Abstract
Background
Clinical in-stent restenosis (CISR) is the main limitation of coronary angioplasty with stent implantation.
Objective
Describe the clinical and angiographic characteristics of CISR and the outcomes over a minimum follow-up of 12 months after its diagnosis and treatment.
Methods
We analyzed in 110 consecutive patients with CISR the clinical presentation, angiographic characteristics, treatment and combined primary outcomes (cardiovascular death, nonfatal acute myocardial infarction [AMI]) and combined secondary (unstable angina with hospitalization, target vessel revascularization and target lesion revascularization) during a minimal follow-up of one year.
Results
Mean age was 61 ± 11 years (68.2% males). Clinical presentations included acute coronary syndrome (ACS) in 62.7% and proliferative ISR in 34.5%. CISR was treated with implantation of drug-eluting stents (DES) in 36.4%, Bare Metal Stent (BMS) in 23.6%, myocardial revascularization surgery in 18.2%, balloon angioplasty in 15.5% and clinical treatment in 6.4%. During a median follow-up of 19.7 months, the primary outcome occurred in 18 patients, including 6 (5.5%) deaths and 13 (11.8%) AMI events. Twenty-four patients presented a secondary outcome. Predictors of the primary outcome were CISR with DES (HR = 4.36 [1.44–12.85]; p = 0.009) and clinical treatment for CISR (HR = 10.66 [2.53–44.87]; p = 0.001). Treatment of CISR with BMS (HR = 4.08 [1.75–9.48]; p = 0.001) and clinical therapy (HR = 6.29 [1.35–29.38]; p = 0.019) emerged as predictors of a secondary outcome.
Conclusion
Patients with CISR present in most cases with ACS and with a high frequency of adverse events during a medium-term follow-up.
Keywords: Myocardial Infarction; Stents; Graft Occlusion, Vascular; Coronary Restenosis; Myocardial Ischemia
Introduction
Since the first angioplasty performed in 1977 by Andreas Gruentzig, and despite technical and pharmacological improvements, restenosis continues to be the main limitation of interventional cardiology1,2. The introduction of stents has eliminated the occurrence of elastic recoil and chronic negative remodeling, and reduced the rate of restenosis. However, since neointimal hyperplasia still persists, restenosis has not been completely eliminated3.
Clinical in-stent restenosis (CISR) is defined as the presence of symptoms of myocardial ischemia and/or evidence of ischemia on functional tests after percutaneous coronary intervention (PCI), associated with coronary angiographic evidence of stenosis ≥ 50% either on the site of the previously treated vessel, inside the stent, or 5 millimeters proximally or distally to the previously treated vessel, requiring a new revascularization procedure of the target lesion4. Rates of CISR are around 10%-15%5,6, whereas angiographic ISR occurs at rates up to 50%7-10.
In this context, drug-eluting stents (DES) have been developed to delay or eliminate the vascular response to the injury caused by the metal. The use of DES has decreased the restenosis rate to around 6%11-13, with maintained results on short- and long-term follow-up14,15.
CISR may present as an acute coronary syndrome (ACS) with increased morbidity and mortality2,16,17. However, there are limited data in the literature regarding clinical outcomes after treatment of CISR. The aim of this study is to report the clinical and angiographic characteristics of CISR and the outcomes of patients followed up for a minimum of twelve months after the diagnosis and treatment of CISR.
Methods
Design
The cohort consisted of patients presenting with CISR and consecutively admitted to the Hemodynamics and Interventional Cardiology Service of Hospital Madre Teresa in Belo Horizonte from January 1, 2009 to April 30, 2011. After the CISR event and its treatment, patients were followed up for at least twelve months.
Ethical aspects
In addition, whe examined with the patient was supported by the public health care system (SUS- Sistema Único de Saúde) or a private health care plan.
Patients selection
We included all patients aged ≥ 18 years who presented to Hospital Madre Teresa after the first episode of CISR from January 1, 2009 to April 30, 2011, and who were treated at this institution. Exclusion criteria were restenosis in arterial or venous grafts and occurrence of a second CISR (re-restenosis).
The initial selection included 119 patients who presented with CISR in the period mentioned above. Nine of these patients were excluded, four of them due to restenosis in a saphenous vein graft and five due to re-restenosis. The final cohort consisted of 110 patients. The outcomes were assessed in all patients and none were lost to follow-up.
