Abstract
Objectives
The study provides a novel model and more comprehensive estimates of the burden of occupational morbidity and mortality in food-related industries, using a farm-to-table approach.
Methods
The authors analyzed 2008–2010 US Bureau of Labor Statistics data for private industries in the different stages of the farm-to-table model (production; processing; distribution and storage; retail and preparation).
Results
The morbidity rate for food system industries were significantly higher than the morbidity rate for non-food system industries (Rate Ratio (RR)=1.62, 95% Confidence Interval (CI): 1.30–2.01). Furthermore, the occupational mortality rate for food system industries was significantly higher than the national non-food occupational mortality rate (RR=9.51, 95% CI: 2.47–36.58).
Conclusions
This is the first use of the farm-to-table model to assess occupational morbidity and mortality, and these findings highlighting specific workplace hazards across food system industries.
INTRODUCTION
Recent interest in infectious and non-infectious foodborne disease outbreaks has brought increasing public attention to food production, processing, and preparation.1 However, the focus has largely been on consumer illness and death, with less attention paid to worker health and safety. Overall, the annual economic burden of occupational morbidity and mortality in the United States is estimated to be approximately $250 billion, including direct and indirect costs.2 Many industries related to food production, including agriculture, manufacturing, and food preparation have high occupational morbidity rates.3,4 Food production workers, especially those engaged in fishing, hunting, and trapping, have the highest rate of job-related fatalities in the US, compared to other private industry workers.5–7 A large body of literature exists regarding occupational morbidity and mortality during food production,8–10 but the health of workers in food-related industries is less studied. We are not aware of any systematic attempts to calculate the combined burden of worker injury and illness associated with feeding an industrialized nation.
The farm-to-table framework for understanding the pathways and processes necessary for modern food has been widely used in microbial risk assessment,11,12 food safety education,13 contextualization of outbreaks,14,15 and popular discussion of food-related issues16 pertaining to consumers. In this paper, we use the farm-to-table continuum (sometimes referred to as the food system) as a heuristic for organizing categories of food system industries, in order to better understand the impact of food production on worker health. The five major steps in the model are food production, processing, distribution and storage, retail, and preparation (Figure 1).17,18 Between and within each step there are transportation and the creation of waste. We have included transportation that occurs within steps along the farm-to-table continuum (e.g. on farms or in processing centers) though transportation between steps has not been (e.g. the transportation industry). We did not include industries that manage food waste in this analysis because they are not traditionally part of the farm-to-table continuum. While different commodities follow diverse paths en route to consumers, the farm-to-table model provides a broad framework with which to capture the diverse paths to the consumer and may be stratified later by industry or food, as necessary. In order to present a more integrated perspective of the impact of modern food production and processing on worker health, we sought to calculate estimates of the increased burden of occupational illness, injury, and death related to each stage in the farm-to-table continuum, a conceptual model of food production.
Figure 1.
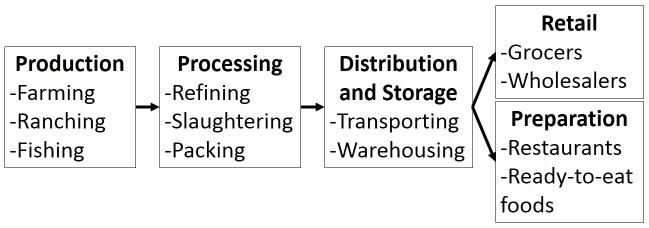
Schematic of pathway of food from farm to table with examples of generic industry categories within each stage.
METHODS
We used morbidity and mortality data from private industries included in the US Bureau of Labor Statistics’ (BLS) Illnesses Injuries and Fatalities program’s Survey of Occupational Injuries and Illnesses (SOII)19–21 and Census of Fatal Occupational Injuries (CFOI).5–7 SOII is a federal and state program in which approximately 176,000 private industry establishments provide annual reports on the number of injuries and illnesses each employer has recorded in their logs. Non-fatal occupational injuries are reportable if they cause lost work time, require medical treatment other than first aid, restrict work or motion, cause loss of consciousness, require transfer to another job, or meet other criteria outlined by the Occupational Safety and Health Administration.22 CFOI is a nation-wide program that compiles death counts using state and federal sources including death certificates, workers’ compensation reports, and administrative reports.23 Deaths due to traumatic injuries for which exposures or actions that occurred as part of an employee’s work-related activities during a single workday or shift are eligible for inclusion, though deaths during commuting are excluded. CFOI does not include fatal occupational illnesses. Deaths are reported to BLS by states, and the final dataset is compiled by cross-referencing various source materials, including reports by other agencies.
We analyzed the morbidity and mortality data from private industry from 2008 to 2010, the most recent years with final corrected data available, to estimate illness, injury, and fatality rates. We used employment numbers from the BLS’s National Industry Employment Estimates and National Occupational Employment and Wage Estimates included with each year’s SOII.19–21 Industries explicitly involved in food production, processing, storage, retail, and preparation were included (Table 1). We chose to group both wholesale and retail businesses in the food-related retail category. For food production stage-level categories (i.e. production, processing, etc.), we calculated injury and fatality rates by dividing each industry’s counts by their total employment. Food-specific transportation statistics were not available, so transportation was not included in estimates for distribution and storage stage industries. We excluded food-related industries to calculate non-food private industry morbidity and mortality rates (Supplementary Table 1). Rates from industries from within the same farm-to-table stage were averaged together, weighted by employment, to get a group rate. To compare rates between groups, we used Wald tests after fitting negative binomial regression models with general estimating equations (GEE). We used negative binomial models for all analyses and reported medians because diagnostic analyses indicated overdispersion and non-normal distribution. We used GEE to control for year to year correlation within industries. We specified the contrast statements to obtain estimated rate ratios. We also estimated excess morbidity and mortality by calculating the difference between observed food industry counts of illnesses, injuries, and deaths and the number expected by applying mean non-food industry morbidity and mortality rates for each industry sector to food-industry employment numbers from the same sector.
