Abstract
Context:
Lateral ankle sprains are among the most common injuries in sport, with the anterior talofibular ligament (ATFL) most susceptible to damage. Although we understand that after a sprain, scar tissue forms within the ligament, little is known about the morphologic changes in a ligament after injury.
Objective:
To examine whether morphologic differences exist in the thickness of the ATFL in healthy, coper, and unstable-ankle groups.
Design:
Cross-sectional study.
Setting:
Laboratory.
Patients or Other Participants:
A total of 80 National Collegiate Athletic Association Division I collegiate athletes (43 women, 37 men, age = 18.2 ± 1.1 years, height = 175.8 ± 11.1 cm, body mass = 75.0 ± 16.9 kg) participated in this study. They were categorized into the healthy, coper, or unstable group by history of ankle sprains and score on the Cumberland Ankle Instability Tool.
Main Outcome Measure(s):
A musculoskeletal sonographic image of the ATFL was obtained from each ankle. Thickness of the ATFL was measured at the midpoint of the ligament between the attachments on the lateral malleolus and talus.
Results:
A group-by-limb interaction was evident (P = .038). The ATFLs of the injured limb for the coper group (2.20 ± 0.47 mm) and the injured limb for the unstable group (2.28 ± 0.53 mm) were thicker than the ATFL of the “injured” limb of the healthy group (1.95 ± 0.29 mm) at P = .015 and P = .015, respectively. No differences were seen in the uninjured limbs among groups.
Conclusions:
Because ATFL thicknesses of the healthy group's uninjured ankles were similar, we contend that lasting morphologic changes occurred in those with a previous injury to the ankle. Similar differences were seen between the injured limbs of the coper and unstable groups, so there must be another explanation for the sensations of instability and the reinjuries in the unstable group.
Key Words: ankle instability, anterior talofibular ligament, morphology
Key Points
The anterior talofibular ligament can be viewed using musculoskeletal ultrasound imaging.
The anterior talofibular ligaments of previously sprained ankles were thicker than those of uninjured ankles.
Although coper ankles were more functionally similar to healthy ankles than to unstable ankles, they were structurally different. Only further research can determine the relationship between ligament damage and functional stability of the ankle.
Musculoskeletal ultrasound (MSUS) imaging is a new technique being used in the sports medicine setting. Compared with other imaging techniques, such as radiographic or magnetic resonance imaging (MRI), MSUS offers a safer, more time-efficient, and more cost-effective alternative. A real-time image can be captured via MSUS by using a transducer to send high-frequency sound waves into the body and recording the echo of the sound waves reflecting back, providing an image of the internal structure.1,2 This method has been found to be effective in imaging upper extremity, lower extremity, and joint injuries.1,3,4
Oae et al3 reported greater than 90% accuracy for both MSUS and MRI in identifying injuries to the ankle. Lateral ankle sprains (LASs) are among the most common injuries in sport.5 An estimated 850 000 new ankle sprains occur each year in the United States,7 which does not include a 70% reinjury rate at the ankle.6 Ankle stability plays an important role in injury prevention. Passive stability of the ankle is predominantly the responsibility of ligaments supporting the bony structure of the talocrural joint because there are no musculotendinous insertions on the talus. Ligaments supporting the lateral complex of the ankle include the anterior talofibular ligament (ATFL), calcaneofibular ligament, and posterior talofibular ligament. The ATFL is a flat ligament that attaches from the anterior border of the lateral malleolus to the talus, just anterior to the lateral malleolus articular surface.8 The ATFL limits plantar flexion and inversion, motions that coincide with the most common mechanism of injury.8 As a result, the ATFL becomes vulnerable in a plantar-flexed and inverted position and is most susceptible to damage during an LAS.5,6,9 An isolated tear of the ATFL occurs in about 80% of LASs.10,11
After an LAS, the fibrous structure of an ankle ligament is often disrupted by severe damage. Using MRI, Takao et al12 reported visible scarring of the ATFL after injury. Using MSUS, McCarthy et al13 described a thickened ATFL, osseous spurs, and synovitic lesions after injury. Thickness values for the ATFL have been derived primarily from cadaveric studies14,15; however, MRI-based in vivo studies demonstrated thickness of the ATFL to be in the range of 2 to 3 mm.16,17 An abnormal ligament could affect the stabilizing properties of the ligament. In animal studies, although scar tissue formed within a ligament after injury, the newly scarred ligament allowed normal movement; however, the load capacity of that ligament was decreased by 60%.18–20 Therefore, the strength of a ligament can be sufficient for active movement and injury rehabilitation soon after injury, but the decrease in load capacity of the scarred ligament may affect its stabilizing properties.
