Pediatricians have an obligation to protect the health of children and adolescents. Human immunodeficiency-virus (HIV)/AIDS-remains the second leading cause of death for adolescents worldwide and the leading cause for adolescents in sub-Saharan Africa.1 Youth aged 15 to 24 years represent one-third of new infections.2 While AIDS-related mortality declined for adults and children from 2005 to 2012, there was a 50% increase in mortality among HIV-infected adolescents.2 For perinatally HIV-infected youth, worse outcomes largely reflect developmental struggles with treatment adherence they face as they enter adolescence. For adolescents with behaviorally acquired HIV, late diagnosis, poor linkage to and retention in care, low rates of antiretroviral therapy (ART) prescription, and inadequate treatment adherence all affect mortality.2 In the United States, nearly 60% of HIV-infected youth do not know they are infected.3 In sub-Saharan Africa, only 1 in 5 HIV-infected young women knows her status.2
Despite these sobering statistics, the global impact of HIV/AIDS in adolescents has often been invisible. While adolescents constitute an estimated 1.2 billion of the world’s population, adolescent health is often not prioritized in resource-limited settings.2 Pediatricians and other health care professionals receive little training relevant to the unique health needs of adolescents, and youth older than 13 years are often treated as adults. Yet, adolescence is a distinct period of physical, psychosocial, and neurocognitive development that leaves youth highly vulnerable to HIV infection. Autonomy seeking, social pressures, and slow maturation of impulse control lead to increased risk-taking behaviors such as unprotected sex and substance use.1 These same factors render HIV-infected adolescents vulnerable to treatment failure owing to poor adherence. Globally, two-thirds of all new HIV infections among 15- to 19-year-olds occur in young women.2 Child marriage, intimate partner violence, and high school dropout rates limit young women’s power to negotiate sexual decision making. In the United States, most adolescent infections occur among young men who have sex with men and transgender women. For these youth, stigma and discrimination related to sexual and gender identity may increase risk for HIV infection and create substantial barriers to accessing care and/or achieving optimal health outcomes.3
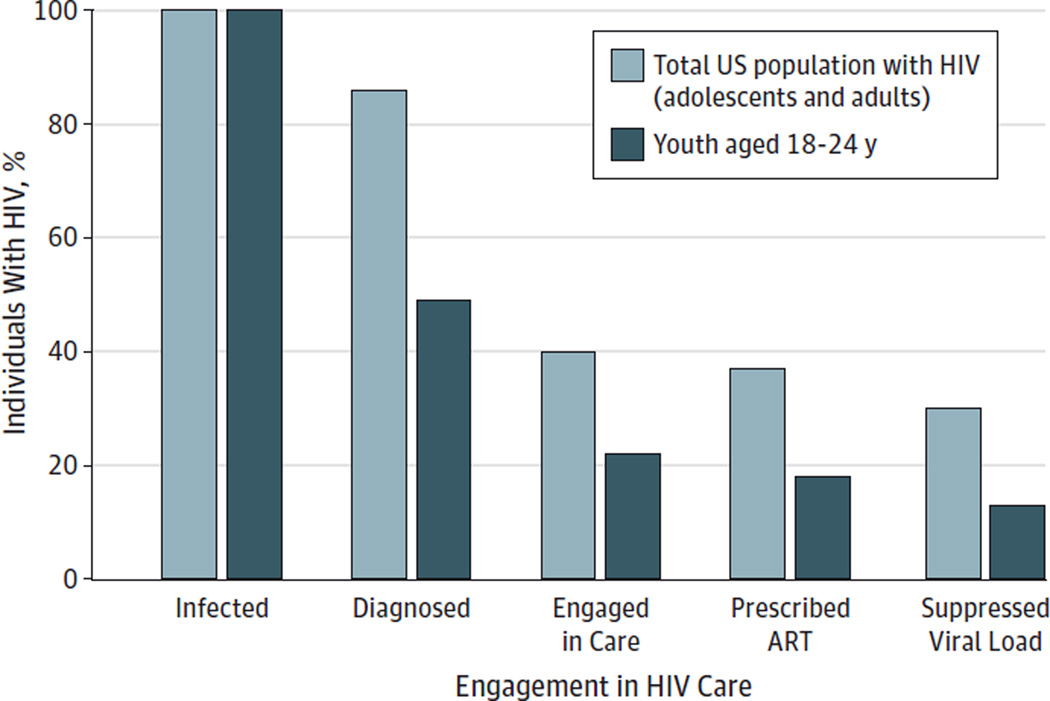
In 2011, the Obama administration heralded a new era in the HIV/AIDS global discourse with the promise that an AIDS-free generation was within reach. This concept is defined as a generation in which there are virtually no perinatal infections, high-impact prevention interventions avert most adolescent infections, and youth who acquire HIV have access to treatment that prevents development of AIDS and forward transmission of HIV.2 Unfortunately, few countries or nongovernmental organizations collect or report data on adolescent-specific HIV/AIDS outcomes. Treatment statistics typically segregate data into age categories of 0 to 14 years and 15 years or older, which obscures our ability to define the scope of the adolescent HIV/AIDS epidemic.2 To optimize adolescent HIV/AIDS care, we need to understand how youth enter and are retained in the HIV treatment continuum—the process of engagement in care that begins with testing and prevention and ends with virologic suppression on ART (Figure). The barriers to success at each step in the continuum need to be recognized and ameliorated. In the United States, estimates suggest that the proportion of HIV-infected adolescents who are tested, retained in care, receiving ART, and virologically suppressed is as low as 6% to 13%, a significantly smaller proportion than among adults.4–6 In resource-limited settings this proportion is unknown, but it is likely even lower.
