Abstract
Background:
The purpose of this study was to determine the risk factors for postoperative finger stiffness after open reduction and internal fixation of unstable proximal phalangeal fractures using a low-profile plate and/or screw system. We hypothesized that dorsal plate placement is a risk factor for postoperative finger stiffness.
Methods:
Seventy consecutive patients (50 men, 20 women; average age, 40 years) with 75 unstable proximal phalangeal fractures were treated with titanium plates and/or screws and evaluated at a minimum follow-up of 1 year. Thirty-six comminuted fractures and 24 intra-articular fractures were included, and 16 fractures had associated soft-tissue injuries. Plate fixation was performed in 59 fractures, and the remaining 16 were fixed with screws only. The implants were placed in a dorsal location in 33 fractures and in a lateral or volar location in 42 fractures. Finger stiffness was defined as a total active range of finger motion <80% for the treated finger. Univariate and multivariate analyses were performed on 8 variables: patient characteristics (age and sex), fracture characteristics (fracture comminution, joint involvement, and associated soft-tissue injury), and surgical characteristics (type and location of implants and removal of the implants).
Results:
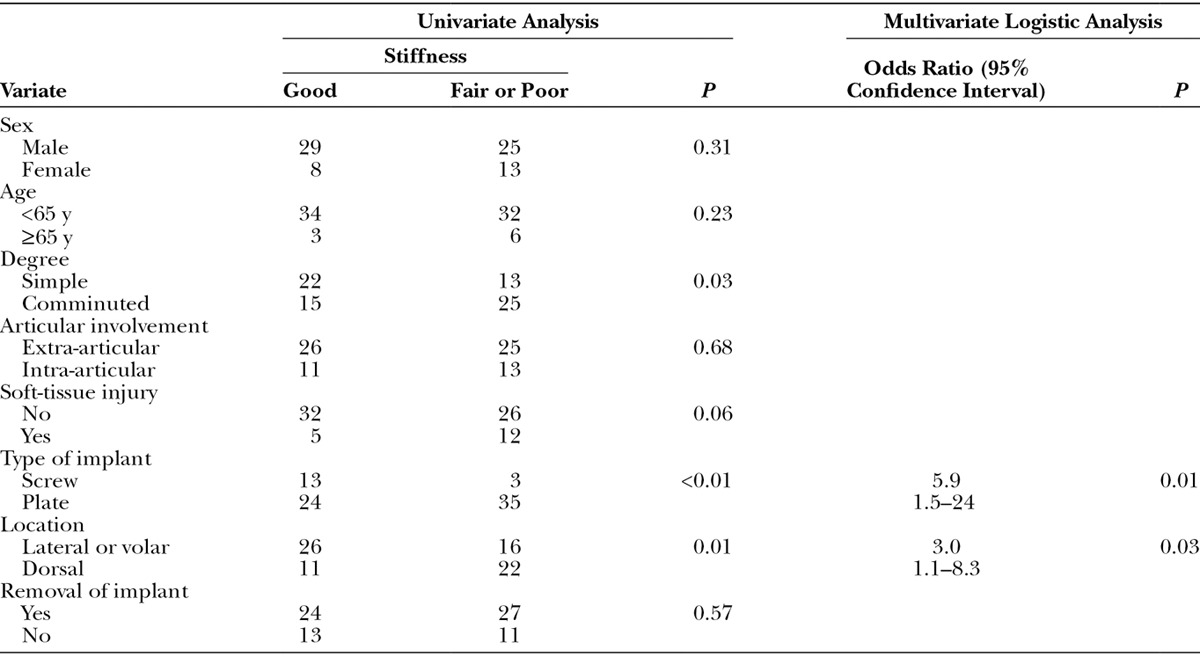
Postoperative finger stiffness occurred in 38 fractures. The multivariate analysis indicated that plate fixation (odds ratio, 5.9; 95% confidence interval, 1.5–24.0; P = 0.01) and dorsal placement (odds ratio, 3.0; 95% confidence interval, 1.1–8.3; P = 0.03) were independent risk factors for finger stiffness.
Conclusion:
We recommend the use of screw fixation as much as possible for unstable proximal phalangeal fractures using a midlateral approach.