Despite medical treatment and postinjury rehabilitation, more than 50% of individuals who sustain a moderate or severe ankle sprain experience some degree of residual disability and impairment due to symptoms such as pain, instability, loss of range of motion, and edema.6,21 Those who do not fully recover from their ankle sprain often develop chronic ankle instability (CAI), which limits function not only in sport but also in activities of daily living. Patients with CAI typically complain of the ankle “giving way” or of repeated ankle sprains under seemingly low-risk conditions.22
Typically, CAI researchers have categorized participants into 2 groups: those with ankle instability (unstable) and those without ankle instability (healthy). The unstable group consists of individuals who experience recurrent sprains, sensations of instability, or both. Unfortunately, this method of grouping ignores those who sustained an ankle sprain but did not experience recurrent sprains or sensations of instability. In general, an ankle “coper” refers to an individual who has experienced an initial ankle sprain but not a subsequent sprain.23 Only recently have copers been addressed in ankle-instability research.24–29 Because copers are still a new cohort in this research, the classification of ankle copers differs somewhat among researchers.25,28
Although we understand that the fibrous nature of a ligament is disrupted after an LAS, little is known about the actual morphologic changes in a ligament. Therefore, the purpose of our study, using a mixed-model analysis, was to determine whether MSUS can be used to see differences in ligament thickness between the uninjured limb and the injured limb among the healthy, coper, and unstable groups. We hypothesized that the ligaments of the previously injured ankles would be thicker than the uninjured ankles.
METHODS
Participants
A total of 80 National Collegiate Athletic Association Division I collegiate athletes (43 women, 37 men, mean age = 18.2 ± 1.1 years, mean height = 175.8 ± 11.1 cm, mean body mass = 75.0 ± 16.9 kg) participated in this study. Each participant completed the Cumberland Ankle Instability Tool (CAIT) and reported the number of sprains for each ankle (Table 1). Participants were excluded if they had a history of ankle surgery, had any sprain other than an LAS, or had experienced an ankle sprain within 6 months of data collection (excluding any acute physiologic response to the injury). Participants with a history of bilateral ankle sprains were excluded. All participants read and signed the informed consent approved by the University of Delaware Institutional Review Board, which also approved the study.
Table 1.
Detailed Demographic Data for Each Group
| Variable |
Healthy Group: Uninjured, “Injured” |
Coper Group: Uninjured, Injured |
Unstable Group: Uninjured, Injured |
| Number of participants | 46 | 24 | 10 |
| Sex, women/men | 24/22 | 13/11 | 6/4 |
| Mean ± SD | |||
| Height, cm | 174.4 ± 11.02 | 178.2 ± 11.8 | 176.8 ± 10.0 |
| Mass, kg | 73.7 ± 17.5 | 77.1 ± 16.0 | 76.0 ± 17.8 |
| Age, y | 18.3 ± 0.6 | 18.0 ± 1.8 | 18.3 ± 0.5 |
| Cumberland Ankle Instability Tool score | Uninjured: 28.6 ± 1.3 | Uninjured: 28.9 ± 1.2 | Uninjured: 29.0 ± 1.5 |
| “Injured”: 28.5 ± 1.4 | Injured: 28.4 ± 1.4 | Injured: 22.3 ± 4.3a,b | |
| Ankle sprains, No. | Uninjured: 0.0 ± 0.0 | Uninjured: 0.0 ± 0.0 | Uninjured: 0.0 ± 0.0 |
| “Injured”: 0.0 ± 0.0 | Injured: 1.0 ± 0.0c | Injured: 1.8 ± 0.6a,b | |
Indicates statistical significance between the unstable and coper limbs.