Table 1.
Food-related industries included in the analysis and their annual average employment, US Bureau of Labor Statistics, 2008–2010.
| Industries included in the analysis, grouped by farm-to-table stage | NAICSa code | Average employment (thousands) |
|---|---|---|
| All non-food private industry | 90,147.2 | |
| Food production | ||
| Crop production | 111 | 416.5 |
| Animal production | 112 | 161.4 |
| Fishing, hunting, and trapping | 114 | 8.8 |
| Support activities for agriculture and forestry | 115 | 332.6 |
| Food processing | ||
| Food manufacturing | 311 | 1,467.3 |
| Beverage and tobacco product manufacturing | 312 | 193.6 |
| Pesticide, fertilizer, and other agricultural chemical manufacturing | 3253 | 36.5 |
| Agricultural implement manufacturing | 33311 | 75.4 |
| Food storage | ||
| Refrigerated warehousing and storage | 49312 | 48.7 |
| Farm product warehousing and storage | 49313 | 9.0 |
| Food retail | ||
| Grocery and related product merchant wholesalers | 4244 | 725.6 |
| Farm product raw material merchant wholesalers | 4245 | 74.0 |
| Beer, wine, and distilled alcoholic beverage merchant wholesalers | 4248 | 162.7 |
| Food and beverage stores | 445 | 2,876.4 |
| Food service | ||
| Food services and drinking places | 722 | 9,586.2 |
North American Industry Classification System.
First, we compared the occupational morbidity and mortality rates for non-food producing private industries to food system occupational morbidity and mortality rates. Second, we compared industry sector-specific occupational mortality and morbidity rates to food system occupational mortality and morbidity rates. For example, we compared food production worker morbidity rates to the national rate for goods-producing industries. Third, we assessed specific causes of any differences in morbidity or mortality rates by comparing event-specific injury and fatality data. Lastly, we compared separate rates for industries producing and processing meat, fish, and dairy (collectively referred to as meat) products and industries producing and processing non-meat, non-dairy products in order to assess for possible product-specific effects.
Models comparing food system and non-food system industries included a variable to distinguish between the categories, as did models comparing meat and non-meat industries. All analyses were conducted in SAS 9.3 (Cary, NC) with a significance level of 0.05.
RESULTS
From our analyses, food system jobs, excluding individuals employed in transportation, make up an estimated 15% of all private industry jobs in the United States. We excluded individuals employed in transportation because no numbers were available for the proportion of laborers employed in food-specific transportation. As measured by the number of total food industry workers, food service (59.28%), retail (23.74%), and processing (10.96%) were the first, second and third most populous steps in the farm-to-table continuum. Storage had the highest median morbidity level among the steps in the farm-to-table continuum (7.02 annual cases/100 full-time workers, Table 2), and production had the highest mortality level (7.17 deaths/10,000 full-time workers, Table 2).
Table 2.
Morbidity rate, mortality rate, and rate ratios (RR) comparing of morbidity and mortality rates for food system jobs by farm-to-table stage to same-sector non-food private industry morbidity and mortality rates, US Bureau of Labor Statistics, 2008–2010.
| Industry | Median morbidity ratea (IQR) | RR (95% CI) | Median mortality rateb (IQR) | RR (95% CI) |
|---|---|---|---|---|
| All non-food industry | 2.65 (1.62–4.00) | Ref. | 0.17 (0.09–0.33) | Ref. |
| All food industry | 2.33 (2.16–4.17) | 1.62 (1.30–2.01) | 0.13 (0.12–0.28) | 9.51 (2.47–36.58) |
| Production to retail | ||||
| Non-food | 2.33 (1.66–3.97) | Ref. | 0.13 (0.09–0.33) | Ref. |
| Food | 4.17 (3.83–5.74) | 1.71 (1.39–2.10) | 0.33 (0.28–0.47) | 10.28 (2.68–3.45) |
| Production | ||||
| Non-food | 2.34 (2.16–3.83) | Ref. | 1.18 (1.15–1.24) | Ref. |
| Food | 4.00 (3.58–4.06) | 1.30 (0.82–2.06) | 7.17 (1.42–7.76) | 6.50 (1.49–28.44) |
| Processing | ||||
| Non-food | 4.61 (2.90–5.64) | Ref. | 0.22 (0.16–0.29) | Ref. |
| Food | 5.74 (5.70–6.25) | 1.34 (0.97–1.85) | 0.39 (0.33–0.47) | 1.75 (1.10–2.77) |
| Storagec | ||||
| Non-foodd | 5.45 (5.40–6.20) | Ref. | 1.43 (1.31–1.56) | Ref. |
| Food | 7.02 (6.56–7.58) | 1.19 (1.04–1.35) | 1.24 (1.02–1.24) | 11.89 (5.35–26.42) |
| Retail | ||||
| Non-food | 3.49 (1.63–4.49) | Ref. | 0.29 (0.09–0.33) | Ref. |
| Food | 3.83 (3.83–4.17) | 1.90 (1.38–2.61) | 0.28 (0.19–0.31) | 2.72 (1.10–6.71) |
| Service | ||||
| Non-food | 1.81 (0.94–3.10) | Ref. | 0.10 (0.08–0.26) | Ref. |
| Food | 2.16 (2.07–2.33) | 0.95 (0.74–1.21) | 0.12 (0.12–0.13) | 0.42 (0.26–0.68) |
Abbreviations: Interquartile Range (IQR), Rate Ratio (RR), Confidence Interval (CI), Referent group (Ref.) Estimates from negative binomial GEE models.
Reported injuries and illnesses per 100 full-time workers, weighted based on average annual employment;
Reported fatal occupational injuries per 10,000 full-time workers, weighted based on average annual employment;
Excludes distribution and does not include retail storage;
Excludes transportation.
