Supplemental Digital Content is available in the text.
Abstract
Background:
Ideally, breast reconstruction is performed at the time of mastectomy in a single stage with minimal scarring. However, postoperative complications with direct-to-implant subpectoral reconstruction remain significant. These include asymmetry, flap necrosis, animation deformity, and discomfort. We report on a series of patients who have undergone immediate single-stage prepectoral, implant-based breast reconstruction with a smooth, adjustable saline implant covered with mesh/acellular dermal matrix for support using a vertical mastectomy incision. This technique, when combined with an adjustable implant, addresses the complications related to subpectoral implant placement of traditional expanders. Our follow-up time, 4.6 years (55 months), shows a low risk of implant loss and elimination of animation deformity while also providing patients with a safe and aesthetically pleasing result.
Methods:
All patients who underwent immediate implant-based prepectoral breast reconstruction using a vertical mastectomy incision as a single-staged procedure were included. Charts were reviewed retrospectively. Adjustable smooth round saline implants and mesh/acellular dermal matrix were used for fixation in all cases.
Results:
Thirty-one patients (62 breasts) underwent single-staged implant-based prepectoral breast reconstruction using a vertical mastectomy incision. Postoperative complications occurred in 9 patients, 6 of which were resolved with postoperative intervention while only 2 cases resulted in implant loss.
Conclusions:
There can be significant morbidity associated with traditional subpectoral implant-based breast reconstruction. As an alternative, the results of this study show that an immediate single-stage prepectoral breast reconstruction with a smooth saline adjustable implant, using a vertical incision, in conjunction with mesh/matrix support can be performed with excellent aesthetic outcomes and minimal complications.
Reconstructive breast procedures continue to be a common operation for plastic surgeons. In 2013, 95,589 breast reconstruction procedures were performed, with the large majority of those being implant-based.1 Reconstructive results have continued to improve as we have seen an evolution in mastectomy techniques from radical, to modified radical, to skin-sparing and now to nipple-sparing techniques. However, currently practiced techniques of implant-based reconstruction are far from perfect as, interestingly, in the same year, 18,223 cases of implant removal in reconstructive patients were performed.1
The most common method of breast reconstruction involves the placement of an integral injection port tissue expander beneath the muscle, tissue expansion, and subsequent replacement with a silicone gel implant. Expanders are traditionally placed in a submuscular pocket due to concerns with thin and poorly vascularized skin flaps. As the inferior portion of the pectoralis muscle is thinner and unpredictable, it is preferable to have a horizontal incision overlying the muscle so that the expander can be protected from the incision by the thicker upper muscle. Although excellent results can be obtained, submuscular placement often results in animation deformities, chronic pain, and/or discomfort.2
With the evolution of mastectomies, from modified radical to nipple sparing, the quality of the remaining skin flaps has also improved greatly. With less concern about skin flap vascularity, it is now possible to place a remote injection port expander above the muscle in selected patients, with total freedom of the mastectomy incision placement. In this series, we present 31 patients who have undergone immediate single-stage breast reconstruction with a definitive adjustable saline implant-based prepectoral and complete coverage with mesh/acellular dermal matrix (ADM) using a vertical mastectomy incision. Either Vicryl (Ethicon, Somerville, N.J.) or FlexHD (Musculoskeletal Transplant Foundation, Edison, N.J.) Pliable mesh was used for fixation in all cases. The impetus to perform prepectoral breast reconstruction came from seeing reconstructive and cosmetic patients, with implants in the subpectoral position, who repeatedly complained about animation deformity and discomfort. We give, here, a preliminary report on 31 cases with a mean follow-up time of 2 years resulting in minimal implant loss and no animation deformity, showing excellent results.