Indicates statistical significance between the unstable and uninjured limbs.
Indicates statistical significance between the coper and uninjured limbs.
Grouping
The CAIT is a valid and reliable questionnaire used to determine functional ankle instability from self-reported symptoms.30 Based on a 30-point system, a score of 26 or above is considered healthy, whereas a score of 25 or below is considered functionally unstable.31 Participants were grouped into the healthy, coper, and unstable groups by their CAIT scores and ankle injury histories. A healthy ankle was an ankle with no previous history of a sprain and with a score of 26 or above on the CAIT. Based on previous research,25,28 we developed a more stringent classification for a coper ankle, defining it as an ankle that (1) experienced a single previous sprain at least 12 months ago, (2) returned to the preinjury level of activity, (3) scored in the healthy group (≥26) of the CAIT, and (4) had no episodes of reinjury. An unstable ankle was one that scored 25 or below on the CAIT, regardless of the number of previous ankle sprains. Hence, the healthy group consisted of the participants who had bilaterally uninjured ankles; the coper group consisted of those who experienced unilateral sprains and currently had a healthy, uninjured ankle and a coper ankle; and the unstable group consisted of those who experienced unilateral sprains and currently had a healthy, uninjured ankle and an unstable ankle (Figure 1).
Figure 1.
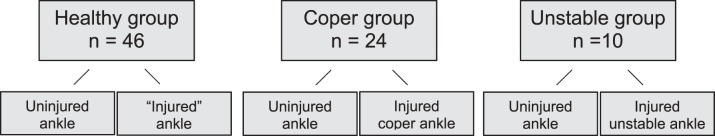
Group assignments.
Procedures
All imaging and thickness measurements were performed by the same examiner, who was blinded to the classification of the ankles. Measurements for thickness of the ATFL were obtained using MSUS. An ultrasound image of the ATFL was taken (model Logiq e compact ultrasound machine; General Electric Company, Waukesha, WI) using a 5- to 13-MHz multifrequency linear transducer. Because the ATFL is a superficial structure, the examiner (K.L.) set the transducer at a frequency of 12 MHz and an image depth of 2.5 cm to capture the clearest, highest resolution image possible. The transducer head was placed obliquely from the distal fibula, over the sinus tarsi area, capturing the origin and insertion point of the ATFL (Figure 2). Ultrasonic gel (Aquasonic 100; Parker Laboratories, Inc, Fairfield, NJ) was used as the conductive medium for the sound waves to travel between the probe and the skin.
Figure 2.

Placement of the transducer head for Imaging the anterior talofibular ligament.
Once the examiner identified the ligament, she manipulated the angle of the transducer head to capture the superficial and deep borders of the ligament. After the full image of the ligament was captured, it was saved. Thickness of the ATFL was measured at the midpoint of the ligament between the attachments on the lateral malleolus and talus using the built-in measuring tool of the MSUS unit (Figure 3). We analyzed the reliability of the thickness measurements by calculating intraclass correlation coefficients (ICCs) between 2 researchers (ICC = 0.91). Measurements were taken from both ankles.
Figure 3.
