Abstract
A number of studies have analyzed the performance of malaria rapid diagnostic tests (RDTs) in Colombia with discrepancies in performance being attributed to a combination of factors such as parasite levels, interpretation of RDT results and/or the handling and storage of RDT kits. However, some of the inconsistencies observed with results from Plasmodium falciparum histidine-rich protein 2 (PfHRP2)-based RDTs could also be explained by the deletion of the gene that encodes the protein, pfhrp2, and its structural homolog, pfhrp3, in some parasite isolates. Given that pfhrp2- and pfhrp3-negative P. falciparum isolates have been detected in the neighboring Peruvian and Brazilian Amazon regions, we hypothesized that parasites with deletions of pfhrp2 and pfhrp3 may also be present in Colombia. In this study we tested 100 historical samples collected between 1999 and 2009 from six Departments in Colombia for the presence of pfhrp2, pfhrp3 and their flanking genes. Seven neutral microsatellites were also used to determine the genetic background of these parasites. In total 18 of 100 parasite isolates were found to have deleted pfhrp2, a majority of which (14 of 18) were collected from Amazonas Department, which borders Peru and Brazil. pfhrp3 deletions were found in 52 of the100 samples collected from all regions of the country. pfhrp2 flanking genes PF3D7_0831900 and PF3D7_0831700 were deleted in 22 of 100 and in 1 of 100 samples, respectively. pfhrp3 flanking genes PF3D7_1372100 and PF3D7_1372400 were missing in 55 of 100 and in 57 of 100 samples. Structure analysis of microsatellite data indicated that Colombian samples tested in this study belonged to four clusters and they segregated mostly based on their geographic region. Most of the pfhrp2-deleted parasites were assigned to a single cluster and originated from Amazonas Department although a few pfhrp2-negative parasites originated from the other three clusters. The presence of a high proportion of pfhrp2-negative isolates in the Colombian Amazon may have implications for the use of PfHRP2-based RDTs in the region and may explain inconsistencies observed when PfHRP2-based tests and assays are performed.
Introduction
Although more than half of the population of Colombia is at risk for malaria infection, malaria in the country has steadily declined from approximately 6 cases per 1000 individuals in 2001 to less than 2 cases per 1000 individuals in 2012 [1]. More than 60% of these malaria cases were caused by Plasmodium vivax while the rest were due to P. falciparum and mixed-species infections [1]. About 79% of all malaria cases (and 71% of all P. falciparum and mixed species malaria infections) reported in 2011 were concentrated in the Departments of Antioquia, Choco, Cordoba, and Nariño [2]. The fixed-dose combination of artemether and lumefantrine is the first-line treatment for P. falciparum infections while chloroquine and primaquine are used to treat P. vivax malaria cases.
In order to administer effective malaria treatment, early and accurate diagnosis is essential. Colombia has a network of diagnostic laboratories and trained microscopists and light microscopy remains the primary method for malaria diagnosis. Nevertheless, malaria rapid diagnostic tests (RDTs) are increasingly being utilized especially in areas where microscopic diagnosis is not feasible [3]. Nowadays, RDT use is not limited to case management in endemic countries; they are also utilized in malaria surveillance and case investigations. Outside malaria endemic countries, RDTs play an important role in disease diagnosis [4]. Pan-specific malaria RDTs target specific antigens, such as lactate dehydrogenase (LDH) and aldolase found in all Plasmodium species, while histidine-rich protein 2 (PfHRP2)-based RDTs are specific for P. falciparum. The majority of the commercially available RDTs target PfHRP2 because of its abundance, high specificity, and thermal stability among other features [5]. A number of PfHRP2-based RDTs cross-react with histidine-rich protein 3 (PfHRP3), a structural homolog with significant sequence similarity and some antigenic cross-reactivity. Factors that affect the accuracy of malaria RDT results include parasite density [6], proper storage and handling of RDT kits [7] and objectivity in interpreting test results [8]. One major concern with RDT performance is the possible false negative results due to the poor quality of tests because they can lead to misdiagnosis and failure to treat. Besides the quality of the tests, other factors such as the absence of the pfhrp2 gene in natural P. falciparum isolates can contribute to false negative test results [4]. The first evidence for large scale pfhrp2 gene deletions in wild P. falciparum parasites came from Peru [9] and was further substantiated in subsequent studies [10,11]. Other investigations have provided evidence for pfhrp2 deletion in some parts of Brazil and Suriname [12,13]. Studies conducted in Africa found very low levels of pfhrp2 deletion especially in Mali, and Senegal but not in the other countries tested [14–16]. One study in India reported very low levels of pfhrp2 deletion in one state [17] and another study conducted in Honduras failed to find any pfhrp2 deleted parasites [18]. Evidence for deletion of pfhrp3, which is a homologue of pfhrp2 and contributes to some cross reactivity at the antigen level, has also been documented in several studies [9–13,18].
Given the above reports of pfhrp2 and pfhrp3 gene deletions, especially in P. falciparum parasites from South America, and the false negative test results associated with these deletions, it was important to determine if deletions of pfhrp2 (and pfhrp3) are present in parasites in Colombia. Since the prevalence of pfhrp2-negative parasites has been reported to be as high as 40% in the Amazon region of neighboring Peru, [9] and PfHRP2-based malaria RDTs are used for malaria diagnosis in Colombia, it is important to determine if pfhrp2- and pfhrp3-negative P. falciparum strains are circulating in Colombia, and contributing to false negative RDT results.
This study investigates the prevalence of pfhrp2- and pfhrp3-negative P. falciparum isolates in Colombia using parasite isolates collected at various time points from different parts of the country. We also characterized the parasite isolates genetically so as to determine the genetic background of pfhrp2- and pfhrp3-negative parasite isolates in relation to their geographical distribution in Colombia.
Materials and Methods
Ethics Statement
This study was reviewed and approved by the Institutional Review Board of Colombia’s Centro Internacional de Entrenamiento e Investigaciones (CIDEIM) and the Centers for Disease Control and Prevention (CDC) provided approval for its staff to provide technical support for the study under non-research category. Blood samples were collected once a signed, written consent was obtained from patients. In the case of children, a signed written consent from parents or guardians in addition to an assent from children was obtained prior to sample collection.
