Abstract
Objective
This study estimates additional average health care expenditures for overweight and obesity for adults with disabilities vs. without.
Design and Methods
Descriptive and multivariate methods were used to estimate additional health expenditures by service type, age group, and payer using 2004–2007 Medical Expenditure Panel Survey data.
Results
In 2007, 37% of community-dwelling Americans with disabilities were obese vs. 27% of the total population. People with disabilities had almost three times ($2,459) the additional average obesity cost of people without disabilities ($889). Prescription drug expenditures for obese people with disabilities were three times as high and outpatient expenditures were 74% higher. People with disabilities in the 45- to 64-year age group had the highest obesity expenditures. Medicare had the highest additional average obesity expenditures among payers. Among people with prescription drug expenditures, obese people with disabilities had nine times the prevalence of diabetes as normal weight people with disabilities. Overweight people with and without disabilities had lower expenditures than normal-weight people with and without disabilities.
Conclusions
Obesity results in substantial additional health care expenditures for people with disabilities. These additional expenditures pose a serious current and future problem, given the potential for higher obesity prevalence in the coming decade.
Introduction
Obesity is a major public health problem and a risk factor for other medical conditions, including hypertension, dyslipidemia, cardiovascular disease, diabetes, and arthritis (1–9). It is also associated with increased disability (10–13) and, at the highest weight levels, mortality (14–17). Health care expenditures attributable to obesity were ~10% of total health care spending in 2006 (18).
Obesity, typically defined as having a body mass index (BMI) of 30 or greater, has become more prevalent among adults in the US in recent years according to National Health and Nutrition Examination Survey (NHANES) data. Age-adjusted obesity among men age 20 and greater increased 17.1% between 1999 and 2008. Among women age 20 and over during the same period, the increase was 6.3% (19). However, recent research suggests that the growth rate in obesity for some population groups is slowing (20).
People with disabilities are an important segment of the population with excess weight (overweight or obese). Approximately 18.7% of the civilian noninstitutionalized US population in 2010 had a disability lasting any length of time (21). People with disabilities also have high health care expenditures (22,23). Disability-associated health care expenditures totaled $397.8 billion in 2006, with disability status adding an average of $11,637 additional health care expenditures (24).
To date, researchers, clinicians, and public health policy makers have considered obesity generally without focusing on people with disabilities who have excess weight. Obesity is a leading secondary condition reported by people with disabilities (25). Obesity expenditures may be higher for people with disabilities compared to those without disabilities for several reasons. People with disabilities may be heavier than those without disabilities, which may make them sicker. Thus, people with disabilities who are obese may require additional monitoring or medical care, and may have higher expenditures. In addition, obesity in people with disabilities may limit mobility such that they may not get to the doctor for regular medical care until their problems become more urgent, and perhaps more expensive.
If health care expenditures are higher among obese people with disabilities compared to those without disabilities, additional focus on obese people with disabilities may be warranted to address unmet health care needs. In addition, policy makers may want to focus on obese people most at risk for disability to prevent even higher health care expenditures and loss of health. Understanding these expenditures for important subgroups (e.g., age and payer) may also inform choices by policy makers in designing programs and allocating resources.
This study compares differences in health care expenditures between people with excess weight who have disabilities and people with excess weight without disabilities. It addresses the following research questions: (1) What is the prevalence of overweight and obesity among noninstitutionalized adults with and without disabilities? (2) What are the relative additional health care expenditures for being overweight and obese (compared to normal weight) among noninstitutionalized adults with and without disabilities? (3) What types of health care services have the highest expenditures associated with obesity for people with and without disabilities? (4) Which age and payer (Medicare, Medicaid, private pay) subgroups within these two populations have the highest expenditures?
Methods
Data were obtained from two sources. First, a disability measure was developed from the 2003–2006 National Health Interview Survey (NHIS), a nationally representative survey sponsored by the National Center for Health Statistics. Second, measures of health care expenditures, weight status, and demographic and socioeconomic information on the civilian noninstitutionalized adult population were developed from the 2004–2007 Medical Expenditure Panel Survey (MEPS), a nationally representative survey sponsored by the Agency for Healthcare Research and Quality (AHRQ) and drawn from a subsample of households that participated in the NHIS. The analytic sample of 39,457 adults aged 19 and older was taken from the NHIS Sample Adult File.