Characterization of restenosis
CISR was defined as the occurrence of symptoms of myocardial ischemia or evidence of myocardial ischemia on functional tests after PCI, along with evidence of either a new stenosis ≥ 50% in the previously treated vessel, inside the stent or 5 mm proximally or distally to the lesion requiring a new revascularization of the target lesion4.
Risk factors, comorbidities and medications
Information about the clinical characteristics of the patients at baseline was retrieved from medical records.s We considered in their personal history the occurrence of prior AMI, prior coronary bypass surgery (CAGB), ejection fraction (LVEF) determined by echocardiogram, medication use on admission and risk factors for cardiovascular disease (age, gender, hypertension, dyslipidemia, diabetes mellitus [DM], smoking, family history of coronary heart disease [CHD] and chronic renal failure [CRF] not treated with dialysis). We assessed the use of the following medications: aspirin, thienopyridine derivatives (clopidogrel), beta-blockers, angiotensin-converting enzyme inhibitors (ACE inhibitor), angiotensin II receptor blockers (ARB), nitrates, calcium channel blockers and statins.
Information about most risk factors was obtained from self-reported morbidity. Hypertension was considered present if reported by the patient or if the patient reported use of antihypertensive medication. Similarly, dyslipidemia was considered present if reported by the patient, if the patient reported use of lipid-lowering medication, or if evidenced on a laboratory test. A diagnosis of DM was established if the patient reported use of diabetes medications. If the use of such medications was reported, we identified whether it was an oral hypoglycemic drug or insulin. A positive smoking status was considered for those patients who smoked regularly until the collection of the data.
Creatinine was measured at baseline and was considered elevated when ≥ 1.5 mg/dL. Family history was considered positive for CHD when a first-degree male and/or female presented AMI when aged ≤ 55 years and ≤ 65 years, respectively. In addition, we examined whether the admission was covered by Brazil’s Unified Health System (Sistema Único de Saúde - SUS) or by supplementary health insurance.
Clinical presentation and management
We evaluated the types of clinical presentation, the average time for occurrence of CISR, whether CISR occurred after implantation of Bare Metal Stent (BMS) or drug-eluting stent (DES), the type of treatment performed, angiographic characteristics of CISR and the outcomes that occurred within twelve months from the date of the clinical presentation.
Clinical presentation was divided into six categories: asymptomatic with a positive test for ischemia, congestive heart failure (CHF), stable angina, unstable angina (UA), non-ST-segment elevation myocardial infarction (NSTEMI) and ST-segment elevation myocardial infarction (STEMI).
The average time for the occurrence of CISR was assessed in months from the date of the stent implantation to the date of the clinical presentation.
Treatment of CISR was divided into five types: PCI with BMS implantation, PCI with DES implantation, balloon PCI, CAGB and clinical treatment.
Follow-up and outcomes
The primary outcome was the occurrence of a major cardiac event (MACE), defined as cardiovascular death and nonfatal AMI, including periprocedural events. The secondary outcome was a composite of documented UA requiring hospitalization, target vessel revascularization (TVR) and target lesion revascularization (TLR).
Outcomes were initially assessed via telephone contact at least one year after the treatment for CISR. In the occurrence of an event, a face-to-face visit was then performed. All the events were confirmed with information retrieved from medical records, laboratory tests and electrocardiogram. In the case of death, the death certificate was checked. If more than one event had occurred during follow-up, the outcome that occurred first was considered.
Deaths were classified as cardiac and non-cardiac18. Nonfatal AMI was defined as the presence of at least two of the following criteria: clinical presentation of chest pain, presence of a new pathological Q wave in two or more contiguous electrocardiographic leads, or increase in myocardial necrosis markers18. We considered UA as the occurrence of a documented Braunwald class IIIB UA, defined as an acute, unstable primary angina with one or more episodes in the previous 48 hours19 and requiring hospital admission. We defined as a TLR those reinterventions due to recurrence of the lesion within the stent implanted in the index procedure, or in the vascular segment extending 5 mm proximally or distally to the stent. A TVR was defined as a percutaneous or surgical reintervention for revascularization of the treated vessel.
Angiographic analysis
Angiographic analysis was performed with a previously validated digital system (Philips XCelera PACS, Amsterdam, the Netherlands) and independently conducted by two experienced and blinded interventional cardiologists. In the event of a disagreement, the assessment was then conducted by a third interventional cardiologist, and the final analysis was then considered.
The data analyzed from the angiographic reports included the location of the restenosis in the artery, Mehran’s classification of restenosis20, the Thrombolysis in Myocardial Infarction (TIMI) flow grade prior to the procedure21, the presence of lesions ≥ 50% in the left coronary trunk (LCT) or ≥ 70% in other vessels, and the semiquantitative ventriculography.
