Abstract
Background
Some patients referred for kidney transplant evaluation fail to attend the visit. Our goal was to compare demographic, socioeconomic, and psychological factors between evaluation visit attendees and absentees.
Methods
A convenience sample of patients referred and scheduled for kidney transplant evaluation at a single center from November 2012 to December 2013 participated in a phone survey reporting socioeconomic, demographic and clinical characteristics; health literacy; and perceived knowledge and concerns about transplantation. Absentees were matched by race with attendees. Analyses of differences between groups were performed with Chi-square, Fisher’s exact test, and t-tests. Multivariable logistic regression adjusted for relevant demographic characteristics.
Results
104 adults participated (61% male, 46% Caucasian, 52±12 years). Financial concerns were the most prevalent (67.3% affording medication, 64.1% affording operation). Prior evaluation at a different transplant center (p=0.029) and being on dialysis (p=0.008) were significantly associated with absence. Attendance was associated with concerns about finding a living donor (p=0.038) and higher perceived general knowledge about transplantation (p ≤0.001). No differences were appreciated in demographic, socioeconomic or health literacy factors between groups.
Conclusions
Both attendee and absentee patients were most concerned with the financial burden of kidney transplantation. While concerns and perceived knowledge are important correlates of behavior, other considerations such as psychological factors and prior medical experiences may influence patients’ ability to complete the kidney transplant evaluation process. Although this pilot study was conducted in a small sample and has limited generalizability, our findings can guide future research.
Keywords: kidney transplantation, education, evaluation, perceived knowledge, patient concerns, health literacy
Introduction
Socioeconomic and demographic disparities including minority race, older age and less educational attainment persist despite interventions designed to improve access to kidney transplantation (1-7). The complex kidney transplant process begins with referral to a transplant center, but there are several steps at which patients may fail to progress through the system. The referral process is often influenced by factors over which patients have limited control (nephrologists’ actions, dialysis unit policies, insurance status, etc.). However, failure to attend an initial evaluation visit after the referral has been initiated is a patient-dependent behavior. Not only does the failure to attend a visit negatively impact the evaluation timeline for the patient, unused clinic appointments financially burden the health-care system and delay evaluation for other potential transplant candidates. Increasing the proportion of successfully completed initial evaluation visits would improve quality of care.
Factors such as social and financial support, personal knowledge of and attitudes towards transplantation, and psychological burdens (e.g., fear, anxiety, and guilt) all influence patients’ decision making (8-10). Studies of barriers to transplantation have often been focused on racial disparities (11, 12). An expanded assessment of patient-reported thoughts, beliefs and concerns, beyond considerations of racial disparities, is necessary to better understand factors that may contribute to patient’s not completing their evaluation. Previous studies have evaluated either patients who had not yet been referred for evaluation, or those who had attended the evaluation visit (8-10, 13).
There is less research available describing the characteristics or experiences of patients who were referred but did not attend the initial evaluation visit because these patients are often difficult to contact and less likely to engage in research (11). A recent survey identified several perceived barriers to transplantation among a small mixed group of patients at various points in the evaluation process, but did not detect differences in concerns between patients based on evaluation visit completion status. Furthermore, health literacy was not assessed as a potential barrier to transplantation (14, 15). The aim of our study was to evaluate socioeconomic, demographic and clinical characteristics, health literacy, perceived knowledge, and concerns about evaluation and transplantation that may impact patients’ motivation and ability to complete the first step in the kidney transplantation process, which is the evaluation visit.