The study used descriptive and multivariate methods. Means or proportions were estimated to compare demographic and socioeconomic characteristics, expenditures, and prevalence of conditions for those with excess weight for two different subgroups: those people with and without disabilities. Means were also estimated for people by weight category, disability status and prevalence of having various medical conditions.
Multivariate methods were used to estimate the additional expenditures of being overweight or obese for people with disabilities vs. without. Two types of dependent variables for total and service-specific expenditures were developed. The first type was a dummy variable for any MEPS health care expenditures (e.g., any expenditures for use in Logit models), and the second type was a continuous variable for the amount of expenditures (e.g., amount of total expenditures if expenditures greater than zero). Expenditures are presented in 2007 dollars and the weights for each person adjusted to obtain 2007 annual health care expenditures. The dependent variable for total health care expenditures comprised inpatient, outpatient, prescription drug, home health care, emergency room, vision and dental services, and durable medical equipment for all payers. Mean total health care expenditures for the entire weighted sample in 2007 dollars were $4,841 ($5,510 for the 33,846 sample adults with any health expenditures).
The study included several policy variables. Variables for weight status were defined as underweight (BMI < 18.5, 3.9% of the sample), normal weight (BMI 18.5–24.99, 34.3% of the sample), overweight (BMI 25.0–29.99, 34.2% of the sample), and obese weight (BMI ≥30, 27.6% of the sample). Using questions in the NHIS, disability was defined as having a limitation in any way in any activity because of a physical, mental, or emotional problem. The definition included all people reporting a deficit in activities of daily living (ADL), such as bathing, eating, or toileting, or instrumental activities of daily living (IADL), such as shopping and bill paying. Approximately 15.7% of respondents in the weighted sample reported a disability. Independent variables included in the models were self-reported health status, demographic characteristics (age, gender, race/ethnicity, and marital status), socioeconomic status (education and income), geographic region, and dummy variables for MEPS year. Summary statistics for the variables used in the analysis appear in Table 1.
TABLE 1.
Means of variables used in analysis (n = 39,457)
| Characteristic | Variable | Mean or proportion | Std. Dev. | Std. Err. |
|---|---|---|---|---|
| Expenditures | Total (2007 dollars) | 4,841 | 11,483 | — |
| Inpatient (if any use) | 14,528 | 21,336 | — | |
| Outpatient (if any use) | 2,068 | 5,366 | — | |
| Home health (if any use) | 6,272 | 9,393 | — | |
| Prescription drug (if any use) | 1,651 | 3,387 | — | |
| Emergency room (if any use) | 1,054 | 1,918 | — | |
| Disability status | Any disability | 0.157 | 0.005 | |
| Weight status | Obese (BMI ≥30) | 0.276 | 0.004 | |
| Overweight (BMI 25.0–29.99) | 0.342 | 0.003 | ||
| Normal weight (BMI 18.5–24.99) | 0.343 | 0.004 | ||
| Underweight (BMI <18.5) | 0.039 | 0.001 | ||
| Age | 19–44 years | 0.451 | 0.006 | |
| 45–64 years | 0.347 | 0.004 | ||
| 65–74 years | 0.099 | 0.003 | ||
| 75–84 years | 0.075 | 0.003 | ||
| 85+ years | 0.028 | 0.001 | ||
| Gender | Female | 0.549 | 0.004 | |
| Race or ethnicity | White | 0.719 | 0.007 | |
| Black | 0.117 | 0.005 | ||
| Hispanic | 0.107 | 0.005 | ||
| Asian | 0.036 | 0.002 | ||
| Other race | 0.021 | 0.002 | ||
| Marital status | Married | 0.475 | 0.005 | |
| Education | Less than high school | 0.139 | 0.004 | |
| High school graduate | 0.497 | 0.006 | ||
| College graduate or some college | 0.185 | 0.005 | ||
| Graduate degree | 0.095 | 0.004 | ||
| Other degree | 0.084 | 0.002 | ||
| Income | <100% of federal poverty level | 0.117 | 0.003 | |
| 100–199% of federal poverty level | 0.183 | 0.004 | ||
| >200% of federal poverty level | 0.700 | 0.006 | ||
| Region | Midwest | 0.228 | 0.009 | |
| South | 0.365 | 0.013 | ||
| West | 0.220 | 0.014 | ||
| Northeast | 0.188 | 0.008 | ||
| MEPS year | Year 2004 | 0.246 | 0.003 | |
| Year 2005 | 0.251 | 0.002 | ||
| Year 2006 | 0.252 | 0.002 | ||
| Year 2007 | 0.252 | 0.004 |
MEPS, Medical Expenditure Panel Survey. Source: RTI International Analysis of the 2004–2007 Medical Expenditure Panel Survey.