Mehran’s classification20 divides ISR into four classes, namely class I (“focal”; < 10 mm in length), class II (“diffuse”; > 10 mm in length, but confined to the stent), class III (“proliferative”; > 10 mm and extending beyond the margins of the stent) and class IV (“occlusive”; presenting as a total occlusion).
TIMI21 flow was graded as TIMI 0 if there was no opacification beyond the occlusion point, TIMI 1 if there was no opacification of the terminal portion of the vessel (penetration without perfusion), TIMI 2 when there was complete opacification of the vessel, but with delayed flow compared with the adjacent vessels and TIMI 3 if there was complete opacification of the vessel with similar flow as the adjacent vessels.
Semiquantitative ventriculography was classified as normal, or as having a mild, moderate, or severe dysfunction.
Statistical analysis
Continuous variables are presented as mean ± standard deviation (SD) or median (interquartile range), whereas categorical variables are presented as frequency (%). The Kolmogorov-Smirnov test was used to test the normality of the distribution of continuous variables. Clinical and angiographic characteristics of patients with and without outcomes were compared with the chi-square test, Fisher's exact test, Student's t test, or Mann-Whitney test, according to the type and distribution of the variable. Two-tailed p values < 0.05 were considered statistically significant. A cumulative survival curve was constructed with the Kaplan-Meier method, and the events rates were compared using the log-rank test. Univariate and multivariate analysis with the Cox proportional hazards model was used to determine the contribution of independent variables. Variables identified with p < 0.10 in the univariate analysis were included in the final Cox proportional model. All analyses were performed with SPSS version 20.0 (SPSS Inc., Chicago, IL).
Results
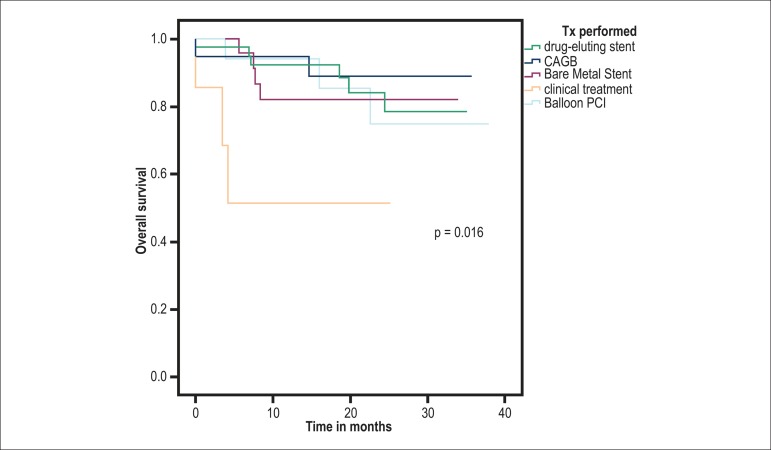
The cohort consisted of 110 patients with CISR who were followed up for 19.5 ± 10.2 months (median of 19.7 months, minimum of 12 months and maximum of 38 months; Graph 1). Clinical and angiographic characteristics of the general cohort and of the groups with and without a primary outcome are shown in Table 1. The only statistical difference between these groups occurred in the frequency of treatment with nitrates (p < 0.001).
Graph 1.
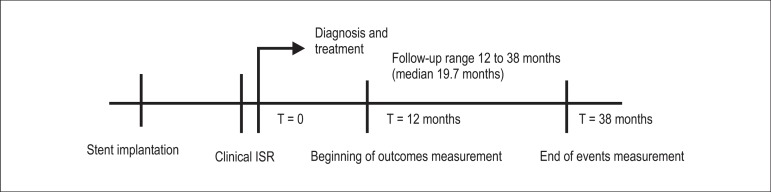
Study design analyzing CISR patients after treatment. CISR: clinical in-stent restenosis; T: time
Table 1.