Results
Comparisons by Visit Completion Status
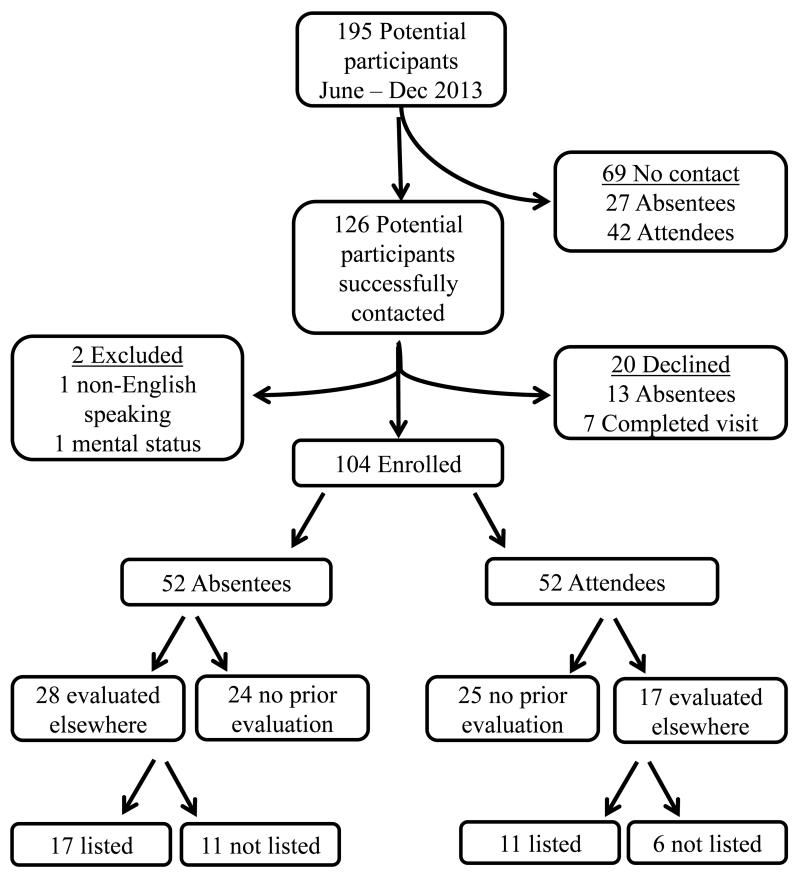
The final study cohort consisted of 104 participants (52 attendees, 52 absentees) (Figure 1). The study sample was 61% male, 46% Caucasian, and 52 ± 12 years of age. Among the attendees, two had previously not shown for an evaluation visit and 27 (51.9%) had previously cancelled an appointment between one and three times before the visit completion. Among the absentees, six had previously not shown for an evaluation appointment and 46 (88.5%) had previously cancelled an appointment. There were no significant differences in the age, race, gender, education, income, insurance, body mass index, distance to the transplant center, and the months from the scheduled visit to the interview date between the attendees and absentees. Prior evaluation at a different transplant center (p=0.029) and being on dialysis (p=0.008) were significantly correlated with absence. The majority of participants (77%) had adequate health literacy. There was no difference in the proportion of participants with limited health literacy in the absent and attended groups (Table 1).
Figure 1.
Flow chart of enrollment and participant visit status. Absentee and attendee participant groups were matched on race.
Table 1.
There were no significant differences in the demographic characteristics of participants based on visit attendance. GED = General Educational Development, SD = standard deviation
| Demographics | Absent | Attended | p-value |
|---|---|---|---|
|
| |||
| Age (years) – Mean ± SD | 54 ± 11 | 51 ± 13 | 0.189 |
|
| |||
| Race – n (%) | |||
| White | 24 (46.2%) | 24 (46.2%) | 1.000 |
| non-White | 28 (53.8%) | 28 (53.8%) | |
|
| |||
| Gender – n (%) | |||
| Male | 31 (59.6%) | 33 (63.5%) | 0.687 |
| Female | 21 (40.4%) | 19 (36.5%) | |
|
| |||
| Education – n (%) | |||
| ≤ 8th grade | 2 (3.8%) | 2 (3.8%) | 0.980 |
| High School or GED | 23 (44.2%) | 22 (42.3%) | |
| Some college | 27 (51.9%) | 28 (53.8%) | |
|
| |||
| Annual Household Income – n (%) | |||
| ≤ $20,000 | 25 (25.1%) | 21 (43.8%) | 0.716 |
| $20,000 - $60,000 | 17 (35.4%) | 20 (41.7%) | |
| > $60,000 | 6 (12.5%) | 7 (14.6%) | |
|
| |||
| Insurance Status – n (%) | |||
| Private only | 10 (19.2%) | 18 (34.6%) | 0.192 |
| Public only | 23 (44.2%) | 17 (32.7%) | |
| Both public and private | 19 (36.5%) | 17 (32.7%) | |
|
| |||
| Time from visit to interview (months) – Mean ± SD |
2.8 ± 2.4 | 3.3 ± 2.1 | 0.228 |
|
| |||
| Body Mass Index – Mean ± SD | 29.7 ± 6.2 | 29.3 ± 5.8 | 0.896 |