Sample Collection
Dried blood spot samples were prospectively collected from patients with uncomplicated and microscopically confirmed P. falciparum infections residing in three malaria endemic Departments in Colombia. Blood samples were collected between October 2008 and June 2009 from the Department of Cordoba (N = 20), which is located in northwestern Colombia, and from Nariño (N = 35) and Valle del Cauca (N = 35) Departments, both of which are located along the Pacific West coast. Additionally, filter paper blood spot samples collected from patients residing in the southeastern Departments of Amazonas (N = 21), Guaviare (N = 3) and Meta (N = 1) during epidemiological studies carried out between 1999 and 2007 were also included in this study. Amazonas and Meta Departments report relatively fewer numbers of malaria cases annually [19]. In total, 115 samples collected from six Departments were used (Fig 1).
Fig 1. Map of Colombia showing the six departments where patient samples were collected.
A total of 115 samples were collected from Nariño (N = 35), Valle del Cauca (N = 35) and Cordoba (N = 20) between 2008 and 2009, and from Amazonas (N = 21), Guaviare (N = 2) and Meta (N = 1) between 1999 and 2007. Blue dots indicate the specific sites where the samples were collected in each department. Map adapted from http://d-maps.com/carte.php?num_car=15145&lang=es.
Microscopy and Rapid Diagnostic Test Analyses
The 90 blood samples collected from Cordoba, Nariño and Valle were used to prepare Giemsa-stained thick and thin smears and filter paper blood spots (Whatman FTA card and Whatman 3MM, Piscataway, NJ, USA) and for testing with malaria RDTs. After blood collection, all patients received antimalarial treatment according to Colombia’s national guidelines for malaria based on the microscopic diagnosis at the time of presentation (independent of the study results). Thick and thin smears were stained using 5% and 10% Giemsa stain, respectively, for 15 minutes. Stained blood smears were examined using light microscopy by laboratory staff in local clinics and the microscopy results were confirmed by an expert microscopist at CIDEIM. Parasitemia was calculated by counting the number of parasites observed per 200 leukocytes, and assuming a total of 8,000 leukocytes per microliter.
All blood samples were also simultaneously tested using two different malaria RDTs in the field. One test was the PfHRP2-based First Response Malaria Ag HRP2 RDT (Premier Medical Corporation Ltd, Nani Danam, India) and the second was a pLDH-specific Advantage MAL card pLDH (J. Mitra & Co. Pvt Ltd, New Delhi, India). The RDT assays were performed and the results interpreted following the instructions provided by the manufacturers at each site.
Extraction of Parasite DNA and PCR Analysis
The genomic DNA used for molecular analysis was extracted from filter paper blood spots using the Qiagen DNA extraction kit (QIAGEN, Valencia, California USA). Before conducting molecular analysis for the presence of pfhrp2, pfhrp3 and contiguous flanking genes, each sample was first tested for the successful amplification of merozoite surface protein (msp)1, msp2 and glutamate-rich protein (glurp) genes (for samples collected 1999–2007) and msp2 and 18S rRNA [20] genes (for samples collected 2008–2009) by nested PCR. Testing for pfhrp2, pfhrp3 and their respective flanking genes were then conducted on samples that met our inclusion criteria of positive amplifications of msp1, msp2, and glurp or msp2 and 18S rRNA.
pfhrp2, pfhrp3 and flanking gene amplifications were performed in 20 μl total volume consisting of 10X buffer with 15mM MgCl2, 200 μM dNTPs, 15 μM forward and reverse primers, 0.69 units of Taq Polymerase (Roche, F. Hoffman-LaRoche Ltd, Basel, Switzerland), and 2 μl of DNA template. An in vitro cultured P. falciparum parasite isolate from the Amazon region of Peru was used as a positive control for all pfhrp2, pfhrp3, and flanking gene amplification experiments. Genomic DNA from cultured Dd2 (5ng/μL) was used as the negative control for all PCR experiments because this isolate lacks pfhrp2 [21] and its flanking genes [9,11]. Dd2 was also used as a positive control for all the PCR experiments on pfhrp3 and its flanking genes because it has retained these genes. Similarly, genomic DNA from cultured parasite isolate HB3 (5ng/μL) (A clone from a CDC parasite strain, Honduras I, isolated from a person who travelled to Honduras) was used as the negative control for all pfhrp3 and flanking gene amplifications because pfhrp3 [22] and its flanking genes [9] were reported to be absent in this isolate. Additionally, HB3 was used as a positive control for all PCR experiments on pfhrp2 and its flanking genes because these genes were present in this isolate. Primers and reaction conditions used and expected PCR product sizes have been described previously [18]. All PCR products were separated and visualized on a 2% agarose gel.
For all PCR experiments, a positive gene amplification was recorded as final. When a negative result was obtained, the amplification was repeated for confirmation. If the result from the second amplification was concordant with the first result indicating no gene product amplification, the result was scored as negative. However, if the second result was discordant with the first, the PCR was performed a third time and the two matching results out of three reported as the final result.
Microsatellite Genotyping and Cluster Analysis
Microsatellite markers were genotyped using whole genome amplified DNA. The whole-genome amplification was performed using 5 μl of genomic DNA per reaction and the Repli-G amplification kit (Qiagen, Valencia, CA, USA). Seven neutral microsatellites were selected for this study so as to determine the population structure of parasites from these sites based on previous studies [23,24]. These microsatellites correspond to the following loci: TA1 and TA109, which are both located on chromosome 6; Poly-α (chromosome 4); PfPK2 (chromosome 12) and 2490 (chromosome 10)[23,25–28]; C2M34 (chromosome 2) and C3M69 (chromosome 3) and amplified using primers and conditions as described [11,29]. The amplification products were labeled with fluorescent dyes (FAM or HEX) and their sizes assayed by capillary electrophoresis on an Applied Biosystems 3130 xl sequencer. The fragments were then scored using GeneMapper software v.3.7 (Applied Biosystems, Foster City, CA, USA) with default microsatellite settings, where allele peaks that were lower than 200 relative fluorescence units (rfu) were defined as background. Allele peaks that were greater than 33% of the height of the predominant allele (which had the highest peak) were scored as additional alleles. When more than one allele was identified in a locus, the sample was deemed to be infected with two or more genetically distinct clones. Samples that did not amplify alleles at some loci on the first attempt were re-tested to get complete data. Only those samples presumed to be infected by a single parasite strain (defined as the amplification of only one allele at each of the seven neutral microsatellite loci) were used for cluster analysis.