Health care expenditures were estimated with the MEPS sample weights using a two-part model using Logit in the first part and a general linear model (GLM) with a gamma distribution and a log link in the second part on positive expenditures. Weight and disability status were the principal variables of interest. Health care expenditures were estimated separately for people using specific services (inpatient, outpatient, home health, prescription drug, and emergency room). These expenditures were also estimated separately for people in various age groups, and separately for people with specific payer types, using either total expenditures or expenditures for specific service types (e.g., inpatient hospital care). After each regression ran, predictions were made for two subgroups—those people with and without disabilities—to estimate the additional average expenditures of being overweight and obese. A total of 21 regressions were estimated to generate the expenditures and bootstrapped standard errors presented in the study. The regression coefficients are available from the authors upon request. The methods used are similar to prior studies estimating additional health care expenditures for obesity (18) and disability (24).
The additional health care expenditures associated with being obese (compared with being of normal weight) were calculated post-estimation in 2007 dollars by predicting the dependent variable for the Logit and GLM models and then multiplying the predicted values for each respondent. This product is the predicted probability of any expenditures for each person times the predicted amount of expenditures for each person from the GLM regression. Then, people with obesity were recoded as having no obesity, to remove the obesity-related effect on health care expenditures. Predictions for the dependent variable were again made for the Logit and GLM models and multiplied. The average of the difference between these two products for each person, the first calculated using the whole MEPS sample, and the second for the same respondents less any obesity-related expenditures, was the amount of health care expenditures associated with obesity in the sample. The same predictions of additional health care expenditures for overweight people (as compared with people of normal weight) were also obtained. The models used in our analyses control for disability status as an independent variable, so the additional overweight and obesity cost estimates are independent of disability costs.
Results
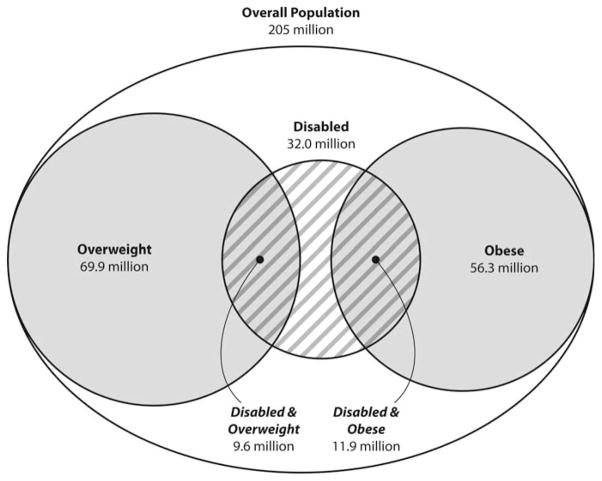
Our descriptive analyses found that 69.9 million (34%) of 205 million community-dwelling Americans were overweight in 2007, and 56.3 million people (27%) were obese (Figure 1). Of the 32 million people with disabilities in these data, 30% were overweight and 37% were obese. Comparatively, obesity prevalence was about 1.35 times higher among people with disabilities as in the general community-dwelling population. For each weight status level, people with disabilities have approximately three times higher mean total health care expenditures as people without disabilities (Table 2).
FIGURE 1.
Population with disability, overweight and obesity.
TABLE 2.
Mean expenditures by disability and weight status (n = 39,457)
| People with disabilities | People without disabilities | |
|---|---|---|
| Normal weight | 10,863 | 3,459 |
| Overweight | 9,907 | 3,375 |
| Obese | 11,460 | 4,132 |
Source: RTI International Analysis of the 2004–2007 Medical Expenditure Panel Survey.
In multivariate analyses estimating total health care expenditures, the additional average cost of being obese for people with disabilities ($2,459) was almost three times the additional cost of obesity for people without disabilities ($889) (Table 3). Additional average expenditures for obese people with disabilities by service type were at least as high as, and sometimes considerably higher than, additional average expenditures for obese people without disabilities. The service type with the highest additional average obesity expenditures was prescription drugs, whose expenditures were three times as high for people with disabilities ($1,297) as for those without disabilities ($414). Additional average obesity outpatient and emergency room expenditures were also statistically significantly higher (each being 74% higher for people with disabilities than without).
TABLE 3.