When comparing within industry category, there was still a significant difference between morbidity rates in food producing industries and non-food producing industries (Table 2). Food production industries had a higher rate of injuries and illnesses than the rate for all goods producing industries, and food processing industries had a slightly higher rate of injuries and illnesses than did manufacturing industries overall, though neither was significant ((Rate Ratio (RR)=1.30, p=0.269; RR=1.34, p=0.073, respectively). Food storage industries had a significantly higher morbidity rate than other storage industries (RR=1.19, p=0.002). Food retail industries had a significantly higher rate of injuries and illnesses than did other types of retail industries (RR=1.90, p<0.001). Food service industries had a similar occupational morbidity rate to other same-sector non-food industries.
In addition to having higher morbidity rates overall, food system industries as a whole had a higher rate of more severe injuries—those requiring days away from work—compared with non-food private industries overall (RR=2.38, p=0.005, Table 3). This did not appear to be driven by any specific industry sector with inordinately higher rates than other industry sector, as food industries in all sectors except food service had higher rates of severe injuries than same-sector non-food industries (Table 3). Food processing, storage, and retail industries all had significantly higher rates of injuries and illnesses requiring days away from work compared with non-food private industries from the same sectors (p=0.042, p=0.009, and p<0.001, respectively). Conversely, food service industries had a significantly lower rate of severe injuries than all non-food private industries (RR=0.75, p=0.029).
Table 3.
Severe injury and illness rate and rate ratios (RR) comparing of severe injury and illness rates for food system jobs by farm-to-table stage to same-sector non-food private industry severe injury and illness rates for specific injury and illness causes, US Bureau of Labor Statistics, 2008–2010.
| Industry | Median severe injury ratea (IQR) | Severe injury RR (95% CI) | Contact object or equipment RR (95% CI) | Slips, trips, and falls RR (95% CI) | Overexertion RR (95% CI) | Repetitive motion RR (95% CI) | Exposure substances or environment RR (95% CI) | Transportation incident RR (95% CI) | Assault by person RR (95% CI) | Assault by other cause RR (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|
| All non-food industry | 0.82 (0.48–1.25) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| All food industry | 0.56 (0.53–1.24) | 2.38 (1.38–4.08) | 2.43 (1.43–4.14) | 1.08 (1.33–3.24) | 2.56 (1.20–5.45) | 1.78 (0.83–3.80) | 1.68 (1.12–2.52) | 2.75 (1.18–6.40) | 0.76 (0.26–2.20) | 8.73 (2.35–32.40) |
| Production to retail | ||||||||||
| Non-food | 0.67 (0.49–1.18) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Food | 1.29 (1.13–1.43) | 2.55 (1.49–4.37) | 2.60 (1.53–4.42) | 2.19 (1.40–3.43) | 2.81 (1.32–5.96) | 1.94(0.91–4.15) | 1.64 (1.06–2.53) | 3.04 (1.31–7.03) | 0.71 (0.23–2.20) | 9.42 (2.55–3.75) |
| Production | ||||||||||
| Non-food | 1.44 (1.20–1.50) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Food | 1.29 (1.20–1.52) | 1.22 (0.78–1.91) | 1.27 (0.81–2.00) | 1.10 (0.59–2.05) | 0.68 (0.36–1.28) | 1.41 (0.76–2.61) | 1.49 (0.74–3.03) | 0.87 (0.42–1.82) | 9.26 (2.20–38.92) | 28.98 (5.67–148.18) |
| Processing | ||||||||||
| Non-food | 1.09 (0.73–1.30) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Food | 1.40 (1.31–1.43) | 1.38 (1.01–1.89) | 1.16 (0.74–1.83) | 1.54 (1.18–2.00) | 1.61 (0.98–2.64) | 0.90 (0.52–1.57) | 1.61 (1.01–2.56) | 3.11 (1.50–6.44) | 1.74 (0.26–11.44) | 3.69 (0.93–14.64) |
| Storagec | ||||||||||
| Non-foodd | 1.55 (1.48–1.87) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Food | 2.58 (2.54–25.37) | 4.06 (1.70–9.72) | 4.35 (1.77–10.67) | 4.15 (2.45–7.02) | 3.48 (1.08–11.17) | 3.23 (0.75–13.92) | 4.32 (1.09–17.21) | 4.10 (1.03–16.27) | Not estimatede | Not estimatede |
| Retail | ||||||||||
| Non-food | 1.00 (0.67–1.13) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Food | 1.24 (1.08–1.44) | 2.22 (1.51–3.27) | 2.21 (1.58–3.09) | 1.88 (1.39–2.53) | 2.58 (1.20–5.56) | 2.12 (1.29–3.48) | 0.92 (0.52–1.62) | 2.26 (1.06–4.84) | 1.60 (0.45–5.69) | 7.13 (1.13–44.76) |
| Service | ||||||||||
| Non-food | 0.59 (0.31–1.04) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Food | 0.53 (.49–0.56) | 0.75 (0.59–0.97) | 1.13 (0.83–1.53) | 0.78 (0.62–0.99) | 0.49 (0.34–0.70) | 0.52 (0.42–0.65) | 2.10 (1.57–2.80) | 0.21 (0.14–0.33) | 0.59 (0.27–1.31) | 0.04 (0.03–0.07) |
Abbreviations: Interquartile Range (IQR), Rate Ratio (RR), Confidence Interval (CI), Referent group (Ref.) Estimates from negative binomial GEE models.
Reported injuries requiring days away from work per 100 full-time workers, weighted based on average annual employment;
Includes unintentional assault by a person or assault by an animal or insect;
Excludes distribution and does not include retail storage;
Excludes transportation;
Not estimated because model did not converge due to small numbers of events.