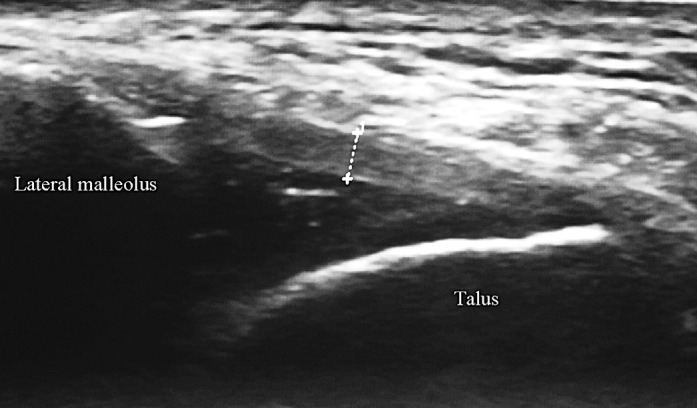
A musculoskeletal ultrasound image of the anterior talofibular ligament and thickness measurement.
Data Analysis
The independent variables were group (healthy, coper, unstable) and limb (uninjured, injured). The healthy group consisted of the participants who had bilaterally uninjured ankles. However, 1 limb of each participant in the healthy group was operationally defined as “injured” for the sake of statistical analyses, even though it was not truly an injured limb. The coper group consisted of those who had experienced a unilateral sprain and currently had an uninjured ankle and a coper ankle. The unstable group consisted of those who had experienced a unilateral sprain and currently had an uninjured ankle and an unstable ankle. The dependent variable was the thickness of the ATFL. A mixed-model 3 × 2 analysis of variance was used to analyze between-subjects and within-subject interactions of group and limb factors. We conducted post hoc analyses using a Bonferroni adjustment. Data were analyzed using SPSS (version 19.0; SPSS, Inc, Chicago, IL). Statistical significance was set at P ≤ .05.
RESULTS
No statistically significant differences were demonstrated in demographic data among groups in sex, age, height, and body mass. The CAIT scores between the unstable and coper groups, as well as between the unstable and healthy groups, were different at P < .001. The mean number of sprains among groups was also statistically different at P < .001.
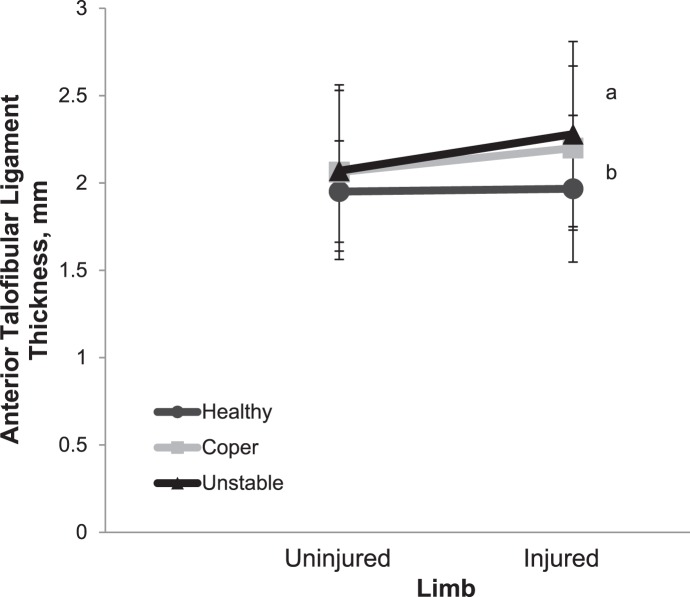
We observed group-by-limb interaction (F2,73 = 3.432, P = .038, effect size = 0.086), as shown in Figure 4. The partial η2 was used for the effect size. A partial η2 of 0.086 represents a greater than medium effect size.32 The Bonferroni post hoc analysis (Table 2) revealed a thicker ATFL for the injured limb of the coper group compared with the “injured” limb of the healthy group (P = .015). The ATFL was also thicker in the injured limb of the unstable group compared with the “injured” limb of the healthy group (P = .015). No differences were detected in the uninjured control limbs among the groups (Table 3).
Figure 4.
