Abstract
OBJECTIVE
To estimate the effects of obesity on the duration and progression of the first stage of labor in a predominantly obese population and estimate the dose–effect with increasing classes of obesity.
METHODS
We performed a retrospective cohort study of labor progression among 5,204 consecutive parturients with singleton term pregnancies (37 weeks of gestation or more) and vertex presentation who completed the first stage of labor. Two comparison groups were defined by body mass index (BMI) less than 30 (n=2,413) or 30 or more (n=2,791). Repeated-measures analysis with polynomial modeling was used to construct labor curves. The duration and progression among women with BMIs less than 30 and BMIs of 30 or more were compared in a multivariable interval-censored regression model adjusting for parity, type of labor onset, race, and birth weight more than 4,000 g.
RESULTS
The labor curves indicate longer duration and slower progression of the first stage of labor among women with BMIs of 30 or more for both nulliparous and multiparous women. Multivariable interval-censored regression analysis confirmed significantly longer duration (4–10 cm: 4.7 compared with 4.1 hours, P<.01) and slower progression of cervical dilation from 4 to 6 cm (2.2 compared with 1.9 hours, P<.01 with a range of 0.5–10.0 hours) among women with BMIs of 30 or more after adjusting for confounders.
CONCLUSION
The overall duration is longer and progression of the early part of the first stage of labor is slower in obese women. This suggests that obesity should be considered in defining norms for management of labor, particularly in the early part of the first stage.
In the United States, the increasing number of cesarean deliveries performed is expected to have a great public health effect. The potential complications and morbidity associated with cesarean deliveries disproportionately affect obese women.1–3 Obese women have a higher rate of wound infections, wound separation, dehiscence, anesthetic complications, thrombosis, and surgical tissue injury associated with cesarean deliveries.2,4,5 In addition, many studies have identified maternal obesity as an independent risk factor for cesarean delivery.5–7 Therefore, it is prudent to re-examine our indications for cesarean deliveries, especially as it relates to the obese population.
Although there are many cited reasons for indicated cesarean delivery, one commonly used indication is arrest of dilatation, also known by other terminologies such as failure to progress in labor and active-phase arrest.8 In daily practice, the Friedman curve of labor progression has been used to define what is normal and what is abnormal.9,10 Based on these standards, developed in the 1950s in a small homogenous population, women in labor have been measured by the same reference without regard to individual differences. As a result, many women are advised to undergo cesarean delivery at the time of labor arrest using a single definition despite individual differences. Recent publications have shown that perhaps the Friedman curve was neither perfectly accurate nor broadly applicable to all women, particularly to those who are obese.11–13 The effect of such findings, if confirmed, could give health care providers additional characteristics to consider before diagnosing first-stage arrest, potentially lowering the cesarean delivery rate and associated morbidity in at-risk populations.14 We sought to confirm these reports, by estimating the dose–response effects of obesity on the duration and progression of the first stage of labor, in a population with a high rate of obesity.
MATERIALS AND METHODS
We conducted a retrospective cohort study of all women with term pregnancies who completed the first stage of labor at Washington University Medical Center in St. Louis, Missouri, between July 2004 and June 2008. Before initiation of the study, approval was obtained from the Washington University human research protection board. Women who met inclusion criteria carried a singleton pregnancy in cephalic presentation and were at least 37 weeks 0 days of gestation on admission to labor and delivery. Exclusion criteria were women who delivered preterm, had fetuses with congenital anomalies, or delivered by cesarean before 10-cm dilation.
Detailed demographic information was extracted from the records including medical and surgical history, obstetrics and gynecology history, prenatal history, antepartum records, and labor and delivery records. The available information in labor and delivery records included medications, labor type, cervical examination times, dilation and station, length of labor stages, mode of delivery, and postpartum record. Cervical dilation was measured in centimeters, ranging from 0 to 10 cm. Weight and height were recorded based on patient report on admission to labor and delivery. Body mass index (BMI, calculated as weight (kg)/[height (m)]2) was calculated from data in the medical record. Obesity was defined as BMI 30 or greater according to the World Health Organization criteria.14 Pregnancies were dated by a woman's last menstrual period if that date was within 7 days of a first-trimester, 10 days of a second-trimester, or 21 days of a third-trimester ultrasonogram. Pregnancies were dated by ultrasonography if the last menstrual period was unknown or if the ultrasonographic dating was outside the aforementioned parameters.