Screw and/or plate systems are often used for unstable finger fractures. Although plate fixation provides strong stabilization and allows earlier and more intensive digital rehabilitation, postoperative finger stiffness is more likely to occur. Several patient and fracture variables have been reported to contribute to postoperative finger stiffness, including patient age, associated soft-tissue injury, and articular and phalangeal involvement.1–7 However, how surgical variables contribute to the occurrence of postoperative finger stiffness remains unclear.
Many investigators have reported that phalangeal fractures have a higher relative risk of finger stiffness because of the complex structure of the extensor mechanism.4–7 Therefore, in the present study, we only enrolled patients with proximal phalangeal fractures to assess the effects of surgical variables on finger stiffness. We hypothesized that dorsal plate placement is a risk factor for postoperative finger stiffness. The purpose of this study was to determine the risk factors for postoperative finger stiffness after open reduction and internal fixation of unstable proximal phalangeal fractures using a low-profile plate and/or screw system.
METHODS
Patients and Fracture Treatments
This study was approved by the Human Research Committee at our institution. Written informed consent was obtained from each patient, and the study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in prior approval by the appropriate institutional review committee. From February 2002 to January 2013, patients who were surgically treated for unstable proximal phalangeal fractures also underwent objective physical evaluations. A total of 70 consecutive patients (75 proximal phalangeal fractures) were treated with titanium plates and/or screws. Inclusion criteria for this study were as follows: (1) unstable (comminution and/or displacement) proximal phalangeal fractures; (2) operative treatment with titanium plates and/or screws; and (3) follow-up duration of at least 1 year. Patients with multiphalanx, wrist, or other upper-extremity fractures, as well as those with previous fracture histories, were excluded.
The patient cohort included 50 men and 20 women with a mean age of 40 years. Thirty-six patients had comminuted fractures, which were multifragmentary with more than 2 fragments at the fracture site, and 24 patients had intra-articular fractures. Sixteen patients had associated soft-tissue injuries, which were defined as an open fracture, extensor tendon injury, collateral ligament injury, or neurovascular injury. The mean duration from injury to surgery was 8 days (range, 0–35 days). Fifty-nine fractures were treated with titanium plates (locking plate: 5 fractures), and 16 fractures were treated with screws only. The implants (plate and screw head) were placed dorsal in 33 fractures and lateral and volar in 42 fractures.
Postoperative Physiotherapy
All patients underwent a consistent postoperative physiotherapy regimen following a standard protocol. After surgery, a bulky hand bandage with a forearm-based splint was applied for 3 days to control pain and swelling, and active motion was initiated thereafter. A buddy-tape bandage with the neighboring finger was used for protection and assisted movement of the injured finger. A static night splint was recommended for patients who had extension lag in the injured finger. Active assisted motion was started 6 weeks after the fracture and surrounding soft tissues had completely healed. Hand therapy was continued until rehabilitation was complete or there were no further improvements in the range of finger motion or grip strength.
Plate Removal
We recommended the removal of implants for patients who had plate fixations. Screw removal in the patients with screw fixation was done based on the patient preference. We removed the plate and screws in 45 patients (76%) and removed the screws only in 10 patients (63%). Concomitant procedure of tenolysis was performed when the implant was removed. Joint release was performed in 5 fingers in addition to the tenolysis when the patients complained of stiffness.
Evaluations
The total active motion was measured for all fingers at the final follow-up. The percent of total active motion (%TAM) was defined as the TAM of the injured finger relative to that of the maximum TAM according to Duncan’s criteria.6 They reported the maximum finger motion (260°) and maximum thumb motion (140°). We defined finger stiffness as a %TAM of <80% for the treated finger.
Statistical Analysis
Eight independent variables were examined: 2 patient characteristics (sex and age); 3 fracture characteristics (fracture comminution, articular involvement, and associated soft-tissue injury); and 3 surgical characteristics (type of implant, location of the implant, and removal of the implant). Univariate analyses were performed to compare the 8 independent variables between patients with and without postoperative finger stiffness using the Pearson chi-square test for categorical data. Factors that were significantly (P < 0.05) associated with finger stiffness in the univariate analyses were entered into a multivariate analysis using stepwise logistic regression (backward selection). We used the Hosmer-Lemeshow test to assess the model fit and calculated odds ratios (ORs) and 95% confidence intervals (CIs) using Statistical Package for the Social Sciences software (version 17.0; Statistical Package for the Social Sciences, Chicago, Ill.).