Limb-by-group analysis showing interaction. a Indicates a difference between the “injured” limb of the healthy group and the injured limb of the unstable group (P = .015). b Indicates a difference between the “injured” limb of the healthy group and the injured limb of the coper group (P = .015).
Table 2.
Post Hoc Pairwise Comparisons
| Limb Comparison |
P Value |
| Healthy uninjured to coper uninjured | .424 |
| Healthy uninjured to unstable uninjured | .512 |
| Coper uninjured to unstable uninjured | .963 |
| Healthy “injured” to coper injured | .015a |
| Healthy “injured” to unstable injured | .015a |
| Coper injured to unstable injured | .584 |
Indicates statistical significance.
Table 3.
Anterior Talofibular Ligament Thickness Between Groups, mm (Mean ± SD)
| Group |
Anterior Talofibular Ligament Thickness |
|
| Uninjured Limb |
Injured Limb |
|
| Healthy | 1.97 ± 0.42 | 1.95 ± 0.29 |
| Coper | 2.06 ± 0.50 | 2.20 ± 0.47a |
| Unstable | 2.07 ± 0.46 | 2.28 ± 0.53b |
Indicates a difference between the “injured” limb of the healthy group and the injured limb of the coper group (P = .015).
Indicates a difference between the “injured” limb of the healthy group and the injured limb of the unstable group (P = .015).
DISCUSSION
The thickness of the ATFL was not different between the uninjured ankles of the same participants in the healthy group. Yet the ATFL was thicker in the previously injured ankles of the coper and unstable groups compared with the “injured” ankle of the healthy group. Therefore, we conclude that morphologic changes occurred in the ATFLs of previously injured ankles. The thicknesses of the ATFLs measured using MSUS in this study were similar to those reported by Dimmick et al16 using MRI. We found a 0.25- to 0.33-mm increased thickness of the injured coper and unstable ankles compared with the healthy “injured” ankles. Although differences of 0.25 to 0.33 mm may not seem substantial, they represent an increase of nearly 16% in ligament thickness compared with the ATFL of an ankle that had never been injured. Understanding the morphologic changes to the static restraints of the ankle joint after injury is needed to determine the extent of the injury and to make postinjury treatment recommendations.
The interaction of the group-by-limb factors shows that the differences within the limbs depend on the group (Figure 4). The nearly horizontal line of the healthy group shows that the ankles of the healthy group did not differ. The steeper slopes of the lines for the coper and unstable groups show the interaction of the differences between groups. These morphologic changes are reflected by the increased thickness of the ATFL in previously injured ankles. Because ligament thickness did not differ among the uninjured, control ankles across groups, we suggest that the morphologic changes that occurred were secondary to the ankle injury. However, a prospective study is needed to confirm this hypothesis.
To reduce the 70% reinjury rate for patients with ankle sprains,6 we need to understand why copers (a new cohort in ankle-instability research) do not experience recurrent sprains. Although scarred ligaments have a reduced tolerance for high loads,20 our findings showed that the morphologies of the coper and unstable ankles were similar. Therefore, a previous injury may have caused lasting morphologic changes in the ligament, but it is not simply the structure of the ligament that causes instability. Given that CAI is a multifaceted problem, it is important to have a comprehensive understanding of all of the changes an individual experiences to understand the difference between those who are ankle copers and those who suffer from the long-term effects of multiple ankle sprains. Because CAI can be caused not only by mechanical insufficiencies but also by functional deficiencies,33 appreciating the sensorimotor changes is necessary. Continued research on the uninjured, coper, and unstable groups is required to acquire a more robust comprehension of the differences among groups and ways to prevent recurrent ankle sprains. We acknowledge that a paired comparison of participants with an unstable ankle and a coper ankle would strengthen this study. In fact, 4 participants presented with an unstable ankle and a coper ankle. However, the low power of such a small participant pool meant that we could not identify true differences between those ankles.