Baseline characteristics were compared between the two study groups: BMI less than 30 and BMI 30 or greater. Continuous variables were compared using the Student's t test for all normally distributed data. Normality was tested using the Shapiro-Francia test.15 Categorical variables were compared using the χ2 test.
Additional analyses were performed, stratifying by parity as well as by BMI strata: less than 25, 25–29, 30–39, and 40 or greater. The Bonferroni correction was used for the multiple comparisons in the analysis, and the adjusted significance level was P<.01 for the data stratified by parity. The labor curve models were created using a repeated-measures regression with a polynomial function.16 The regression analysis was executed in a reverse approach; therefore, the starting point was set at the time a patient reached 10 cm dilation and then calculated backwards to 0 cm. A ninth-order polynomial in time was found to be the best fit for dilation values in the data set.
The primary outcome investigated was median time of cervical dilation from 4 cm to 10 cm as well as by increments of 2 cm (eg, 4–6 cm) and 1 cm (eg, 4–5 cm). We used interval-censored regression analysis because cervical dilation is not monitored in a continuous fashion, and therefore it is not possible to know exactly when the cervix changes from one interval to the next. We calculated the time interval between each consecutive cervical dilation for individual patients, giving them an interval-censored value for each level of dilatation. As previously described, labor data follow a log normal distribution, allowing us to estimate the mean, fifth, and 95th percentiles for time intervals.17,18 Multivariable models were then used to adjust for confounding factors identified by bivariate analysis. Only those variables that were statistically significant (P<.05) were used in the final models, which included parity, labor type, race, and birth weight greater than 4,000 g for the primary analysis. Statistical analyses were completed using the STATA 11.1 software package and PROC LIFEREG of SAS 9.2 to fit a log normal distribution to the time interval and estimated median, fifth, and 95th percentiles.
RESULTS
There were 5,388 consecutive term deliveries meeting inclusion during the study period; 5,204 women presented before complete dilation allowing the reconstruction of their first-stage labor curves and thus were included in this analysis. Of those, 53.6% (n=2,791) were obese, with BMIs of 30 or greater; 10.8% (n=563) had BMIs greater than 40. Obese women were older with higher gravidity and parity and were more likely to be of African American race. They also differed with respect to maternal comorbidities with obese women having higher rates of hypertension of pregnancy, diabetes, and gestational diabetes. The groups were similar in rates of tobacco and alcohol use as well as rates of prior cesarean delivery. The rates of spontaneous vaginal deliveries and cesarean deliveries, once the second stage of labor was reached, were similar between groups. However, operative vaginal delivery rates were lower among obese women (11.9% compared with 13.8%). The likelihood of the Bishop score being 5 or greater on admission was lower in obese women and the rate of induction compared with spontaneous labor was higher among women with BMIs of 30 or greater. Mean birth weight and incidence of neonatal weight more than 4,000 g were significantly higher in obese women (Table 1).
Table 1.
Baseline Characteristics of Obese and Nonobese Women
| BMI |
|||
|---|---|---|---|
| 30 or More (n=2,791) | Less Than 30 (n=2,413) | P | |
| Maternal age (y) | 24.8±5.7 | 23.8±6.0 | <.01 |
| Gravidity | 3.1 ±2.1 | 2.5±1.8 | <.01 |
| Nulliparous (n = 1,929) | 31.7 | 43.3 | <.01 |
| Prior cesarean delivery (n = 338) | 6.8 | 6.2 | .38 |
| Labor type | |||
| Induction (n = 1,604) | 36.5 | 24.2 | <.01 |
| Augmentation (n = 1,677) | 31.9 | 32.6 | .62 |
| Spontaneous (n = 1,923) | 31.5 | 43.2 | <.01 |
| Bishop score of 5 or more at admission (n = 1,924) | 31.9 | 43.5 | <.01 |
| African American race (n=3,840) | 76.8 | 70.2 | <.01 |
| Mode of delivery | |||
| Vaginal, spontaneous (n=4,453) | 86.4 | 84.6 | .07 |
| Vaginal, operative (n=666) | 11.9 | 13.8 | .04 |
| Cesarean (n = 85) | 1.7 | 1.5 | .60 |
| Tobacco use (n = 963) | 18.4 | 18.6 | .80 |
| Alcohol use (n = 84) | 1.4 | 1.8 | .27 |
| Hypertension of pregnancy (n=478) | 10.9 | 7.2 | <.01 |
| Diabetes mellitus (n = 178) | 4.7 | 2.0 | <.01 |
| Gestational diabetes (n = 147) | 3.8 | 1.7 | <.01 |
| Gestational age at delivery (wk) | 39.4±1.2 | 39.3±1.1 | <.01 |
| Birth weight (g) | 3,321±524 | 3,157± 519 | <.01 |
| Birth weight more than 4,000 g (n= 289) | 7.2 | 3.6 | <.01 |
BMI, body mass index.