The higher rate of injuries and illnesses requiring days away from work among food system industries compared to non-food system industries was mostly due to industry sector-specific differences rather than inter-sector patterns of morbidity differences between food and non-food industries (Supplementary Figure 1). However the rates of severe injuries from contact with an object or equipment and slips, trips and falls were elevated among all sectors of food industries compared to non-food industries, with the exception of food service industries (Table 3). Workers in food production industries were significantly more likely to be injured severely by assault by a person (p=0.002) and assault by other causes, including animals or insects (p<0.001) than workers in non-food production industries were. Workers in food processing industries were significantly more likely to be severely injured by a slip, trip, or fall (p=0.002); exposure to harmful substances (p=0.044); and transportation incidents (p=0.002) than workers in non-food manufacturing industries. Food storage and food retail industries had higher rates of severe injuries compared to non-food storage and retail industries, and this was reflected in significantly higher rates of most categories of severe injury events (Table 3). Workers in food service industries were less likely than workers in other service industries to be severely injured, and this extended to most categories of severe injury events, with the exception of injuries from exposure to harmful substances (RR=2.10, p<0.001).
There was a significantly higher mortality rate for workers in food system industries compared to all non-food private industries, though the effect estimate was imprecise (RR=9.51, p=0.002, Table 2). When comparing within industry sector, food production, processing, storage, and retail industries had higher mortality rates than their non-food system counterparts (p=0.013, p=0.017, p<0.001, and p=0.030, respectively). Food service industries had a significantly lower mortality rate than same-sector non-food industries (RR=0.42, p<0.001).
Elevated rates of fatal occupational injuries among food production and food processing industries as compared to non-food production and manufacturing industries, respectively, were due to significantly higher rates of fatal transportation injuries, fatal assaults (includes assaults by people and other animals), and fatal exposures to substances or environments (Table 4, Supplementary Figure 2). Elevated fatal injury rates for food retail industries compared with non-food retail industries were due to higher rates of fatal transportation incidents, assaults, and fatal injuries from contact with objects or equipment, though the only significantly elevated cause of fatal injuries was from contact with objects or equipment (p=0.012). Compared to non-food service industries, food service industries had significantly lower rates of mortality due to all causes considered, except for fatal assaults.
Table 4.
Mortality rate and rate ratios (RR) comparing of severe injury rates for food system jobs by farm-to-table stage to same-sector non-food private industry severe injury rates for specific injury causes, US Bureau of Labor Statistics, 2008–2010.
| Industry | Median mortality ratea (IQR) | Mortality RR (95% CI) | Transportation RR (95% CI) | Assault RR (95% CI) | Contact with object or equipment RR (95% CI) | Slip, trip, fall RR (95% CI) | Exposure to substance or environment RR (95% CI) | Fire or explosion RR (95% CI) |
|---|---|---|---|---|---|---|---|---|
| All non-food industry | 0.17 (0.09–0.33) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| All food industry | 0.13 (0.12–0.28) | 9.51 (2.47–36.58) | 19.61 (3.91–98.29) | 5.11 (1.92–13.59) | 4.30 (1.09–16.94) | 2.44 (0.67–8.90) | 16.75 (3.25–86.45) | 1.13 (0.29–4.31) |
| Production to retail | ||||||||
| Non-food | 0.13 (0.09–0.33) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Food | 0.33 (0.28–0.47) | 10.28 (2.68–39.45) | 21.30 (4.26–106.39) | 5.35 (1.98–14.49) | 4.67 (1.18–18.43) | 2.67 (0.73–9.72) | 18.18 (3.53–93.71) | 1.23 (0.33–4.65) |
| Production | ||||||||
| Non-food | 1.18 (1.15–1.24) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Food | 7.17 (1.42–7.76) | 6.50 (1.49–28.44) | 14.79 (3.10–70–63) | 20.76 (6.95–62.00) | 1.66 (0.39–7.17) | 2.00 (0.59–6.78) | 9.67 (2.17–43.12) | 0.68 (0.22–2.09) |
| Processing | ||||||||
| Non-food | 0.22 (0.16–0.29) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Food | 0.39 (0.33–0.47) | 1.75 (1.10–2.77) | 2.78 (1.16–6.63) | 2.10 (1.17–3.77) | 0.40 (0.10–1.65) | 1.12 (0.32–4.01) | 2.55 (1.36–4.78) | 0.60 (0.11–3.23) |
| Storageb | ||||||||
| Non-foodc | 1.43 (1.31–1.56) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Food | 1.24 (1.02–1.24) | 11.89 (5.35–26.42) | Not estimatedd | Not estimatedd | Not estimatedd | Not estimatedd | Not estimatedd | Not estimatedd |
| Retail | ||||||||
| Non-food | 0.29 (0.09–0.33) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Food | 0.28 (0.19–0.31) | 2.72 (1.10–6.71) | 2.51 (0.90–6.94) | 1.33 (0.52–3.39) | 9.55 (1.64–55.62) | 0.95 (0.45–2.00) | 0.34 (0.08–1.37) | Not estimatedd |
| Service | ||||||||
| Non-food | 0.10 (0.08–0.26) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Food | 0.12 (0.12–0.13 | 0.42 (0.26–0.68) | 0.14 (0.08–0.28) | 1.38 (0.87–2.22) | 0.09 (0.03–0.22) | 0.48 (0.29–0.79) | 0.44 (0.26–0.72) | Not estimatedd |
Abbreviations: Interquartile Range (IQR), Rate Ratio (RR), Confidence Interval (CI), Referent group (Ref.) Estimates from negative binomial GEE models.
Reported fatal occupational injuries per 10,000 full-time workers, weighted based on average annual employment;
Excludes distribution and does not include retail storage;
Excludes transportation;
Not estimated because model did not converge due to small numbers of events.
