Abstract
Purpose
To describe what knowledge heart failure patients expect to acquire in relation to their upcoming cardiac resynchronization therapy (CRT) device implantation, to describe their self-care and health complaints, and to explore the relationship between knowledge expectations and self-care, health complaints, and background factors.
Patients and methods
Cross-sectional multicenter study with 104 patients scheduled for a first-time, elective CRT implantation in Swedish and Icelandic hospitals. Data were collected with the Knowledge Expectations of hospital patient Scale, European Heart Failure Self-care Behavior Scale, and Adjusted Postoperative Recovery Profile.
Results
Patients expected most knowledge related to their disease and its treatment (median 4.0, interquartile range 0.13) and least on social issues (median 3.5, interquartile range 0.83). Their self-care was average (standardized mean 51.0±19.6) before the procedure. Patients had on average 8.2 (±4.7) health complaints and rated fatigue and sexual problems as the most severe. Age was independently associated with knowledge expectations (Expβ 0.049, P=0.033).
Conclusion
Heart failure patients waiting for a CRT device implantation have high expectations for multiple aspects of knowledge, including self-care issues, before their procedure. These expectations are similar to those of other surgical patients and they increase with age.
Keywords: cardiac devices, CRT treatment, patient education
Introduction
Optimal education for patients with chronic diseases is high on most current agendas within health care, for example, the World Health Organization’s Chronic Diseases and Health Promotion program,1 in order to ensure that patients have the necessary knowledge needed for appropriate self-care, adherence to therapy, and general well-being.
The goal of patient education has been defined as to support the empowerment and self-care of patients and must therefore meet their own knowledge expectations,2 that is, the knowledge they expect to acquire in relation to their health care. Knowledge is acquired through processing and retaining information that should address biophysiological, functional, experiential, ethical, social, and financial issues.3 The patient education process should start by assessing what the learner needs to know.4 However, it is common in practice that the learning needs of patients are not self-defined but mainly determined by health care professionals. Patients undergoing treatment in hospitals have been found to have high knowledge expectations. These are highest not only for the issues related to their disease and treatment and how it affects their daily activities but also for experiential, social, and financial issues, and those expectations are insufficiently fulfilled, although to a varying extent.2,5–7
One of the most prevalent chronic medical conditions worldwide is heart failure, a serious and common condition that affects around 1%–2% of the population of Western countries.8 Most heart failure patients need to engage in a complex, disease-specific self-care,9 consisting of maintenance, monitoring, and management.10,11 Even with optimal self-care, patients with heart failure are known to suffer from several health complaints they may have as a consequence of their disease, treatment, or other comorbidities. Heart failure has been shown to affect all dimensions of quality of life in patients, but problems with their usual physical functioning,12 fatigue, anxiety and depression,13 pain,14 and sexual problems15,16 are among their most common health complaints.
To reduce mortality and morbidity and increase quality of life in heart failure patients, pacemaker cardiac resynchronization therapy (CRT), with (CRT-D) or without (CRT-P) a defibrillating function, is being increasingly used.17 After CRT device implantation, additional self-care is expected of patients, such as monitoring complications, performing exercises to prevent shoulder stiffness, and wound care.18 This requires new knowledge and self-care skills, and sometimes, adjustment of daily activities in order to reach optimal recovery and accustomization to the device.
At first glance, CRT implantation might seem a rather simple surgical procedure but receiving the device may be a stressful experience for patients, especially for those with CRT-D devices who expect and may experience defibrillating shocks.19 They have been found to suffer from psychological distress, depressive symptoms, and impaired quality of life, even though they experience physical improvement.20 The Heart Failure Association of the European Society of Cardiology has recently urged policy makers to improve education and support for heart failure patients and their families.21 Implantation of a device increases educational needs even further, and emerging evidence suggests that education and psychosocial support play a fundamental part in patients’ adjustment to cardiac devices.19,22,23 Individualized education, which starts with the assessment of learning needs, delivered in multiple doses and the use of multiple media is recommended for both heart failure patients24,25 and surgical patients.26,27 However, content analysis of all written educational material for recipients of implantable cardioverter defibrillators in Sweden has revealed that biophysical content dominates the material while other relevant contents are scarce or nonexistent.28 It is therefore timely to involve patients more, both individually and on a general level, when targeted patient education is being developed for special patient populations. Research is still lacking on the knowledge expectations of heart failure patients undergoing CRT treatment, and little is known about their self-care behavior or health complaints before the implantation and if those factors affect patients’ knowledge expectations.
Aims
The aims of this study were 1) to describe what knowledge heart failure patients expect to receive before undergoing CRT implantation, 2) to describe their self-care and health complaints, and 3) to explore the relationship between knowledge expectations and self-care, health complaints, and background factors.
Materials and methods
Design
This was a multicenter, cross-sectional survey study, and data were collected with self-reported questionnaires in 2012–2014.