Data are mean±standard deviation or % unless otherwise specified.
BMI is calculated as weight (kg)/[height (m)]2.
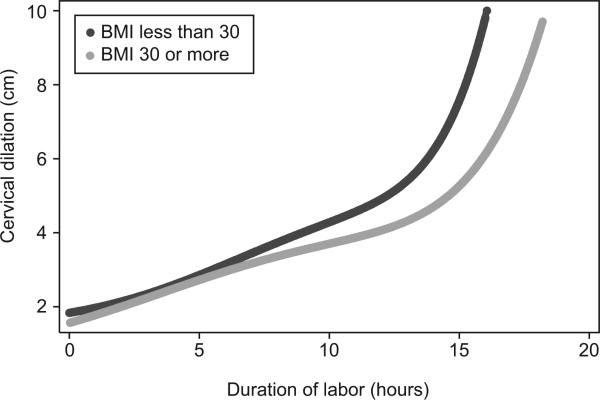
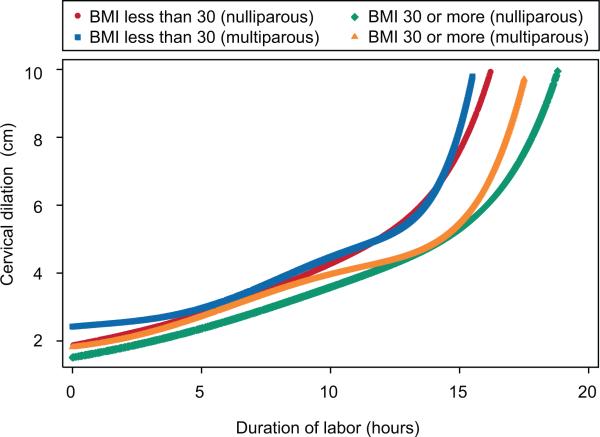
Obese women had longer duration and slower progression of the first stage of labor. Even after adjusting for parity, labor type, race, and birth weight greater than 4,000 g, duration of progress from 4 cm to complete cervical dilation took longer on average for women with BMIs of 30 or greater (4.7 compared with 4.1 hours, P<.01; Table 2). When analyzed in 2-cm intervals, the difference in the progression of dilation from 4 cm to 6 cm was the most pronounced (2.2 compared with 1.9 hours, P<.01). There was no difference for obese compared with nonobese women in the timing of cervical dilation from 6 cm to complete dilation. The labor curves for BMIs less than 30 and BMIs of 30 or greater showed a more gradual slope for obese women from 4 cm to 6 cm and then relatively similar slopes thereafter in the active phase of labor (Figs. 1 and 2). African American race was adjusted for given the differences seen in Table 1; however, data were not stratified by race given that previous data show no difference in timing of the first stage of labor.19
Table 2.
Median Duration of First Stage of Labor (4–10 cm) in Hours (5th, 95th Percentile) for Obese Compared With Nonobese Women and in Increments of 2 cm
| Cervical Dilation (cm) | BMI |
||
|---|---|---|---|
| 30 or More | Less Than 30 | P * | |
| n | 2,791 | 2,413 | |
| 4–10 | 4.7 (1.3, 16.4) | 4.1 (1.2, 14.3) | <.01 |
| 4–6 | 2.2 (0.5, 10.02) | 1.9 (0.4, 8.5) | <.01 |
| 6–8 | 0.5 (0.1, 4.4) | 0.5 (0.1, 4.2) | .49 |
| 8–10 | 0.3 (0.03, 2.5) | 0.3 (0.03, 2.4) | .46 |
BMI, body mass index.