Additional average weight expenditures (total expenditures and by service type) (n = 39,457)
| Total
|
Inpatient
|
Outpatient
|
Home health
|
Prescription drugs
|
Emergency room
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Std. Err. | Mean | Std. Err. | Mean | Std. Err. | Mean | Std. Err. | Mean | Std. Err. | Mean | Std. Err. | |
| People with disabilities (compared with normal weight) | ||||||||||||
| Cost of being overweight | −$482 | (299) | −$733 | (207)* | −$76 | (91) | −$138 | (92) | $296 | (80)* | −$2 | (15) |
| Cost of being obese | $2,459 | (351)* | $36 | (184) | $609 | (114)* | $1 | (89) | $1,297 | (132)* | $61 | (14)* |
| People without disabilities (compared with normal weight) | ||||||||||||
| Cost of being overweight | −$120 | (98) | −$213 | (59)* | −$13 | (44) | −$5 | (3) | $101 | (21)* | −$1 | (7) |
| Cost of being obese | $889 | (112)* | $27 | (54) | $350 | (56)* | $1 | (4) | $414 | (34)* | $35 | (8)* |
Source: RTI International Analysis of the 2004–2007 Medical Expenditure Panel Survey. Numbers in parenthesis are standard errors.
p < 0.05.
For some types of services overweight people with and without disabilities had statistically significantly lower expenditures than persons of normal weight with and without disabilities. For example, overweight people with disabilities had lower inpatient expenditures (−$733) than normal weight people with disabilities; overweight persons without disabilities also had lower inpatient expenditures than normal weight people without disabilities (−$213), but the difference was not as great. Across services types, overweight people with disabilities usually had much lower expenditures than normal weight people with disabilities. The same was true for overweight people without disabilities. The exception was the statistically significantly positive additional prescription drug expenditures for overweight people with ($296) and without ($101) disabilities, as compared with normal weight people with and without disabilities.
To help explain the large additional overweight- and obesity-related prescription drug expenditures among people with disabilities, the prevalence of having various medical conditions in MEPS data was estimated using descriptive statistics (Table 4). Among prescription drug users, the top 10 (out of 32) conditions among people with disabilities were similar for both overweight and obese people. However, the prevalence of such conditions was 25–60% higher among obese than among normal-weight people. Compared with normal-weight people with disabilities, overweight people with disabilities had approximately a 10, 20, and 30% higher prevalence of arthritis, hypertension, and high cholesterol, respectively. These conditions represent the top three conditions for both the overweight and obesity subgroups. Among prescription drug users, diabetes was the fourth-leading condition experienced by obese people with disabilities, even though it was not among the top 10 conditions for overweight or normal-weight people with disabilities with such expenditures.
TABLE 4.
Frequent condition prevalences for people with disabilities with prescription drug expenditures (by weight category) (n = 7,301)
| Rank | Normal weight
|
Overweight
|
Obese
|
|||||
|---|---|---|---|---|---|---|---|---|
| Condition | Prevalence | Condition | Prevalence | Odds of having condition if overweight as compared to normal weight | Condition | Prevalence | Odds of having condition if obese as compared to normal weight | |
| 1 | Arthritis | 46.3 % | Arthritis | 50.8 % | 1.10 | Hypertension | 60.2 % | 1.45 |
| 2 | Hypertension | 41.5 % | Hypertension | 50.1 % | 1.21 | Arthritis | 57.8 % | 1.25 |
| 3 | Infection | 33.2 % | High Cholesterol | 33.1 % | 1.31 | High Cholesterol | 40.1 % | 1.59 |
| 4 | Injury | 32.1 % | Infection | 28.8 % | 0.87 | Diabetes | 35.1 % | 9.24 |
| 5 | GERD | 27.2 % | GERD | 27.6 % | 1.02 | Infection | 34.5 % | 1.04 |
| 6 | Other heart diseasea | 25.4 % | Injury | 26.8 % | 0.83 | GERD | 30.9 % | 1.14 |
| 7 | High cholesterol | 25.3 % | Depression | 24.8 % | 1.06 | Depression | 30.3 % | 1.30 |
| 8 | Depression | 23.4 % | Back disorder | 24.0 % | 1.08 | Injury | 30.2 % | 0.94 |
| 9 | Back disorder | 22.3 % | Other heart diseasea | 22.8 % | 0.90 | Back disorder | 29.8 % | 1.34 |
| 10 | Respiratory condition | 21.4 % | Respiratory condition | 22.1 % | 1.03 | Other heart diseasea | 25.6 % | 1.01 |
Other heart disease excludes hypertension, chronic heart failure, and chronic heart disease. Source: RTI International Analysis of the 2004–2007 Medical Expenditure Panel Survey.