METHODS
A retrospective review was performed on all patients who had undergone an immediate implant-based prepectoral breast reconstruction as a single-staged procedure. Vertical mastectomy incisions were used in all patients. All patients had adjustable smooth round saline implants placed and complete implant coverage with either Vicryl or FlexHD Pliable mesh (ADM) used for fixation. All patients meeting these criteria were included. There were no exclusion criteria. The cases were all performed by a single surgeon in a private practice setting. Informed verbal and written consent were given by all of the patients. The Declaration of Helsinki principles were strictly followed. Aggressive clinical follow-up was performed in all cases. Follow-up was done daily for the first 3 days and then twice weekly for the first 2 weeks. All charts were reviewed in a retrospective fashion. Data collected included the patient’s age, the diagnosis, the type of mesh/matrix used, any history of radiation, postoperative complications, need for postoperative interventions, implant loss, conversion to silicone gel implants, and follow-up time (Table 1) (See Video 1, Supplemental Digital Content 1, which demonstrates the operative technique used for prepectoral breast implant placement with complete ADM coverage using a vertical incision. This video is available in the “Related Videos” section of the full-text article at http://www.PRSGO.com or available at http://links.lww.com/PRSGO/A98).
Table 1.
Collection of Patient Data
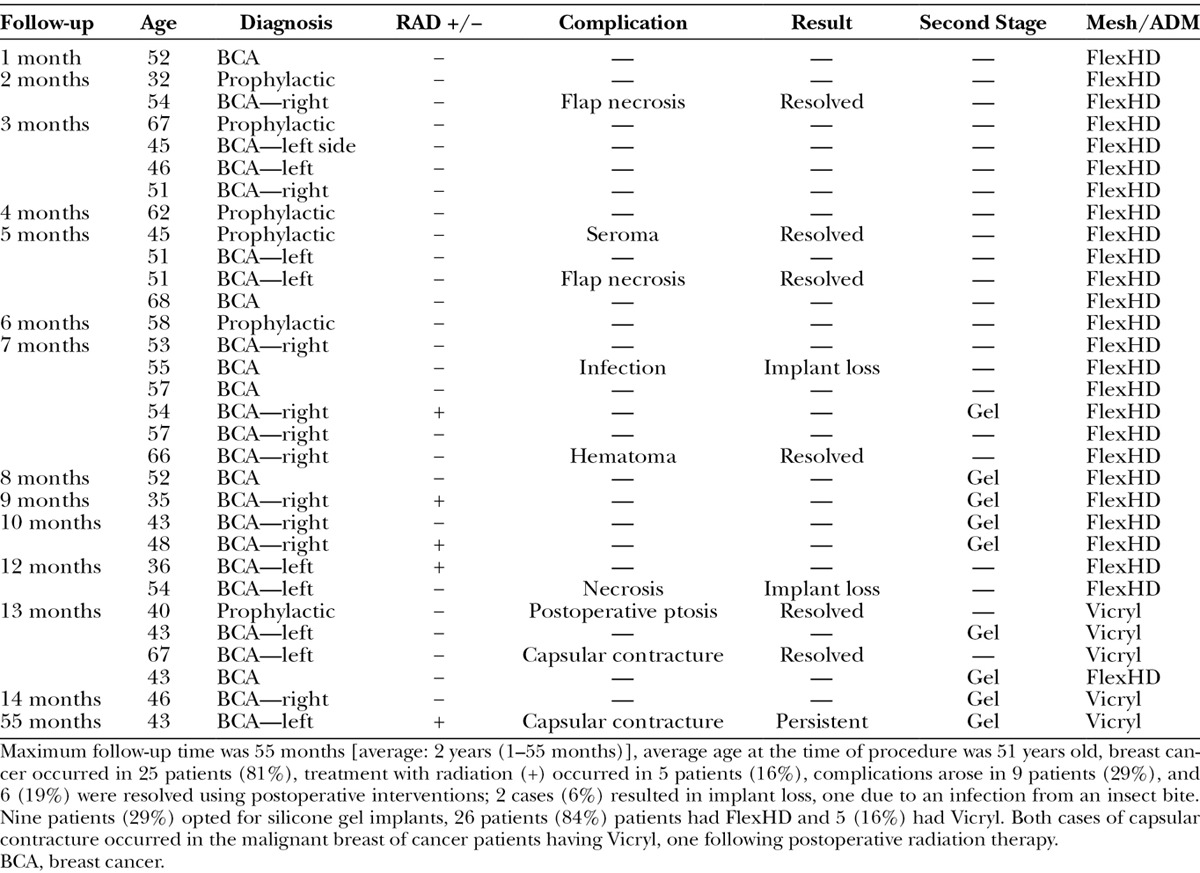
Fig. 1.