|
| |||
| Distance (miles) – Mean ± SD | 164 ± 142 | 131 ± 79 | 0.321 |
|
| |||
| Health Literacy – n (%) | |||
| Limited (3-9) | 12 (23.1%) | 12 (23.1%) | 1.000 |
| Adequate (10-15) | 40 (76.9%) | 40 (76.9%) | |
|
| |||
| Time from scheduled visit to interview (months) – Mean ± SD |
2.8 ± 2.4 | 3.3 ± 2.1 | 0.228 |
|
| |||
| Not currently on dialysis | 2 (3.8%) | 12 (23.1%) | 0.008 |
|
| |||
| Already evaluated elsewhere | 28 (53.8%) | 17 (32.7%) | 0.029 |
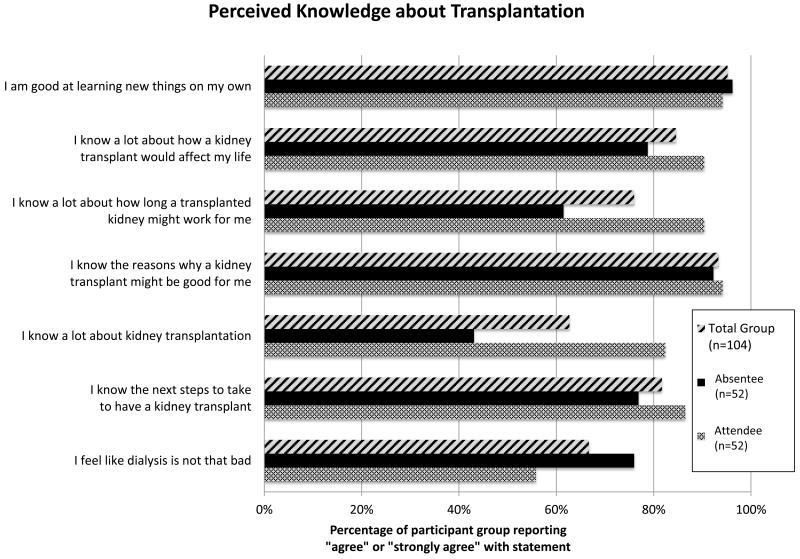
Perceived Knowledge about Transplantation
Overall, 93% of the entire cohort of participants agreed that they knew the reasons why a transplant might be beneficial. A higher proportion of attendees agreed that they “knew a lot about transplantation” and that they “knew how long a transplant would work for them” compared to the participants who did not have a visit (both p≤0.001). In contrast, a higher proportion of absentees agreed “dialysis is not that bad” compared to attendees (p=0.040) (Figure 2). In an analysis restricted to the absentee group, having adequate health literacy (n=40), compared to limited health literacy (n=12), was associated with agreement that “I know the next steps to take to have a kidney transplant” (90% vs. 34%; p<0.001).
Figure 2.
The proportion of participants reporting any agreement with statements on perceived knowledge about kidney transplantation. Percentages are displayed for the overall cohort and for each of the participant groups. Attendees at our center were more likely to report general knowledge about transplantation than participants in the absentee group.
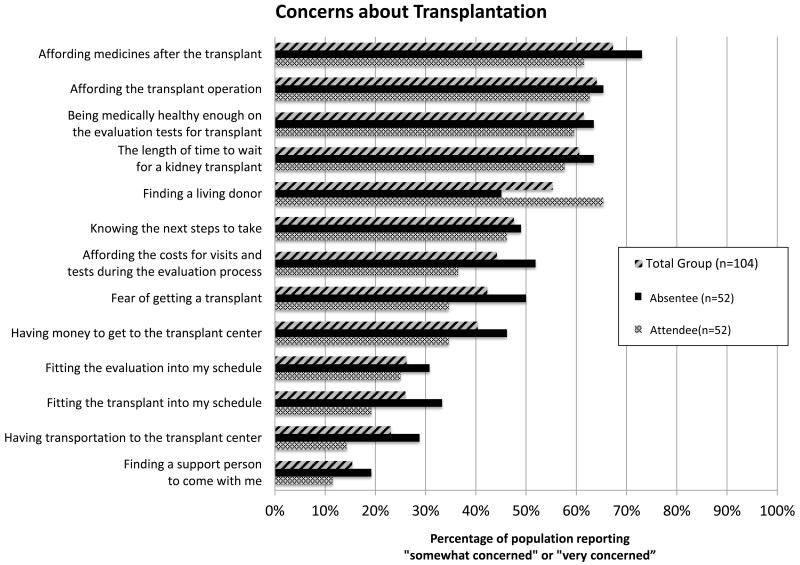
Concerns about Kidney Transplantation and Transplant Evaluation
Affording medication after transplantation (n=70, 67.3%) and affording the transplant operation (n=66, 64.1%) were the most common concerns reported by participants in the total cohort (Figure 3). There was no significant difference in the proportion of patients reporting these concerns based on race, income or type of insurance (all p>0.150). Of the 78 participants who indicated they were “very concerned” about any statement, 31 participants (39.7%) reported financial concerns and monetary issues were the most burdensome. The only concern noted by a higher proportion of attendees (n=34, 65.4%) than absentees (n=23, 40.4%) was “finding a living donor” (p=0.038). In all other potential concerns, a higher proportion of the absent group expressed concern but statistical significance was not reached.