Participants
All consecutive heart failure patients scheduled for an elective, first-time CRT device implantation in five Swedish and one Icelandic hospital were eligible for the study. The institutions included four university hospitals and two regional hospitals. Patients were included if they were aged 18 or older, able to understand Swedish/Icelandic, and had no cognitive impairment diagnosed and documented in their medical records. Patients were excluded if they had received an upgrade of any type of cardiac devices.
Measurements
Four previously validated instruments were used for data collection. Knowledge expectations were measured with the Knowledge Expectations of hospital patients (KEhp) Scale, which consists of 40 items, each preceded with “I expect knowledge on…”. The instrument is divided into six subscales of empowering knowledge, ie, biophysiological (eg, on disease, treatment, possible complications), functional (eg, on daily activities such as diet, rest, mobility, hygiene), experiential (eg, emotions, previous hospital experience), ethical (rights and duties of patients and health care providers), social (available support), and financial (costs of treatment and rights in social security system). Responses are ranked on a four-point Likert Scale (1= fully disagree, 4= fully agree, and 0= not applicable). Patient expectations are the average score for the total scale and subscales of the instrument with the possible range of 1–4. Lower scores reflect lower knowledge expectations. The KEhp instrument has previously been tested and its content validated.2,3 Self-care was measured with the nine-item European Heart Failure Self-care Behavior Scale, a validated instrument developed to measure the behaviors that heart failure patients engage in to maintain life, healthy functioning, and well-being.29 The items are rated on a five-point Likert Scale (1= fully agree, 5= fully disagree). Possible scores are 9–45 and scores can be standardized to 0–100, after which higher scores indicate better self-care.30 Health complaints were measured with items derived and adapted from the Postoperative Recovery Profile (PRP).31 Each item in this 19-item instrument has four response options: severe (=1), moderate, mild, and none (=4). Health complaints are the average score for the total scale of the instrument with a possible range of 1–4 (possible scores 19–76). Lower scores reflect more serious problems. The number of health complaints was calculated by totaling the health complaints (ie, score 1–3) with a possible count of 0–19.
Demographic and background data were collected with specific questions in the questionnaire, ie, on education, employment, living arrangements (living alone, with others, or in a nursing home), previous work experience with health care or social services, and from where patients had received information about their prospective CRT treatment. Data on New York Heart Association Functional Classification class, medication, and comorbidities were collected from hospital records.
Procedure
All consecutive heart failure patients scheduled for an elective CRT device implantation were screened for eligibility by research nurses in each of the centers according to the inclusion criteria. Patients who met the criteria were sent an information letter, a consent form, a reply form, and the questionnaire within a month of the scheduled procedure. Patients who wanted to join the study filled out the questionnaire and the consent form. The information package included a stamped, addressed envelope, and all patients were asked to use this to send the required documents to the researchers before the CRT implantation.
Data analysis
Descriptive statistics (mean [standard deviation] and median [interquartile range]), frequencies, and proportions (%) were used to describe the sample characteristics, as well as knowledge expectations, self-care, and health complaints. Background variables on education and employment were collected and were dichotomized into “low” (=basic education ≤9 years) and “high” (=college and academic education) education, “retired” and “employed” (employed and other), and “living alone” and “living with others” for further analysis.
Variables of the total scale and the six subscales of KEhp were computed (possible scores 1–4) and then further dichotomized into “low” and “high” expectations with the median value as a cut-off point as the data were not normally distributed. A total scale of health complaints (adjusted PRP) was computed (possible scores 1–4) and then further dichotomized into “no complaints” (score 4) and “health complaints” (scores 1–3) to assess the difference between those who had and those who did not have health complaints.
Nonparametric tests (Mann–Whitney U-test, chi-square test, and Fisher’s exact test) were used, as appropriate for nonnormally distributed data, to assess the difference between high and low knowledge expectations and background factors, self-care, and health complaints. A binary logistic regression analysis with enter method was performed to assess the association between high or low knowledge expectations and univariate significantly related factors. A P-value of <0.10 was required to enter a variable into a multivariate model. In all other tests, the level of statistical significance was set at <0.05. The software package IBM SPSS-21 statistics was used for analysis (IBM Corporation, Armonk, NY, USA).
Ethical approval
The study conforms to the Declaration of Helsinki.32 The study was approved by the relevant ethical committees in each country (Sweden Dnr 2012/120-31, Iceland 12-029-S1). Patients were informed in writing of the purpose of the study and the principles of informed consent, confidentiality, and their right to withdraw from the study at any point.
Results
Sample
Of 175 eligible patients, 104 accepted the invitation to participate in the study (59% response rate). The nonrespondents had a mean age of 72 (±9.3) years and 27% were women.
