Abstract
Background
The aim of this study was to compare the novel needle-over-cannula vs. the Braun continuous peripheral nerve block catheter set (Contiplex A) in postoperative analgesics after total knee arthroplasty (TKA).
Material/Methods
Sixty patients undergoing total knee arthroplasty were randomly assigned to Braun continuous peripheral nerve block catheter set group (Braun Group, n=30) or the novel needle-over-cannula group (Cannula Group, n=30). All the patients in the 2 groups received continuous femoral nerve block (CFNB) for postoperative analgesics.
Results
We found no significant difference in analgesic effect between the 2 groups. The time of catheter or cannula insertion was shorter in the Cannula Group than in the Braun Group. Four (13.32%) out of 30 patients had failed catheter insertions in the Braun Group compared to none in the Cannula Group. Twelve (46%) out of 26 patients in the Braun Group had serious local anesthetic leakage at puncture sites during 12 h compared to none in the Cannula Group.
Conclusions
The novel needle-over-cannula is effective, convenient, and safe in CFNB after TKA.
MeSH Keywords: Analgesia; Arthroplasty, Replacement, Knee; Femoral Nerve; Nerve Block
Background
Although total knee arthroplasty (TKA) improves patients’ long-term quality of life, it often results in severe pain immediately after surgery, which is difficult to control solely with oral or intravenous analgesics. Postoperative pain of TKA is one of the most serious problems in clinics and is difficult to manage [1–3]. A patient who has a high level of post-TKA pain is more likely to have poor functional outcomes [4]. Multiple techniques of postoperative pain control have been used after TKA, including intravenous (IV) opioids, continuous epidural analgesia (CEA) [5,6], and continuous femoral nerve block (CFNB) [7–12]. Nerve block is the foundation of multiple pain management modalities in TKA and offers the potential benefit of extended postoperative analgesia; it has few adverse effects and allows faster rehabilitation compared with intravenous analgesia [13–17]. The Braun (Contiplex A) continuous peripheral nerve block catheter is widely used in China and many other countries and is very effective in peripheral nerve block analgesia. Nevertheless, it has many disadvantages, such as complicated procedure of catheter insertion, the tip of the catheter is not visible, and sometimes local anesthesia liquid leaks at the puncture site. A novel needle-over-cannula has been invented to solve these problems (Figure 1A). The novel needle-over-cannula (22-gauge needle, 90-mm length external indwelling cannula; Tuoren Group, Xinxiang, China) is an innovative product invented by Dr. Bin Yu, who is also the first author of the present article. The novel needle-over-cannula had an authorized patent in China, and a related patent had also been applied for in the U.S. (application number 14357772).
Figure 1.
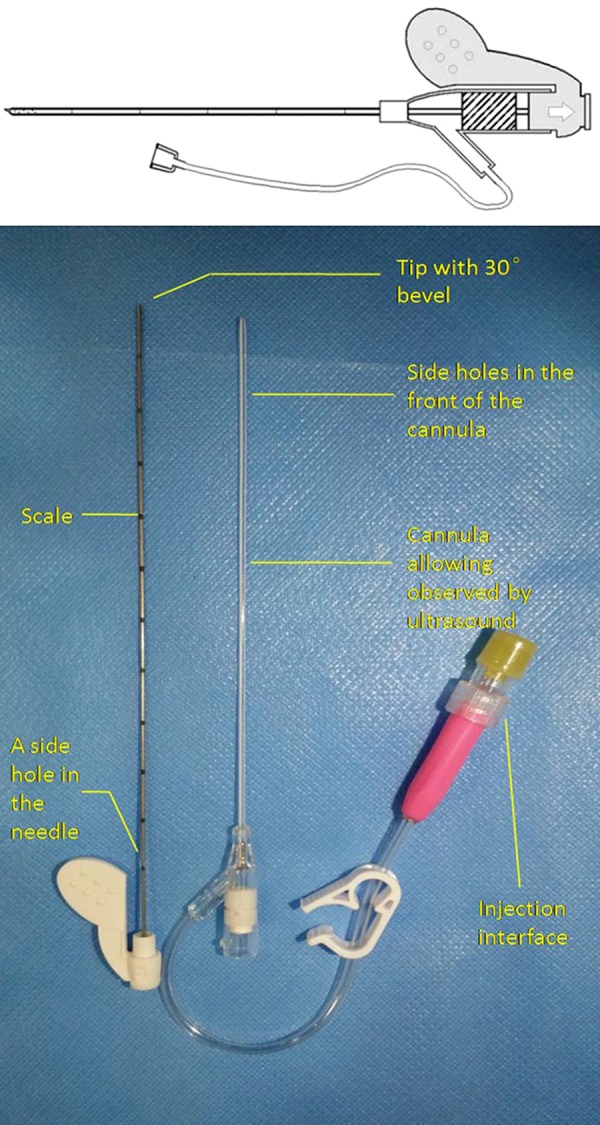
(A) A schematic of the novel needle-over-cannula; (B) The novel needle-over-cannula (22-gauge needle, 90-mm-length external indwelling cannula; Tuoren Group, Xinxiang, China) invented by Dr. Bin Yu, who is also the first author of the article.