RESULTS
Correlation Coefficient of Independent Variables
Low correlations (|r| = 0.30–0.49) were found between age and sex, age and removal of implant, fracture comminution and type of implant, and removal of implant and type of implant. Little correlation (|r| = 0–0.29) was found in the other 20 comparisons.
The Univariate and Multivariate Logistic Analyses
Postoperative %TAM was evaluated at a mean follow-up time of 19 months (range, 12–60 months) after surgery. The mean postoperative range of motion of the affected fingers was 214° (range, 99–270°) and that of the affected thumbs was 104° (range, 62–140°). Thirty-eight fingers (51%) had stiffness (%TAM < 80%). The univariate analyses indicated that comminuted fracture (P=0.03), plate fixation (P = 0.004) and dorsal implant placement (P = 0.01) were significant factors. The multivariate logistic analysis indicated that plate fixation (OR, 5.9; 95% CI, 1.5–24.0; P = 0.01) and dorsal placement (OR, 3.0; 95% CI, 1.1–8.3; P = 0.03) were independent risk factors for finger stiffness (Table 1). Averaged %TAM of each surgical groups were 73% ± 18% (plate, dorsal), 81% ± 11% (plate, not dorsal), 88% ± 11% (screw, dorsal), and 92% ± 7% (screw, not dorsal). Using the backward stepwise procedure in the final multivariate logistic model, the type of implant and location of the implant resulted in a formula that could account for 63% of the variability in postoperative finger stiffness.
Table 1.
Univariate and Multivariate Associations of Patient, Fracture, and Surgical Characteristics with Postoperative Finger Stiffness
DISCUSSION
The results of this study indicated that plate fixation and dorsal placement of the implant were independent risk factors during the surgical treatment of unstable proximal phalangeal fractures. Based on these data, plate fixation was 5.9 times more likely to result in postoperative finger stiffness than screw fixation, whereas dorsal placement of the implant was 3.0 times more likely to result in postoperative finger stiffness than lateral and volar placement. Considering the complexity of the extensor mechanism at the proximal phalangeal level, it is clear that dorsal plate placement can affect postoperative finger motion, even if longitudinal splitting of the extensor tendon is used during the dorsal surgical approach.8,9 Because there is no intervening soft tissue between the dorsal plate and the extensor tendon, the inevitable adhesions between them may have caused postoperative restriction of the finger motion observed here. Field et al10 suggested that a midlateral approach was less likely to cause scarring of the dorsal apparatus than the dorsal approach and also minimized extensor lag of the proximal interphalangeal joint. Freeland et al11 recommended a midlateral skin incision, with excision of the oblique spiral fibers and the adjacent portion of the lateral band as a triangle. For the lateral plate placement in the present series, we used a midlateral approach to the lateral band to avoid damaging the extensor tendon apparatus.
Based on the present multivariate analysis, we recommend the use of screw fixation where possible for unstable proximal phalangeal fractures using a midlateral approach (Figs. 1, 2). In cases with transverse or comminuted fractures, which are difficult fractures to fix with screws alone, lateral plate fixation is recommended (Figs. 3–5). We agree with Jones et al12 that lateral plate fixation prevents interference with gliding of the overlying extensor tendon.5 In addition, a biomechanical study indicated that the mechanical properties of the proximal phalanx after lateral plate fixation were comparable with those after dorsal plate fixation.13
Fig. 1.
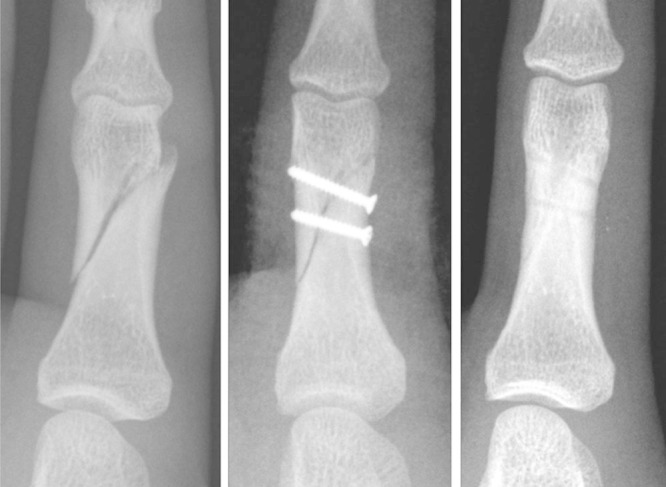
Case 1: A simple oblique fracture of the proximal phalanx in the left little finger of a 17-year-old boy. Preoperative and postoperative radiographs.