The mean age of patients was 70 years (±10) and ranged from 41 years to 90 years (Table 1), with 21% being women. In total, 56% of the patients had college education or higher, 72% were retired, and 79% lived with a spouse or other person, thereof one in a nursing home. Hypertension (47%), a previous myocardial infarction (38%), and diabetes mellitus (23%) were the most common comorbidities. Patients were prescribed an average of 8.6 (±4.0) different medications. Most patients reported having received information about the CRT treatment from physicians or nurses at an outpatient cardiac clinic (79%) and/or from brochures (49%), Internet (18%), family or friends (8%), and patient organizations (1%). The characteristics of the sample, including comparison between those who had high and low knowledge expectations are described in Table 1.
Table 1.
Characteristics of the total sample (N=104) and comparison between patients with low and high knowledge expectations
| Total sample (N=104) | Low knowledge expectations (n=51) | High knowledge expectations (n=53) | Pa | |
|---|---|---|---|---|
| Age in years (mean ± standard deviation) | 70 (10) | 67 (10) | 72 (8) | 0.029 |
| N (%) | N (%) | N (%) | Pb | |
| Sex (n=104) | ||||
| Male | 82 (79) | 39 (76) | 43 (81) | 0.366 |
| Education (n=102) | ||||
| Basic education (≤9 years) | 45 (44) | 19 (37) | 26 (49) | 0.382 |
| College level | 29 (28) | 13 (25) | 16 (30) | |
| Academic degree | 27 (27) | 17 (33) | 10 (19) | |
| Other | 1 (1) | 1 (2) | 0 (0) | |
| Employment status (n=104) | ||||
| Employed | 21 (20) | 13 (25) | 8 (15) | 0.433 |
| Retired | 75 (72) | 34 (67) | 41 (77) | |
| Other | 8 (8) | 4 (8) | 4 (8) | |
| History of employment within health care (n=99) | 18 (18) | 9 (18) | 9 (17) | 0.546 |
| Living with a spouse/other person (n=102) | 81 (79) | 38 (75) | 43 (81) | 0.452 |
| NYHA functional classification (n=88) | ||||
| Class I | 5 (6) | 3 (6) | 2 (4) | 0.378 |
| Class II | 35 (40) | 21 (41) | 14 (26) | |
| Class III | 47 (53) | 21 (41) | 26 (49) | |
| Class IV | 1 (1) | 0 (0) | 1 (2) | |
| Comorbidities (n=102) | ||||
| Hypertension | 48 (47) | 24 (47) | 24 (45) | 0.430 |
| Myocardial infarction | 39 (38) | 20 (39) | 19 (36) | 0.377 |
| Diabetes mellitus | 23 (23) | 10 (20) | 13 (25) | 0.398 |
| Chronic kidney disease | 15 (15) | 7 (14) | 8 (15) | 0.566 |
| Chronic obstructive pulmonary disease | 11 (11) | 4 (8) | 7 (13) | 0.310 |
| Medication (n=99) | ||||
| Beta-blockers | 92 (93) | 44 (86) | 48 (91) | 0.596 |
| Diuretics | 82 (83) | 38 (75) | 44 (83) | 0.409 |
| Statins | 60 (61) | 24 (47) | 36 (68) | 0.050 |
| Angiotensin-converting enzyme inhibitors | 54 (55) | 24 (47) | 31 (58) | 0.257 |
| Antiplatelets | 49 (50) | 21 (41) | 28 (53) | 0.239 |
| Anticoagulants | 44 (44) | 19 (37) | 24 (45) | 0.356 |
| Angiotensin II receptor blockers | 40 (40) | 21 (41) | 18 (34) | 0.207 |
| Vasodilators | 32 (32) | 13 (25) | 18 (34) | 0.299 |
| Digitalis | 19 (19) | 7 (14) | 12 (23) | 0.219 |
Notes:
Mann–Whitney U-test.
Chi-square test (Fisher’s exact test).
Abbreviation: NYHA, New York Heart Association.
Knowledge expectations
The knowledge expectations of patients are presented in Table 2. The median (interquartile range) score of the KEhp total scale was 3.68 (0.5), and patients expected to receive most knowledge within the biophysiological dimension and the least knowledge within the social dimension.
Table 2.
Expected knowledge of patients undergoing CRT implantation (N=104)
| KEhp scale median (IQR) | Highest expectations–top three items per subscale | % of patients who fully agree | |
|---|---|---|---|
| Total scale | 3.68 (0.50) | ||
| Knowledge dimensions | “I expect knowledge on…” | ||
| Biophysiological | 4.00 (0.13) | Possible complications | 91 |
| Examinations which will be performed | 89 | ||
| How I can help to prevent complications | 89 | ||
| Functional | 3.88 (0.38) | When I can wash/shower/sauna | 89 |
| What I can do myself to meet personal needs | 85 | ||
| Physical exercise which I can do | 84 | ||
| Experiential | 3.67 (1.00) | Feelings illness and its treatment may cause | 63 |
| Who I can talk with about those feelings | 59 | ||
| How I can use earlier hospital experience in current care | 57 | ||
| Financial | 3.67 (1.00) | Medication cost | 68 |
| Costs of further care or treatment provided at home | 65 | ||
| Rehabilitation and adaptation training courses and their costs | 62 | ||
| Ethical | 3.57 (0.50) | Own responsibility for the success of care | 80 |
| How I can take part in decision-making about own care | 77 | ||
| Rights in the hospital | 75 | ||
| Social | 3.50 (0.83) | Where to get further care or treatment if needed | 79 |
| Who informs next of kin about patient’s illness and treatment | 71 | ||
| How next of kin can take part in care | 60 |
Notes: Scores range between 1 and 4; high scores indicate high expectations.