Figure 3.
Percentages of participants reporting concerns are displayed for each statement in the total cohort and in each participant group. Participants who attended the initial visit were more likely to report concern about finding a living donor than absentee participants.
Logistic Regression
After adjusting for age, gender and income, attendance at the evaluation visit was significantly associated with reporting a concern about finding a living donor (p=0.031). A model that substituted insurance status for income demonstrated similar results, where attendance remained significantly related to concerns about finding a living donor (p<0.001). In adjusted models, attendance at the evaluation visit was also significantly associated with higher perceived knowledge, specifically with greater agreement with the statements “knowing a lot about transplantation” and “knowing how long a transplant works” (both p≤0.005).
Comparison of Previously Evaluated Absentees and Evaluation Visit Attendees
While it was anticipated that some participants had been evaluated at other transplant centers, unexpectedly, forty-five participants (43%) were evaluated elsewhere. Twenty-eight of the absentees (55%) had undergone evaluation elsewhere. Since these 28 participants likely had more education and exposure to transplantation than other absentees, we performed analyses comparing the 28 absentee participants who had been evaluated elsewhere to the 52 participants who attended the evaluation visit at our center. Seventeen (33%) of the 52 attendees had also been evaluated elsewhere and were included in the attendee group (Figure 2).
The proportions of attendees reporting knowledge about the next steps to take towards transplantation and general transplant knowledge trended towards being higher than those of absentees who had been evaluated elsewhere, but these comparisons did not reach statistical significance (both p<0.100) (Table 2). Absentees evaluated elsewhere reported more concern about having transportation to the transplant center and the length of time to wait for a kidney transplant (both p=0.027). The proportions of participants reporting agreement with statements about all others areas of perceived knowledge and concerns about transplantation were similar in both groups.
Table 2.
Participants attending the evaluation visit at our center (n=52) had less concern about transportation and about the length of time to wait for a transplant compared to those evaluated another transplant center and not evaluated at our center (n=28). The p-value for all other perceived knowledge statements and concerns not listed in the below table was > 0.200.
| Absentees previously evaluated at another center (n=28) |
Attendees (n=52) |
p-value | |
|---|---|---|---|
| Perceived knowledge about transplantation | |||
| I know the next steps to take to have a kidney transplant |
21 (75.0%) | 45 (86.5%) | 0.197 |
| I know a lot about kidney transplantation |
18 (64.2%) | 43 (82.4%) | 0.069 |
| I know a lot about how long a transplanted kidney might work for me |
21 (75.0%) | 47 (90.4%) | 0.066 |
| Concerns about transplantation | |||
| Finding a support person to come with me |
7 (25.0%) | 6 (11.5%) | 0.118 |
| Having transportation to the transplant center |
10 (35.7%) | 7 (14.3%) | 0.027 |
| Fitting the transplant into my schedule |
9 (32.1%) | 10 (19.2%) | 0.196 |
| Affording the costs for visits and tests during the evaluation process |
16 (57.1%) | 19 (36.5%) | 0.076 |
| Finding a living donor | 14 (50.0%) | 34 (65.4%) | 0.180 |
| The length of time to wait for a kidney transplant |
23 (82.1%) | 30 (57.7%) | 0.028 |
Comparison by Wait-Listing Status among Evaluation Visit Absentees
Among the 28 absentee participants evaluated elsewhere, 17 (61%) were wait-listed. Active wait-list participants were more concerned about the length of time to wait for a transplant and financial means to afford the transplant operation than those who were not wait-listed (both p≤0.040). The financial affordability of pre-transplant medical tests trended toward statistical significance, with 71% of wait-listed participants being concerned compared to 36% of non-wait listed participants (p=0.074). No other statistically significant differences in reported concerns or perceived knowledge were appreciated between the wait-listed and non-wait-listed absentee subgroups.