A, Intraoperative photograph immediately following bilateral vertical mastectomy. B, Following insertion of dermal graft and de-epithelialization of lateral flap and temporary intraoperative expander within subdermal pocket. C, Following prepectoral placement of adjustable spectrum implant into the subdermal pocket partially filled and final skin closure.
Video 1.

See video, Supplemental Digital Content 1, which demonstrates the operative technique used for prepectoral breast implant placement with complete ADM coverage using a vertical incision. This video is available in the “Related Videos” section of the full-text article at http://www.PRSGO.com or available at http://links.lww.com/PRSGO/A98.
The mastectomy skin incision is planned preoperatively in conjunction with the general surgeon. The inframammary fold is outlined. A determination is made as to whether or not the nipple can be preserved. If the nipple is going to be resected, the areolar skin can often be retained. Where the nipple is to be removed, a vertical incision is planned encompassing the nipple and extending to the inframammary fold. If the nipple is to be retained, a vertical incision is planned from the inferior edge of the areola to the inframammary fold. In the case of a large breast requiring skin reduction, the skin incisions are outlined together with the amount of lateral reduction required. The vertical incision can be tilted medially or laterally depending on each specific condition.
At the completion of the mastectomy, the patient is re-prepared and draped. The pocket is irrigated with an antibiotic solution. The vascularity of the flaps is evaluated, and debridement is performed where necessary. The lateral skin flap is anchored to the serratus and pectoralis muscle by advancing the flap medially. A temporary inflatable sizer (Mentor Corp., Goleta, Calif.) is placed in the pocket to assess the position and shape of the prepectoral pocket. The pocket is adjusted where necessary. A sheet of mesh/matrix is then selected. Products used in this series consisted of either Vicryl or FlexHD Pliable mesh. We now prefer using FlexHD Pliable. A 16 × 16 cm piece is trimmed to the appropriate shape and sutured to the superior medial and lateral edges of the pectoralis major muscle. The inferior edge is sutured to the fascia at the level of the inframammary fold (Fig. 1).
Two drains are inserted through long subcutaneous tunnels and sutured to the skin. The pocket is again irrigated with an antibiotic solution to further minimize the risk of infection. Gloves are changed and the adjustable smooth round saline implant (Spectrum, Mentor Corp., Goleta, Calif.) is sterilely prepared. Air is evacuated from the implant, and it is then inserted in to the newly created subacellular dermal pocket (Fig. 2A). The implant may be left virtually empty if there is concern regarding the circulation of blood supply to the skin flaps. If the circulation is satisfactory, saline may be added to a volume that will not result in undue tension on the skin flaps, using a closed filling system (Aseptic Transfer System, Mentor) (Fig. 2B). The filling tube is then shortened and attached to the injection dome. A subcutaneous pocket is dissected inferolaterally, and the injection dome is secured in this pocket with 2 absorbable sutures.
Fig. 2.
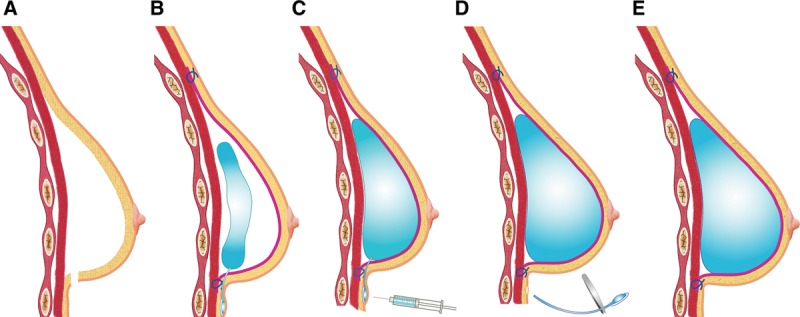
Illustration (A) following mastectomy, pocket is empty. B, The ADM (shown in magenta) is sutured to the periphery of the mastectomy pocket and the underfilled adjustable implant is placed beneath the ADM in the prepectoral position. C, The implant is filled postoperatively using the remote injection port. D, After 5 or 6 months, the injection port can be removed using a local anesthetic. E, Filled implant.