Abbreviations: CRT, cardiac resynchronization therapy; KEhp, Knowledge Expectations of hospital patients; IQR, interquartile range.
Patients found most items relevant for them to learn about, although some support issues were not found to be so applicable; such as information about sickness benefits (38%), the hospital priest (34%), insurance (23%), how to obtain aid needed for own care (22%), and available support from patient organizations (19%) (not tabulated). The highest knowledge expectations of patients in the different subscales concerned possible complications of the treatment (91%), when they could wash or shower (89%), their own responsibility for the success of their care (80%), where to get further care or treatment (79%), medication costs (68%), and what feelings the treatment could cause (63%).
Self-care behavior and health complaints
The mean score of self-care measured with the European Heart Failure Self-care Behavior Scale was 27.4 (±7.1), and after standardization 51.0 (±19.6). Of those patients who scored 1–2 on the scale, 100% reported taking their medications as prescribed, while 28% weigh themselves daily and 30% consult their doctor or nurse when experiencing deterioration in their condition, for example shortness of breath, increased swelling of legs, weight increase, or fatigue. Of other self-care activities, 52% of patients reported to limit their fluid intake, 40% to exercise regularly, and 36% limit their salt intake.
Patients had, on average, 8.2 health complaints (±4.7) with 87% reporting fatigue, 66% anxiety and worry, 64% muscle weakness, 64% difficulties with daily activities, and 55% problems with sexual activity. The most serious health complaints were fatigue (22% responded “severe”), sexual problems (21%), muscle weakness (9%), and problems with daily activities (9%) (Figure 1).
Figure 1.
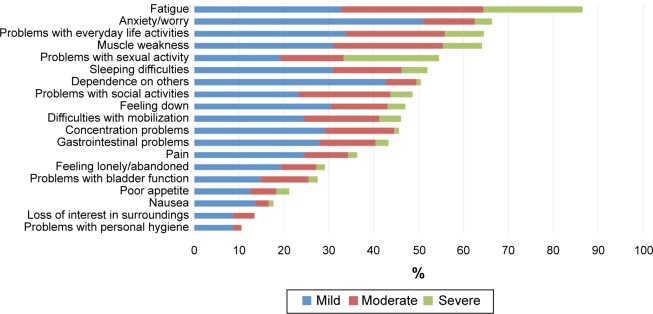
Health complaints (measured with the Adjusted Postoperative Recovery Profile) in CRT patients presented as a proportion (%) of the group (N=104) who had mild, moderate, or severe problems with each complaint.
Abbreviation: CRT, cardiac resynchronization therapy.
Relationship between knowledge expectations and background factors, self-care, and health complaints
Knowledge expectations were positively correlated with age, with older patients having higher expectations, both on the total scale (rs=0.203, P=0.012) and the social, financial, and experiential subscales (Table 3). No statistically significant relationship was found between knowledge expectations and other demographic and clinical factors, self-care behavior, or health complaints.
Table 3.
Correlation coefficients (Spearman) among knowledge expectations of CRT patients (N=104) and their age, self-care, and health complaints
| KEhp scale total | Knowledge dimensions (subscales)
|
||||||
|---|---|---|---|---|---|---|---|
| Biophysiological | Functional | Experiential | Ethical | Social | Financial | ||
| Age rs | 0.203* | 0.162 | 0.102 | 0.281* | 0.233* | 0.253* | 0.248* |
| Self-carea rs | 0.083 | 0.150 | 0.165 | 0.185 | 0.091 | −0.048 | −0.001 |
| Health complaintsb rs | −0.047 | −0.002 | −0.095 | −0.155 | −0.011 | −0.020 | −0.048 |
Notes:
P<0.05.
European Heart Failure Self-care Behavior Scale.
Health complaints: Adjusted Postoperative Recovery Profile (Scale).
Abbreviations: CRT, cardiac resynchronization therapy; KEhp, Knowledge Expectations of hospital patients.
Patients with high knowledge expectations had more health complaints than patients with low knowledge expectations, with ratings of 9 (±5.0) vs 7 (±4.2), although this difference was not statistically significant (P=0.091).
Age and health complaints were entered as independent variables into a binary logistic regression analysis as they were the only variables that fulfilled the inclusion criteria of P<0.10. The model was statistically significant, χ2(2)=9.826, P<0.05, and explained 12.0% (Nagelkerke R2) of the variance in high or low knowledge expectations and correctly classified 64.4% of cases. Only increasing age was independently associated with an increased likelihood of having high knowledge expectations (Table 4).