Clinical and angiographic characteristics on presentation of patients with CISR with and without a primary outcome
| All patients (n = 110) | With outcome (n = 18) | Without outcome (n = 92) | p | |
|---|---|---|---|---|
| Age(years) | 61 ± 11 | 61 ± 12 | 61 ± 10 | 0.93 |
| Male gender | 75 (68.2) | 9(50.0) | 66 (71.7) | 0.70 |
| SUS | 56 (50.9) | 10 (55.6) | 46 (50.0) | 0.66 |
| CISR in DES | 12 (10.9) | 5(27.8) | 7 (7.6) | 0.26 |
| CISR time (months) * | 13.5 (4.7 - 55) | 11.0 (5 - 28) | 20 (4 - 65) | 0.79 |
| Clinical presentation | ||||
| CHF | 5 (4.5) | 2(11.1) | 3(3.3) | |
| Asymptomatic and positive test | 5 (4.5) | 0 | 5(5.4) | |
| Stable angina | 31 (28.2) | 5(27.8) | 26 (28.3) | 0.93 |
| Unstable angina | 50 (45.5) | 7(38.9) | 43 (46.7) | |
| NSTEMI | 14 (12.8) | 4(22.2) | 10 (10.9) | |
| STEMI | 5 (4.5) | 0 | 5(5.4) | |
| Hypertension | 98 (89.1) | 18 (100) | 80 (87) | 0.21 |
| Dyslipidemia | 100 (90.9) | 17 (94.4) | 83 (90.2) | 0.77 |
| Smoking | 15 (13.6) | 2(11.1) | 13 (14.1) | 0.72 |
| Diabetes Mellitus (DM) | 40 (36.4) | 9 (50) | 61 (33.7) | 0.18 |
| DM - insulin | 17 (15.5) | 5(27.8) | 12 (13) | 0.15 |
| Baseline creatinine (mg/dL) | 1.0 (0.8 - 1.2) | 1.0 (0.8 - 1.2) | 1.1 (0.8 - 1.15) | 0.84 |
| Creatinine ≥ 1.5 mg/dL | 9 (8.2) | 3 (16.7) | 6 (6.5) | 0.12 |
| Prior AMI | 68 (61.8) | 14 (77.8) | 54 (58.7) | 0.19 |
| Prior CAGB | 18 (16.4) | 3 (16.7) | 15 (16.3) | 0.97 |
| Positive FH | 23 (20.9) | 5 (27.8) | 18 (19.6) | 0.52 |
| LVEF(%) | 54 (40-63) | 45 (38-63) | 57 (40 - 63) | 0.36 |
| Restenosis treatment | ||||
| CAGB | 20 (18.2) | 2(11.1) | 18 (19.6) | |
| PCI DES | 40 (36.4) | 6 (33.3) | 34 (37) | |
| PCI BMS | 26 (23.2) | 4 (22.2) | 22 (23.9) | 0.37 |
| Balloon PCI | 17 (15.5) | 3 (16.7) | 14 (15.2) | |
| Clinical therapy | 7 (6.4) | 3 (16.7) | 4 (4.3) | |
| ISR arterial location | ||||
| Anterior descending | 58 (52.7) | 10 (55.6) | 48 (52.2) | |
| Circumflex | 20 (18.2) | 4 (22.2) | 16 (17.4) | 0.76 |
| Right coronary | 30 (27.3) | 4 (22.2) | 26 (28.3) | |
| Left coronary trunk | 2 (1.8) | 0 | 2(2.2) | |
| TIMI flow before the procedure | ||||
| TIMI 0 or 1 | 12 (10.9) | 18 (11.1) | 10 (10.9) | |
| TIMI 2 | 13 (11.8) | 4 (22.2) | 9(9.8) | 0.37 |
| TIMI 3 | 85 (77.3) | 12 (66.7) | 73 (79.3) | |
| Type of ISR † | ||||
| Focal | 25 (22.7) | 4(22.2) | 21 (22.8) | |
| Diffuse | 36 (32.7) | 5 (27.8) | 31 (33.7) | 0.95 |
| Proliferative | 38 (34.5) | 7 (38.9) | 31 (33.7) | |
| Occlusive | 11 (10.0) | 2(11.1) | 9(9.8) | |
| Semiquantitative LVEF | ||||
| Normal LV | 12 (10.9) | 1 (5.6) | 11 (12.0) | |
| Mild LV dysfunction | 20 (18.2) | 5 (27.8) | 15 (16.5) | 0.64 |
| Moderate LV dysfunction | 34 (30.9) | 4 (22.2) | 30 (32.6) | |
| Severe LV dysfunction | 36 (32.7) | 7 (38.9) | 29 (31.5) | |
| Other vessels ≥ 70‡ | 46 (41.8) | 8 (44.4) | 38 (41.3) | 0.80 |
| Medication after ISR Tx | ||||
| Aspirin | 109 (99.1) | 18 (100) | 91 (98.9) | 0.65 |
| Clopidogrel | 98 (82.7) | 17 (94.4) | 74 (80.4) | 0.19 |
| Beta-blocker | 91 (82.7) | 14 (77.8) | 77 (83.7) | 0.51 |
| ACEi | 43 (39.1) | 7 (38.9) | 36 (39.1) | 0.98 |
| ARB | 28 (25.5) | 3 (16.7) | 25 (27.2) | 0.55 |
| Calcium channel blocker | 7 (6.4) | 1 (5.6) | 6 (6.5) | 0.89 |
| Nitrate | 17 (15.5) | 9 (50) | 8 (8.7) | 0.00 |
| Statin | 109 (99.1) | 18 (100) | 91 (98.9) | 0.65 |
Quantitative variables are presented as mean ± standard deviation and median (interquartile range), whereas qualitative variables are presented as absolute number (%).