Therefore, in addition to understanding the anatomic differences of the ATFL after an ankle sprain, it is important to be familiar with the physiologic and sensorimotor changes. The ankle ligaments have been assumed to become more lax with each subsequent sprain. Yet a previous study involving our participants casts doubt on this theory.34 Liu et al34 found that ligament laxity, as assessed by an ankle arthrometer, did not increase with each subsequent sprain. Croy et al29 reported similar increases in ligament length in the anterior and inversion directions of the coper and CAI groups. Thus, ligament laxity does not seem to be affected by the number of ankle sprains, even though an apparent change is seen in the ligaments of previously injured ankles. We know that the load capacity of a newly scarred ligament can be decreased by 60%.20 Hence, understanding both the anatomic and physiologic alterations to the ligament is essential to appreciating the effect of injury on the passive restraints of the ankle. Other biomechanical factors could also affect the integrity of the ligament. Perhaps passive joint stiffness explains the lack of difference in ligament laxity despite a structural difference. Joint stiffness is characterized by the resistance to change during stretching.35 Recognizing changes in joint laxity with force may better explain the physiologic changes in the ligament after injury and the anatomic changes seen in this current study. However, further research is necessary to comprehend the biomechanical alterations of a ligament resulting from injury.
Because CAI does not stem solely from mechanical insufficiencies, it is possible that the symptoms experienced by these individuals are caused in part by sensorimotor changes. This could further explain why morphologic changes were similar between the coper and unstable groups, yet only the participants in the unstable group complained of lasting symptoms of instability. Balance deficits affected by the sensorimotor system are a major symptom of ankle instability.36,37 Changes in motor control of the brain in both feedback and feedforward mechanisms have been reported.37 This could explain why, although both the coper and unstable groups presented with ligamentous abnormalities, only the unstable group complained of the symptoms of instability.
We acknowledge limitations to this study. First, injury history was based only on participant recall. Second, the group sizes were unequal. However, although the latter factor may affect the statistical analyses, it may still clinically represent those who experience these unilateral injuries. Third, the lack of further physiologic data, such as laxity or sensorimotor measures, limits our ability to justify the differences among groups. Further research incorporating these data would add to our understanding of joint changes after injury.
Morphologic changes occur in the ATFLs of previously injured ankles. Because one of the main roles of ligaments is to provide stability to a joint, these morphologic changes could compromise joint stability. Yet not all patients with a history of ankle sprain complain of residual symptoms. Therefore, during the rehabilitation of an ankle sprain, clinicians should focus on preventing permanent alterations of ligaments and targeting functional deficiencies. Interventions such as prophylactic bracing and modalities that lessen uncontrolled scar tissue formation could be useful.
REFERENCES
- 1.Chew K, Stevens KJ, Wang TG, Fredericson M, Lew HL. Introduction to diagnostic musculoskeletal ultrasound: part 2, examination of the lower limb. Am J Phys Med Rehabil. 2008;87(3):238–248. doi: 10.1097/PHM.0b013e31816198c2. [DOI] [PubMed] [Google Scholar]