At this stage, the amount of lateral flap de- epithelialization is determined. Saline is injected into the skin to facilitate de-epithelialization. The de- epithelialized flap is advanced beneath the medial flap and sutured into position (Fig. 3). The skin edges are then approximated in 2 layers. Sterile dressings are applied.
Fig. 3.
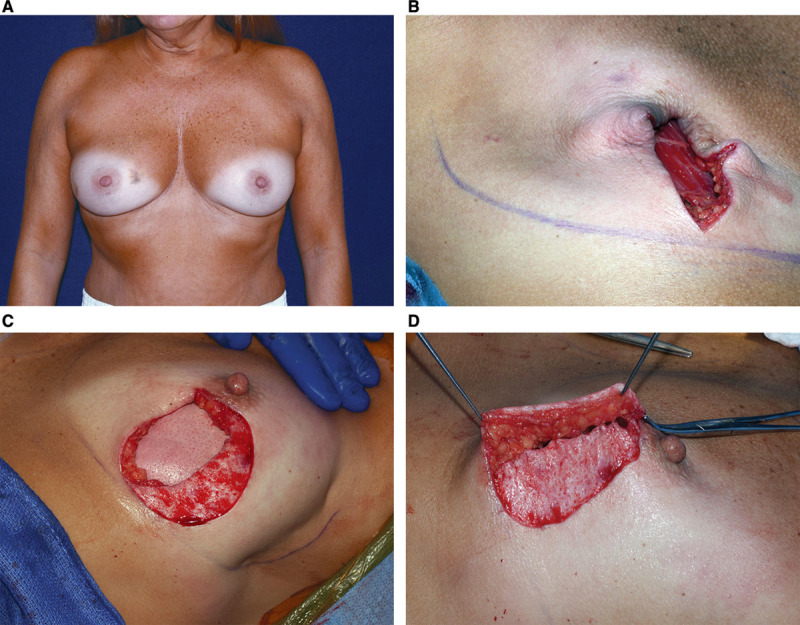
A, Preoperative view of a 42-year-old patient with carcinoma of the right breast. B, Intraoperative view after right areolar sparing mastectomy with a vertical incision. C, FlexHD sutured to the periphery of the mastectomy pocket. Adjustable implant placed in the prepectoral position beneath the ADM, and the medial edge of lateral flap de-epithelialized. D, Dermal flap advanced beneath the medial flap.
The patient is evaluated the following day. Dressings are removed with the patient in the upright position. Circulation and implant position are assessed. Filling of the adjustable implant is usually started within a few days following surgery (Fig. 2C). Under sterile conditions, a 23G butterfly needle (Kawasumi, Tokyo, Japan) is inserted into the injection dome adding 50–100 mL of saline at a time (Fig. 4).
Fig. 4.