Table 4.
The results of binary logistic regression analysis of the contribution of age and health complaints to high or low knowledge expectations (95% confidence intervals for odds ratio)
| β (SE) | Lower | Odds ratio | Upper | P | |
|---|---|---|---|---|---|
| Constant | −0.860 (2.250) | 0.423 | 0.702 | ||
| Age | 0.049 (0.023) | 1.004 | 1.050 | 1.098 | 0.033 |
| Health complaints | −0.757 (0.425) | 0.204 | 0.469 | 1.079 | 0.075 |
Notes: R2=0.374 (Hosmer and Lemeshow), 0.090 (Cox and Snell), 0.0120 (Nagelkerke). Model χ2(2)=9.726, P<0.05.
Abbreviation: SE, standard error.
Discussion
This is the first study that describes what knowledge the heart failure patients waiting for CRT implantation expect and need in relation to the upcoming procedure. Although several studies have previously addressed the psychosocial impact of device implantation and the content of educational material and have found that patients need better education,23,28 they have not actually described the knowledge expectations of patients.
In general, the patients in this study had high knowledge expectations, and those with high expectations, both in general and specifically in relation to experiential, ethical, social, and financial issues, were older than those with low expectations. This information can help to improve and tailor education that meets the patients’ needs.
Patients expected that most knowledge they would acquire would be related to their illness, symptoms, treatment, and possible complications, and how these could affect their daily functions and activities. They had reduced knowledge expectations on experiential, financial, and ethical issues and least on available social support and how the family could contribute to their care. This ranking of expectations is similar to previous studies on knowledge expectations in different surgical patient populations, for example, ambulatory orthopedic surgery patients,5 arthroplasty patients,33 breast cancer patients,34 and a mixed group of surgical patients.2 These similarities indicate, as stated before, that although CRT implantation may seem a rather simple procedure that requires short hospitalization, patients do have high expectations about the information they will receive in common with other surgical patients, regardless of the nature of the procedure.
Theories of adult learning emphasize that adults want to learn what is relevant to them in their current situation35 and before a hospital procedure patients may indeed be prioritizing their needs according to relevance. The upcoming procedure and its effect on daily life may be experienced as very urgent to deal with before the procedure, while social and financial issues become more important postoperatively. Also, heart failure patients scheduled for CRT implantation are likely to have lived with their chronic illness for a long time and they may already have quite good knowledge of available social and financial support resources.
This study shows that around 90% of patients undergoing CRT implantation expect to receive information on possible complications of the treatment and how they themselves can help to prevent those complications. This reflects an interest and willingness of patients to be actively involved in their self-care. However, providing risk information is a sensitive issue and raises an ethical challenge for health care providers. Guided by their ethical principles of respect for autonomy, beneficence, and nonmaleficence,36 they are expected to provide patients with appropriate and sufficient information in order to support their empowerment and self-care, but simultaneously they must avoid distressing the patients. However, previous studies have shown that patients want information on the risks of complications. In a sample of cardiac surgery patients, around 70% wanted information about both common and rare complications37 and expressed dissatisfaction about not receiving such information. When complications arose, some thought they were caused by maltreatment.38 This issue is relevant for patients receiving CRT devices. Although complications are rare and seldom of major severity, a recent study in a Danish cohort of cardiac implantable electronic device recipients revealed that a total of 9.5% of patients experienced at least one complication, and among those at a higher risk were those receiving CRT-D devices.39 Age was found to be independently related to knowledge expectations in our study and older patients had more knowledge expectations than the younger patients. This is in line with both Rankinen et al2 and Heikkinen et al5 who found similar differences. Older patients may need more social support and have different financial concerns than those who are younger. While the CRT treatment is likely to improve their quality of life and life expectancy, the older patients may find the ethical and experiential issues more relevant as their end of life approaches. No other individual background variables than age explained the profile of patients with high and low expectations in the current study. Another plausible explanation, on system level, could be variations between centers or the two countries. However, the Icelandic sample constituted only 4% of the total sample, and as the Swedish and Icelandic health care systems are both rooted in the Nordic model of the welfare state,40 the Icelandic cardiac care is modeled from Sweden and all participating centers are similar public hospitals, other explaining variables need to be identified in future studies.