Time between the stent implantation and CISR presentation.
Restenosis classification according to Mehran.
Other vessels with ≥ 70% lesion in addition to the artery with restenosis. CISR: clinical in-stent restenosis; CHF: cardiac heart failure; SUS: Unified Health System; DM: diabetes mellitus; ISR: in-stent restenosis; AMI: acute myocardial infarction; CAGB: coronary bypass surgery; FH: family history; LVEF: ejection fraction; PCI: percutaneous coronary intervention; DES: drug-eluting stent; BMS: bare metal stent; STEMI: ST-segment elevation myocardial infarction; NSTEMI: non-ST-segment elevation myocardial infarction; TIMI: Thrombolysis In Myocardial Infarction flow; LV: left ventricle; Tx: treatment; ACEi: angiotensin-converting enzyme inhibitor; ARB: angiotensin II receptor blocker.
There were 75 (68.2%) male patients, with an average age of 61 ± 11 years (range 37 to 87 years). As for the types of treatment performed, there was a predominance of DES implantation (40 patients, 36.4%), followed by BMS implantation in 26 (23.6%), CAGB in 20 (18.2%), balloon PCI in 17 (15.5%) and clinical treatment in seven (6.4%; Table 2). CAGB was uneventful in 17 cases, but two patients had postoperative AMI and one had a stroke. There were no deaths related to CISR therapy during hospitalization.
Table 2.
Outcomes of patients with CISR after a minimum follow-up of 12 months
| Outcomes | N (%) |
|---|---|
| Primary outcome* (MACE) | 18 (16.4) |
| Nonfatal AMI | 13 (11.8) |
| Q AMI | 4 |
| Non-Q AMI | 9 |
| Cardiovascular death | 6(5.5) |
| Secondary outcome† | 24 (21.8) |
| TVR | 11 (10) |
| TLR | 3 (2.7) |
| TVR -TLR | 11 (10) |
| Unstable angina with readmission | 13 (11.8) |
The total number of individual primary outcomes was 19: 18 patients had a single event and one patient had two events.
The total number of individual secondary outcomes was 27: three patients had two events, TVR and TLR. Qualitative variables are presented as number (%). CISR: clinical in-stent restenosis; MACE: major cardiac events; AMI: acute myocardial infarction; Q AMI: Q acute myocardial infarction; Non-Q AMI: non-Q acute myocardial infarction; TLR: target lesion revascularization; TVR: target vessel revascularization; TVR + TLR: target vessel revascularization + target lesion revascularization.
Fifty-four (49.1%) patients were covered by supplementary health insurance, whereas 56 (50.9%) were covered by SUS. An analysis of the type of treatment according to the health coverage (SUS vs. supplementary health) showed that treatment with BMS predominated in patients covered by SUS (21.8% vs. 1.8%), whereas supplementary health insurance predominated in patients treated with DES (34.5% vs. 1.8%).
The median time between the stent implantation and the occurrence of CISR was 13.5 months (4.7 to 55 months). As for the angiographic classification, proliferative ISR (type III) occurred in 38 (34.5%) patients, followed by diffuse ISR (type II) in 36 (32.7%) of the cases.
An ACS was the main clinical presentation, occurring in 69 patients (62.7%), with 50 (45.5%) of the patients presenting with UA, followed by 14 (12.8%) cases of NSTEMI and 5 (4.5%) cases of STEMI. In the remaining cases, there were 31 (28.2%) cases of stable angina, 5 (4.5%) cases of CHF and 5 (4.5%) asymptomatic patients. As for the clinical presentation according to the health coverage plan (SUS vs. supplementary health), ACS occurred in 35.5% of the patients covered by SUS and in 27.3% of the patients covered by supplementary health insurance (p = 0.643).