To evaluate whether pfhrp2- (and pfhrp3-) negative isolates had similar genetic backgrounds and if the microsatellite haplotypes we identified clustered according to the geographic origins of the parasite isolates, we applied the Bayesian model-based algorithm implemented in Structure v2.3.3 software [30]. Structure uses a clustering approach to assign isolates to K populations characterized by a set of allele frequencies at each locus. We used the same parameters as described previously [11] to test the likelihood of finding between one and ten clusters (K = 1 to K = 10). We selected these values of K based on previous reports of the numbers of distinct sub-populations identified in other South American countries such as Peru [11,24,31] and Colombia [32]. The most likely number of clusters (K) was estimated as the value of K at the plateau of the mean estimated natural log of the probability estimates of the data [LnP(D)] calculated using the Evanno method [33] and output from the Structure Harvester program [34].
Results
Genetic deletion of pfhrp2, pfhrp3 and their flanking genes
Fifteen of the 115 patient samples collected were excluded from genotyping analysis because they failed to amplify one or more of msp1, msp2 and glurp or msp2 and18s rRNA. The remaining 100 samples were analyzed for the presence of pfhrp2, pfhrp3 and their respective flanking genes.
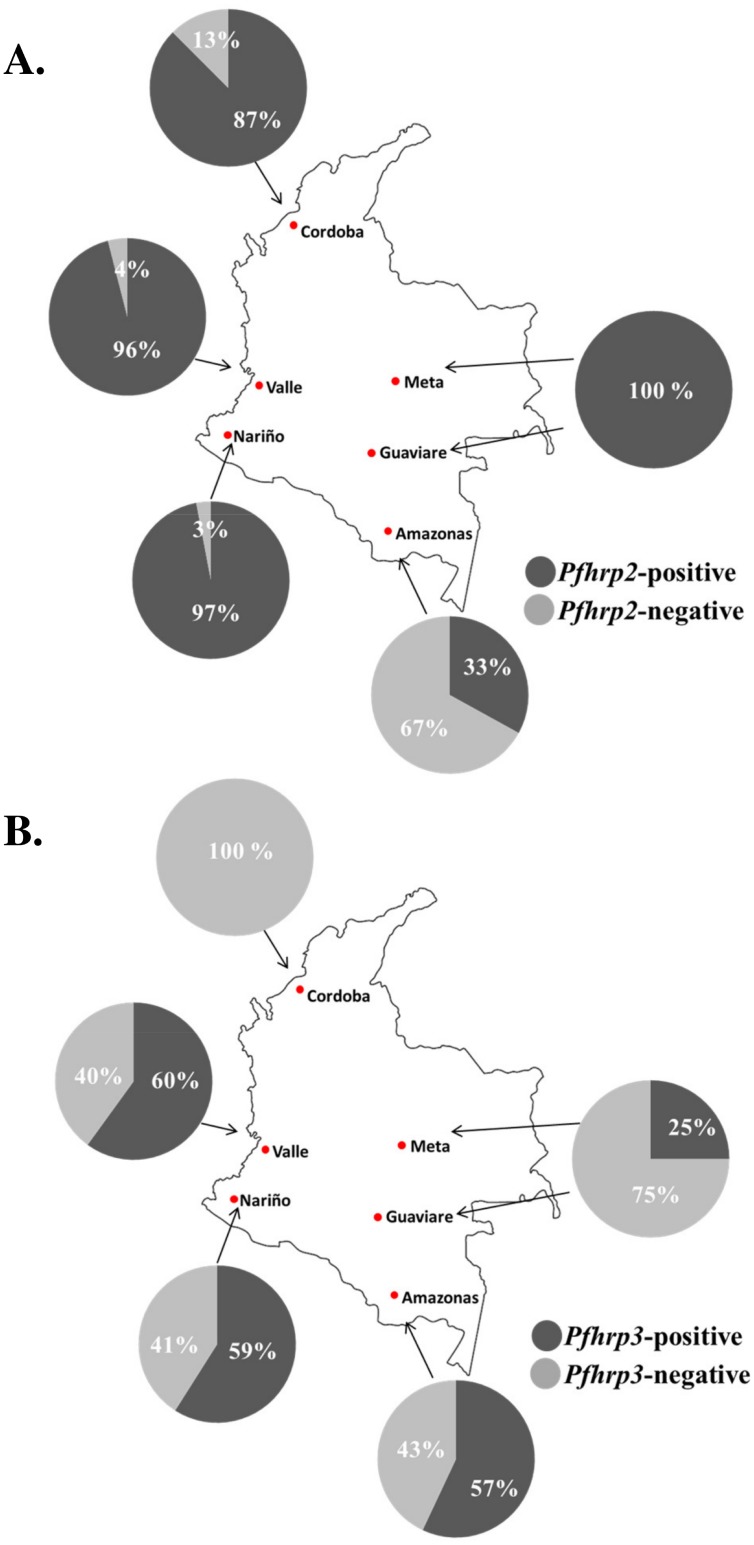
We found that 18 (18%) of the isolates genotyped were negative for pfhrp2 while 52 (52%) were lacking pfhrp3 (Fig 2). A large proportion (14 of 18) of the pfhrp2-negative isolates were collected in Amazonas Department while two (sample IDs TA03 and TA08) were from Cordoba, and one isolate each was collected from Nariño (TU005) and Valle del Cauca (BV22) (Fig 3). The highest proportion of pfhrp3 deletion mutants was found in Cordoba Department where none of the 16 samples tested showed amplification of pfhrp3 (Fig 3B). In Valle, Nariño, and Amazonas Departments, the proportions of parasites with pfhrp3 deletions were 40%, 41% and 43%, respectively. In Meta and Guaviare Departments combined, in 3 of the 4 samples tested pfhrp3 was not amplified.
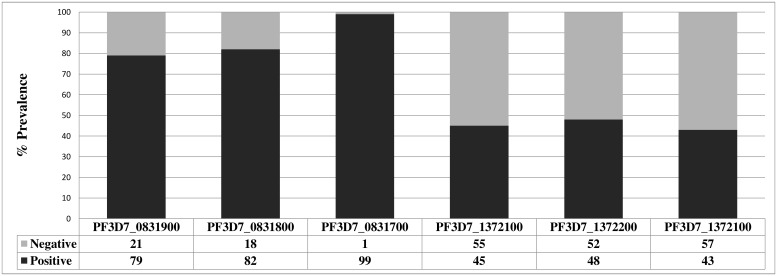
Fig 2. Gene amplification results for pfhrp2, pfhrp3 and their respective flanking genes in P. falciparum isolates from Colombia.