The novel needle-over-cannula has many characteristics [7–12]. It is different from Braun continuous peripheral nerve block catheter set with indwelling catheter. The cannula is outside of the needle, so it could be indwelled directly after withdrawing the needle instead of indwelling another catheter again. It not only saves much time but also dramatically enhanced the success rate of cannula indwelling. Additionally, the novel needle-over-cannula has a short needle tip with a 30° bevel. The feeling of needle tip breaking through the sheath could be more obvious. It could also reduce direct injury to the peripheral nerves (Figure 1B). The indwelling cannula is made from biocompatible polyurethane, and the side holes in the tip allow smooth infusion. The indwelling cannula is labeled with a radiological-opaque scale allowing the placement of the cannula and the infusion could be observed by radiography or ultrasound. The novel needle-over-cannula has lengths from 5 cm to15 cm and each has a 20-gauge cannula.
Material and Methods
Patient enrollment
The clinical trial was approved by the Ethics Committee of Tongji Hospital of Shanghai (Shanghai, China) (ref.230), and was registered in Chinese Clinical Trial Registry (ChiCTR) (ref: ChiCTR-TRC-14004697). Written consents have been obtained from patients after they understood the concept and technological processes of the research. The study was implemented in accordance with the principles of the Helsinki Declarations.
This randomized, single blind, parallel-group trial was conducted in a single center from June to October in 2014. Patients who were going to accept TKA were recruited in Tongji Hospital of Shanghai. The exclusion criteria included severe heart and lung diseases, skin infection at the puncture site, or patient refusal.
Sixty enrolled patients were equally randomized to 2 groups by using a computer-generated randomization program: the Braun continuous peripheral nerve block catheter (B. Braun Melsungen AG) set group (Braun Group, n=30) and the novel needle-over-cannula group (Cannula Group, n=30). Independent researchers who were not involved in the anesthesia procedures or outcome assessment conducted patient enrollment, generated the random allocation and prepared a sealed envelope. Intravenous access for anesthesia was obtained on the night before the surgery. All patients were fasted for 8 h and received intramuscular atropine (0.01 mg/kg) as premedication 30 min before induction of anesthesia.
Anesthetic procedures
After patients entered the operating room, assistants opened a ranked envelope marked labeled “Braun Group” or “Cannula Group”. Noninvasive blood pressure, electrocardiogram, heart rate, pulse oxygen saturation, end-tidal carbon dioxide, and end-tidal sevoflurane concentrations were monitored throughout the surgery. All the nerve blocks were performed by 2 investigators (Dr. Bin Yu or Dr. Xiaoxue Hu), who both have substantial experience in ultrasound-guided peripheral nerve block. Follow-up visits were performed by the same standardized training anesthesiologists.
A loading infusion of dexmedetomidine of 1 ug/kg was pumped over 10 min before ultrasound-guided CFNB. Then the patient entered moderate sedation and the speed of the pump was reduces to 0.3 ug/kg/h.
Continuous femoral nerve block was performed after routine sterilization of the inguinal region. Sterile gel was applied to the inguinal area. A linear 6–13 MHz ultrasound probe wrapped with a sterilized plastic sheath was used for CFNB.