We also examined whether obesity expenditures varied by age for people with disabilities compared to people without disabilities. Age-group multivariate analyses in Table 5 show that additional average obesity expenditures among people with disabilities were highest in the 45- to 64-year age group ($2,822), almost 2.5 times the additional average expenditures of obese people without disabilities in that age group ($1,197). Moreover, additional average obesity expenditures for people with disabilities aged 18 to 44 ($2,442) were triple those of people without disabilities ($812). Because MEPS data exclude persons in institutions, substantial amounts of obesity expenditures among people with disabilities aged 65 years and older were not included in the analyses, and mean excess costs in the analyses might have been higher had they been included.
TABLE 5.
Additional average weight expenditures by age group (n = 39,457)
| Overall population
|
Ages 18–44
|
Ages 45–64
|
Age 65 and over
|
|||||
|---|---|---|---|---|---|---|---|---|
| Mean | Std. Err. | Mean | Std. Err. | Mean | Std. Err. | Mean | Std. Err. | |
| People with disabilities (compared with normal weight) | ||||||||
| Cost of being overweight | −$482 | (299) | −$116 | (289) | $45 | (427) | −$1,375 | (574)* |
| Cost of being obese | $2,459 | (351)* | $2,442 | (433)* | $2,822 | (523)* | −$96 | (586) |
| People without disabilities (compared with normal weight) | ||||||||
| Cost of being overweight | −$120 | (98) | −$28 | (95) | $76 | (161) | −$698 | (337)* |
| Cost of being obese | $889 | (112)* | $812 | (134)* | $1,197 | (192)* | $73 | (342) |
Source: RTI International Analysis of the 2004–2007 Medical Expenditure Panel Survey. Numbers in parenthesis are standard errors.
p < 0.05.
Lastly, we examined whether obesity expenditures varied by payer type for people with disabilities compared to those without. Health care expenditures for obese people with disabilities were higher, and the difference was statistically significant, for each third-party and other payers (Table 6). Compared with normal-weight people with disabilities for each respective payer, additional obesity expenditures were highest for people with disabilities who had Medicare coverage ($2,929), followed by those who had private insurance ($2,449) and those with Medicaid ($2,397).
TABLE 6.
Additional average weight expenditures for people with disabilities by payer type (n = 7,345)
| People with disabilities (compared with normal weight) | Medicare
|
Medicaid
|
Private
|
|||
|---|---|---|---|---|---|---|
| Mean | Std. Err. | Mean | Std. Err. | Mean | Std. Err. | |
| Cost of being overweight | −$623 | (371) | −$431 | (280) | −$528 | (316) |
| Cost of being obese | $2,929 | (441)* | $2,397 | (348)* | $2,449 | (377)* |
BMI, body mass index. Source: RTI International Analysis of the 2004–2007 Medical Expenditure Panel Survey. Numbers in parenthesis are standard errors.
p < 0.05.
Discussion
It is widely recognized that obesity results in substantial additional expenditures for the US health care system (18,26). Much less is known about the additional per person obesity expenditures for people with disabilities compared to those without. This study found that in the 2004–2007 civilian, community-dwelling adult population, average additional expenditures for obesity among people with disabilities were $2,459, compared with an average additional $889 for obese people without disabilities (2007 dollars). Prescription drugs, followed by outpatient service expenditures, were the largest drivers of higher additional obesity expenditures among people with disabilities. Other studies have also found high prescription drug expenditures among obese people in the general population (18,26).
Incremental expenditures associated with obesity by disability status vary by age. Our findings revealed that nonelderly obese persons with disabilities had almost triple the obesity expenditures of nonelderly obese persons without disabilities. In particular, the 45- to 64-year age group had the highest additional average obesity expenditures. Noninstitutionalized elderly persons with and without disabilities had far lower obesity expenditures than younger age groups, which is consistent with previous findings (27).
A substantial portion of people with disabilities are obese. People with disabilities are at higher risk of obesity because some conditions such as arthritis and diabetes are characterized by high levels of functional impairment. Arthritis can readily limit mobility, which may result in substantial weight gain over time. For diabetes, weight gain can be a byproduct of insulin use if patients do not effectively manage their weight (28). The coexistence of disability, obesity, and serious chronic conditions may result in very high health care expenditures.
