which are natural communities based on geography, while service provision and general practitioner (GP) surgeries are ‘the engine room of integration’. Each HSCP will comprise at least two localities. The importance of localities in improving health and, in particular, addressing the widening gap in health inequalities is emphasised in the Marmot Review ‘Effective local delivery requires effective participatory decision making at local levels. This can only happen by empowering individuals and local communities’.7
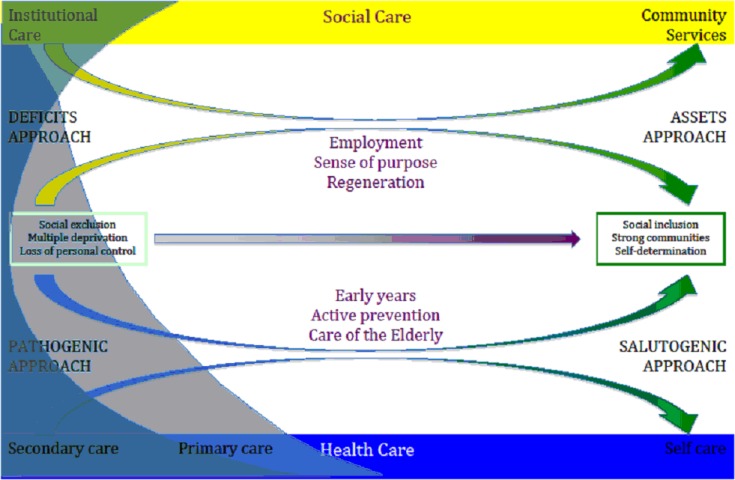
In Scotland, an assets-based approach will harness the collective resources that individuals and communities have at their disposal that protect against negative health outcomes and promote positive health. This approach is underpinned by Antonovsky's theory of salutogenesis, a perspective on how health is viewed and how the use of personal resources (assets)8 either from within the individual or the environment maintains a healthy status. We therefore aim to shift health and care from correcting deficits and illness to promoting individual and community well-being (Figure 1).
Figure 1.
© druce&efardon
In order to ensure that localities are promoted, work is currently being undertaken to promote locality arrangements within health and social care partnerships to ensure joint strategic commissioning is coproduced based upon needs assessment. Robust shared data with the local population along with health and social care services, including the third and independent sectors will ensure localities’ strengths and assets are exploited.
The next steps
Workforce development and education funding has been made available to the shadow health and social care partnerships to support integration. National organisations including NHS Education for Scotland (NES) and the Scottish Social Services Council (SSSC) have a programme of workforce development and education to support integration.
Each outcome has a programme of activity to support the health and social care workforce, which includes the development of an e-learning resource to support joint strategic commissioning. Working alongside and supporting workforce developments are learning and development leads from the health board and local authorities. In addition, a resources toolkit and a development programme for integrated joint boards are also in place.
NES and SSSC have invited health and social care partnerships to engage in an appreciative inquiry process. Broadly, the process will aim to identify:
what is working well to support workforce development;
some of the challenges or gaps likely to be encountered;
actions that can be taken forward locally to strengthen what's working well and address the challenges?
Through appreciative inquiry (AI), it is anticipated that the HSCP will be able to create strategic change through collective analysis, problem solving and decision-making – fundamentally creating change to the system of health and social care delivery to a locality through collaborative strengths based approach.
A collaborative partnership between RCGP (Scotland), SSSC and NES – Leadership for Integration – proposes paired learning with primary care professionals, middle managers and chief officers in social work. This programme will also include third sector representatives who work in relevant integration roles. The aim is for collaborative leadership skills and capability to operate effectively at locality level and to influence joint integrated boards. Through collaborative leadership by building trusting partnerships, it is anticipated that primary care professionals will create values, outcomes, a shared purpose, and a vision for localities by working in partnership to find solutions to challenges that face the implementation of health and social care that ultimately lead to better outcomes for individuals, families and communities. Such an approach has many benefits, including primary care professionals gaining better understanding of differing perspectives of health and social care services; their own and others’ unique contribution; utilisation of a range of robust improvement models; and tools that could be utilised to support leadership roles and to strengthen leadership roles through collaboration.
Conclusion
The Public Bodies (Joint Working) (Scotland) Act 2014 and its implementation are at a very early stage. Much activity is being undertaken in what is one of the single biggest changes to care services in Scotland. The Christie Commission report called for major changes in the way public services are delivered, and for a radical new collaborative culture throughout. Our task is now to work alongside our communities and organisations to make this vision happen.
Contributor Information
David Bruce, Director of Postgraduate General Practice Education, NHS Education for Scotland, Dundee, UK.
Bob Parry, Associate Director, Health and Social Care Integration, NHS Education for Scotland, Edinburgh, UK.
FURTHER READING
- Ham C, Walsh N. (2013) Making integrated care happen at scale and pace. Kings Fund: London: http://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/making-integrated-care-happenkingsfund-mar13.pdf [Google Scholar]
- Ham C, Heenan D, Longley M, Steel DR. (2013) Integrated care in Northern Ireland, Scotland and Wales: Lessons for England. King's Fund: London: http://www.kingsfund.org.uk/publications/integrated-carenorthern-ireland-scotland-and-wales [Google Scholar]
REFERENCES
- 1.Beveridge C. et al. (2010) Independent Budget Review – The Reports of Scotland's Independent Budget Review Panel.
- 2.Scottish Government (2009) Reshaping Care for Older People: A Programme for Change 2011–2021.
- 3.Scottish Government (2011) Commission on the Future Delivery of Public Services Scotland Act (1998).
- 4.Christie C. (2011) Commission on the future delivery of public services, Edinburgh: Scottish Government. [Google Scholar]
- 5.Public Bodies (Joint Working) (Scotland) Act 2014. http://www.legislation.gov.uk/asp/2014/9/pdfs/asp_20140009_en.pdf
- 6.http://www.scotland.gov.uk/Topics/Health/Policy/Adult-Health-SocialCare-Integration (accessed 4th May 2015).
- 7.The Marmot Review – Fair Society, Healthy Lives. http://www.instituteofhealthequity.org/projects/fair-society-healthy-lives-the-marmot-review/fair-society-healthy-lives-full-report
- 8.Asset based approaches for health improvement: redressing the balance. Mclean. J. Glasgow Centre for Population Health http://www.gcph.co.uk/assets/0000/2627/GCPH_Briefing_Paper_CS9web.pdf