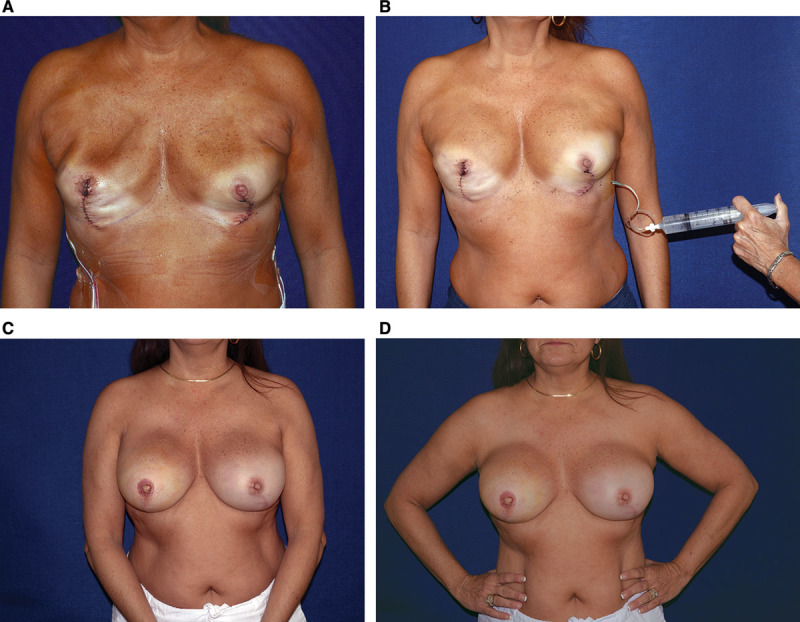
A, Early postoperative result following right areolar sparing mastectomy and left nipple-sparing mastectomy with immediate bilateral prepectoral implant placement. B, Saline added to adjustable implant. C, Postoperative anterior view of final result with definitive adjustable saline implants. D, No postoperative animation deformity upon muscle contraction.
If the patient is satisfied with the result after 5 or 6 months, the injection port can be removed using a local anesthetic (Figs. 2D, E). Thin skin flaps can be augmented with fat injections and/or the patient can be converted to a silicone gel implant if desired (Figs. 5 and 6).
Fig. 5.
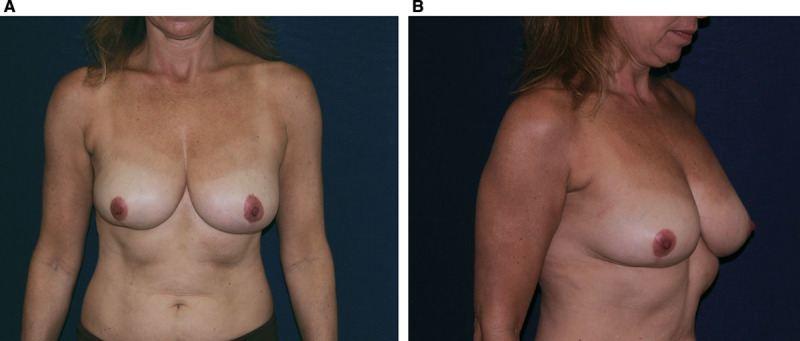
Preoperative anterior (A) and side (B) views of a 52-year-old patient with ductal carcinoma in situ of the right breast.
Fig. 6.

A, Anterior view of final result following replacement of spectrum adjustable implant with silicone gel implant. B, Postoperative side view. C, No postoperative animation deformity upon muscle contraction.
RESULTS
A series of 31 patients (62 breasts) who underwent single-stage breast reconstruction with prepectoral smooth, adjustable saline implants using a vertical mastectomy incision over a 4.6-year period are presented. The average age of the patients was 51 years at the time of the operation. Mean follow-up time was 2 years (1–55 months). Five patients (16%) had synthetic mesh (Vicryl) support. Twenty-six patients (84%) had a biologic ADM (FlexHD Pliable) support. Seven patients (23%) had a need for postoperative interventions, 6 (19%) of which resolved. Postoperative complications occurred in 9 patients all together and consisted of 1 case of seroma and 1 case of hematoma requiring operative drainage, 2 cases of flap necrosis requiring debridement, 1 patient with bilateral ptosis requiring bilateral tightening for elevation of the breasts, 2 cases with capsular contracture (one following postoperative radiation), and 2 cases of implant loss—one due to infection caused by an insect bite and another due to a necrotic wound. Interestingly, both cases of capsular contracture occurred in the malignant breast of cancer patients having Vicryl, one following postoperative radiation. Both cases of implant loss occurred in patients in the FlexHD Pliable group. Five patients had deep radiation therapy, none of which experienced implant loss. Fat grafting was done in 4 patients, and 29% (9) of the patients opted for second-stage reconstruction having their implants exchanged for silicone gel implants.