Conversely, as shown in Figure 1, over one-fifth of obese people have a disability. Obese people may be at a higher risk of disability because of their higher prevalence of chronic conditions, such as cardiovascular disease and dyslipidemia, which may result in disability-producing events such as heart attack and stroke (1,2,4). Obesity may also result in depression (29), injury (30), and back disorders (31), all of which may produce lengthy periods of disability.
The additional obesity expenditures are so much higher for people with disabilities compared to those without disabilities highlights the need to focus on preventing, reducing, or better controlling secondary conditions for obese people with disabilities. The multivariate analyses in this study controlled for the effects of disability, so the higher additional obesity expenditures for people with disability compared with those without are for conditions secondary to their disability. Given the higher prevalence of arthritis, high cholesterol, hypertension, and diabetes among obese people with disabilities as compared with normal-weight people with disabilities, and that disability per se does not cause these conditions, care management initiatives to lower the prevalence or reduce the effects of these secondary conditions may reduce ensuing disability or its effects. Health promotion and disease-prevention initiatives may also help reduce secondary conditions among people with disabilities (32–34). Such a focus may also help to reduce the substantially higher outpatient service expenditures related to these conditions experienced by obese people with disabilities.
In addition, given that people with disabilities have poorer health and high health care expenditures, identifying obese persons most at risk for disability offers the potential to have a high impact on the health of obese persons and on health care expenditures. Identifying such people should be the focus of future research. Targeted health promotion and disease-prevention initiatives that consider special needs of obese people with disabilities alsomay be beneficial to the overall obese population.
Among the nonobese population with disabilities, additional clinic-level interventions focusing on prevention are needed. People with disabilities at normal weight may benefit from counseling regarding physical activity and nutrition. Care coordination efforts should focus not only on a person’s disability (35), but also on the prevention and treatment of secondary conditions that may lead to obesity (25). In addition, clinicians may require further education on the extra burden that obesity places on people with disabilities, both in terms of trying to help people lose weight, but also in watching for additional complications (35).
Most public health interventions (e.g., exercise) targeting obesity are not designed to meet the needs of people with disabilities. Consequently, community-level environmental interventions with appropriate outreach should be designed to help people with disabilities make healthier lifestyle choices in terms of physical activity and nutrition. For example, wheelchair accessible sidewalks, parks and exercise centers to facilitate physical activity and funding for initiatives to encourage access to grocery stores, supermarkets, and farmers markets may help promote wise food choices. Finally, interventions designed to prevent, delay, or reduce obesity for people with disabilities would benefit from the input of people with disabilities and specific data on people with disabilities.
This study found lower expenditures for being overweight (BMI of 25 to <30) compared with normal weight (regardless of disability status), which may indicate a protective effect for being overweight. Prior work on expenditure outcomes with similar methods found no difference in additional mean expenditures for normal weight vs. overweight (26), and being overweight may improve survival for noncancer, noncardiovascular mortality (36). In addition, previous studies in the older population (12,37), particularly those in nursing homes (38), have shown a protective effect for higher BMI (being either overweight or obese) as opposed to being normal weight in terms of reducing health care expenditures. Our study’s finding suggests that overweight people may benefit from interventions to prevent them from becoming obese. The “protective effect” for being overweight is larger for people with disabilities because their average total expenditures are much higher than people without disabilities, so the potential cost savings may be larger.
This study has at least four limitations. First, we estimated additional average expenditures for overweight and obesity using an inclusive definition of disability and estimated prevalence. Alternatively, other researchers might have chosen a different definition of disability, for example, one with more stringent permanence or severity criteria. How the concept of disability is measured depends on the definition chosen and available data. Given that we estimated per person additional overweight and obese expenditures for people with vs. without disabilities, we believe any differences in effects estimated using a narrower definition of disability may have been slightly larger than what we reported in this study.
Second, the regression methodology used did not control for other medical conditions such as diabetes. Therefore, the reported estimates for additional average obesity and overweight expenditures would have been somewhat lower had these other medical conditions been taken into account. Third, the methodology used did not assess the issue of causality—whether obesity was the cause of disability, and vice versa. Although causality was not within the scope of the study, research on causality would be of particular interest to practitioners as well as policy makers. Fourth, BMI is just one measure of obesity; other measures of obesity may be more or less relevant for people with disabilities, whose impairments as well as medicines may predispose them to greater obesity prevalence. In addition, obesity measures derived from self-reported weight are subject to underreporting of weight (39).