Based on non-food industry sector-specific mean morbidity and mortality, food industries had an estimated 57,975 excess injuries and illnesses and 439 excess deaths annually (subsequent results in Supplementary Table 2). The greatest numbers of excess injuries and illnesses were in food processing and retail. Food processing had 28,436 estimated excess injuries and illnesses and food retail had an estimated 48,717 estimated excess injuries and illnesses. The greatest numbers of excess fatalities were in food production and processing. Food production had 408 estimated excess deaths and food processing had 59 estimated excess deaths. Food service was the only farm-to-table stage without excess morbidity and mortality. Food service industries had 27,216 fewer injuries and illnesses than expected and 64 fewer deaths than expected, compared to the mean rates from other service industries.
Industries related primarily to meat, fish, and dairy production and processing did not have significantly higher morbidity rates than industries related to produce and other non-meat food production and processing (RR=1.15, p=0.303, Supplementary Table 3). However, meat-related food industries had a significantly higher rate of injuries requiring days away from work compared to non-meat food production and processing industries (RR=1.40 p=0.008, Supplementary Table 3). Workers in meat-related industries were significantly more likely to be severely injured by contact with an object or equipment (RR=1.50, p=0.005, Supplementary Table 3), but the largest driver of the difference in severe injury rates was assaults by people and other animals (RR=16.80, p=0.002, Supplementary Table 3). In addition, meat, fish, and dairy related industries had a much higher mortality rate compared to non-meat related food industries (RR=7.33, p=0.020, Supplementary Table 3). This was due to a higher rate of fatalities due to assaults by people or other animals (RR=9.22, p=0.001, Supplementary Table 3) and fatal exposures to substances or environments (RR=21.67, p=0.003, Supplementary Table 3).
DISCUSSION
The purpose of this research is to provide a novel model and estimates of the burden of occupational illness, injury, and death in food-related industries in the US, using a farm-to-table approach. Food industries, especially those involved in processing, storage, and retail, have significantly higher rates of illnesses and injuries, as compared to non-food private industries in the U.S. We observed a pattern of elevated rates of morbidity across most of the farm-to-table continuum, underscoring the need for concerted action to reduce unnecessary injuries and illnesses across this diverse industry spectrum. We also observed significantly elevated rates of occupational mortality in food production, processing, and retail.
Occupational Morbidity
The morbidity rate for food system industries along the farm-to-table spectrum was higher in all sectors, except food service, when compared to non-food industries. Even when compared with industries from the same category (e.g., workers employed by industries processing other types of products) to make a comparison between more similar industries, food system industries generally had higher rates of occupational injury and illness than their same industry sector counterparts. Potential workforce and process-related reasons for this finding merit future research.
From a workforce standpoint, these industries may have different job requirements, there may be different safety procedures in place with different levels of adherence, there may be geographic differences in the workforce, there may be different experience levels, differential vulnerabilities, or differences in the language or culture of the workforces. Food system workforces often are demographically different from the general population and the jobs themselves are distinct.24 Food system workers also tend to be younger than other workers in similar occupational categories,25 and younger workers tend to have higher rates of injuries than older workers,26 though this may be a surrogate for being newly-hired and having less training and experience. There may also be socioeconomic differences. Eight of the ten lowest paying occupations in the US are food system jobs, suggesting that workers in these industries may be uniquely disadvantaged.27 Within the manufacturing sector, all manufacturing industries (e.g. chemical manufacturing, furniture manufacturing, etc.) except textile and apparel manufacturing have higher mean and median hourly wages than food manufacturing.28 Some workforce-related causes of higher rates of occupational morbidity may be amenable to change by improved training, and there are successful programs that have been developed to target food industry workers.29 One example is severe injuries due to contact with objects or equipment. All food-related industries except for food service had higher rates of severe injuries due to contact with objects or equipment than non-food industries from the same sectors. Lack of experience with a particular task has been associated with higher rates of machinery-related injury among farmworkers and meatpackers,30,31 suggesting that increased training may reduce injury rates. However, hazards related to equipment can also vary by the equipment provided and other process-related factors.32
Process-related reasons for differences in occupational morbidity include differences in the activities and occupational practices of food-related industries compared to non-food-related industries. Our data indicate that the differences between causes of severe injuries among food system industries and non-food system industries from the same sector vary. Some of these differences are indicative of unique job responsibilities or conditions. For example, workers in food production industries (e.g. ranchers and fishermen), are more likely to be severely injured by animals compared to workers in non-food production industries (e.g. miners and forestry workers). There are also different working environments required when food is present. One possible reason for significantly elevated rates of severe injuries due to slips, trips, and falls in food processing, storage, and retail industries compared to non-food same-sector industries may be the preponderance of refrigeration.33 Many food products are processed and stored at cooler temperatures to maintain freshness, this can lead to precipitation that may make floors slippery34 in factories, warehouses, or on-site storage areas in retail facilities.35
In estimating product-specific morbidity rates, meat, fish, and dairy production and processing industries did not have significantly higher rates of occupational injury and illness than non-meat, non-dairy production and processing industries. However, the illnesses and injuries were more severe, suggesting that some of the differences in rates of severe injuries and illnesses between food and non-food industries may be driven by a subset of all food industries.
Occupational Mortality
Though occupational fatalities are relatively rare events, the overall food industry mortality rate is high when compared to the occupational mortality rate for non-food private industries, with the exception of food service industries. The increased risk of mortality in food production has also been established by other researchers.36,37
The fatal injuries in food production and food processing industries are largely the result of transportation incidents, assaults, and exposure to toxic substances or environments. In many food system industries, practices to prevent occupational fatalities exist, though they are not consistently used. Use that differs within an industry may be associated with occupational health disparities.37 For example, though tractor roll-over fatalities are a well-documented hazard for agricultural workers, only an estimated 59% of tractors in operation are equipped with roll-over protection,38 and the prevalence of such protection is lower among lower income farmers.36,39. Whether causes of fatal injuries across other food-related industry sectors are due to similar shortcomings in safety equipment, protocols, and training is an important topic for future research.