Thus, it is anticipated that with the adjustable gel implant (Mentor, currently only available outside the United States), the percentage of single-stage reconstructions will be higher with this technique.
DISCUSSION
The majority of breast reconstructions performed today are done as a two-staged procedure where an expander is placed in the submuscular position followed by exchange for an implant several months later after tissue expansion. Sometimes, in the appropriate patients, a single-stage reconstruction can be performed where an implant is placed in the submuscular position at the time of the mastectomy.3 Although good cosmetic results can be achieved with these forms of reconstruction, the submuscular placement of the prosthetic device in both of these methods of breast reconstruction can result in problems such as increased pain and/or animation deformity or asymmetry that may necessitate a further procedure to place the implant above the muscle.4
In our series, we propose an alternative to the submuscular placement of prosthetic devices in immediate breast reconstruction patients. We endorse placing the implant prepectoral, using a vertical mastectomy incision, a dermal flap for coverage, and a definitive adjustable smooth saline implant with mesh/ADM fixation in this patient series. From our viewpoint, this technique has been shown to achieve excellent results in this series with low complication rate and implant loss although it seems to eliminate some of the pitfalls seen in submuscular prosthetic placement.
This technique can be performed in a high percentage of patients, including patients with ptotic and/or large breasts. Implant-based breast reconstruction results are largely dependent on the status of the tissues following the mastectomy. Therefore, the general surgeon’s comprehension of the reconstructive techniques and understanding of complications due to thin flaps are essential to obtain the desired results. Preoperative planning and incision marking should be performed in conjunction with the general surgeon.5 Nipple- and skin-sparing mastectomies have been shown to be oncologically safe and allow for much more flexibility in implant-based breast reconstruction.6,7
In our experience, to correct ptosis in skin reducing mastectomy, less skin needs to be resected compared with standard mastopexy or reduction mammoplasty. Exact skin tailoring along a wise pattern excision results in unacceptably high complication rates that may be easily avoided by adopting a versatile and a conservative vertical excision pattern.8 There are numerous advantages to a vertical incision over a horizontal incision.9 From the surgical excision perspective, the vertical incision allows for ease of access for the mastectomy, with comparable visualization to other incision patterns. There is less interference with the blood supply to the flaps as the incision runs parallel to the direction of blood flow, running in the watershed area of the lateral and medial blood supply to the breast. We also feel that this incision leads to a better cosmetic result. The scar resembles that of a breast lift procedure, resulting in a more natural projection of the reconstructed breast with improved nipple position. The nipple does not tend to drift laterally. Horizontal incisions tend to flatten the breast, particularly if tissue is excised or if scar contracture occurs. Should postoperative debridement of the flaps be necessary, further flattening and distortion occurs with horizontal incisions and lateral shift of the nipple is also common. By contrast, debridement of a vertical incision causes elevation of the breast without lateral distortion. This technique has applicability to small breasts and large ptotic breasts (particularly where reduction and/or elevation is necessary) (Figs. 7A–C). Large ptotic breasts require some degree of skin envelope reduction. With the vertical scar technique, rather than excising the skin, the delineated area is de-epithelialized and advanced medially. This dermal flap forms a dermal barrier to the implant and also adds soft-tissue support.3,4,10,11 Further tightening of the vertical incision can also be performed postoperatively without additional scarring if needed. Further elevation can also be achieved easily (Fig. 8).
Fig. 7.
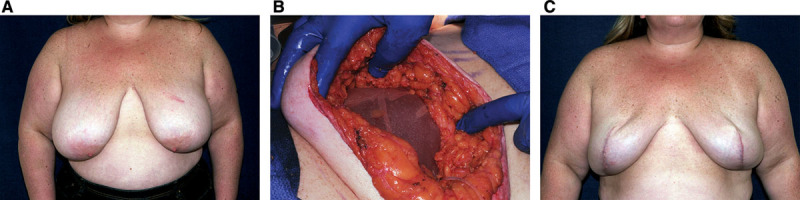
A, Preoperative view of a 40-year-old BRCA-positive patient. B, Adjustable implant placed beneath mesh support. C, Postoperative result at 6 months.