In the Braun Group, both ultrasound and nerve stimulator guided CFNB were performed with the transducer parallel to the arcus cruralis, which was vertical to the femoral nerve. In the ultrasound image, vein, artery, and femoral nerve were ranked from inside to outside. The puncture point was on the outside of the transducer at an angle of about 30° to the transducer. A 18-gauge, 110-mm needle was inserted in-plane from the superior-lateral to inferior-medial position after the puncture point was infiltrated with 1 ml of 1% lidocaine [18]. The nerve stimulator was connected to the needle. The initial stimulus current was set as 1 mA and stimulating frequency as 2 Hz. While causing quadriceps contraction with knees, the current was reduced to 0.3–0.5 mA. Twenty ml of 0.5% ropivacaine was injected to create a perineural fluid space around the femoral nerve with the guide of ultrasound. At the same time, unit 4 biceps rhythmic contraction was stopped. The needle was then pulled out and the cannula was left, and catheter was inserted to 10 cm through the cannula. We confirmed that the catheter was not in blood vessels by pulling back and bolus normal saline before fixed the catheter.
In the Cannula Group, the transducer was also parallel to the arcus cruralis. The puncture point was 1 cm below the transducer at the lateral of femoral nerve 0.5 cm to avoid nerve injury. The novel needle-over-cannula was inserted out-plane at an angle of about 30° to skin, vertical to the arcus cruralis, and parallel to the femoral nerve (Figure 2). There was a double click when breaking through the fascia iliaca and fascia lata. After breaking through the 2-layer fascias, we injected 20 ml 0.5% ropivacaine to create a perineural fluid space with ultrasound guidance (Figure 3). Then the needle kept still, and the cannula was inserted forward 3–4 cm, then we pulled the needle out and fixed the cannula to the skin with no-pressure medical tape (Figure 4). The cannula could be observed clearly in the ultrasound image (Figure 5). A liquid area appeared at the tip of cannula when injecting normal saline through the injection interface, which could also be connected to the analgesia pump after the operation.
Figure 2.

The novel needle-over-cannula was inserted out-plane at an angle of about 30° to skin, vertical to arcus cruralis, parallel to femoral nerve.
Figure 3.
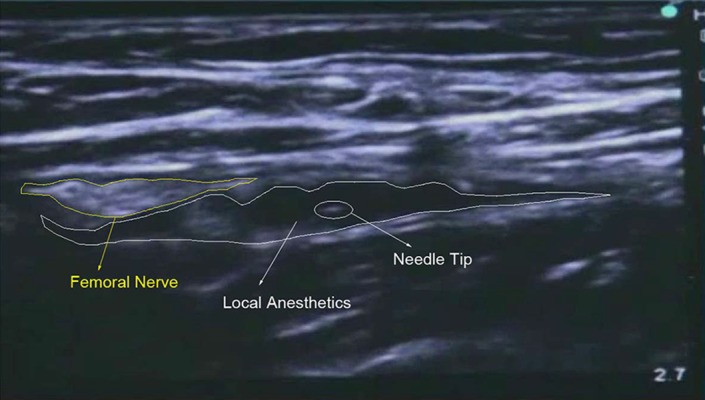
Ultrasound of the perineural fluid space with injection of 20 ml 0.5% ropivacaine after the needle breaking through fascia iliaca and fascia lata.
Figure 4.

After the needle was pulled out and the cannula was fixed to the skin with no-pressure medical tape.
Figure 5.
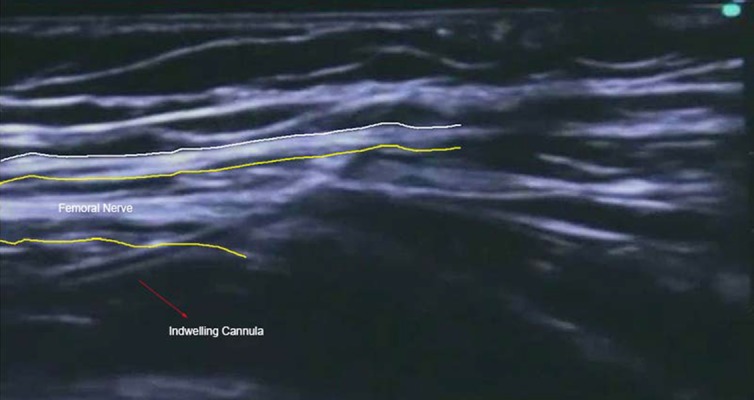
Ultrasound image of the cannula after procedures.