The outcomes were assessed in all patients and none of the patients were lost to follow-up. Eighteen (16.4%) patients had a MACE, 13 (11.8%) of which consisted of nonfatal AMI, and 6 (5.5%) of cardiovascular death. One patient presented two primary events, and the event that occurred first was the one considered in the analysis. The secondary outcome occurred in 24 (21.8%) cases, 13 (11.8%) of which consisted of UA requiring readmission, and 11 (10%) of TVR and TLR (Table 2).
During follow-up there were 6 (5.5%) deaths and 13 (11.8%) nonfatal AMI events. All deaths were cardiovascular-related; none of the deaths were related to the procedures of surgical or percutaneous intervention and two infarcts occurred after CAGB and one after PCI.
Overall, 98 patients (89.1%) had a BMS implantation and 12 (10.9%) had a DES implantation. Among patients with a primary outcome, 13 (72.2%) had an ISR in an implanted BMS and 5 (27.8%) had an ISR in an implanted DES. In the group presenting a secondary outcome, there were 20 (83.3%) ISR in an implanted BMS, and 4 (16.7%) ISR in an implanted DES.
Initial clinical and angiographic characteristics of the group of patients with and without secondary outcomes are shown in Table 3.
Table 3.
Clinical and angiographic characteristics on presentation of patients with CISR with and without a secondary outcome
| All patients (n = 110) | With outcome (n = 24) | Without outcome (n = 86) | P | |
|---|---|---|---|---|
| Age (years) | 61 ± 11 | 61 ± 12 | 61 ± 10 | 0.93 |
| Male gender | 75 (68.2) | 16 (66.7) | 59 (68.6) | 0.85 |
| SUS | 56 (50.9) | 16 (66.7) | 40 (46.5) | 0.08 |
| CISR in DES | 12 (10.9) | 4 (16.7) | 8 (9.3) | 0.24 |
| CISR time (months) * | 13.5 (4.7 - 55) | 11 (5.0 - 28) | 20 (4.0 - 65) | 0.79 |
| Clinical presentation | ||||
| CHF | 5 (4.5) | 1 (4.2) | 4 (4.7) | |
| Asymptomatic and positive test | 5 (4.5) | 1 (4.2) | 4 (4.7) | |
| Stable angina | 31 (28.2) | 5 (20.8) | 26 (30.2) | 0.87 |
| Unstable angina | 50 (45.5) | 11 (45.8) | 39 (45.3) | |
| NSTEM | 14 (12.8) | 4 (16.7) | 10 (11.6) | |
| STEMI | 5 (4.5) | 2 (8.3) | 3 (3.5) | |
| Hypertension | 98 (89.1) | 23 (95.8) | 75 (87.2) | 0.21 |
| Dyslipidemia | 100 (90.9) | 24 (100) | 76 (88.4) | 0.31 |
| Smoking | 15 (13.6) | 2 (11.1) | 13 (14.1) | 0.72 |
| Diabetes Mellitus (DM) | 40 (36.4) | 9 (50.0) | 61 (33.7) | 0.18 |
| DM - insulin | 17 (15.5) | 5 (27.8) | 12 (13.0) | 0.15 |
| Baseline creatinine (mg/dL) | 1.0 (0.8 - 1.2) | 1.0 (0.8 - 1.2) | 1.0 (0.8 - 1.1) | 0.84 |
| Creatinine ≥ 1.5 mg/dL | 9 (8.2) | 3 (16.7) | 6 (6.5) | 0.12 |
| Prior AMI | 68 (61.8) | 15 (62.5) | 53 (61.6) | 0.93 |
| Previous CAGB | 18 (16.4) | 5 (20.8) | 13 (15.1) | 0.53 |
| Positive FH | 23 (20.9) | 7 (29.2) | 16 (18.6) | 0.26 |