Discussion
Patients with end stage renal disease referred for kidney transplantation were concerned about the financial aspects of transplantation. These financial concerns outweighed fears about transplantation, and concerns about scheduling, health, and transportation. Attending the evaluation visit at our center was associated with more perceived general knowledge about transplantation and more concern about finding a living donor. Unexpectedly, a high proportion of absentee participants at our center had already been evaluated at another center and reported more concern about the wait-list time for a transplant and transportation to the center. Patients who have been previously listed at another center may be seeking a second listing to increase their likelihood of transplantation. These same patients, who had been listed elsewhere, were more likely to be absent for their transplant evaluation visit at our center. Perhaps the logistical, travel, time and financial burden of a second visit are more of a challenge than the perceived benefit of a second listing. Further research should explore patients’ perceptions and expectations around being listed for transplantation at multiple centers.
Prior studies indicate that patient concerns and perceived knowledge about end stage dialysis treatment options are determinants of patient behavior (3, 6, 8, 9, 12, 15). Also, patient education has been associated with improved graft and patient survival following transplantation as well as decreased racial disparities in transplantation (16, 17). While participants evaluated at any center reported more perceived knowledge than those not evaluated, the proportion of absentees evaluated elsewhere expressing general knowledge about transplantation was slightly lower than participants evaluated at our center. Differences in perceived knowledge may be due to absentees who were evaluated elsewhere having completed the evaluation visits months or years prior to this study. If transplant education effectiveness wanes with time as has been observed with other chronic medical conditions (18-20), perhaps more frequent and structured educational sessions are necessary throughout evaluation, wait-list, and post-transplant periods (17).
In a prior study of barriers to transplantation by Kazley et al., perceived knowledge about transplantation did not vary based on completion of an education class; however, only a portion of participants completed the education class (38.6%) and not all who had attended the class had seen a physician (42.2%) (15). In contrast, at our center, all participants who attended the evaluation visit participated in an education class and were evaluated by both a physician and social worker. Provider interactions at our center’s initial evaluation visit may partially explain the reported perceived knowledge differences between the attendee and absentee participant groups appreciated in our study. Patients who have more knowledge about the survival benefits of transplantation compared to dialysis may be more motivated to pursue transplantation, especially preemptive transplantation. This study was not designed to examine patients’ actual knowledge about transplantation prior to the evaluation visit. Future research should examine the role of pre-evaluation factual knowledge of transplantation.
Patients’ financial concerns are a potential barrier to engagement in kidney transplant evaluation (15, 21). All participants, regardless of visit status, were concerned about the cost of the evaluation visit, transplant operation, transportation, and medications. Interestingly, attendees reported increased concern about finding a living donor compared to those who did not attend the evaluation visit. This finding was not replicated among participants who had been evaluated previously at another center. The high rate of concern among attendees warrants further review of education processes and content, particularly regarding living donation. The goal of transplant education and evaluation is not to heighten concerns, but to better equip patients for shared decision-making and transplantation.
Patients have previously reported difficulty when discussing transplantation as a treatment option for end stage renal disease and live kidney donation with family and friends (15). Factors other than education and knowledge are likely influencing the process of living donor recruitment and the willingness of patients to discuss living donation with others. Specifically, the response of the persons within the patient’s social support system may impact the patient’s level of concern and his or her willingness to discuss living donation (22-24). Our study was not designed to include support persons or potential living donors accompanying patients to the evaluation visit. Future work should include more investigation of the specific factors about living donation that concerns patients.
Health literacy and other demographic and socioeconomic factors did not differ significantly between the attendees and absentees. Other studies of access to transplantation found race and other socioeconomic factors such as income and insurance type to be significantly associated with access to transplantation (5, 13). In most of these studies, patient information was collected from large databases, Medicare claims, and census data, which introduces concerns about data accuracy and detail. Additionally, these studies often included a large proportion of patients who had not been referred for transplantation. Our study was performed with direct interview, thus reducing potential limitations associated with analyses of incomplete or extrapolated data. Prior studies were primarily focused on racial disparities in transplantation (1, 5, 6), whereas we chose to match participant groups on race to expand the investigation beyond the question of racial disparity. Our choice to survey patients who had been referred and scheduled for evaluation visits, but who did not attend the visit, may account for our findings
To reduce the absences at our evaluation appointments, our center already employs multiple reminder systems including: 1) an automated appointment reminder system, 2) a personalized confirmation phone call, and 3) mailed instructions for the evaluation visit including directions, maps, and appointment lists. The high proportion of prior evaluations in the absentee group suggests that these reminders may not be sufficient for patients undergoing evaluation at an additional transplant center for the purpose of either double listing or to transfer wait-list time. A screening tool to identify patients at increased risk of absenteeism at the scheduled evaluation visit would increase efficiency and allow for directed intervention, which would ultimately benefit both patients and transplant centers. Enhanced educational information, including the benefits of transplantation compared to dialysis, may encourage patients to attend the evaluation visit and complete the evaluation process.