BMI is calculated as weight (kg)/[height (m)]2.
Adjusted for parity, labor type, race, birth weight greater than 4,000 g.
Fig. 1.
Labor curve for obese compared with nonobese women. BMI, body mass index.
Norman. Effect of Obesity on the Labor Curve. Obstet Gynecol 2012.
Fig. 2.
Labor curve by obesity status and parity. BMI, body mass index.
Norman. Effect of Obesity on the Labor Curve. Obstet Gynecol 2012.
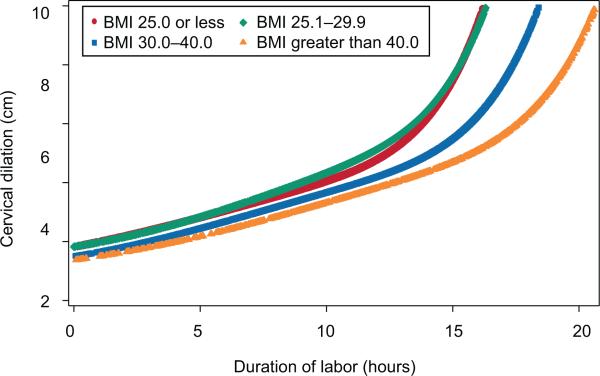
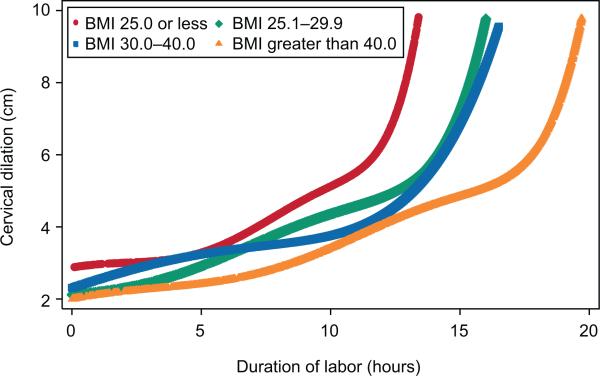
When stratified by BMI, increasing BMI was associated with longer time to reach each respective cervical dilation up to 6 cm for both nulliparous and multiparous women (Table 3). There was no difference in time of labor progression for BMIs 25 or less and BMIs 25.1–29.9 for either parity group. For both nulliparous and multiparous women, there was no clinically significant difference in median time of labor progression after 6 cm. The median time needed to complete the first stage of labor increased significantly as BMI increased over 30 and was approximately 2 hours longer in women with BMIs greater than 40 compared with women with BMIs of 25 or less (6.7 compared with 4.6 for nulliparous women and 5.0 compared with 3.3 for multiparous women). However, there was no association between labor velocity after 6 cm dilation and BMI (Figs. 3 and 4).
Table 3.