Fig 3. Prevalence of (A) pfhrp2- and (B) pfhrp3-deleted P. falciparum isolates in Amazonas (N = 21), Cordoba (N = 16), Valle (N = 25), Nariño (N = 34) and Guaviare-Meta (N = 4).
Overall, 13% of all isolates included deletions of both pfhrp2 and pfhrp3 genes (Table 1). Nine of these 13 samples were collected in Amazonas department, while two were from Cordoba, and one each originated from Nariño and Valle. Only five samples were pfhrp2-negative and pfhrp3-positive, and all five were collected in Amazonas Department.
Table 1. Results of PCR amplification of pfhrp2, pfhrp3 and their respective flanking genes in P. falciparum samples collected in Colombia.
| PF3D7_0831900 | pfhrp2 | PF3D7_0831700 | PF3D7_1372100 | pfhrp3 | PF3D7_1372400 | N |
|---|---|---|---|---|---|---|
| + | + | + | - | - | - | 25 |
| + | + | + | + | + | + | 16 |
| + | + | + | - | + | + | 15 |
| - | + | + | + | + | + | 10 |
| + | + | + | + | - | - | 8 |
| + | - | + | + | - | - | 6 |
| + | - | + | - | - | - | 4 |
| - | + | + | - | - | - | 4 |
| + | - | + | + | + | - | 4 |
| - | - | + | - | - | - | 2 |
| - | - | - | - | - | - | 1 |
| - | + | + | + | - | - | 1 |
| + | + | + | - | + | - | 1 |
| - | - | + | - | + | - | 1 |
| - | + | + | - | - | + | 1 |
| - | + | + | - | + | + | 1 |
| Total | 100 | |||||
Sixteen different pfhrp2 and pfhrp3 deletion patterns were observed in our samples (Table 1). A greater proportion of parasite isolates had deleted the gene located 5’ of pfhrp2, PF3D7_0831900, compared to the 3’ flanking gene, PF3D7_0831700 (Fig 2). In contrast, there were an almost equal proportion of PF3D7_1372100 gene deletions (upstream of pfhrp3) as there were of PF3D7_1372400 deletions (downstream of pfhrp3) (Fig 2).
Malaria RDT performance
In order to corroborate the results from our PCR-based genetic deletion analyses, samples collected from Cordoba, Nariño and Valle Departments (N = 90) at the time of blood sampling were tested using a PfHRP2-based RDT. Additionally, pLDH-based RDTs were also used to detect all P. falciparum parasites regardless of their pfhrp2 gene deletion status. RDT results for five samples were considered invalid because the control line was reported as negative. Therefore, 85 samples had valid RDT results.
One of the 85 samples (TU009) tested negative with the First Response Malaria Ag HRP2-based test, although the PCR based assay tested positive for pfhrp2. However, this specimen was found to have only mature sexual-stage parasites present (Table 2). Three of the 85 samples (TA05, TA10 and TU035) tested negative with the Advantage MAL card pLDH-based RDT (Table 2). TA05 and TA10 had less than 1,000 parasites/μl (Table 2).
Table 2. Results for samples for which discordant results were obtained.
Pos—Positive result; Neg—Negative result; ND—Sample was not tested.
| State of Collection | SampleID | pfhrp2 PCR | pfhrp3 PCR | Parasitemia (p/μl) | First Response (PfHRP2) | Advantage MalCard (pLDH) |
|---|---|---|---|---|---|---|
| Cordoba | TA03 | Neg | Neg | 20,515 | Pos | Pos |
| Cordoba | TA08 | Neg | Neg | 2743 | Pos | Pos |
| Nariño | TU005 | Neg | Neg | 168 | Pos | Pos |
| Valle | BV22 | Neg | Neg | ND | ND | Pos |
| Nariño | TU009 | Pos | Pos | 1120 (only sexual stages) | Neg | Pos |
| Cordoba | TA05 | Pos | Pos | 558 | Pos | Neg |
| Cordoba | TA10 | Pos | Pos | 262 | Pos | Neg |
| Nariño | TU035 | Pos | Pos | 3675 | Pos | Neg |
We noted that three of the four isolates collected outside of Amazonas Department (TA03, TA08 and TU005) that were determined to be pfhrp2 negative by PCR, as well as pfhrp3 negative, tested positive for the HRP2 protein using the PfHRP2-based RDT kit and also positive for pLDH using the Advantage MalCard RDT (Table 2).
Cluster Analysis
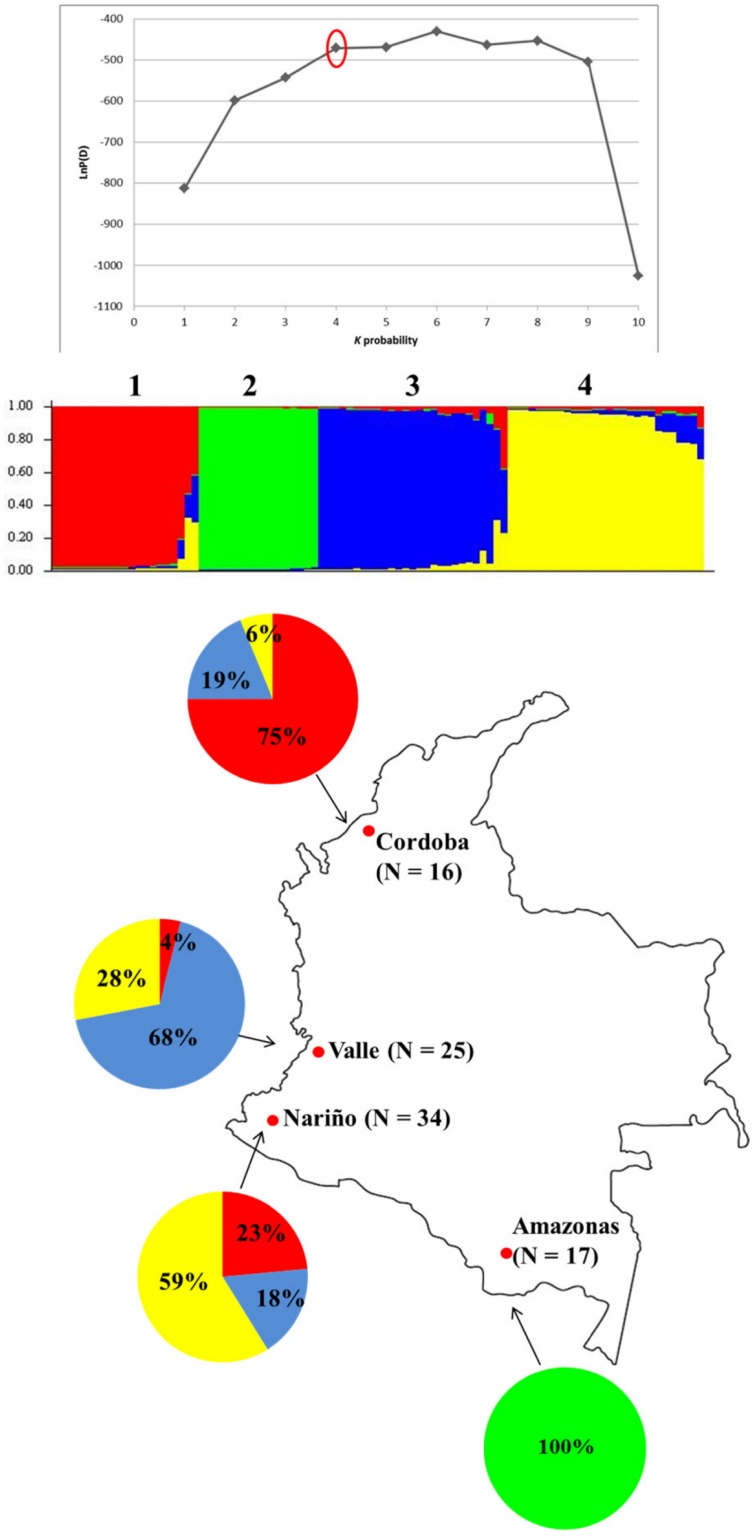
We genotyped seven neutral microsatellite loci in singly infected isolates that met our inclusion criteria (N = 92) and performed cluster analysis to investigate the association between the geographic origins of the P. falciparum isolates, their pfhrp2/pfhrp3 deletion status and their membership in the groups predicted by Structure software. Cluster analysis inferred population substructure in this group of isolates and the number of population clusters (K) was predicted to be four (Fig 4).
Fig 4. Population structure of P. falciparum-infected samples from Colombia (N = 104).