- 2.Nofsinger C, Konin JG. Diagnostic ultrasound in sports medicine: current concepts and advances. Sports Med Arthros Rev. 2009;17(1):25–30. doi: 10.1097/JSA.0b013e3181982add. [DOI] [PubMed] [Google Scholar]
- 3.Oae K, Takao M, Uchi Y, Ochi M. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skeletal Radiol. 2010;39(1):41–47. doi: 10.1007/s00256-009-0767-x. [DOI] [PubMed] [Google Scholar]
- 4.Petranova T, Vlad V, Porta F, et al. Ultrasound of the shoulder. Med Ultrason. 2012;14(3):133–140. [PubMed] [Google Scholar]
- 5.Garrick JG. The frequency of injury, mechanism of injury, and epidemiology of ankle sprains. Am J Sports Med. 1977;5(6):241–242. doi: 10.1177/036354657700500606. [DOI] [PubMed] [Google Scholar]
- 6.Yeung MS, Chan KM, So CH, Yuan WY. An epidemiological survey on ankle sprain. Br J Sports Med. 1994;28(2):112–116. doi: 10.1136/bjsm.28.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ., Jr The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92(13):2279–2284. doi: 10.2106/JBJS.I.01537. [DOI] [PubMed] [Google Scholar]
- 8.Taser F, Shafiq Q, Ebraheim NA. Anatomy of lateral ankle ligaments and their relationship to bony landmarks. Surg Radiol Anat. 2006;28(4):391–397. doi: 10.1007/s00276-006-0112-1. [DOI] [PubMed] [Google Scholar]
- 9.Dufek JS, Bates BT. Biomechanical factors associated with injury during landing in jump sports. Sports Med. 1991;12(5):326–337. doi: 10.2165/00007256-199112050-00005. [DOI] [PubMed] [Google Scholar]
- 10.Broström L. Sprained ankles, 3: clinical observations in recent ligament ruptures. Acta Chir Scand. 1965;130(6):560–569. [PubMed] [Google Scholar]
- 11.Renstrom PA, Konradsen L. Ankle ligament injuries. Br J Sports Med. 1997;31(1):11–20. doi: 10.1136/bjsm.31.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Takao M, Innami K, Matsushita T, Uchio Y, Ochi M. Arthroscopic and magnetic resonance image appearance and reconstruction of the anterior talofibular ligament in cases of apparent functional ankle instability. Am J Sports Med. 2008;36(8):1542–1547. doi: 10.1177/0363546508315537. [DOI] [PubMed] [Google Scholar]
- 13.McCarthy CL, Wilson DJ, Coltman TP. Anterolateral ankle impingement: findings and diagnostic accuracy with ultrasound imaging. Skeletal Radiol. 2008;37(3):209–216. doi: 10.1007/s00256-007-0411-6. [DOI] [PubMed] [Google Scholar]
- 14.Burks RT, Morgan J. Anatomy of lateral ankle ligaments. Am J Sports Med. 1994;22(1):72–77. doi: 10.1177/036354659402200113. [DOI] [PubMed] [Google Scholar]
- 15.Muhle C, Frank LR, Rand T, et al. Collateral ligament of the ankle: high-resolution MR imaging with a local gradient coil and anatomic correlation in cadavers. Radigraphics. 1999;19(3):673–683. doi: 10.1148/radiographics.19.3.g99ma06673. [DOI] [PubMed] [Google Scholar]
- 16.Dimmick S, Kennedy D, Daunt N. Evaluation of thickness and appearance of anterior talofibular and calcaneofibular ligaments in normal versus abnormal ankles with MRI. J Med Imaging Radiat Oncol. 2009;52(6):559–563. doi: 10.1111/j.1440-1673.2008.02018.x. [DOI] [PubMed] [Google Scholar]
- 17.Ahmad MA, Pandey UC, Crerand JJ, al-Shareef Z, Lapinsuo M. Magnetic resonance imaging of the normal and injured lateral collateral ligaments of the ankle. Ann Chir Gynaecol. 1998;87(4):311–316. [PubMed] [Google Scholar]
- 18.Clayton ML, Weir GJ., Jr Experimental investigations of ligamentous healing. Am J Surg. 1959;98:373–378. doi: 10.1016/0002-9610(59)90529-x. [DOI] [PubMed] [Google Scholar]
- 19.Korkala O, Rusanen M, Gronblad M. Healing of experimental ligament rupture: findings by scanning electron microscopy. Arch Orthop Trauma Surg. 1984;102(3):179–182. doi: 10.1007/BF00575229. [DOI] [PubMed] [Google Scholar]