The only farm-to-table stage that did not show higher rates of occupational mortality was food service. Food service industries had significantly lower rates of occupational fatalities than other service industries. Food service workers were less likely to die of all causes considered, with the exception of assaults. Though it was not statistically significant, food service industries had a higher rate of fatal assaults than other service workers. This finding was consistent with earlier work.40 The lower rate of fatal occupational injuries by all other documented causes is likely because food service occurs in a controlled environment, relative to some other service industries. Though the food service environment is a common source of injury, these injuries are rarely severe enough to result in death.
In estimating product-specific mortality rates meat, fish, and dairy production and processing industries had significantly higher rates of fatal occupational injuries than non-meat, non-dairy production and processing industries. This is consistent with the known hazards of meat producing industries, such as fishing, hunting, and trapping and animal production, which have the first and third highest mortality rates of all private industries.5–7
Limitations
Because of limited information regarding transportation and storage of food products, transportation jobs were not included in farm-to-table morbidity and mortality estimates. Transportation accidents are a common cause of injury and death in other industries, so the exclusion of these industries from our calculations likely resulted in an underestimate of the full impact across the continuum. An additional area of uncertainty relates to the farm-to-table model’s own limits. An estimated 40% of the American food supply goes uneaten,41 making industries responsible for the disposal of food waste a potentially important are to consider in order to capture all occupational morbidity and mortality related to food. However, the impact of this “post-table” stage of waste management was not assessed in our study. Additionally, some categories include both food and non-food industries, leading to some misclassification in our analysis. For example, refrigerated storage and warehousing includes storage of furs though we categorized it as a food-related industry because of the major role it plays in the storage of food products.
Another limitation of this work is the lack of product-level data. This restricted the degree to which specific illnesses or injuries could be linked to a specific product type, though we attempted to estimate these differences in general product categories by comparing meat and non-meat producing industries. We restricted our analysis to private industry, and therefore this analysis does not include public sector (e.g. military, governmental) food industries. Lastly, this analysis is likely to underestimate morbidity and mortality because of the underreporting of injury and illness rates in the BLS statistics,42–45 as well as other limitations of SOII and CFOI data.23 For example, the underreporting occurs because of employer, employee, physician, and survey design factors. In addition, BLS statistics are not collected for farms with fewer than 11 employees and may exclude migrant or seasonal workers, which may lead to substantial undercounting. A recent interview-based study of migrant and seasonal crop workers identified an injury rate of 12.7 cases per 100 full-time employees—far in excess of our BLS data-based estimates of 4.0 injuries and illnesses per 100 full-time employees46—and a modeling analysis from 2014 estimated that approximately 75% of injuries related to agriculture may not be reported in the SOII.42 There are additional limitations of the CFOI. First, it only includes traumatic causes of death and only those that occurred during a single shift or workday. Thus it fails to capture occupational fatalities caused by long-term exposures, fatalities whose work-relatedness is difficult to establish, latent, or work-related illnesses. Work-related illnesses are associated with an estimated 49,000 deaths annually.47 Therefore it is likely that the true burden of injury and illnesses in food system industries may be higher than we have reported here.
Implications
The increased morbidity and mortality rates for industries in all parts of the farm-to-table chain except for service suggest that considering these industries as a whole may help direct public health efforts towards this major area of American commerce. It also serves to support existing efforts to target improvements to food production worker safety, such as the National Occupational Research Agenda’s (NORA) National Agriculture, Forestry, and Fishing Agenda.48 Furthermore, applying the farm-to-table model can serve as a heuristic for guiding consumer understanding of occupational injury, illness, and mortality as hidden costs of food production. Future work should focus on reducing disparities in occupational risk by continuing interventions to control those risks and developing new interventions when necessary. In addition, the farm-to-table model is easily communicated to consumers as well as policy makers. Future research should consider the impact on consumer purchasing practices of communicating the foodborne burden of occupational injury, illness, and mortality (i.e. that burden of morbidity and mortality related to bringing food to consumers) and employ the farm-to-table model to help estimate the economic impact of occupational morbidity and mortality in food system industries.
Applying the farm-to-table model is a novel construct within occupational health and has the potential to reshape the understanding of how market forces in the food industry may impact producers and consumers. The farm-to-table model unifies diverse industries into a common chain. In this way, it reshapes our understanding of the burden of “food-borne” illness to include not just pathogens and toxins that are transmitted to consumers through contaminated food, but also the costs that society bears for occupational injury, illness, and death that occur in the process of producing and delivering food to consumers.
Supplementary Material
Acknowledgments
FUNDING
This work was supported by funding from the ARCS Foundation and by the National Institute of Diabetes And Digestive and Kidney Diseases of the National Institutes of Health (F30DK100097) to KLN. This work was partially supported by the National Institute of Allergy and Infectious Diseases at the National Institutes of Health (grant 1K01AI087724-01), the National Institute of Food and Agriculture at the U.S. Department of Agriculture (grant 2010-85212-20608), and the Emory University Global Health Institute to JSL.This work was supported in part by grant T42OH009229, funded by the Centers for Disease Control and Prevention, to LSN. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the Centers for Disease Control and Prevention, or the Department of Health and Human Services.
Thank you to Dr. Stephen Reynolds for his advice regarding an earlier draft of this manuscript.
Footnotes
CONFLICT OF INTEREST
None.
Contributor Information
Kira L. Newman, Email: kira.newman@emory.edu, Department of Epidemiology, Rollins School of Public Health and Laney Graduate School, Emory University, 1518 Clifton Rd, NE, Atlanta, GA, USA 30322, Phone: 1-720-201-6043, Fax: 1-404-727-4590.
Juan S. Leon, Email: juan.leon@emory.edu, Hubert Department of Global Health, Rollins School of Public Health, Emory University, Atlanta, GA, USA.
Lee S. Newman, Email: lee.newman@ucdenver.edu, Center for Worker Health and Environment, Colorado School of Public Health and School of Medicine, University of Colorado Denver, Anschutz Medical Campus, Aurora, CO, USA.