After CFNB was accomplished, propofol, fentanyl, and CIS atracurium besilate were injected intravenously for anesthesia induction. Three minutes later, an appropriate-size laryngeal mask was placed to control the airway. Sevoflurane and propofol were adjusted to maintain stable vital signs during the surgery. When the operation was finished, the catheter was connected to a digital analgesia pump. The pump was loaded with 300 ml of 0.2% ropivacaine and 50 ug sufentanil, and its basal flow rate was 6 ml/h. Forty mg of parecoxib was injected intravenously to reach multimodal analgesia. Parecoxib was added at any time when the patient felt unbearable pain after surgery.
Patient safety was foremost. Researchers paid attention to patient reactions, such as electric shock sensation, expiratory dyspnea, dizziness, and tinnitus.
Outcome measurements
During the process, we recorded the time needed for nerve block management, the insertion depth of catheter or cannula, the time needed to place the catheter, and the adverse reactions to local anesthetics. CFNB was maintained for 48 h after the surgery. At the same time, the researchers closely observed the patients. We assessed pain at rest and during movement (the knee was bent passively) using VAS scoring (ranging from VAS=0 for no pain to VAS=10 for maximal pain) [19], muscle strength of 4-unit head muscle (0=strength completely disappeared, no activity; 1=muscle contraction, no joint activities; 2=muscle contraction, slight joint activity, but not against the gravity of the body; 3=joint activities against the gravity of the body, but not against external resistance; 4=joint activities against external resistance, but strength weak; 5=strength normal), low limb motor block using modified Bromage score MBS (0: No motor block, 1: No carrying lower limb, 2: No bending knees, 3: No bending ankles), the skin pain feeling of obturator nerve, femoral nerve, the lateral femoral cutaneous nerve district, local anesthetics intoxication symptoms, local anesthetic leakage at puncture site, catheter or cannula occlusion and slipping, nerve injury related complication, the puncture site inflammation, and incidence of nausea and vomiting were all recorded at 6, 12, 24 and 48 h after the surgery. Patient satisfaction (ranging from 0 for very dissatisfied to 10 for very satisfied) and the maximal degree of knee flexion was recorded when analgesia ended in 48 h. On the seventh day after surgery, we would record if the patients had any nerve injury symptom.
Statistical analysis
Descriptive statistics were applied in statistical analysis of most measurements in this study. Statistical analysis of the enumeration data used Fisher’s exact test. Quantitative data are expressed as mean ± standard deviation (SD) unless otherwise specified. P less than 0.05 was considered statistically significant.
Results
The sex, age, height, body weight, and basis SPO2 were not significantly different between the 2 groups. There were 4 catheter indwelling failures (13.3%) among 30 patients in the Braun Group (Table 1). In these 4 cases, the operators tried more than 30 min, but they still could not insert the catheter. As a result, we used CFNB with fentanyl used as intravenous analgesia instead. Nine of 26 patients we been tried more than once to insert the catheter in the Braun Group. All cannula indwelling were completed at first attempt in the Cannula Group and none of the cannula insertions failed in the Cannula Group. Serious local anesthetic leakage occurred in 12 patients at the puncture site within 12 h in the Braun Group (Table 2). There were no local anesthetic leakages in the Cannula Group. The catheter insertion time of the Braun Group was statistically significantly longer than in the Cannula Group. There were no statistically significant differences in catheter or cannula indwelling depth, VAS (no activities/ activities, except the high scores in activities in 24 h, nausea and vomiting, muscle strength, MBS, patient satisfaction, or maximal degree of knee flexion between the 2 groups. Effect of nerve block was more significant in the region dominated by the lateral cutaneous femoral nerve and femoral nerve than the obturator nerve in the 2 groups.
Table 1.