Fig. 8.

A, Adjustable saline implants replaced with smooth round silicone gel implants medial edge of lateral flap further advanced to elevate breasts. Anterior (B) and side (C) views of final postoperative result.
Several benefits seem to be obtained by placing the implant in the prepectoral position. First, prepectoral implant placement eliminates 100% of animation deformities in this series (Fig. 9). Second, as the muscle is not detached and the implant is not placed beneath the muscle, there seems to be less postoperative pain and a faster recovery in our experience. Having cared for many patients following mastectomies without reconstruction, the pain from breast reconstruction seems to arise not from the mastectomy incision but rather due to the typical submuscular dissection and location of the tissue expander. In our experience, subjectively, those patients with breast reconstruction certainly seem to have more pain than the patients who only underwent mastectomies.
Fig. 9.

A, Preoperative view of a 47-year-old patient with carcinoma of the left breast. B, Postoperative view s/p bilateral breast reconstruction with adjustable implants in the prepectoral position following nipple reconstruction. C, No postoperative animation deformity upon muscle contraction.
The incidence of capsular contractures and saline rippling is always a concern, whether submuscular or prepectoral sub-ADM placement. We correct rippling in this series by replacing the saline implant with silicone gel implants and/or with fat injections. From an oncologic perspective, the supramuscular technique is advantageous because no additional tissue planes are opened, decreasing the area of potential surgical seeding of cancerous cells. Pitcher et al12 reported a case in which a patient who had underwent subpectoral implant-based breast reconstruction was found to have an isolated breast cancer recurrence in the subpectoral space 5 years later during a reconstruction revision surgery. ADM or mesh coverage of the implant together with a dermal overlap incision eliminates the need for muscle coverage13 as the entire anterior surface of the implant is covered with ADM. Prepectoral placement of the implant also simulates the natural position of the removed breast tissue and leads to a more natural feel.
Less pressure on the skin flaps is made possible with the use of an adjustable flat expander/implant with a remote port (Spectrum). The implant is placed underfilled, causing no increased pressure to the flaps during the immediate recovery phase. The expander can later be adjusted once viability of the flaps is assured. Optimal results have been shown to be possible with adjustable implants in a single-stage reconstruction.14
CONCLUSIONS
In summary, it seems that an immediate single-stage prepectoral breast reconstruction with a smooth saline adjustable implant, using a vertical incision, in conjunction with mesh/matrix support can be performed with excellent aesthetic outcomes and minimal complications/implant loss. This technique eliminates some of the morbidity associated with the traditional subpectoral-based implant breast reconstructions, such as pain, animation deformity, and asymmetry. Single-stage breast reconstruction will become more important as there continues to be increasing financial strains on our healthcare system. This is a preliminary study with very low short-term complications and total elimination of animation deformity, therefore warrants early report. Longer follow-up will be needed to ensure the longevity of the aesthetic outcome and to assess any potential long-term morbidity associated with this method of breast reconstruction.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
Disclosure: Hilton Becker, MD, is a paid consultant of Mentor Worldwide LLC, receives royalties from Mentor Worldwide LLC, and is a consultant for Novus Scientific and Greer Medical. Neither of the other authors has any financial disclosures. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.American Society of Plastic Surgeons. 2013 Breast Reconstruction Statistics. Available at: http://www.plasticsurgery.org/news/plastic-surgery-statistics/2013.html. Accessed July 28, 2014.