References
- 1.Boyce B. Trends in Farm-to-Table from a Sociological Perspective. J Acad Nutr Diet. 2013 Jul;113:892. doi: 10.1016/j.jand.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 2.Leigh JP. Economic burden of occupational injury and illness in the United States. Milbank Q. 2011 Dec;89:728–772. doi: 10.1111/j.1468-0009.2011.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Food Chain Workers Alliance. [Accessed July 8, 2014];The hands that feed us: Challenges and opportunities for workers along the food chain. 2012 Available at: http://foodchainworkers.org/wp-content/uploads/2012/06/Hands-That-Feed-Us-Report.pdf.
- 4.Kelly M, Christi E, Lang H, et al. Worker Equity in Food and Agriculture. Boston, MA: Tellus Institute and Sustainalytics; 2012. [Accessed July 8, 2014]. Available at: http://www.sustainalytics.com/sites/default/files/workerequity_october2012.pdf. [Google Scholar]
- 5.Bureau of Labor Statistics. [Accessed December 24, 2014];2008 Census of Fatal Occupational Injuries (revised data): Table 1-A. 2010 Available at: http://www.bls.gov/iif/oshwc/cfoi/cftb0232.pdf.
- 6.Bureau of Labor Statistics. [Accessed December 24, 2014];2009 Census of Fatal Occupational Injuries (revised data): Table 1-A. 2011 Available at: http://www.bls.gov/iif/oshwc/cfoi/cftb0241.pdf.
- 7.Bureau of Labor Statistics. [Accessed December 24, 2014];2010 Census of Fatal Occupational Injuries (revised data): Table 1-A. 2012 Available at: http://www.bls.gov/iif/oshwc/cfoi/cftb0250.pdf.
- 8.Frank AL, McKnight R, Kirkhorn SR, et al. Issues of agricultural safety and health. Annu Rev Publ Health. 2004;25:225–245. doi: 10.1146/annurev.publhealth.25.101802.123007. [DOI] [PubMed] [Google Scholar]
- 9.Cole DW, Cole R, Gaydos SJ, et al. Aquaculture: Environmental, toxicological, and health issues. Int J Hyg Envir Heal. 2009 Jul;212:369–377. doi: 10.1016/j.ijheh.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 10.Kirkhorn SR, Earle-Richardson G, Banks RJ. Ergonomic risks and musculoskeletal disorders in production agriculture: recommendations for effective research to practice. J Agromedicine. 2010 Jul;15:281–299. doi: 10.1080/1059924X.2010.488618. [DOI] [PubMed] [Google Scholar]
- 11.Ding T, Wang J, Forghani F, et al. Development of predictive models for the growth of Escherichia coli O157:H7 on cabbage in Korea. J Food Sci. 2012 May;77:M257–263. doi: 10.1111/j.1750-3841.2012.02660.x. [DOI] [PubMed] [Google Scholar]
- 12.Williams MS, Ebel ED, Vose D. Framework for microbial food-safety risk assessments amenable to Bayesian modeling. Risk Anal. 2011 Apr;31:548–565. doi: 10.1111/j.1539-6924.2010.01532.x. [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine Food Forum. Managing Food Safety Practices from Farm to Table: Workshop Summary. Washington (DC): National Academies Press (US); 2009. [Accessed July 8, 2014]. Available at http://www.ncbi.nlm.nih.gov/books/NBK26433/ [PubMed] [Google Scholar]
- 14.Van Doren JM, Neil KP, Parish M, et al. Foodborne illness outbreaks from microbial contaminants in spices, 1973–2010. Food Microbiol. 2013 Dec;36:456–464. doi: 10.1016/j.fm.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Vital signs: incidence and trends of infection with pathogens transmitted commonly through food--foodborne diseases active surveillance network, 10 U.S. sites, 1996–2010. MMWR Morb Mortal Wkly Rep. 2011 Jun 10;60:749–755. [PubMed] [Google Scholar]
- 16.Nowak AJ, Kolouch G, Schneyer L, et al. Building food literacy and positive relationships with healthy food in children through school gardens. Child Obes. 2012 Aug;8:392–395. doi: 10.1089/chi.2012.0084. [DOI] [PubMed] [Google Scholar]
- 17.Grohn Y, Hertl J, Ivanek R, et al. How university researchers can contribute to farm-to-table risk assessments: Listeria monocytogenes as an example. Foodborne Pathog Dis. 2007;4:527–537. doi: 10.1089/fpd.2007.0012. [DOI] [PubMed] [Google Scholar]
- 18.Escherichia coli O157:H7 in Ground Beef: Review of a Draft Risk Assessment. Washington, DC: The National Academies Press; 2002. Committee on the Review of the USDA E. coli O157:H7 Farm-to-Table Process Risk Assessment. [PubMed] [Google Scholar]
- 19.Bureau of Labor Statistics. [Accessed December 24, 2014];2008 Survey of Occupational Injuries and Illnesses. 2010 Available at: http://www.bls.gov/iif/
- 20.Bureau of Labor Statistics. [Accessed December 24, 2014];2009 Survey of Occupational Injuries and Illnesses. 2011 Available at: http://www.bls.gov/iif/
- 21.Bureau of Labor Statistics. [Accessed December 24, 2014];2010 Survey of Occupational Injuries and Illnesses. 2012 Available at: http://www.bls.gov/iif/
- 22.Occupational Safety and Health Administration. [Accessed July 29, 2014];OSHA Recordkeeping Handbook. 2005 Available at: https://www.osha.gov/recordkeeping/handbook/
- 23.Bureau of Labor Statistics. [Accessed July 29, 2014];BLS handbook of methods: Chapter 9. 2009 Available at: http://www.bls.gov/opub/hom/pdf/homch9.pdf.
- 24.Bureau of Labor Statistics. [Accessed July 29, 2014];Current Population Survey: Table 18. 2013 Available at: http://www.bls.gov/cps/cpsaat18.pdf.