There are some important limitations of this study that must be acknowledged. This is a pilot study in a small sample, and the exploratory analyses performed to identify themes surrounding evaluation visit attendance may require further development. The size of the study cohort was limited due to the number of potential absentee participants whom we were unable to contact for lack of a current phone number. It is likely that this study does not have sufficient statistical power to definitively examine all of the study questions. However, many of the point estimates suggest that achieving or confirming statistical significance would be likely in a larger sample. The current study cohort is comprised of a convenience sample and may be limited by participation bias. Generalizability may be limited as this study was performed at a single transplant center. Factors that may influence attendance, including prior psychological history, depression, hospitalizations and operations, and other medical conditions, were not included in this study because medical data were not available for absentee participants. Also, due to the cross-sectional study design, we were unable to account for non-compliance in the pre-evaluation or during the evaluation process. These factors should be included in future research on this topic. Lastly, the time between the scheduled visit and survey completion did not differ significantly between attendees and absentees, which suggests that recall bias, if present, may have affected both groups equally.
Conclusions
Participants who attended the evaluation visit at our center reported more perceived knowledge about transplantation than absentees, but also more concern about living donation. A higher proportion of absent participants had been evaluated previously at another transplant center. In this race-matched study, there was no significant difference in patient concerns based on visit status. This finding indicates that, while concerns and perceived knowledge are important determinants of behavior, other considerations such as psychological factors, baseline compliance with medical care, and prior medical experiences may influence patients’ ability to complete the kidney transplant evaluation process. Furthermore, transplant centers and providers must have awareness of patient concerns about transplantation and work to develop strategies to overcome diverse factors influencing the initiation of a kidney transplant evaluation.
Materials and Methods
Study Sample
We performed an IRB-approved cross-sectional study of a convenience sample of patients who were referred and scheduled for an initial evaluation for kidney transplantation at a single center between November 2012 and December 2013. Participants were classified based on evaluation visit status: attended or absent. Absentees were matched on race with attendees in order to examine factors other than race that were potentially associated with visit completion. All study participants were >18 years of age and spoke English. Patients with limited mental status impacting their ability to complete the phone interview with intelligible answers were excluded from the study.
Data Collection
Potential participants were sent a letter informing them of the study and were then contacted via phone (up to 10 attempts) for verbal consent and survey completion. Participants completed a structured twenty-minute phone-based survey. Items included: demographic characteristics (educational attainment, income, insurance status, distance to the transplant center), clinical data (dialysis treatment history, body mass index), health literacy, perceived knowledge about kidney transplantation, and concerns about evaluation and transplantation. Topics about barriers to transplantation cited in prior research such as financial, transportation, and knowledge were included (15). Open-ended questions allowed participants to elaborate on particularly concerning topics.
Participants were asked to indicate their agreement with seven different statements relating to perceived knowledge about transplantation using a four-point Likert scale with the following potential responses: “strongly disagree”, “disagree”, “agree”, and “strongly agree.” The four-point Likert scale was combined into two categories of “agree” and “disagree” for analysis. Participants were also asked to indicate how concerned they were about twelve potential barriers to evaluation and transplantation and responded on a three point Likert scale: “not at all concerned”, “somewhat concerned”, and “very concerned.” For analysis, the concerns were grouped dichotomously into “no concern” or “somewhat concerned” and “very concerned”, which were grouped together as “any concern.”
Health literacy was assessed using the Brief Health Literacy Screen, a three-question subjective health literacy questionnaire answered on a five-point Likert scale (25, 26). These questions are valid for assessment of health literacy both via written and verbal administration in the transplant evaluation population (27). The questions are summed totaling 3-15 and then dichotomized into limited (total score=3-9) or adequate (total score=10-15) health literacy (28). Data were collected in RedCAP, a secure online data-management software. Participants were offered a $20 gift-card for their time.
Data Analysis
Proportions of the total cohort of participants citing concerns about transplantation and agreement with items assessing perceived knowledge were calculated and reported. Descriptive statistics were reported using frequencies, means and standard deviations. Analyses of differences between the absentee and attendee participant groups were performed with Chi-square, Fisher’s exact test, and t-tests. When the proportion of participants reporting any concern or agreement significantly differed in unadjusted analyses between the absentee and attendee groups, multivariate logistic regression that adjusted for age, gender and income was performed.