Median Duration of First Stage of Labor (4–10 cm) in Hours (5th, 95th Percentile) for Nulliparous and Multiparous Women Stratified by Body Mass Index and in Increments of 2 cm
| Cervical Dilation (cm) | BMI |
|||
|---|---|---|---|---|
| 25.0 or Less | 25.1–29.9 | 30.0–40.0 | Greater Than 40.0 | |
| Nulliparous | 366 | 676 | 746 | 137 |
| 4–10 | 4.6 (1.5, 14.4) | 5.0 (1.6, 15.7) | 5.5 (1.8, 17.3) | 6.7 (2.1, 21.2) |
| Referent | .18 | <.01 | <.01 | |
| 4–6 | 2.3 (0.6, 8.9) | 2.4 (0.6, 9.1) | 2.8 (0.7, 10.9) | 3.4 (0.9, 12.9) |
| Referent | 0.75 | 0.01 | <0.01 | |
| 6–8 | 0.7 (0.1, 5.1) | 0.8 (0.1, 5.7) | 0.8 (0.1, 5.5) | 1.0 (0.1, 6.9) |
| Referent | .38 | .59 | .11 | |
| 8–10 | 0.5 (0.1, 3.5) | 0.7 (0.1, 4.6) | 0.6 (0.1, 4.2) | 0.6 (0.1, 3.9) |
| Referent | .02 | .10 | .49 | |
| Multiparous | 419 | 952 | 1,482 | 426 |
| 4–10 | 3.3 (0.8, 12.6) | 3.9 (1.0, 15.1) | 4.3 (1.1, 16.5) | 5.0 (1.3, 19.2) |
| Referent | .04 | .01 | <.01 | |
| 4–6 | 1.8 (0.3, 9.2) | 1.9 (0.4, 10.1) | 2.3 (0.4, 11.9) | 2.6 (0.5, 13.9) |
| Referent | .42 | .02 | <.01 | |
| 6–8 | 0.4 (0.1, 3.9) | 0.5 (0.1, 4.2) | 0.5 (0.1, 4.3) | 0.6 (0.1, 5.4) |
| Referent | 0.53 | 0.40 | 0.02 | |
| 8–10 | 0.2 (0.02, 2.1) | 0.3 (0.03, 2.6) | 0.3 (0.03, 2.6) | 0.3 (0.04, 3.1) |
| Referent | .06 | .05 | <.01 | |
BMI, body mass index.
P values are adjusted for labor type, race, birth weight more than 4,000 g. P<.01 is considered significant (adjustment for multiple comparisons).
BMI is calculated as weight (kg)/[height (m)]2.
Fig. 3.
Labor curve for nulliparous women stratified by body mass index (BMI).
Norman. Effect of Obesity on the Labor Curve. Obstet Gynecol 2012.
Fig. 4.
Labor curve for multiparous women stratified by body mass index (BMI).
Norman. Effect of Obesity on the Labor Curve. Obstet Gynecol 2012.
DISCUSSION
We found that the first stage of labor for obese women is of longer median duration and has a slower progression until 6 cm than their nonobese cohorts, even after adjusting for potential confounding factors. The difference in the labor curve is manifested in the so-called “latent” phase of labor for obese women and does not affect the active phase of labor. This indicates that it takes longer for obese women to reach the active stage of labor and opposed to what has been commonly accepted, the active phase of the first stage of labor does not begin until 6 cm in this group. When stratified by BMI category, the increased time required to reach the second stage of labor was pronounced. The median time needed to complete the first stage of labor was almost 2 hours longer in women with BMIs greater than 40 compared with normal-weight women for nulliparous and multiparous women and approximately 7 hours longer among the 95th percentile of women in these categories. These findings confirm earlier studies indicating that the current definition of “normal” labor may need to be changed with respect to obese women.
Previous investigations on the subject of labor progression in obese compared with nonobese women have yielded similar but often conflicting results. In 2004, Nuthalapaty et al performed a secondary analysis of a prospective labor induction study in which all 509 patients were 2 cm or less on admission and all received the same induction protocol with oxytocin. This study concluded that, for nulliparous women, increasing BMI was associated with longer duration of labor and increasing cesarean delivery rate but did not find statistical significance with respect to rate of cervical dilation. Conversely, for multiparous women, maternal weight was not found to affect labor duration or progression.20 Similarly, in a prospective cohort study performed with 612 nulliparous women, Vahratian et al21 found that compared with normal-weight women, obese women have a longer duration of labor manifested before 7 cm dilation. Both of these studies included women who did not reach the second stage of labor, thereby introducing the possibility of selection bias. Unlike earlier findings, in a retrospective case–control study with 105 obese women and 113 lean women, Verdiales et al22 found that obese women had a shorter latent phase of labor than did the lean control participants.
Most recently, Koimniarek et al used a similar interval-censored regression analysis to investigate the effect of BMI on labor progression. In this study, 118,978 nulliparous and multiparous women were included. The study concluded that increasing BMI is associated with slower labor progression in both nulliparous and multiparous women. For obese nulliparous women, there was no inflection point in the labor curve; therefore, no distinction was found between latent and accelerated phases. For obese multiparous women, the difference in labor progression was found only before 7 cm. It is important to note that this study included women who did not complete the first stage of labor in the analysis, potentially biasing the results. In addition, although the study population was comprised of 53% obese women, only 6.8% had BMIs greater than 40.12
Our study cohort included only those women who reached the second stage of labor. If any bias exists from excluding women who did not reach the second stage, the bias is likely toward the null and potentially underestimates the difference in labor progression between obese and nonobese women. The use of a single tertiary care center with a large obese population limits the differing clinical approaches and biases inherent in caring for laboring obese patients given that obesity is greater than 50% of the studied population. Another strength of this study was the detailed extraction of data including baseline demographics and labor variables allowing the risk estimates to be adjusted for potential confounding factors.