Situations and complications of the 2 groups.
| Braun group | Cannula group | P-value | |
|---|---|---|---|
| No. | 30 | 30 | n.s. |
| Placement failure | 4/30 | 0/30 | n.s. |
| Single attempt success | 17/26 | 29/30* | <0.05 |
| Time of placement (min) | 13.13±3.29 | 5.84±0.77* | <0.05 |
| Indwelling depth (cm) | 9.73±1.49 | 7.24±1.15 | n.s. |
| Catheter or cannula occlusion | 0 | 0 | n.s. |
| Catheter or cannula slipping | 0 | 0 | n.s. |
| Infection at puncture site | 0 | 0 | n.s. |
| Nerve injury related complication | 0 | 0 | n.s. |
| Severe intoxication | 0 | 0 | n.s. |
| The maximal degree of knee flexion | 87.69°±12.43° | 88°±12.97° | n.s. |
| Patient satisfaction | 8.65±0.85 | 8.63±1.03 | n.s. |
n.s. – not significant.
P<0.05 considered statistically significant.
Table 2.
Postoperative follow-up of the 2 groups.
| VAS (no activities/activities) | Muscle strength of four unit head muscle | Modified Bromage score | Local anesthetic leakage at puncture site | Sense nerve block LFCN/FN/ON | Nausea/ vomiting | Parecoxib | ||
|---|---|---|---|---|---|---|---|---|
| 6 h | Braun group | 0.54±1.07/2.35±1.98 | 3.81±0.69 | 0.65±0.63 | 7/26 | 1/7/0 | 0/26 | 1/26 |
| Cannula group | 0.40±0.81/2.07±1.44 | 4±0.53 | 0.67±0.61 | 0/30* | 7/15/1 | 0/26 | 0/30 | |
| P-value | n.s. | n.s. | n.s. | <0.05 | n.s | n.s | n.s | |
| 12 h | Braun group | 1.35±1.41/3.19±2.79 | 4.23±0.76 | 0.46±0.58 | 12/26 | 0/2/1 | 2/26 | 2/26 |
| Cannula group | 1.1±1.40/2.27±2.15 | 4.43±0.68 | 0.50±0.68 | 0/30* | 0/7/0 | 1/30 | 1/30 | |
| P-value | n.s | n.s | n.s | <0.05 | n.s | n.s | n.s | |
| 24 h | Braun group | 1.39±1.36/4.12±1.88 | 4.54±0.58 | 0.38±0.57 | 12/26 | 1/3/1 | 0/26 | 0/26 |
| Cannula group | 0.9±1.34/2.87±2.01* | 4.73±0.52 | 0.20±0.48 | 0/30* | 2/3/0 | 0/30 | 2/30 | |
| P-value | <0.05 | n.s | n.s | <0.05 | n.s | n.s | n.s | |
| 48 h | Braun group | 1.31±1.26/3.85±1.60 | 4.77±0.51 | 0.15±0.37 | 12/26 | 0/0/0 | 0/26 | 0/26 |
| Cannula group | 1.27±1.23/3.33±1.40 | 4.90±0.31 | 0.13±0.35 | 0/30* | 0/0/0 | 0/30 | 1/30 | |
| P-value | n.s | n.s | n.s | <0.05 | n.s | n.s | n.s |
n.s. – not significant.
P<0.05considered statistically significant.
In 48-h analgesia, there was no blocked catheter or cannula, no infection at the puncture site, and no local anesthetics intoxication symptoms in the 2 groups. Knee flexion had no statistically significant differences between the 2 groups at 48 h. No patient complained of paresthesia at the affected limb on postoperative day 7 after removal of the catheter or cannula.