(A) Plot of Var[LnP(D) vs. K probability showing the best K subpopulation partition at K = 4. (B) Output from Structure v2.3.3. Each color corresponds to a population (labeled 1 to 4) classified by Structure. Each individual isolate is represented by a vertical bar. The Y axis represents the estimated proportion of membership of an individual to each predicted population cluster. The number of isolates assigned to each cluster were as follows: Cluster 1 (N = 21); 2 (N = 17); 3 (N = 26); 4 (N = 28). (c). Distribution of the four clusters across the four departments. Red—Cluster 1; Green—Cluster 2; Blue—Cluster 3; Yellow—Cluster 4. The total number of samples analyzed from each department is shown in parentheses.
Generally, the parasite isolates appeared to cluster based on their in-country geographic origins. All 17 isolates (100%) assigned to cluster 2 originated only from Amazonas Department (Fig 4B and 4C). More than half (59%) of the 34 parasite isolates collected in Nariño Department could be assigned to cluster 4, while 17 isolates or 68% of those specimens collected in Valle were assigned to cluster 3 (Fig 4B and 4C). Three quarters of the isolates (12) from Cordoba were assigned to cluster 1 (Fig 4B and 4C).
The distribution of pfhrp2- and pfhrp3-negative isolates among the clusters was skewed; we observed that 12 of the 18 pfhrp2-negative isolates (67%) were assigned to cluster 2, which consisted solely of samples from Amazonas Department (Figs 3A and 4B). Three other pfhrp2-negative isolates were each assigned to clusters 1, 3 and 4. Moreover, eight of the 13 pfhrp2/pfhrp3-double negative isolates (61.5%) were also designated to cluster 2. Whereas Structure analysis of the neutral microsatellite allele lengths for samples in cluster 2 predicted the membership of these samples solely to that cluster, some samples assigned to clusters 1, 3 and 4 appeared to have varying levels of admixture indicated by multi-colored bars which showed their relative probability of assignment to more than one cluster (Fig 4B).
Discussion
Overall, this study has shown that pfhrp2-deleted parasites are highly prevalent in Amazonas department, but rarely found in the coastal sites that were examined. This finding suggests that PfHRP2-based RDTs are likely to detect most P. falciparum parasites in Cordoba, Valle del Cauca and Nariño, but not in Amazonas Department, where we detected a 67% deletion rate for pfhrp2 among the limited number of P. falciparum isolates analyzed. This high prevalence of pfhrp2 (and pfhrp3) deletions in samples from Amazonas, was considerably higher compared to the other sites surveyed in Colombia (67% vs 5.0%, respectively). This deletion rate of 5% for pfhrp2 may actually be lower as three of the four non-Amazonas isolates that tested negative for pfhrp2 by PCR were initially positive by an HRP2-based RDT (see below). The presence of parasites with pfhrp2 deletions in Colombia, especially in Amazonas, supports the previous observations that these deletions are more frequent in South America [9–13] compared with other regions where this phenomenon has been investigated [14–17].
Our results also show that pfhrp3 deletions are more prevalent than pfhrp2 deletions in Colombia, which also has been found to be the case in Peru and Honduras [9,11,18]. Interestingly, this is not the case in Suriname where pfhrp2-negative parasites were detected in higher numbers than pfhrp3-negative isolates [13]. Whereas pfhrp2-negative parasites were mostly limited to the Amazon region located on the border with Peru, pfhrp3-negative isolates were distributed across all six departments surveyed. Overall, outside of Amazonas the prevalence of pfhrp3 deletions was 54% compared to 43% within the Department of Amazonas.
Two important questions that arise are why there are multiple patterns of deletion within the region of pfhrp2 and pfhrp3 flanking genes and if there is an orderly pattern for such deletions. It is evident from a previously published study using tiling array that deletion of parts of chromosomal segments within 20 kb of both pfhrp2 and pfhrp3 occurs in natural P. falciparum isolates obtained from Peru [35]. The patterns of deletion varied among the limited isolates studied. In terms of physical location, pfhrp3 is proximal to the end of the chromosome 13 while pfhrp2 is located in the subtelomeric region of chromosome 8. It has been proposed that some subtelomeric regions of the chromosome of P. falciparum laboratory and field isolates are the target of deletional activity which is then accompanied by repair mechanisms via enzymes such as telomerases [36–39]. Thus, it is not clear at this time if pfhrp2 and/or pfhrp3 deletion are driven by any specific mechanism or if they are due to some broad chromosomal deletion events occurring in selected regions of the genome where these genes are located. Clearly, further studies using next generation sequencing methods are needed to answer mechanisms associated with these genetic deletions.