A proportion of participants had been evaluated previously at another center. Univariate analyses (Chi-square, Fisher’s exact test, and t-tests depending on data distribution) were performed to assess differences in perceived knowledge and concerns among absentees who were evaluated at another transplant center and participants who attended the evaluation visit at our center. Finally, because a proportion of participants evaluated elsewhere who did not compete a visit at our center were already listed at the time of the interview, univariate analyses were performed to test the association of listing status with perceived knowledge and concerns about transplantation.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Vanderbilt Transplant Center research funding support for this project. Dasha A. Bond assisted with the funding proposal and the identification of potential participants.
Forms of Support
The REDCap database is funded by the UL1 TR000445 grant from NCATS/NIH.
LA Dageforde is supported by the 2013 Association of Academic Surgery Research Fellowship Award.
A Box was supported by the Student Research Training Program in Kidney Disease (NIH 2T35 DK007383-34) and the O’Brien Center Grant (NIH 1P30 DK079341).
KL Cavanaugh is supported by a grant from the National Institutes of Health (K23 DK080952) and the American Society of Nephrology Carl W. Gottschalk Research Scholar Grant.
Footnotes
Authorship
LA Dageforde designed the study, performed the research, analyzed data, and wrote the paper, and revised the article.
A Box performed the research and revised the article.
ID Feurer designed the study, analyzed data and revised the article.
KL Cavanaugh designed the study, wrote the paper, and revised the article.
Disclosure
The authors of this manuscript have no conflicts of interest to disclose.
REFERENCES
- 1.Alexander GC, Sehgal AR. Barriers to cadaveric renal transplantation among blacks, women, and the poor. JAMA. 1998;280(13):1148. doi: 10.1001/jama.280.13.1148. [DOI] [PubMed] [Google Scholar]
- 2.Alexander GC, Sehgal AR. Why hemodialysis patients fail to complete the transplantation process. Am J Kidney Dis. 2001;37(2):321. doi: 10.1053/ajkd.2001.21297. [DOI] [PubMed] [Google Scholar]
- 3.Kucirka LM, Grams ME, Balhara KS, Jaar BG, Segev DL. Disparities in provision of transplant information affect access to kidney transplantation. Am J Transplant. 2012;12(2):351. doi: 10.1111/j.1600-6143.2011.03865.x. [DOI] [PubMed] [Google Scholar]
- 4.Lockwood MB, Saunders MR, Lee CS, Becker YT, Josephson MA, Chon WJ. Kidney transplant and the digital divide: is information and communication technology a barrier or a bridge to transplant for African Americans? Prog Transplant. 2013;23(4):302. doi: 10.7182/pit2013869. [DOI] [PubMed] [Google Scholar]
- 5.Schold JD, Gregg JA, Harman JS, Hall AG, Patton PR, Meier-Kriesche HU. Barriers to evaluation and wait listing for kidney transplantation. Clin J Am Soc Nephrol. 2011;6(7):1760. doi: 10.2215/CJN.08620910. [DOI] [PubMed] [Google Scholar]
- 6.Keith D, Ashby VB, Port FK, Leichtman AB. Insurance type and minority status associated with large disparities in prelisting dialysis among candidates for kidney transplantation. Clin J Am Soc Nephrol. 2008;3(2):463. doi: 10.2215/CJN.02220507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arthur T. The role of social networks: a novel hypothesis to explain the phenomenon of racial disparity in kidney transplantation. Am J Kidney Dis. 2002;40(4):678. doi: 10.1053/ajkd.2002.35672. [DOI] [PubMed] [Google Scholar]
- 8.Finkelstein FO, Story K, Firanek C, et al. Perceived knowledge among patients cared for by nephrologists about chronic kidney disease and end-stage renal disease therapies. Kidney Int. 2008;74(9):1178. doi: 10.1038/ki.2008.376. [DOI] [PubMed] [Google Scholar]
- 9.Abbott KC, Gaston RS. Counseling patients for kidney transplantation: awkward conversations? Am J Transplant. 2012;12(2):273. doi: 10.1111/j.1600-6143.2011.03868.x. [DOI] [PubMed] [Google Scholar]
- 10.Martin P. Living donor kidney transplantation: preferences and concerns amongst patients waiting for transplantation in New Zealand. J Health Serv Res Policy. 2013 doi: 10.1177/1355819613514957. [DOI] [PubMed] [Google Scholar]
- 11.Ayanian JZ, Cleary PD, Weissman JS, Epstein AM. The effect of patients’ preferences on racial differences in access to renal transplantation. N Engl J Med. 1999;341(22):1661. doi: 10.1056/NEJM199911253412206. [DOI] [PubMed] [Google Scholar]