The potential limitations of our study must be considered as well. Height and weight were based on patient report rather than precise measurement on admission to labor and delivery. However, patient report of weight and height has been found to be a reliable source of information in previous studies of reproductive-aged women.23 In addition, it is possible that patient report of height and weight led to potential inclusion in the incorrect group, causing misclassification bias. However, this would only serve to underestimate the differences identified. Another potential limitation is that our retrospective study design relied on typical labor admission practices, which included few admissions of spontaneous labor in the early latent phase. Thus, the precision of our estimates of labor curve comparisons is restricted with respect to cervical dilation less than 3 cm given the limited number of observations at these earlier dilations. Finally, given the retrospective nature of this study, we can establish only the relationship between obesity and the progression of the first stage of labor and not causality.
We found that women with BMIs of 30 or greater have a longer duration and slower progression of the latent phase of the first stage of labor, confirming earlier studies that excluded women who did not reach the second stage. Our study shows that, for obese women, the accelerated phase of labor does not begin until 6 cm of dilation and that it takes more time to reach the accelerated phase than their nonobese counterparts. Furthermore, we found this difference to increase with increasing obesity class.14 With the increasing number of cesarean deliveries performed, and increased morbidity for obese women undergoing cesarean delivery, it is prudent that we re-evaluate the standard definition of labor arrest. Our findings suggest that the use of a single “normal” labor curve will lead to overdiagnosis of labor dystocia before 6 cm dilation and that definitions of labor arrest should be made with different standards in obese women before the decision for cesarean delivery.
Acknowledgments
Dr Cahill is a Robert Wood Johnson Physician Faculty Scholar, which partially supports this work.
Footnotes
Presented as a poster at the annual meeting of the Society of Maternal Fetal Medicine, February 6–11, 2012, Dallas, Texas.
Financial Disclosure
The authors did not report any potential conflicts of interest.
REFERENCES
- 1.Dodd JM, Grivell RM, Nguyen AM, Chan A, Robinson JS. Maternal and perinatal health outcomes by body mass index category. Aust N Z J Obstet Gynaecol. 2011;51:136–40. doi: 10.1111/j.1479-828X.2010.01272.x. [DOI] [PubMed] [Google Scholar]
- 2.Usha Kiran TS, Hemmadi S, Bethel J, Evans J. Outcome of pregnancy in a woman with an increased body mass index. BJOG. 2005;112:768–72. doi: 10.1111/j.1471-0528.2004.00546.x. [DOI] [PubMed] [Google Scholar]
- 3.Ovsen P, Rasmussen S, Kesmodel U. Effect of prepregnancy maternal overweight and obesity on pregnancy outcome. Obstet Gynecol. 2011;118:305–12. doi: 10.1097/AOG.0b013e3182245d49. [DOI] [PubMed] [Google Scholar]
- 4.Alanis MC, Villers MS, Law TL, Steadman E, Robinson CJ. Complications of cesarean delivery in the massively obese parturient. Am J Obstet Gynecol. 2010;203:271, e1–7. doi: 10.1016/j.ajog.2010.06.049. [DOI] [PubMed] [Google Scholar]
- 5.Robinson HE, O'Connell CM, Joseph KS, McLeod NL. Maternal outcomes in pregnancies complicated by obesity. Obstet Gynecol. 2005;106:1357–64. doi: 10.1097/01.AOG.0000188387.88032.41. [DOI] [PubMed] [Google Scholar]