The results from this study may provide some context to a recent report from Colombia in which the in vitro susceptibility of P. falciparum parasites to various antimalarial drugs was tested [40]. The study utilized schizont maturation and PfHRP2-ELISA methods as read-outs for their assays [40]. It was determined that PfHRP2 could not be detected by ELISA in sixteen out of twenty samples (65%) collected in Leticia (a site located in Amazonas Department) even though the schizont maturation method was able to yield results with these samples [40]. This observation is consistent with current findings indicating deletion of pfhrp2 gene in a majority of samples (67%) in the Amazonas Department.
The results from microsatellite-based genetic diversity data indicate that the P. falciparum population in Colombia has undergone a bottleneck or bottlenecks event sometime in the recent past. Overall, the parasite population in Colombia from analysis of our genetic data appears to be comprised of four major clusters. This finding is consistent with a recent SNP study in Colombia that showed the presence of four clusters of P. falciparum parasites in samples collected from four departments located along Colombia’s Pacific coast (Cauca, Chocó, Valle and Nariño) [32]. Geographic clustering was also apparent in our sample set; one of these four clusters consisted only of isolates collected from Amazonas Department while the majority of isolates in each of the other three clusters originated from specific Departments, Nariño, Valle and Cordoba. Importantly, most of the pfhrp2 deleted parasites were assigned to cluster 2, which consisted of isolates from Amazonas Department. It is likely that this may be due to the clonal expansion of a pfhrp2-deleted lineage. Overall, these findings in Colombia are similar to those from Peru where all deletions of pfhrp2 were found in different frequencies in various geographical locations within the Amazon River basin of Peru. As noted above, given that the Department of Amazonas in Colombia is contiguous with the same ecological zone in Peru, it is possible that the pfhrp2-negative isolates in Colombia are genetically related to some of the pfhrp2-negative parasite isolates circulating in the Peruvian Amazon. Even though the prevalence of pfhrp2-negative parasites is low outside of Amazonas Department, migration events could lead to their spread to other departments in Colombia as was the case for some sulphadoxine-pyrimethamine- resistant parasites [41].
It should be noted, however, that these microsatellite analyses were only performed on samples from Cordoba, Valle, Nariño and Amazonas. Therefore, in order to better elucidate the effect of geographic origin on allele diversity, future studies would require analysis of samples collected from other Departments such as Antioquia, Cauca and Chocó, which have relatively higher prevalence of P. falciparum malaria [19]. In addition, given the results obtained from this study, a larger sampling from regions such as Guaviare and Meta will likely provide greater insights.
We did note some discrepancies in results between the PfHRP2-based RDTs and PCR genotyping for three samples, where the PCR-based genotyping produced a negative result for pfhrp2 while a PfHRP2-based RDT produced positive results. One interpretation of this result is that the PCR test was not able to detect the Pfhrp2 gene that were indeed present, as evidenced by the positive HRP2-based RDT, in these three samples, which originated from the coastal region. This possible failure in the PCR could have occurred if mutations in the priming site complementary to the 3’ end of the PCR primer were present in the samples. The high polymorphism in the pfhrp2 gene found in clinical isolates could support this hypothesis [42]. Another possible explanation is that the results of the PfHRP2-based and pLDH- based RDTs might have been interpreted incorrectly or gave a false positive result, such as has been noted in the past for PfHRP2-based RDTS tested with blood specimens containing with rheumatoid factor (RF). However, PfHRP2-based RDT used in this study is one of the top performing commercial malaria tests with a very high specificity, which makes the occurrence of false positives at this frequency very unlikely. Also, Advantage MalCard pLDH-based RDT were positive, reducing the possibility of the false positive due to RDT factors. Detecting genetic deletions of pfhrp2 and pfhrp3 using PCR requires caution because the absence of a PCR amplified product is being investigated. There are only three short conserved regions in the pfhrp2 and pfhrp3 genes from where primers can be selected, which hampers optimizing for the most robust amplifications possible. And therefore, any loss of DNA through partial degradation or lower parasitemia will compromise obtaining true negative results. In our experience, DNA isolated directly from blood performs significantly better for amplifying the pfhrp2 (or pfhrp3) gene compared to DNA isolated from blood spotted on filter paper, especially, if the paper is not of highest quality and not stored dessicated at or below 4°C. For logistical reasons, only filter paper blood spots were available for this study, and it is therefore possible that this may have contributed to these discordant results. It is very difficult to rule out false negative test results using PCR data alone; complementing gene amplification data with PfHRP2 protein detection for confirmation is ideal. Since we did not have plasma samples available, ELISA confirmatory testing could not be performed. On the other hand, RDT testing can provide additional supporting data, although most samples but not all samples were tested with RDTs in this study.
This study shows that pfhrp2-negative P. falciparum isolates are present in Colombia, mostly in the Amazon region. Regular monitoring for this parasite population will inform national policy on the utilization of PfHRP2-based RDTs for malaria detection in areas where microscopy is not available. Nevertheless, this study had some limitations. For one, samples were collected only from some of the Departments where P. falciparum occurs in Colombia and our findings cannot necessarily be extrapolated to all parts of the country. Moreover, sampling and the type of specimens obtained were done based on logistical convenience and the number of samples from some sites was limited. Furthermore, a proportion of the samples reported here were collected between 1999 and 2007 for other study purposes. A larger and more systematic collection and analysis of parasite isolates from Amazonas and other parts of the country, whether along the coastal regions or in the interior, will clarify the current prevalence and distribution of P. falciparum isolates with pfhrp2 and pfhrp3 deletions in the country overall.
Acknowledgments
To Unidad Ejecutora de Saneamiento del Valle del Cauca, Instituto departamental de salud de Nariño- sede Tumaco, Secretaria de Salud Municipal de Tierralta, Cordoba, Secretaria de Salud del Amazonas. We also acknowledge the support of the Amazon Malaria Initiative, which is financially supported by the United States Agency for International Development. The support of Pan American Health Organization is appreciated. C.M.S was supported by a Doctoral Fellowship from the Instituto Colombiano para el Desarrollo de la Ciencia y la Tecnología Francisco José de Caldas, Colciencias (No.512-2010). S.A.O was partly supported by the CDC based American Society for Microbiology Postdoctoral Fellowship. We acknowledge the partial funding support of Atlanta Research and Educational Foundation in performing the laboratory work.