Fig. 2.
Case 1: Intraoperative photograph and finger motion at the final follow-up.
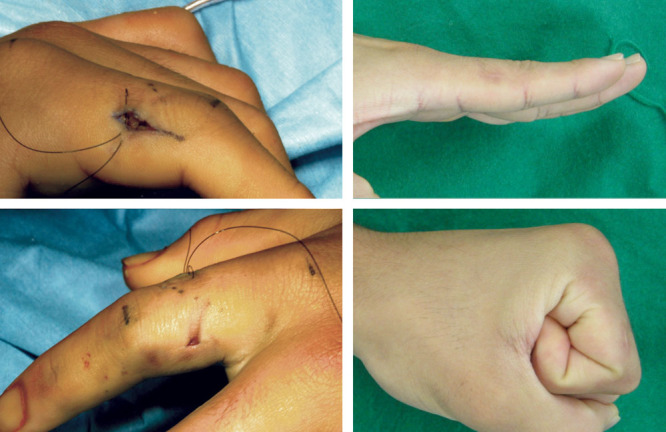
Fig. 3.
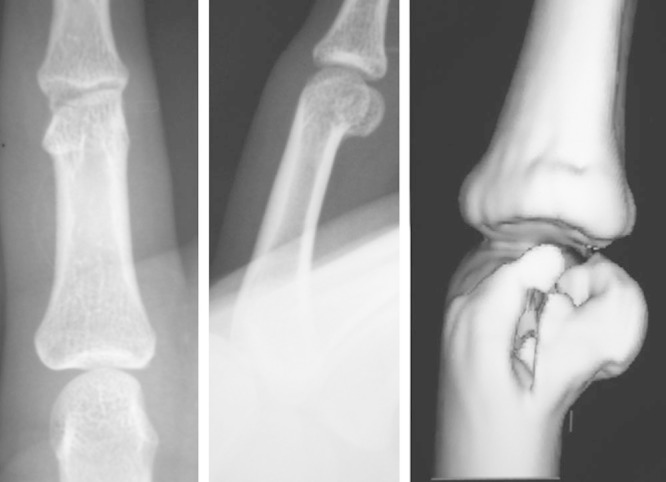
Case 2: A comminuted intra-articular fracture of the unicondylar proximal phalangeal phalanx in the index finger of a 17-year-old boy. Preoperative radiograph and computed tomography image.
Fig. 5.
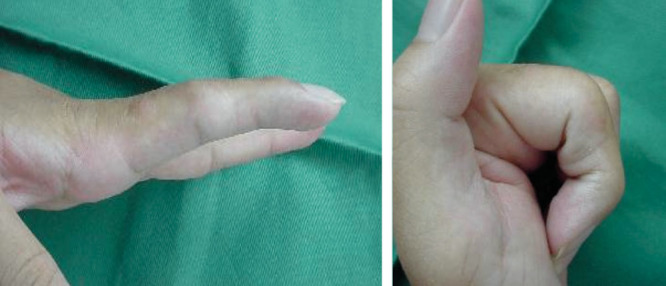
Case 2: Finger motion at the final follow-up.
Fig. 4.
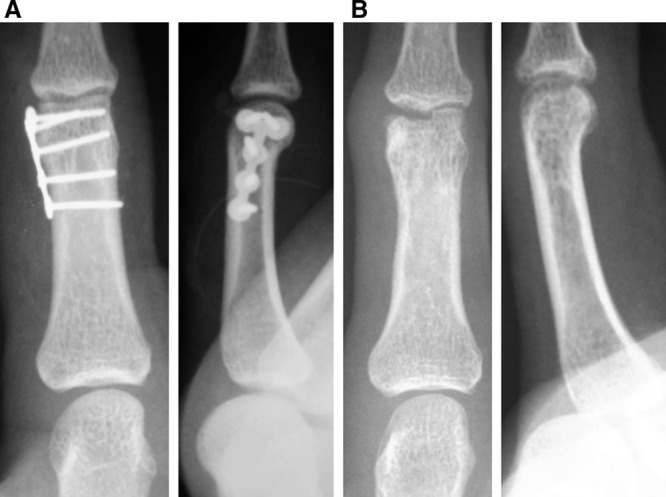
Case 2: Fixation with a 1.5-mm T-plate laterally (A) and a postoperative radiograph after the implant removal procedure (B).