Given that people with disabilities already have higher health care expenditures (40), these additional obesity expenditures pose a serious current as well as future public health problem, because of the potential for higher obesity prevalence in the coming decade (19). With projections of more people with disabilities coupled with more people with obesity (27), the intersection of these two trends might suggest a growing burden of additional health care expenditures for obese people. Finding effective interventions to prevent greater disability among obese people with disabilities, as well as those interventions to prevent disability among those who are currently obese, may help slow the growth rate in health care expenditures as well as improve health for those at risk.
Acknowledgments
Funding agencies: This study was supported by the Centers for Disease Control and Prevention (CDC) [Contract # 200-2007-22644, Task # 05]. The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Disclosure: The authors have no conflict of interest
Author contributions: WA, JW and BA conceived the research design. WA and GK analyzed the data. All authors were involved in writing the article and had final approval of the submitted and published versions.
References
- 1.Brown CD, Higgins M, Donato KA, et al. Body mass index and the prevalence of hypertension and dyslipidemia. Obes Res. 2000;8:605–619. doi: 10.1038/oby.2000.79. [DOI] [PubMed] [Google Scholar]
- 2.Wilson PW, D’Agostino RB, Sullivan L, et al. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med. 2002;162:1867–1872. doi: 10.1001/archinte.162.16.1867. [DOI] [PubMed] [Google Scholar]
- 3.Gregg EW, Cheng YJ, Cadwell BL, et al. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA. 2005;293:1868–1874. doi: 10.1001/jama.293.15.1868. [DOI] [PubMed] [Google Scholar]
- 4.Krauss RM, Winston M, Fletcher BJ, et al. Obesity: impact on cardiovascular disease. Circulation. 1998;98:1472–1476. [PubMed] [Google Scholar]
- 5.Psaltopoulou T, Ilias I, Alevizaki M. The role of diet and lifestyle in primary, secondary, and tertiary diabetes prevention: a review of meta-analyses. Rev Diabet Stud. 2010;7:26–35. doi: 10.1900/RDS.2010.7.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gregg EW, Cadwell BL, Cheng YJ, et al. Trends in the prevalence and ratio of diagnosed to undiagnosed diabetes according to obesity levels in the US. Diabetes Care. 2004;27:2806–2812. doi: 10.2337/diacare.27.12.2806. [DOI] [PubMed] [Google Scholar]
- 7.Blagojevic M, Jinks C, Jeffery A, et al. Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2010;18:24–33. doi: 10.1016/j.joca.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 8.Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 9.Must A, Spadano J, Coakley EH, et al. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 10.Vincent HK, Vincent KR, Lamb KM. Obesity and mobility disability in the older adult. Obes Rev. 2010;11:568–579. doi: 10.1111/j.1467-789X.2009.00703.x. [DOI] [PubMed] [Google Scholar]
- 11.Busetto L, Romanato G, Zambon S, et al. The effects of weight changes after middle age on the rate of disability in an elderly population sample. J Am Geriatr Soc. 2009;57:1015–1021. doi: 10.1111/j.1532-5415.2009.02273.x. [DOI] [PubMed] [Google Scholar]
- 12.Alley DE, Chang VW. The changing relationship of obesity and disability, 1988–2004. JAMA. 2007;298:2020–2027. doi: 10.1001/jama.298.17.2020. [DOI] [PubMed] [Google Scholar]
- 13.Ferraro KF, Su YP, Gretebeck RJ, et al. Body mass index and disability in adulthood: a 20-year panel study. Am J Public Health. 2002;92:834–840. doi: 10.2105/ajph.92.5.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flegal KM, Graubard BI, Williamson DF, et al. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 15.Fontaine KR, Redden DT, Wang C, et al. Years of life lost due to obesity. JAMA. 2003;289:187–193. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 16.Calle EE, Teras LR, Thun MJ. Obesity andmortality. N Engl J Med. 2005;353:2197–2199. doi: 10.1056/NEJM200511173532020. [DOI] [PubMed] [Google Scholar]
- 17.Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 18.Finkelstein EA, Trogdon JG, Cohen JW, et al. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 2009;28:w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 19.Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 20.Sturm R, Hattori A. Morbid obesity rates continue to rise rapidly in the United States. Int J Obes. 2012;37:889–891. doi: 10.1038/ijo.2012.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brault M. Americans with disabilities: 2010. Current Population Reports. Washington, DC: US Census Bureau; 2012. pp. 70–131. [Google Scholar]