Data Availability
All relevant data are within the paper.
Funding Statement
Sample collection and training were supported by Foundation for Innovative New Diagnostics. Genotyping experiments and travel were supported by the Amazon Malaria Initiative, which is funded by the United States Agency for International Development. Instituto Colombiano para el Desarrollo de la Ciencia y la Tecnología Francisco José de Caldas, Colciencias supported CMS (No.512-2010). CDC based American Society for Microbiology Postdoctoral Fellowship partly supported SAO. Atlanta Research and Educational Foundation partly supported the laboratory work. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization. (2013) World malaria report 2013. Geneva, Switzerland. Available: http://www.who.int/malaria/publications/world_malaria_report/en/.
- 2.Pan American Health Organization. (2011.) Report on the situation of malaria in the americas, 2011. Available: http://www.paho.org/hq/index.php?option=com_content&view=article&id=2459%3Areport-on-situation-malaria-americas-2011.
- 3. Ospina OL, Cortes LJ, Cucunuba ZM, Mendoza NM, Chaparro P. Characterization of the national malaria diagnostic network, Colombia, 2006–2010. Biomedica. 2012;32 Suppl 1: 46–59. [DOI] [PubMed] [Google Scholar]
- 4. Cheng Q, Gatton ML, Barnwell J, Chiodini P, McCarthy J, Bell D, et al. Plasmodium falciparum parasites lacking histidine-rich protein 2 and 3: a review and recommendations for accurate reporting. Malar J. 2014;13: 283-2875-13-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. (2012) Malaria rapid diagnostic test performance. results of WHO product testing of malaria RDTs round 4. Available: http://www.who.int/malaria/publications/rapid_diagnostic/en/.
- 6. Bell DR, Wilson DW, Martin LB. False-positive results of a Plasmodium falciparum histidine-rich protein 2-detecting malaria rapid diagnostic test due to high sensitivity in a community with fluctuating low parasite density. Am J Trop Med Hyg. 2005;73: 199–203. [PubMed] [Google Scholar]
- 7. Chiodini PL, Bowers K, Jorgensen P, Barnwell JW, Grady KK, Luchavez J, et al. The heat stability of Plasmodium lactate dehydrogenase-based and histidine-rich protein 2-based malaria rapid diagnostic tests. Trans R Soc Trop Med Hyg. 2007;101: 331–337. [DOI] [PubMed] [Google Scholar]
- 8. Rennie W, Phetsouvanh R, Lupisan S, Vanisaveth V, Hongvanthong B, Phompida S, et al. Minimising human error in malaria rapid diagnosis: clarity of written instructions and health worker performance. Trans R Soc Trop Med Hyg. 2007;101: 9–18. [DOI] [PubMed] [Google Scholar]
- 9. Gamboa D, Ho MF, Bendezu J, Torres K, Chiodini PL, Barnwell JW, et al. A large proportion of P. falciparum isolates in the Amazon region of Peru lack pfhrp2 and pfhrp3: implications for malaria rapid diagnostic tests. PLoS One. 2010;5: e8091 10.1371/journal.pone.0008091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Maltha J, Gamboa D, Bendezu J, Sanchez L, Cnops L, Gillet P, et al. Rapid diagnostic tests for malaria diagnosis in the Peruvian Amazon: impact of pfhrp2 gene deletions and cross-reactions. PLoS One. 2012;7: e43094 10.1371/journal.pone.0043094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Akinyi S, Hayden T, Gamboa D, Torres K, Bendezu J, Abdallah JF, et al. Multiple genetic origins of histidine-rich protein 2 gene deletion in Plasmodium falciparum parasites from Peru. Sci Rep. 2013;3: 2797 10.1038/srep02797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Houze S, Hubert V, Le Pessec G, Le Bras J, Clain J. Combined deletions of pfhrp2 and pfhrp3 genes result in Plasmodium falciparum malaria false-negative rapid diagnostic test. J Clin Microbiol. 2011;49: 2694–2696. 10.1128/JCM.00281-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Akinyi Okoth S, Abdallah JF, Ceron N, Adhin MR, Chandrabose J, Krishnalall K, et al. Variation in Plasmodium falciparum Histidine-Rich Protein 2 (Pfhrp2) and Plasmodium falciparum Histidine-Rich Protein 3 (Pfhrp3) Gene Deletions in Guyana and Suriname. PLoS One. 2015;10: e0126805 10.1371/journal.pone.0126805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ramutton T, Hendriksen IC, Mwanga-Amumpaire J, Mtove G, Olaosebikan R, Tshefu AK, et al. Sequence variation does not confound the measurement of plasma PfHRP2 concentration in African children presenting with severe malaria. Malar J. 2012;11: 276-2875-11-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Koita OA, Doumbo OK, Ouattara A, Tall LK, Konare A, Diakite M, et al. False-negative rapid diagnostic tests for malaria and deletion of the histidine-rich repeat region of the hrp2 gene. Am J Trop Med Hyg. 2012;86: 194–198. 10.4269/ajtmh.2012.10-0665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wurtz N, Fall B, Bui K, Pascual A, Fall M, Camara C, et al. Pfhrp2 and pfhrp3 polymorphisms in Plasmodium falciparum isolates from Dakar, Senegal: impact on rapid malaria diagnostic tests. Malar J. 2013;12: 34-2875-12-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kumar N, Pande V, Bhatt RM, Shah NK, Mishra N, Srivastava B, et al. Genetic deletion of HRP2 and HRP3 in Indian Plasmodium falciparum population and false negative malaria rapid diagnostic test. Acta Trop. 2013;125: 119–121. 10.1016/j.actatropica.2012.09.015 [DOI] [PubMed] [Google Scholar]
- 18. Abdallah JF, Okoth SA, Fontecha GA, Torres RE, Banegas EI, Matute ML, et al. Prevalence of pfhrp2 and pfhrp3 gene deletions in Puerto Lempira, Honduras. Malar J. 2015;14: 19-014-0537-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chaparro P, Padilla J, Vallejo AF, Herrera S. Characterization of a malaria outbreak in Colombia in 2010. Malar J. 2013;12: 330-2875-12-330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Singh B, Bobogare A, Cox-Singh J, Snounou G, Abdullah MS, Rahman HA. A genus- and species-specific nested polymerase chain reaction malaria detection assay for epidemiologic studies. Am J Trop Med Hyg. 1999;60: 687–692. [DOI] [PubMed] [Google Scholar]