- 12.Boulware LE, Hill-Briggs F, Kraus ES, et al. Identifying and addressing barriers to African American and non-African American families’ discussions about preemptive living related kidney transplantation. Prog Transplant. 2011;21(2):97. doi: 10.1177/152692481102100203. [DOI] [PubMed] [Google Scholar]
- 13.Boulware LE, Hill-Briggs F, Kraus ES, et al. Effectiveness of educational and social worker interventions to activate patients’ discussion and pursuit of preemptive living donor kidney transplantation: a randomized controlled trial. Am J Kidney Dis. 2013;61(3):476. doi: 10.1053/j.ajkd.2012.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dageforde LA, Cavanaugh KL. Health literacy: emerging evidence and applications in kidney disease care. Advances in chronic kidney disease. 2013;20(4):311. doi: 10.1053/j.ackd.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kazley AS, Simpson KN, Chavin KD, Baliga P. Barriers facing patients referred for kidney transplant cause loss to follow-up. Kidney Int. 2012;82(9):1018. doi: 10.1038/ki.2012.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldfarb-Rumyantzev AS, Sandhu GS, Barenbaum A, et al. Education is associated with reduction in racial disparities in kidney transplant outcome. Clinical transplantation. 2012;26(6):891. doi: 10.1111/j.1399-0012.2012.01662.x. [DOI] [PubMed] [Google Scholar]
- 17.Haspeslagh A, De Bondt K, Kuypers D, Naesens M, Breunig C, Dobbels F. Completeness and satisfaction with the education and information received by patients immediately after kidney transplant: a mixed-models study. Prog Transplant. 2013;23(1):12. doi: 10.7182/pit2013249. [DOI] [PubMed] [Google Scholar]
- 18.Cavanaugh K, Wallston KA, Gebretsadik T, et al. Addressing literacy and numeracy to improve diabetes care: two randomized controlled trials. Diabetes care. 2009;32(12):2149. doi: 10.2337/dc09-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCarthy DM, Waite KR, Curtis LM, Engel KG, Baker DW, Wolf MS. What did the doctor say? Health literacy and recall of medical instructions. Medical care. 2012;50(4):277. doi: 10.1097/MLR.0b013e318241e8e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dorresteijn JA, Kriegsman DM, Assendelft WJ, Valk GD. Patient education for preventing diabetic foot ulceration. The Cochrane database of systematic reviews. 2012;10 doi: 10.1002/14651858.CD001488.pub4. CD001488. [DOI] [PubMed] [Google Scholar]
- 21.Rodrigue JR, Reed AI, Nelson DR, Jamieson I, Kaplan B, Howard RJ. The financial burden of transplantation: a single-center survey of liver and kidney transplant recipients. Transplantation. 2007;84(3):295. doi: 10.1097/01.tp.0000269797.41202.79. [DOI] [PubMed] [Google Scholar]
- 22.Reese PP, Shea JA, Berns JS, et al. Recruitment of live donors by candidates for kidney transplantation. Clin J Am Soc Nephrol. 2008;3(4):1152. doi: 10.2215/CJN.03660807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rodrigue JR, Pavlakis M, Egbuna O, Paek M, Waterman AD, Mandelbrot DA. The “House Calls” trial: a randomized controlled trial to reduce racial disparities in live donor kidney transplantation: rationale and design. Contemp Clin Trials. 2012;33(4):811. doi: 10.1016/j.cct.2012.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sheu J, Ephraim PL, Powe NR, et al. African American and non-African American patients’ and families’ decision making about renal replacement therapies. Qual Health Res. 2012;22(7):997. doi: 10.1177/1049732312443427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Family medicine. 2004;36(8):588. [PubMed] [Google Scholar]
- 26.Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. Journal of general internal medicine. 2008;23(5):561. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dageforde LA, Cavanaugh KL, Moore DE, et al. Validation of the Written Administration of the Short Literacy Survey. Journal of health communication. 2014 Apr; doi: 10.1080/10810730.2015.1018572. Accepted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Willens DE, Kripalani S, Schildcrout JS, et al. Association of brief health literacy screening and blood pressure in primary care. Journal of health communication. 2013;18(Suppl 1):129. doi: 10.1080/10810730.2013.825663. [DOI] [PMC free article] [PubMed] [Google Scholar]