- 22.Dejong G, Palsbo SE, Beatty PW, et al. The organization and financing of health services for persons with disabilities. Milbank Q. 2002;80:261–301. doi: 10.1111/1468-0009.t01-1-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fried TR, Bradley EH, Williams CS, et al. Functional disability and health care expenditures for older persons. Arch Intern Med. 2001;161:2602–2607. doi: 10.1001/archinte.161.21.2602. [DOI] [PubMed] [Google Scholar]
- 24.Anderson WL, Armour BS, Finkelstein EA, et al. Estimates of state-level healthcare expenditures associated with disability. Public Health Rep. 2010;125:44–51. doi: 10.1177/003335491012500107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Institute of Medicine. The Future of Disability in America. Washington: National Academies Press; 2007. [PubMed] [Google Scholar]
- 26.Finkelstein EA, Fiebelkorn IC, Wang G. National medical spending attributable to overweight and obesity: how much, and who’s paying? Health Aff (Millwood) 2003:W3-219–226. doi: 10.1377/hlthaff.w3.219. Suppl Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 27.Sturm R, Ringel JS, Andreyeva T. Increasing obesity rates and disability trends. Health Aff (Millwood) 2004;23:199–205. doi: 10.1377/hlthaff.23.2.199. [DOI] [PubMed] [Google Scholar]
- 28.Tibaldi J. Initiating and intensifying insulin therapy in type 2 diabetes mellitus. Am J Med. 2008;121:S20–S29. doi: 10.1016/j.amjmed.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 29.McCrea RL, Berger YG, King MB. Body mass index and common mental disorders: exploring the shape of the association and its moderation by age, gender and education. Int J Obes (Lond) 2011 doi: 10.1038/ijo.2011.65. [DOI] [PubMed] [Google Scholar]
- 30.Chaudhry S, Egol KA. Ankle injuries and fractures in the obese patient. Orthop Clin North Am. 2011;42:45–53. doi: 10.1016/j.ocl.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 31.Urquhart DM, Berry P, Wluka AE, et al. Young Investigator Award winner: increased fat mass is associated with high levels of low back pain intensity and disability. Spine (Phila Pa 1976) 2011;36:1320–1325. doi: 10.1097/BRS.0b013e3181f9fb66. [DOI] [PubMed] [Google Scholar]
- 32.Altman B, Bernstein A. Disability and health in the United States, 2001–2005. Hyattsville, MD: National Center for Health Statistics; 2008. Available at: http://www.cdc.gov/nchs/data/misc/disability2001-2005.pdf. [Google Scholar]
- 33.US Department of Health and Human Services. Healthy People 2010. 2. Washington, DC: US Government Printing Office; Nov, 2000. Disability and Secondary Conditions Focus Area 6. [Google Scholar]
- 34.Rimmer JH. Health promotion for people with disabilities: the emerging paradigm shift from disability prevention to prevention of secondary conditions. Phys Ther. 1999;79:495–502. [PubMed] [Google Scholar]
- 35.US Department of Health and Human Services. The 2005 Surgeon General’s call to action to improve the health and wellness of persons with disabilities: calling you to action. Washington, DC: US Department of Health and Human Services, Office of the Surgeon General; 2005. Available at: http://www.surgeongeneral.gov/library/disabilities/calltoaction/whatitmeanstoyou.html. [Google Scholar]
- 36.Flegal KM, Graubard BI, Williamson DF, et al. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298:2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- 37.Grabowski DC, Ellis JE. High body mass index does not predict mortality in older people: analysis of the longitudinal study of aging. J Am Geriatr Soc. 2001;49:968–979. doi: 10.1046/j.1532-5415.2001.49189.x. [DOI] [PubMed] [Google Scholar]
- 38.Grabowski DC, Campbell CM, Ellis JE. Obesity and mortality in elderly nursing home residents. J Gerontol A Biol Sci Med Sci. 2005;60:1184–1189. doi: 10.1093/gerona/60.9.1184. [DOI] [PubMed] [Google Scholar]
- 39.Burkhauser RV, Cawley J. Beyond BMI: the value of more accurate measures of fatness and obesity in social science research. J Health Econ. 2008;27:519–529. doi: 10.1016/j.jhealeco.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 40.Anderson WL, Wiener JM, Finkelstein EA, et al. Estimates of national health care expenditures associated with disability. J Disability Policy Stud. 2011;21:230–240. [Google Scholar]