Discussion
This randomized, single-blind, parallel-group, clinical trial compared Braun catheter sets and cannula for continuous plexus anesthesia (Contiplex A) with a novel needle-over-cannula method, which was a completely novel product [20]. The design is simpler than the Braun Contiplex A. Compared with Braun Contiplex A, it has only 1 cannula and 1 needle. Table 1 shows that inserting the catheter would not be difficult for an anesthesiologist. It not only enhanced the success rate of continuous nerve block, but also saved much more time and made the operation more convenient. There is another serious problem that cannot be ignored in Braun Contiplex A – the catheter was inserted in the needle and when the cannula was drawn out there was a space between the catheter and human tissue. As a result, exosmosis of the local anesthetics is more likely from the puncture site, which causes a dilemma for postoperative nursing and increases the dose of local anesthetics. It may also affect the analgesic effects after surgery. However, this may be an explanation for the VAS score, in which there were no statistical differences between at rest and during movement except for 24 h after surgery. The local anesthetic leakage in the Braun Group may have caused the difference. The Braun catheter was so soft that it caused insertion difficulty. In such situations, the Braun catheter had to be abandoned. We had explicit evidence to support these 2 points from the experimental results.
Ultrasound guide was an important means to elevate the accuracy of nerve block, which is a benefit to both doctors and patients. The novel needle-over-cannula could be clearly seen with ultrasound. Most importantly, the whole indwelling cannula could also be observed instead of the indistinct catheter in the Braun Group, and this makes nerve block more accurate and safe. Although the tip of the cannula is the same softness as the Braun catheter, with the support of the inner needle it is easier to insert and cause no nerve injury.
We had also designed a needle-over-cannula which could be connected to a nerve stimulator. With the guide of ultrasound and nerve stimulator, nerve block would be more and more accurate. There would be more possibilities for a dose of local anesthesia further reduction.
CFNB accelerates the achievement of 120° knee flexion after TKA compared with CEA. It is a promising alternative pain management strategy during postoperative knee flexion rehabilitation, and it can facilitate the early resumption of daily activities. According to data displayed in Tables 1 and 2, there were no significant differences in the maximal degree of knee flexion, muscle strength, and patient satisfaction between the 2 groups. Both the Braun catheter and the cannula could transport local anesthetics to the space around the femoral nerve and there were no adverse reactions caused by CFNB in either group. A limitation of the present study is its small number of participants. Our results may help popularize the novel needle-over-cannula method in continuous femoral nerve block analgesia after total knee arthroplasty, and may lay the foundation for larger and multi-center clinical trials.
Conclusions
Taken together, the novel needle-over-cannula is effective, convenient, and safe in continuous femoral nerve block analgesia after total knee arthroplasty (TKA). When compared with Braun catheter, this novel method has the same function as the Braun catheter but without local anesthetic leakage at puncture sites and it is much more convenient. This novel method may be a better choice that the Braun catheter in clinical practice.
Acknowledgements
The authors thank the Anesthesia Department of Guanghua integrated traditional Chinese and Western medicine Hospital of Shanghai for technical support.
Footnotes
Source of support: Shanghai Municipal Commission of Health and Family Planning; Project of Shanghai Municipal Health Bureau (No. 20124362)
References
- 1.Sakai N, Inoue T, Kunugiza Y, et al. Continuous femoral versus epidural block for attainment of 120 knee flexion after total knee arthroplasty: a randomized controlled trial. J Arthrop. 2013;28:807–14. doi: 10.1016/j.arth.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 2.Maheshwari AV, Blum YC, Shekhar L, et al. Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthop Relat Res. 2009;467:1418–23. doi: 10.1007/s11999-009-0728-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Society KK. Guidelines for the management of Postoperative pain after total knee arthroplasty. Knee Surg Relat Res. 2012;24:201. doi: 10.5792/ksrr.2012.24.4.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams-Russo P, Sharrock NE, Haas SB, et al. Randomized trial of epidural versus general anesthesia: outcomes after primary total knee replacement. Clin Orthop Relat Res. 1996;331:199–208. doi: 10.1097/00003086-199610000-00028. [DOI] [PubMed] [Google Scholar]