The patients who participated in this study had many health complaints, or an average of eight out of the 19 they were asked about, and patients with high knowledge expectations had more complaints and more severe ones than those with low expectations. The most common and most severe complaint was fatigue, which was to be expected in this population of heart failure patients. Of more interest was problems with sexual activities, but this was the second most severe complaint (21% had severe problems) and the fifth most common one, with 55% of patients affected. Sexual problems are common in heart failure patients but are insufficiently addressed by health care professionals,41 although there is an emerging awareness of their importance and a call for improved health care services through sexual counselling.42
The self-care behavior of patients in this sample was similar to what has been reported previously,30,43 and we found no difference in self-care behavior according to knowledge expectations. However, from the knowledge expectation scale, it seemed that most patients wanted to learn about self-care maintenance, monitoring, and management in relation to their device implantation, such as how to prevent complications, attend to activities of daily living, monitor symptoms, and seek assistance after hospitalization. This can guide clinicians in their education of the patient. It also indicates the importance of identifying patients with low self-care behavior before the CRT procedure, because they may need additional support postimplantation in order to maintain or improve both their device-related self-care and heart failure-related self-care.
The study has several limitations. The Knowledge Expectations of hospital patient Scale has previously been validated but has not been used before with heart failure patients undergoing CRT implantation. However, it has been used successfully in an ambulatory surgical patient population5 who also had minimally invasive procedures. The adjusted PRP scale consists of 19 items or health complaints; it is possible that patients in this study had other health complaints that were not included in that list. Another limitation is that the European Heart Failure Self-care Behavior Scale is a generic instrument and not specific to CRT patients, which may have impacted the results of the relationship between self-care and knowledge expectations. Also, patients answered the questionnaire before hospital admission but we could not control how much, or what specific information they had received before participating in the study. In addition, measuring the knowledge patients had beforehand and comparing it with their knowledge expectations might have added valuable data to this study.
Conclusion
Heart failure patients expect to receive a wide range of knowledge before their CRT device implantation and their expectations are related to their age. They also had similar knowledge expectations to those of other populations of surgical patients. Patients had a lot of health complaints and their self-care behavior was average. More research is needed to determine the profile of persons who have high or low knowledge expectations.
Acknowledgments
We acknowledge the assistance of the following people: Elisabeth Wilhelm, statistician at the Department of Medical and Health Sciences, Linköping University, Sweden; the nurses at the participating hospitals for assistance with data collection; Anneli U. Hermansson, research nurse, for coordinating the study; and Professor Arun K. Sigurdardottir, University of Akureyri, Iceland. We also acknowledge the financial support from the Landspitali University Hospital Research Fund, Landspitali–The National University Hospital of Iceland; the Icelandic Nurses’ Association Research Fund and Research Fund of Ingibjörg Magnúsdóttir in Iceland; and Medtronic-Vingmed AB and St. Jude Medical Sweden AB in Sweden.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.World Health Organisation World Health Organization’s Chronic Diseases and Health Promotion Program. 2015. [Accessed March 30, 2015]. Available from: http://www.who.int/chp/topics/en/
- 2.Rankinen S, Salanterä S, Heikkinen K, et al. Expectations and received knowledge by surgical patients. Int J Qual Health Care. 2007;19(2):113–119. doi: 10.1093/intqhc/mzl075. [DOI] [PubMed] [Google Scholar]
- 3.Leino-Kilpi H, Johansson K, Heikkinen K, Kaljonen A, Virtanen H, Salantera S. Patient education and health-related quality of life: surgical hospital patients as a case in point. J Nurs Care Qual. 2005;20(4):307–316. doi: 10.1097/00001786-200510000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Redman BK. The Practice of Patient Education: A Case Study Approach. St. Lois: Mosby Inc; 2007. [Google Scholar]
- 5.Heikkinen K, Leino-Kilpi H, Hiltunen A, et al. Ambulatory orthopaedic surgery patients’ knowledge expectations and perceptions of received knowledge. J Adv Nurs. 2007;60(3):270–278. doi: 10.1111/j.1365-2648.2007.04408.x. [DOI] [PubMed] [Google Scholar]