One limitation of the present study was that surgeon preferences regarding implant selection and the surgical approach were not controlled. There is a bias related to selection of implant (plate or screw). However, based on the current analysis, type of implant had low correlation with comminuted fracture, and little correlation was found with intra-articular fracture and associated soft-tissue injury. Additionally, controlling for surgical variables, such as duration from injury to surgery and the surgical procedure, is difficult in a prospective cohort study. Future prospective controlled trials comparing different surgical interventions, such as between locking and nonlocking plate fixation, would help to determine which strategy is most beneficial for patients with difficult finger fractures.
CONCLUSION
We recommend the use of screw fixation as much as possible for unstable proximal phalangeal fractures using a midlateral approach.
ACKNOWLEDGMENTS
We thank Dr. Kobata Yasunori, Dr. Yasuaki Nakanishi, and Dr. Kenichi Nakano for their valuable help during clinical treatments.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Pun WK, Chow SP, So YC, et al. A prospective study on 284 digital fractures of the hand. J Hand Surg Am. 1989;14:474–481. doi: 10.1016/s0363-5023(89)80006-1. [DOI] [PubMed] [Google Scholar]
- 2.Ouellette EA, Freeland AE. Use of the minicondylar plate in metacarpal and phalangeal fractures. Clin Orthop Relat Res. 1996;327:38–46. doi: 10.1097/00003086-199606000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am. 1998;23:827–832. doi: 10.1016/S0363-5023(98)80157-3. [DOI] [PubMed] [Google Scholar]
- 4.Bannasch H, Heermann AK, Iblher N, et al. Ten years stable internal fixation of metacarpal and phalangeal hand fractures—risk factor and outcome analysis show no increase of complications in the treatment of open compared with closed fractures. J Trauma. 2010;68:624–628. doi: 10.1097/TA.0b013e3181bb8ea0. [DOI] [PubMed] [Google Scholar]
- 5.Omokawa S, Fujitani R, Dohi Y, et al. Prospective outcomes of comminuted periarticular metacarpal and phalangeal fractures treated using a titanium plate system. J Hand Surg Am. 2008;33:857–863. doi: 10.1016/j.jhsa.2008.01.040. [DOI] [PubMed] [Google Scholar]
- 6.Duncan RW, Freeland AE, Jabaley ME, et al. Open hand fractures: an analysis of the recovery of active motion and of complications. J Hand Surg Am. 1993;18:387–394. doi: 10.1016/0363-5023(93)90080-M. [DOI] [PubMed] [Google Scholar]
- 7.Shimizu T, Omokawa S, Akahane M, et al. Predictors of the postoperative range of finger motion for comminuted periarticular metacarpal and phalangeal fractures treated with a titanium plate. Injury. 2012;43:940–945. doi: 10.1016/j.injury.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 8.Nunley JA, Kloen P. Biomechanical and functional testing of plate fixation devices for proximal phalangeal fractures. J Hand Surg Am. 1991;16:991–998. doi: 10.1016/s0363-5023(10)80057-7. [DOI] [PubMed] [Google Scholar]
- 9.Pratt DR. Exposing fractures of the proximal phalanx of the finger longitudinally through the dorsal extensor apparatus. Clin Orthop. 1959;15:22–26. [PubMed] [Google Scholar]
- 10.Field LD, Freeland AE, Jabaley ME. Midaxial approach to the proximal phalanx for fracture fixation. Contemp Orthop. 1992;25:133–137. [Google Scholar]
- 11.Freeland AE, Sud V, Lindley SG. Unilateral intrinsic resection of the lateral band and oblique fibers of the metacarpophalangeal joint for proximal phalangeal fracture. Tech Hand Up Extrem Surg. 2001;5:85–90. doi: 10.1097/00130911-200106000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Jones NF, Jupiter JB, Lalonde DH. Common fractures and dislocations of the hand. Plast Reconstr Surg. 2012;130:722e–736e. doi: 10.1097/PRS.0b013e318267d67a. [DOI] [PubMed] [Google Scholar]
- 13.Ouellette EA, Dennis JJ, Latta LL, et al. The role of soft tissues in plate fixation of proximal phalanx fractures. Clin Orthop Relat Res. 2004;418:213–218. doi: 10.1097/00003086-200401000-00036. [DOI] [PubMed] [Google Scholar]