- 6.Fyfe EM, Anderson NH, North RA, Chan EHY, Taylor RS, Dekker GA, et al. Risk of first-stage and second-stage cesarean delivery by maternal body mass index among nulliparous women in labor at term. Obstet Gynecol. 2011;117:1315–22. doi: 10.1097/AOG.0b013e318217922a. [DOI] [PubMed] [Google Scholar]
- 7.Kominiarek MA, VanVeldhuisen P, Hibbard J, Landy H, Haberman S, Learman L, et al. The maternal body mass index: a strong association with delivery route. Am J Obstet Gynecol. 2010;203:264, e1–7. doi: 10.1016/j.ajog.2010.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai ER, Illuzzi JL. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011;118:29–38. doi: 10.1097/AOG.0b013e31821e5f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friedman E. The graphic analysis of labor. Am J Obstet Gynecol. 1954;68:1568–75. doi: 10.1016/0002-9378(54)90311-7. [DOI] [PubMed] [Google Scholar]
- 10.Friedman EA. Primigravid labor: a graphicostatistical analysis. Obstet Gynecol. 1955;6:567–89. doi: 10.1016/s0029-7844(02)02398-0. [DOI] [PubMed] [Google Scholar]
- 11.Zhang J, Troendle J, Mikolajczyk R, Sundaram R, Beaver J, Fraser W. The natural history of the normal first stage of labor. Obstet Gynecol. 2010;115:705–10. doi: 10.1097/AOG.0b013e3181d55925. [DOI] [PubMed] [Google Scholar]
- 12.Kominiarek MA, Zhang H, VanVeldhuisen P, Troendle J, Beaver J, Hibbard JU. Contemporary labor patterns: the impact of maternal body mass index. Am J Obstet Gynecol. 2011;205:244, e1–8. doi: 10.1016/j.ajog.2011.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang J, Landy HJ, Branch DW, Burkman R, Haberman S, Gregory KD, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol. 2010;116:1281–7. doi: 10.1097/AOG.0b013e3181fdef6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Obesity: preventing and managing a global epidemic . Report of a WHO consultation. Vol. 894. World Health Organ Tech Rep Ser; 2000. pp. i–xii.pp. 1–253. [PubMed] [Google Scholar]
- 15.Royston P. Estimating departure from normality. Stat Med. 1991;10:1283–93. doi: 10.1002/sim.4780100811. [DOI] [PubMed] [Google Scholar]
- 16.Crowder KJ, Hand DJ. Analysis of repeated measures. Chapman and Hall; New York (NY): 1990. [Google Scholar]
- 17.Klein JP, Moeschberger ML. Survival analysis: techniques for censored and truncated data. Springer; Berlin (Germany): 1997. [Google Scholar]
- 18.Vahratian A, Troendle JF, Siega-Riz AM, Zhang J. Methodological challenges in studying labor progression. Paediatr Perinat Epidemiol. 2006;20:72–8. doi: 10.1111/j.1365-3016.2006.00696.x. [DOI] [PubMed] [Google Scholar]
- 19.Greenberg MB, Cheng YW, Hopkins LM, Stotland NE, Bryant AS, Caughey AB. Are there ethnic difference in the length of labor? Am J Obstet Gynecol. 2006;195:743–8. doi: 10.1016/j.ajog.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 20.Nuthalapaty FS, Rouse DJ, Owen J. The association of maternal weight with cesarean risk, labor duration, and cervical dilation rate during labor induction. Obstet Gynecol. 2004;103:452–6. doi: 10.1097/01.AOG.0000102706.84063.C7. [DOI] [PubMed] [Google Scholar]
- 21.Vahratian A, Zhang J, Troendle JF, Savitz DA, Siega-Riz AM. Maternal prepregnancy overweight and obesity and the pattern of labor progression in nulliparous women. Obstet Gynecol. 2004;104:943–51. doi: 10.1097/01.AOG.0000142713.53197.91. [DOI] [PubMed] [Google Scholar]
- 22.Verdiales M, Pacheco C, Cohen WR. The effect of maternal obesity on the course of labor. J Perinat Med. 2009;37:651–5. doi: 10.1515/JPM.2009.110. [DOI] [PubMed] [Google Scholar]
- 23.Brunner Huber LR. Validity of self-reported height and weight in women of reproductive age. Matern Child Health J. 2007;11:137–44. doi: 10.1007/s10995-006-0157-0. [DOI] [PubMed] [Google Scholar]