- 5.Mahoney OM, Noble PC, Davidson J, Tullos HS. The effect of continuous epidural analgesia on postoperative pain, rehabilitation, and duration of hospitalization in total knee arthroplasty. Clin Orthop Relat Res. 1990;260:30–37. [PubMed] [Google Scholar]
- 6.Chloropoulou P, Iatrou C, Vogiatzaki T, et al. Epidural anesthesia followed by epidural analgesia produces less inflammatory response than spinal anesthesia followed by intravenous morphine analgesia in patients with total knee arthroplasty. Med Sci Monit. 2013;19:73–80. doi: 10.12659/MSM.883749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sundarathiti P, Ruananukul N, Channum T, et al. A comparison of continuous femoral nerve block (CFNB) and continuous epidural infusion (CEI) in postoperative analgesia and knee rehabilitation after total knee arthroplasty (TKA) J Med Assoc Thai. 2009;92:328–34. [PubMed] [Google Scholar]
- 8.Singelyn FJ, Deyaert M, Joris D, et al. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg. 1998;87:88–92. doi: 10.1097/00000539-199807000-00019. [DOI] [PubMed] [Google Scholar]
- 9.Capdevila X, Barthelet Y, Biboulet P, et al. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology. 1999;91:8–15. doi: 10.1097/00000542-199907000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Ilfeld BM, Le LT, Meyer RS, et al. Ambulatory continuous femoral nerve blocks decrease time to discharge readiness after tricompartment total knee arthroplasty: a randomized, triple-masked, placebo-controlled study. Anesthesiology. 2008;108:703–13. doi: 10.1097/ALN.0b013e318167af46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barrington MJ, Olive D, Low K, et al. Continuous femoral nerve blockade or epidural analgesia after total knee replacement: a prospective randomized controlled trial. Anesth Analg. 2005;101:1824–29. doi: 10.1213/01.ANE.0000184113.57416.DD. [DOI] [PubMed] [Google Scholar]
- 12.Paul JE, Arya A, Hurlburt L, et al. Femoral nerve block improves analgesia outcomes after total knee arthroplasty: a meta-analysis of randomized controlled trials. Anesthesiology. 2010;113:1144–62. doi: 10.1097/ALN.0b013e3181f4b18. [DOI] [PubMed] [Google Scholar]
- 13.Morin AM, Kratz CD, Eberhart LHJ, et al. Postoperative analgesia and functional recovery after total-knee replacement: comparison of a continuous posterior lumbar plexus (psoas compartment) block, a continuous femoral nerve block, and the combination of a continuous femoral and sciatic nerve block. Region Anesth Pain Med. 2005;30:434–45. doi: 10.1016/j.rapm.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 14.Strassels SA, Chen C, Carr DB. Postoperative analgesia: economics, resource use, and patient satisfaction in an urban teaching hospital. Ants Analg. 2002;94:130–37. doi: 10.1097/00000539-200201000-00025. [DOI] [PubMed] [Google Scholar]
- 15.Barrington JW, Halaszynski TM, Sinatra RS. Perioperative pain management in hip and knee replacement surgery. Am J Orthop. 2014;43:S1–16. [PubMed] [Google Scholar]
- 16.Ilfeld BM, Mariano ER, Girard PJ, et al. A multicenter, randomized, triple-masked, placebo-controlled trial of the effect of ambulatory continuous femoral nerve blocks on discharge-readiness following total knee arthroplasty in patients on general orthopaedic wards. Pain. 2010;150:477–84. doi: 10.1016/j.pain.2010.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Ruyter ML, Brueilly KE, Harrison BA, et al. A pilot study on continuous femoral perineural catheter for analgesia after total knee arthroplasty: the effect on physical rehabilitation and outcomes. J Arthroplasty. 2006;21:1111–17. doi: 10.1016/j.arth.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 18.Wang A-Z, Gu L, Zhou Q-H, et al. Ultrasound-guided continuous femoral nerve block for analgesia after total knee arthroplasty: catheter perpendicular to the nerve versus catheter parallel to the nerve. Reg Anesth Pain Med. 2010;35:127–31. doi: 10.1097/aap.0b013e3181d24529. [DOI] [PubMed] [Google Scholar]
- 19.Bodian CA, Freedman G, Hossain S, et al. The visual analog scale for pain: clinical significance in postoperative patients. Anesthesiology. 2001;95:1356–61. doi: 10.1097/00000542-200112000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Yu B, Zhang X, Sun P, et al. Non-stimulation needle with external indwelling cannula for brachial plexus block and pain management in 62 patients undergoing upper-limb surgery. Int J Med Sci. 2012;9:766–71. doi: 10.7150/ijms.5007. [DOI] [PMC free article] [PubMed] [Google Scholar]