| LVEF (%) | 54 (40 - 63) | 45 (38 - 63) | 57 (40 - 63) | 0.36 |
| Restenosis treatment | ||||
| CAGB | 20 (18.2) | 2 (8.3) | 18 (20.9) | |
| PCI DES | 40 (36.4) | 5 (20.8) | 35 (40.7) | |
| PCI BMS | 26 (23.2) | 12 (50.0) | 14 (16.3) | 0.01 |
| Balloon PCI | 17 (15.5) | 3 (12.5) | 14 (16.3) | |
| Clinical treatment | 7 (6.4) | 2 (8.3) | 5 (5.8) | |
| ISR arterial location | ||||
| Anterior descending | 58 (52.7) | 7 (29.2) | 51 (59.3) | |
| Circumflex | 20 (18.2) | 6 (25) | 14 (16.3) | 0.03 |
| Right coronary | 30 (27.3) | 11 (45.8) | 19 (22.1) | |
| Left coronary trunk | 2(1.8) | 0 | 2 (2.3) | |
| TIMI flow before the procedure | ||||
| TIMI 0 or 1 | 12 (10.9) | 1 (4.2) | 11 (12.8) | |
| TIMI 2 | 13 (11.8) | 2 (8.3) | 11 (12.8) | 0.36 |
| TIMI 3 | 85 (77.3) | 21 (87.5) | 64 (74.4) | |
| Type of ISR† | ||||
| Focal | 25 (22.7) | 4 (16.7) | 21 (24.4) | |
| Diffuse | 36 (32.7) | 12 (50.0) | 24 (27.9) | 0.20 |
| Proliferative | 38 (34.5) | 7 (29.2) | 31 (36.0) | |
| Occlusive | 11 (10.0) | 1 (4.2) | 10 (11.6) | |
| Semiquantitative LVEF | ||||
| Normal LV | 12 (10.9) | 3 (12.5) | 9 (10.5) | |
| Mild LV dysfunction | 20 (18.2) | 6(25.0) | 14 (16.3) | 0.55 |
| Moderate LV dysfunction | 34 (30.9) | 9(37.5) | 25 (29.1) | |
| Severe LV dysfunction | 36 (32.7) | 5(20.8) | 31 (36.0) | |
Quantitative variables are presented as mean ± standard deviation and median (interquartile range), whereas qualitative variables are presented as absolute number (%).
Time between the stent implantation and CISR presentation.
Restenosis classification according to Mehran. CISR: clinical in-stent restenosis; CHF: cardiac heart failure; SUS: Unified Health System; DM: diabetes mellitus; ISR: in-stent restenosis; AMI: acute myocardial infarction; CAGB: coronary bypass surgery; FH: family history; LVEF: ejection fraction; PCI: percutaneous coronary intervention; DES: drug-eluting stent; BMS: bare metal stent; STEMI-ST: segment elevation myocardial infarction; NSTEMI: non-ST-segment elevation myocardial infarction; TIMI: Thrombolysis In Myocardial Infarction flow; LV: left ventricle.
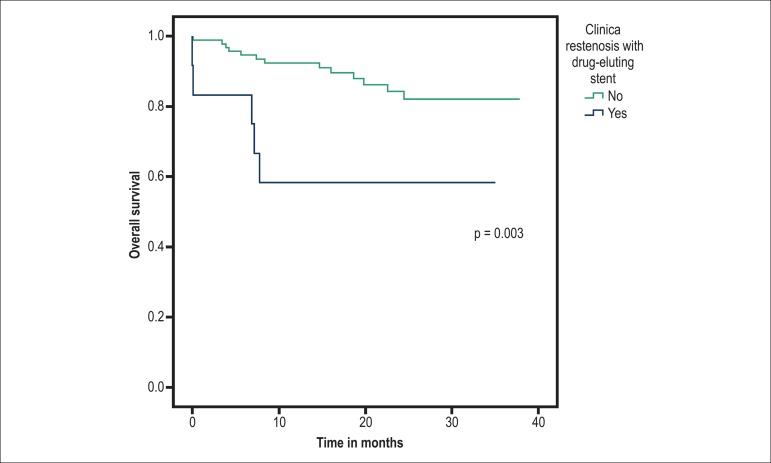
On univariate analysis, the selected variables were CISR with DES (HR = 4.36; 95% confidence interval [CI] 1.53-12.41; p = 0.006), clinical treatment of CISR (HR = 6.71; 95% CI 1.90-23.7; p = 0.003), DM using insulin (HR = 2.71; 95% CI 0.96–7.63; p = 0.058) and male gender (HR = 0.38; 95% CI 0.15-0.97; p = 0.043). On multivariate analysis, CISR with DES (HR = 4.36; 95% CI 1.44–12.85; p = 0.009) and clinical treatment of CISR (HR = 10.66; 95% CI 2.53–44.87; p = 0.001) remained as independent risk factors for death or nonfatal AMI (MACE; Table 4; Graphs 2 and 3).
Table 4.