- 6.Ingadottir B, Johansson Stark A, Leino-Kilpi H, Sigurdardottir AK, Valkeapaa K, Unosson M. The fulfilment of knowledge expectations during the perioperative period of patients undergoing knee arthroplasty – a Nordic perspective. J Clin Nurs. 2014;23(19–20):2896–2908. doi: 10.1111/jocn.12552. [DOI] [PubMed] [Google Scholar]
- 7.Johansson Stark A, Ingadottir B, Salanterä S, et al. Fulfilment of knowledge expectations and emotional state among people undergoing hip replacement: a multi-national survey. Int J Nurs Stud. 2014;51(11):1491–1499. doi: 10.1016/j.ijnurstu.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 8.Ponikowski P, Anker S, AlHabib K, et al. Heart failure: preventing disease and death worldwide. ESC Heart Failure. 2014;1(1):4–25. doi: 10.1002/ehf2.12005. [DOI] [PubMed] [Google Scholar]
- 9.McMurray JJ, Adamopoulos S, Anker SD, et al. ESC Committee for Practice Guidelines ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2012;14:803–869. doi: 10.1093/eurjhf/hfs105. [DOI] [PubMed] [Google Scholar]
- 10.Riegel B, Jaarsma T, Stromberg A. A middle-range theory of self-care of chronic illness. ANS Adv Nurs Sci. 2012;35:194–204. doi: 10.1097/ANS.0b013e318261b1ba. [DOI] [PubMed] [Google Scholar]
- 11.Lee CS, Mudd JO, Hiatt SO, Gelow JM, Chien C, Riegel B. Trajectories of heart failure self-care management and changes in quality of life. Eur J Cardiovasc Nurs. 2014 Jun 30; doi: 10.1177/1474515114541730. Epub. [DOI] [PubMed] [Google Scholar]
- 12.Cleland JG, Calvert MJ, Verboven Y, Freemantle N. Effects of cardiac resynchronization therapy on long-term quality of life: an analysis from the CArdiac Resynchronisation-Heart Failure (CARE-HF) study. Am Heart J. 2009;157(3):457–466. doi: 10.1016/j.ahj.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 13.Dekker RL, Lennie TA, Doering LV, Chung ML, Wu JR, Moser DK. Coexisting anxiety and depressive symptoms in patients with heart failure. Eur J Cardiovasc Nurs. 2014;13(2):168–176. doi: 10.1177/1474515113519520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Godfrey CM, Harrison MB, Friedberg E, Medves JM, Tranmer JE. The symptom of pain in individuals recently hospitalized for heart failure. J Cardiovasc Nurs. 2007;22(5):368–374. doi: 10.1097/01.JCN.0000287035.77444.d9. discussion 366–367. [DOI] [PubMed] [Google Scholar]
- 15.Jaarsma T, Fridlund B, Martensson J. Sexual dysfunction in heart failure patients. Curr Heart Fail Rep. 2014;11(3):330–336. doi: 10.1007/s11897-014-0202-z. [DOI] [PubMed] [Google Scholar]
- 16.Berg SK, Elleman-Jensen L, Zwisler AD, et al. Sexual concerns and practices after ICD implantation: findings of the COPE-ICD rehabilitation trial. Eur J Cardiovasc Nurs. 2013;12(5):468–474. doi: 10.1177/1474515112473528. [DOI] [PubMed] [Google Scholar]
- 17.Yu CM, Hayes DL. Cardiac resynchronization therapy: state of the art 2013. Eur Heart J. 2013;34(19):1396–1403. doi: 10.1093/eurheartj/ehs454. [DOI] [PubMed] [Google Scholar]
- 18.Saul L. Cardiac resynchronization therapy. Crit Care Nurs Q. 2007;30(1):58–66. doi: 10.1097/00002727-200701000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Padeletti L, Mascioli G, Perini AP, et al. Critical appraisal of cardiac implantable electronic devices: complications and management. Med Devices (Auckl) 2011;4:157–167. doi: 10.2147/MDER.S15059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Knackstedt C, Arndt M, Mischke K, et al. Depression, psychological distress, and quality of life in patients with cardioverter defibrillator with or without cardiac resynchronization therapy. Heart Vessels. 2014;29(3):364–374. doi: 10.1007/s00380-013-0372-8. [DOI] [PubMed] [Google Scholar]
- 21.Cowie M, Anker S, Cleland J, et al. Improving Care for Patients with Acute Heart Failure Before, During and After Hospitalisation. Oxford: Oxford PharmaGenesis; 2014. [DOI] [PubMed] [Google Scholar]
- 22.Morken IM, Bru E, Norekval TM, Larsen AI, Idsoe T, Karlsen B. Perceived support from healthcare professionals, shock anxiety and post-traumatic stress in implantable cardioverter defibrillator recipients. J Clin Nurs. 2014;23(3–4):450–460. doi: 10.1111/jocn.12200. [DOI] [PubMed] [Google Scholar]
- 23.Dunbar SB, Dougherty CM, Sears SF, et al. American Heart Association Council on Cardiovascular Nursing, Council on Clinical Cardiology, and Council on Cardiovascular Disease in the Young Educational and psychological interventions to improve outcomes for recipients of implantable cardioverter defibrillators and their families: a scientific statement from the American Heart Association. Circulation. 2012;126(17):2146–2172. doi: 10.1161/CIR.0b013e31825d59fd. [DOI] [PubMed] [Google Scholar]