- 21. Wellems TE, Walker-Jonah A, Panton LJ. Genetic mapping of the chloroquine-resistance locus on Plasmodium falciparum chromosome 7. Proc Natl Acad Sci U S A. 1991;88: 3382–3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wellems TE, Walliker D, Smith CL, do Rosario VE, Maloy WL, Howard RJ, et al. A histidine-rich protein gene marks a linkage group favored strongly in a genetic cross of Plasmodium falciparum. Cell. 1987;49: 633–642. [DOI] [PubMed] [Google Scholar]
- 23. Anderson TJ, Haubold B, Williams JT, Estrada-Franco JG, Richardson L, Mollinedo R, et al. Microsatellite markers reveal a spectrum of population structures in the malaria parasite Plasmodium falciparum. Mol Biol Evol. 2000;17: 1467–1482. [DOI] [PubMed] [Google Scholar]
- 24. Griffing SM, Mixson-Hayden T, Sridaran S, Alam MT, McCollum AM, Cabezas C, et al. South American Plasmodium falciparum after the malaria eradication era: clonal population expansion and survival of the fittest hybrids. PLoS One. 2011;6: e23486 10.1371/journal.pone.0023486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Anderson TJ, Su XZ, Bockarie M, Lagog M, Day KP. Twelve microsatellite markers for characterization of Plasmodium falciparum from finger-prick blood samples. Parasitology. 1999;119 (Pt 2): 113–125. [DOI] [PubMed] [Google Scholar]
- 26. dalla Martha RC, Tada MS, Ferreira RG, da Silva LH, Wunderlich G. Microsatellite characterization of Plasmodium falciparum from symptomatic and non-symptomatic infections from the Western Amazon reveals the existence of non-symptomatic infection-associated genotypes. Mem Inst Oswaldo Cruz. 2007;102: 293–298. [DOI] [PubMed] [Google Scholar]
- 27. Hoffmann EH, Ribolla PE, Ferreira MU. Genetic relatedness of Plasmodium falciparum isolates and the origin of allelic diversity at the merozoite surface protein-1 (MSP-1) locus in Brazil and Vietnam. Malar J. 2003;2: 24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Machado RL, Povoa MM, Calvosa VS, Ferreira MU, Rossit AR, dos Santos EJ, et al. Genetic structure of Plasmodium falciparum populations in the Brazilian Amazon region. J Infect Dis. 2004;190: 1547–1555. [DOI] [PubMed] [Google Scholar]
- 29. McCollum AM, Mueller K, Villegas L, Udhayakumar V, Escalante AA. Common origin and fixation of Plasmodium falciparum dhfr and dhps mutations associated with sulfadoxine-pyrimethamine resistance in a low-transmission area in South America. Antimicrob Agents Chemother. 2007;51: 2085–2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pritchard JK, Stephens M, Donnelly P. Inference of population structure using multilocus genotype data. Genetics. 2000;155: 945–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Branch OH, Sutton PL, Barnes C, Castro JC, Hussin J, Awadalla P, et al. Plasmodium falciparum genetic diversity maintained and amplified over 5 years of a low transmission endemic in the Peruvian Amazon. Mol Biol Evol. 2011;28: 1973–1986. 10.1093/molbev/msq311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Echeverry DF, Nair S, Osorio L, Menon S, Murillo C, Anderson TJ. Long term persistence of clonal malaria parasite Plasmodium falciparum lineages in the Colombian Pacific region. BMC Genet. 2013;14: 2-2156-14-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Evanno G, Regnaut S, Goudet J. Detecting the number of clusters of individuals using the software STRUCTURE: a simulation study. Mol Ecol. 2005;14: 2611–2620. [DOI] [PubMed] [Google Scholar]
- 34. Earl DA, VonHoldt BM (2011) STRUCTURE HARVESTER: A website and program for visualizing STRUCTURE output and implementing the Evanno method. Conservation Genetics Resources. [Google Scholar]
- 35. Dharia NV, Plouffe D, Bopp SE, Gonzalez-Paez GE, Lucas C, Salas C, et al. Genome scanning of Amazonian Plasmodium falciparum shows subtelomeric instability and clindamycin-resistant parasites. Genome Res. 2010;20: 1534–1544. 10.1101/gr.105163.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Biggs BA, Kemp DJ, Brown GV. Subtelomeric chromosome deletions in field isolates of Plasmodium falciparum and their relationship to loss of cytoadherence in vitro. Proc Natl Acad Sci U S A. 1989;86: 2428–2432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Shirley MW, Biggs BA, Forsyth KP, Brown HJ, Thompson JK, Brown GV, et al. Chromosome 9 from independent clones and isolates of Plasmodium falciparum undergoes subtelomeric deletions with similar breakpoints in vitro. Mol Biochem Parasitol. 1990;40: 137–145. [DOI] [PubMed] [Google Scholar]
- 38. Scherf A, Mattei D. Cloning and characterization of chromosome breakpoints of Plasmodium falciparum: breakage and new telomere formation occurs frequently and randomly in subtelomeric genes. Nucleic Acids Res. 1992;20: 1491–1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bopp SE, Manary MJ, Bright AT, Johnston GL, Dharia NV, Luna FL, et al. Mitotic evolution of Plasmodium falciparum shows a stable core genome but recombination in antigen families. PLoS Genet. 2013;9: e1003293 10.1371/journal.pgen.1003293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Aponte SL, Diaz G, Pava Z, Echeverry DF, Ibarguen D, Rios M, et al. Sentinel network for monitoring in vitro susceptibility of Plasmodium falciparum to antimalarial drugs in Colombia: a proof of concept. Mem Inst Oswaldo Cruz. 2011;106 Suppl 1: 123–129. [DOI] [PubMed] [Google Scholar]
- 41. Corredor V, Murillo C, Echeverry DF, Benavides J, Pearce RJ, Roper C, et al. Origin and dissemination across the Colombian Andes mountain range of sulfadoxine-pyrimethamine resistance in Plasmodium falciparum. Antimicrob Agents Chemother. 2010;54: 3121–3125. 10.1128/AAC.00036-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Deme AB, Park DJ, Bei AK, Sarr O, Badiane AS, Gueye Pel H, et al. Analysis of pfhrp2 genetic diversity in Senegal and implications for use of rapid diagnostic tests. Malar J. 2014;13: 34-2875-13-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.