- 25.Bureau of Labor Statistics. [Accessed December 24, 2014];Current Population Survey: Employed persons by detailed occupation and age, 2013 annual averages. Available at: http://www.bls.gov/cps/occupation_age.htm.
- 26.Salminen S. Have young workers more injuries than older ones? An international literature review. J Safety Res. 2004;35:513–521. doi: 10.1016/j.jsr.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 27.Bureau of Labor Statistics. [Accessed July 29, 2014];Employment and wages for the highest and lowest paying occupations, May 2012. 2013 Available at: http://www.bls.gov/oes/2012/may/high_low_paying.htm.
- 28.Bureau of Labor Statistics. [Accessed July 29, 2014];May 2013 National Industry-Specific Occupational Employment and Wage Estimates. 2013 Available at: http://www.bls.gov/oes/current/oessrci.htm.
- 29.Chapman LJ, Brunette CM, Karsh BT, et al. A 4-Year Intervention to Increase Adoption of Safer Dairy Farming Work Practices. Am J Ind Med. 2011;54:232–243. doi: 10.1002/ajim.20920. [DOI] [PubMed] [Google Scholar]
- 30.Lander L, Sorock GS, Stentz TL, et al. A case-crossover study of occupational laceration injuries in pork processing: methods and preliminary findings. Occup Environ Med. 2010;67:686–692. doi: 10.1136/oem.2009.048611. [DOI] [PubMed] [Google Scholar]
- 31.Sprince NL, Park H, Zwerling C, et al. Risk factors for machinery-related injury among Iowa farmers: A case-control study nested in the agricultural health study. Int J Occup Env Heal. 2002;8:332–338. doi: 10.1179/107735202800338641. [DOI] [PubMed] [Google Scholar]
- 32.Cai CB, Perry MJ, Sorock GS, et al. Laceration injuries among workers at meat packing plants. Am J Ind Med. 2005;47:403–410. doi: 10.1002/ajim.20157. [DOI] [PubMed] [Google Scholar]
- 33.James SJ, James C. The food cold-chain and climate change. Food Res Int. 2010;43(7):1944–1956. [Google Scholar]
- 34.Bentley TA, Haslam RA. Slip, trip and fall accidents occurring during the delivery of mail. Ergonomics. 1998;41:1859–1872. doi: 10.1080/001401398186027. [DOI] [PubMed] [Google Scholar]
- 35.Bentley T, Tappin D, Moore D, et al. Investigating slips, trips and falls in the New Zealand dairy farming sector. Ergonomics. 2005;48:1008–1019. doi: 10.1080/00140130500182072. [DOI] [PubMed] [Google Scholar]
- 36.Waggoner JK, Henneberger PK, Kullman GJ, et al. Pesticide use and fatal injury among farmers in the Agricultural Health Study. Int Arch Occ Env Hea. 2013;86:177–187. doi: 10.1007/s00420-012-0752-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Steege AL, Baron SL, Marsh SM, et al. Examining occupational health and safety disparities using national data: a cause for continuing concern. Am J Ind Med. 2014 May;57:527–538. doi: 10.1002/ajim.22297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.National Agricultural Statistics Service, Agricultural Statistics Board. [Accessed July 8, 2014];2011 Farm and Ranch Safety Survey: United States Department of Agriculture. 2013 Available at: http://usda01.library.cornell.edu/usda/current/FarmSafe/FarmSafe-05-30-2013.pdf.
- 39.Loringer KA, Myers JR. Tracking the prevalence of rollover protective structures on U.S. farm tractors: 1993, 2001, and 2004. J Safety Res. 2008;39:509–517. doi: 10.1016/j.jsr.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 40.Menendez CC, Konda S, Hendricks S, et al. Disparities in work-related homicide rates in selected retail industries in the United States, 2003–2008. J Safety Res. 2013;44:25–29. doi: 10.1016/j.jsr.2012.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hall KD, Guo J, Dore M, et al. The Progressive Increase of Food Waste in America and Its Environmental Impact. PLoS One. 2009 Nov 25;:4. doi: 10.1371/journal.pone.0007940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Leigh JP, Du J, McCurdy SA. An estimate of the U.S. government’s undercount of nonfatal occupational injuries and illnesses in agriculture. Ann Epidemiol. 2014;24:254–259. doi: 10.1016/j.annepidem.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Azaroff LS, Levenstein C, Wegman DH. Occupational injury and illness surveillance: conceptual filters explain underreporting. Am J Public Health. 2002 Sep;92:1421–1429. doi: 10.2105/ajph.92.9.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Leigh JP, Marcin JP, Miller TR. An estimate of the U.S. Government’s undercount of nonfatal occupational injuries. J Occup Env Med. 2004 Jan;46:10–18. doi: 10.1097/01.jom.0000105909.66435.53. [DOI] [PubMed] [Google Scholar]
- 45.Ruser JW. Examining evidence on whether BLS undercounts workplace injuries and illnesses. Mon Labor Rev. 2008 Aug;131:20–32. [Google Scholar]
- 46.Scribani M, Wyckoff S, Jenkins P, et al. Migrant and seasonal crop worker injury and illness across the northeast. Am J Ind Med. 2013;56:845–855. doi: 10.1002/ajim.22150. [DOI] [PubMed] [Google Scholar]
- 47.Steenland K, Burnett C, Lalich N, et al. Dying for work: The magnitude of US mortality from selected causes of death associated with occupation. Am J Ind Med. 2003;43:461–482. doi: 10.1002/ajim.10216. [DOI] [PubMed] [Google Scholar]
- 48.National Occupational Research Agenda Agricultural, Forestry, and Fishing Sector Council. National Agriculture, Forestry, and Fishing Agenda. Washington, DC: NIOSH; 2008. [Accessed July 8, 2014]. Available at: http://www.cdc.gov/niosh/nora/comment/agendas/AgForFish/pdfs/AgForFishDec2008.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