- 24.Fredericks S, Beanlands H, Spalding K, Da Silva M. Effects of the characteristics of teaching on the outcomes of heart failure patient education interventions: a systematic review. Eur J Cardiovasc Nurs. 2010;9(1):30–37. doi: 10.1016/j.ejcnurse.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 25.Boyde M, Song S, Peters R, Turner C, Thompson DR, Stewart S. Pilot testing of a self-care education intervention for patients with heart failure. Eur J Cardiovasc Nurs. 2013;12(1):39–46. doi: 10.1177/1474515111430881. [DOI] [PubMed] [Google Scholar]
- 26.Fredericks S, Guruge S, Sidani S, Wan T. Postoperative patient education: a systematic review. Clin Nurs Res. 2010;19(2):144–164. doi: 10.1177/1054773810365994. [DOI] [PubMed] [Google Scholar]
- 27.Veronovici NR, Lasiuk GC, Rempel GR, Norris CM. Discharge education to promote self-management following cardiovascular surgery: an integrative review. Eur J Cardiovasc Nurs. 2014;13(1):22–31. doi: 10.1177/1474515113504863. [DOI] [PubMed] [Google Scholar]
- 28.Bolse K, Johansson I, Stromberg A. Organisation of care for Swedish patients with an implantable cardioverter defibrillator, a national survey. J Clin Nurs. 2011;20(17–18):2600–2608. doi: 10.1111/j.1365-2702.2010.03540.x. [DOI] [PubMed] [Google Scholar]
- 29.Jaarsma T, Årestedt KF, Mårtensson J, Dracup K, Strömberg A. The European Heart Failure Self-care Behaviour Scale revised into a nine-item scale (EHFScB-9): a reliable and valid international instrument. Eur J Heart Fail. 2009;11(1):99–105. doi: 10.1093/eurjhf/hfn007. [DOI] [PubMed] [Google Scholar]
- 30.Vellone E, Jaarsma T, Strömberg A, et al. The European Heart Failure Self-care Behaviour Scale: new insights into factorial structure, reliability, precision and scoring procedure. Patient Educ Couns. 2014;94(1):97–102. doi: 10.1016/j.pec.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 31.Allvin R, Ehnfors M, Rawal N, Svensson E, Idvall E. Development of a questionnaire to measure patient-reported postoperative recovery: content validity and intra-patient reliability. J Eval Clin Pract. 2009;15(3):411–419. doi: 10.1111/j.1365-2753.2008.01027.x. [DOI] [PubMed] [Google Scholar]
- 32.World Medical Association World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 33.Valkeapää K, Klemetti S, Cabrera E, et al. Knowledge expectations of surgical orthopaedic patients: a European survey. Int J Nurs Pract. 2014;20(6):597–607. doi: 10.1111/ijn.12189. [DOI] [PubMed] [Google Scholar]
- 34.Ryhanen AM, Rankinen S, Siekkinen M, Saarinen M, Korvenranta H, Leino-Kilpi H. The impact of an empowering internet-based breast cancer patient pathway programme on breast cancer patients’ knowledge: a randomised control trial. Patient Educ Couns. 2012;88(2):224–231. doi: 10.1016/j.pec.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 35.Merriam SB, Caffarella RS, Baumgartner LM. Learning in Adulthood: A Comprehensive Guide. 3 ed. San Francisco, Calif: Jossey-Bass; 2007. A Wiley Imprint. [Google Scholar]
- 36.Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 6th ed. New York: Oxford University Press; 2009. [Google Scholar]
- 37.Ivarsson B, Larsson S, Luhrs C, Sjoberg T. Extended written preoperative information about possible complications at cardiac surgery–do the patients want to know? Eur J Cardiothorac Surg. 2005;28(3):407–414. doi: 10.1016/j.ejcts.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 38.Ivarsson B, Larsson S, Luhrs C, Sjoberg T. Patients perceptions of information about risks at cardiac surgery. Patient Educ Couns. 2007;67(1–2):32–38. doi: 10.1016/j.pec.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 39.Kirkfeldt RE, Johansen JB, Nohr EA, Jorgensen OD, Nielsen JC. Complications after cardiac implantable electronic device implantations: an analysis of a complete, nationwide cohort in Denmark. Eur Heart J. 2014;35(18):1186–1194. doi: 10.1093/eurheartj/eht511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Magnussen J, Vrangbaek K, Saltman RB, editors. Nordic Health Care Systems: Recent Reforms and Current Policy Challenges. Berkshire: Open University Press; 2009. [Google Scholar]
- 41.Schwarz ER, Kapur V, Bionat S, Rastogi S, Gupta R, Rosanio S. The prevalence and clinical relevance of sexual dysfunction in women and men with chronic heart failure. Int J Impot Res. 2008;20(1):85–91. doi: 10.1038/sj.ijir.3901613. [DOI] [PubMed] [Google Scholar]
- 42.Steinke EE, Jaarsma T, Barnason SA, et al. Council on Cardiovascular and Stroke Nursing of the American Heart Association and the ESC Council on Cardiovascular Nursing and Allied Professions (CCNAP) Sexual counseling for individuals with cardiovascular disease and their partners: a consensus document from the American Heart Association and the ESC Council on Cardiovascular Nursing and Allied Professions (CCNAP) Eur Heart J. 2013;34(41):3217–3235. doi: 10.1093/eurheartj/eht270. [DOI] [PubMed] [Google Scholar]
- 43.Jaarsma T, Strömberg A, Ben Gal T, et al. Comparison of self-care behaviors of heart failure patients in 15 countries worldwide. Patient Educ Couns. 2013;92(1):114–120. doi: 10.1016/j.pec.2013.02.017. [DOI] [PubMed] [Google Scholar]