- 20.Frank C, Amiel D, Woo SL, Akeson W. Normal ligament properties and ligament healing. Clin Orthop Related Res. 1985;196:15–25. [PubMed] [Google Scholar]
- 21.Bosien WR, Staples OS, Russell SW. Residual disability following acute ankle sprains. J Bone Joint Surg Am. 1955;37(6):1237–1243. [PubMed] [Google Scholar]
- 22.Freeman MA. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47(4):669–677. [PubMed] [Google Scholar]
- 23.Hertel J, Kaminski TW. Second international ankle symposium summary statement. J Orthop Sports Phy Ther. 2005;35(5):A2–A6. [PubMed] [Google Scholar]
- 24.Brown C. Foot clearance in walking and running in individuals with ankle instability. Am J Sports Med. 2011;39(8):1769–1776. doi: 10.1177/0363546511408872. [DOI] [PubMed] [Google Scholar]
- 25.Brown C, Padua D, Marshall SW, Guskiewicz K. Individuals with mechanical ankle instability exhibit different motion patterns than those with functional ankle instability and ankle sprain copers. Clin Biomech (Bristol Avon) 2008;23(6):822–831. doi: 10.1016/j.clinbiomech.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 26.Brown CN, Padua DA, Marshall SW, Guskiewicz KM. Variability of motion in individuals with mechanical or functional ankle instability during a stop jump maneuver. Clin Biomech (Bristol Avon) 2009;24(9):762–768. doi: 10.1016/j.clinbiomech.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 27.Wikstrom EA, Fournier KA, McKeon PO. Postural control differs between those with and without chronic ankle instability. Gait Posture. 2010;32(1):82–86. doi: 10.1016/j.gaitpost.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 28.Wikstrom EA, Tillman MD, Chmielewski TL, Cauraugh JH, Naugle KE, Borsa PA. Self-assessed disability and functional performance in individuals with and without ankle instability: a case control study. J Orthop Sports Phy Ther. 2009;39(6):458–467. doi: 10.2519/jospt.2009.2989. [DOI] [PubMed] [Google Scholar]
- 29.Croy T, Saliba SA, Saliba E, Anderson MW, Hertel J. Differences in lateral ankle laxity measured via stress ultrasonography in individuals with chronic ankle instability, ankle sprain copers, and healthy individuals. J Orthop Sports Phys Ther. 2012;42(7):593–600. doi: 10.2519/jospt.2012.3923. [DOI] [PubMed] [Google Scholar]
- 30.Hiller CE, Refshauge KM, Bundy AC, Herbert RD, Kilbreath SL. The Cumberland ankle instability tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006;87(9):1235–1241. doi: 10.1016/j.apmr.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 31.Wright CJ, Arnold B, Ross SE. Validation of a recalibrated Cumberland Ankle Instability Tool cutoff score for chronic ankle instability. J Athl Train. 2011;46:S124. [Google Scholar]
- 32.Cohen JE. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates Inc; 1988. [Google Scholar]
- 33.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364–375. [PMC free article] [PubMed] [Google Scholar]
- 34.Liu K, Gustavsen G, Kaminski TW. Increased incidence of ankle sprain does not lead to an increase in ligament laxity. Med Sci Sports Exerc. 2011;43(5):S84. doi: 10.1097/JSM.0b013e31829afc03. [DOI] [PubMed] [Google Scholar]
- 35.Latash ML, Zatsiorsky VM. Joint stiffness: myth or reality. Hum Mov Sci. 1993;12(6):653–692. [Google Scholar]
- 36.McKeon PO, Hertel J. Systematic review of postural control and lateral ankle instability, part I: can deficits be detected with instrumented testing? J Athl Train. 2008;43(3):293–304. doi: 10.4085/1062-6050-43.3.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hertel J. Sensorimotor deficits with ankle sprains and chronic ankle instability. Clin Sports Med. 2008;27(3):353–370. doi: 10.1016/j.csm.2008.03.006. [DOI] [PubMed] [Google Scholar]