- 2.Spear SL, Schwartz J, Dayan JH, et al. Outcome assessment of breast distortion following submuscular breast augmentation. Aesthetic Plast Surg. 2009;33:44–48. doi: 10.1007/s00266-008-9275-y. [DOI] [PubMed] [Google Scholar]
- 3.Davila AA, Mioton LM, Chow G, et al. Immediate two-stage tissue expander breast reconstruction compared with one-stage permanent implant breast reconstruction: a multi-institutional comparison of short-term complications. J Plast Surg Hand Surg. 2013;47:344–349. doi: 10.3109/2000656X.2013.767202. [DOI] [PubMed] [Google Scholar]
- 4.Lesavoy MA, Trussler AP, Dickinson BP. Difficulties with subpectoral augmentation mammaplasty and its correction: the role of subglandular site change in revision aesthetic breast surgery. Plast Reconstr Surg. 2010;125:363–371. doi: 10.1097/PRS.0b013e3181c2a4b0. [DOI] [PubMed] [Google Scholar]
- 5.Toth BA, Lappert P. Modified skin incisions for mastectomy: the need for plastic surgical input in preoperative planning. Plast Reconstr Surg. 1991;87:1048–1053. [PubMed] [Google Scholar]
- 6.Mallon P, Feron JG, Couturaud B, et al. The role of nipple-sparing mastectomy in breast cancer: a comprehensive review of the literature. Plast Reconstr Surg. 2013;131:969–984. doi: 10.1097/PRS.0b013e3182865a3c. [DOI] [PubMed] [Google Scholar]
- 7.Maxwell GP, Storm-Dickerson T, Whitworth P, et al. Advances in nipple-sparing mastectomy: oncological safety and incision selection. Aesthet Surg J. 2011;31:310–319. doi: 10.1177/1090820X11398111. [DOI] [PubMed] [Google Scholar]
- 8.Di Candia M, Lie KH, Forouhi P, et al. Experience with the Wise mammaplasty skin resection pattern in skin-sparing mastectomy and immediate breast reconstruction for large breast volumes. Int J Surg. 2011;9:41–45. doi: 10.1016/j.ijsu.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 9.Hunter JE, Malata CM. Refinements of the LeJour vertical mammaplasty skin pattern for skin-sparing mastectomy and immediate breast reconstruction. J Plast Reconstr Aesthet Surg. 2007;60:471–481. doi: 10.1016/j.bjps.2006.04.028. [DOI] [PubMed] [Google Scholar]
- 10.Bayram Y, Kulahci Y, Irgil C, et al. Skin-reducing subcutaneous mastectomy using a dermal barrier flap and immediate breast reconstruction with an implant: a new surgical design for reconstruction of early-stage breast cancer. Aesthetic Plast Surg. 2010;34:71–77. doi: 10.1007/s00266-009-9452-7. [DOI] [PubMed] [Google Scholar]
- 11.Mestak J, Sukop A, Mestak O. Use of deepithelialized flap in mammoplasties: simple method with excellent results. Aesthetic Plast Surg. 2011;35:1106–1111. doi: 10.1007/s00266-011-9745-5. [DOI] [PubMed] [Google Scholar]
- 12.Pitcher AA, Chao JW, Varma S, et al. Recurrent breast cancer in the subpectoral space after implant reconstruction. J Surg Oncol. 2014;109:431–433. doi: 10.1002/jso.23505. [DOI] [PubMed] [Google Scholar]
- 13.Becker H, Lind JG., II The use of synthetic mesh in reconstructive, revision, and cosmetic breast surgery. Aesthetic Plast Surg. 2013;37:914–921. doi: 10.1007/s00266-013-0171-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eskenazi LB. New options for immediate reconstruction: achieving optimal results with adjustable implants in a single stage. Plast Reconstr Surg. 2007;119:28–37. doi: 10.1097/01.prs.0000244744.27540.cc. [DOI] [PubMed] [Google Scholar]
- 15.Atiyeh B, Becker H, Ibrahim A, et al. Simplified skin excision pattern for skin sparing/reducing mastectomy and direct-to-implant single-stage immediate (dissi) breast reconstruction. Ann Plast Surg. In press [Google Scholar]
- 16.Atiyeh B, Abbas J, Costagliola M. Dermal barrier for immediate prosthetic breast reconstruction. Rev Bras Cir Plást. 2012;27:630––635. [Google Scholar]