Figure. Adult and Youth HIV Treatment Continuum in the Total US Population and Specific to Youth.
Estimated proportions of the human immunodeficiency virus (HIV)–infected US population as compared with youth at the various stages of the HIV treatment continuum. ART indicates antiretroviral therapy. Created based on data from the Centers for Disease Control and Prevention.4 Of note, youth estimates do not include adolescents younger than 18 years. Zanoni and Mayer5 estimate the rate of virologic suppression among youth aged 13 to 29 years to be 6%.
Treatment and prevention of adolescent HIV/AIDS should be a global health funding priority. Early initiation of ART improves health outcomes, decreases mortality, and reduces secondary HIV transmission.7,8 As ART access expands for adolescents, it must be accompanied by interventions to engage and retain youth at every stage of the continuum. We first need to define the global adolescent continuum, including younger teens who are historically absent from these statistics. We can then invest in targeted interventions to improve care delivery and treatment adherence support for youth. Rather than envisioning the continuum as a series of steps, we need to invest in models visualizing care as a dynamic process of overlapping stages. Increasing testing rates among adolescents must be matched with programs assisting youth in linking to and navigating care. Similarly, it is not enough to simply prescribe ART. To reach the goal of sustained virologic suppression, we need developmentally and culturally tailored adherence support programs that can maintain youth on treatment through the challenges and growth of adolescence. We must identify targets for intervention by learning from the resilience of the scores of youth living with HIV who have successfully navigated the transition to adult care.
Increasing and sustaining ART access for adolescents is in itself a powerful HIV prevention strategy. Treatment as prevention, using ART to suppress the viral load and prevent transmission, can reduce heterosexual HIV transmission by up to 96%.7 Early data suggest the efficacy of treatment as prevention among men who have sex with men and injection drug users as well.8 Yet, ART cannot stand alone in the arsenal of prevention tools for youth living with HIV. We must also increase access to reproductive and sexual health services. Reducing unintended pregnancies, increasing access to condoms and comprehensive sexual education, and identifying and treating sexually transmitted infections among youth living with HIV will be paramount in preventing future perinatal and sexual transmission. Successful implementation of these strategies will require training a health care workforce that is skilled in delivering adolescent-focused care tailored to the appropriate cognitive, social-emotional, and physical stages of development. Finally, preventing HIV infections will mean addressing the syndemics of gender-based violence, racism, and homophobia that serve as barriers to treatment success for youth.
While the cost of developing, testing, and implementing such interventions will be considerable, the price of inaction is far higher. At the current levels of global funding, rates of new adolescent infections and AIDS-related mortality will continue to rise.2 Investment in youth-focused treatment and prevention can offset the costs of increasing adolescent morbidity and mortality. Recent data show that adopting the UNAIDS Investment Framework would lead to a 50% reduction in adolescent infections by 2020.2 As we determine how to react to the growing epidemic, the future of a generation is at stake.
Acknowledgments
Funding/Support: Dr Dowshen is supported by grant K23 MH102128 from the National Institutes of Health. Dr Lowenthal is supported by grant K23 MH095669 from the National Institutes of Health.
Role of the Funder/Sponsor: The National Institutes of Health had no role in the preparation, review, or approval of the manuscript, and the decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: None reported.
Contributor Information
Sarah M. Wood, Craig-Dalsimer Division of Adolescent Medicine, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania.
Nadia Dowshen, Craig-Dalsimer Division of Adolescent Medicine, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania; and Department of Pediatrics, University of Pennsylvania Perelman School of Medicine, Philadelphia.
Elizabeth Lowenthal, Departments of Pediatrics and Epidemiology, University of Pennsylvania Perelman School of Medicine, Philadelphia; and Division of General Pediatrics, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania.
REFERENCES
- 1.World Health Organization. Health for the World’s Adolescents: A Second Chance in the Second Decade. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 2.United Nations Children’s Fund. Towards an AIDS-Free Generation: Children and AIDS: Sixth Stocktaking Report, 2013. New York, NY: UNICEF; 2013. [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC). Vital signs: HIV infection, testing, and risk behaviors among youths: United States. MMWR Morb Mortal Wkly Rep. 2012;61(47):971–976. [PubMed] [Google Scholar]
- 4.Monitoring Selected HIV Prevention and Care Objectives by Using HIV Surveillance Data: United States and Six Dependent Areas, 2012. Atlanta, GA: Centers for Disease Control & Prevention; 2014. Centers for Disease Control and Prevention. [Google Scholar]
- 5.Zanoni BC, Mayer KH. The adolescent and young adult HIV cascade of care in the United States: exaggerated health disparities. AIDS Patient Care STDS. 2014;28(3):128–135. doi: 10.1089/apc.2013.0345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen MS, Chen YQ, McCauley M, et al. HPTN-052 Study Team. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Recommendations for HIV Prevention With Adults and Adolescents With HIV in the United States, 2014. Atlanta, GA: Centers for Disease Control & Prevention; 2014. Health Resources and Services Administration; National Institutes of Health; American Academy of HIV Medicine; Association of Nurses in AIDS Care; International Association of Providers of AIDS Care; National Minority AIDS Council; Urban Coalition for HIV/AIDS Prevention Services. [Google Scholar]