Univariate and multivariate analysis with Cox proportional hazard model of the risk of occurrence of a primary outcome (MACE) and a secondary outcome in patients with CISR
| HR | Univariate 95% CI | p | HR | Multivariate 95% CI | p | |
|---|---|---|---|---|---|---|
| Primary outcome | ||||||
| Male gender | 0.38 | 0.15 - 0.97 | 0.043 | 0.38 | 0.13 - 1.05 | 0.62 |
| DM - insulin | 2.71 | 0.96 - 7.63 | 0.058 | 1.18 | 0.38 - 3.61 | 0.768 |
| CISR in DES | 4.36 | 1.53 - 12.41 | 0.006 | 4.36 | 1.44 - 12.85 | 0.009 |
| Clinical treatment of CISR* | 6.71 | 1.90 - 23.7 | 0.003 | 10.66 | 2.53 - 44.87 | 0.001 |
| Secondary outcome | ||||||
| Clinical treatment of CISR* | 6.46 | 1.22 - 34.00 | 0.028 | 6.29 | 1.35 - 29.38 | 0.019 |
| Treatment of CISR with BMS* | 4.18 | 1.46 - 11.89 | 0.007 | 4.08 | 1.75 - 9.48 | 0.001 |
CISR: clinical in-stent restenosis; DM: diabetes mellitus; DES: drug-eluting stent; BMS: bare metal stent.
Adjusted by other types of treatment.
Graph 2.
Kaplan-Meier curve of cardiovascular mortality and nonfatal heart attack according to CISR treatment (n = 110). Tx performed: treatment performed; CAGB: coronary bypass surgery; PCI: percutaneous coronary intervention; CISR: clinical in-stent restenosis.
Graph 3.
Kaplan-Meier curve of cardiovascular mortality and non-fatal heart attack according to CISR with drug-eluting stent (n = 110). CISR: clinical in-stent restenosis.
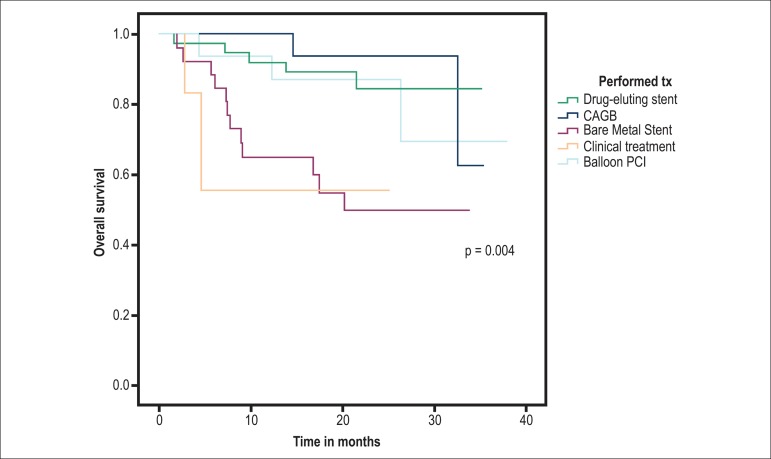
As for the secondary outcome, univariate analysis identified clinical treatment of CISR (HR = 6.46; 95% CI 1.22–34.00; p = 0.028) and treatment of CISR with a BMS (HR = 4.18; 95% CI 1.46–11.89; p = 0.007). These factors remained as independent predictors in the multivariate analysis of the risk of the combined outcome of UA with readmission, TVR and TLR, clinical treatment of CISR (HR = 6.29; 95% CI 1.35–29.38; p = 0.019) and treatment of CISR with implantation of a BMS (HR = 4.08; 95% CI 1.75–9.48; p = 0.001; Table 4; Graph 4).
Graph 4.
Kaplan-Meier curve for TVR, TLR and UA according to the treatment of CISR (n = 110). TVR: target lesion revascularization; TLR: target vessel revascularization; UA: unstable angina; CISR: clinical in-stent restenosis; Performed Tx: performed treatment; CAGB: coronary bypass surgery; Balloon PCI: balloon percutaneous coronary intervention.
Discussion
This study demonstrated in the context of a routine clinical practice that there is a long-term increased risk of death or nonfatal AMI in patients with CISR in whom restenosis occurred in DES, and in those who received clinical treatment. It also showed an increased risk of UA with hospital readmission or with revascularization in patients treated with a new BMS implantation and in those who remained in clinical treatment.
The main clinical presentation in our study was ACS, both in the general cohort (62.7%) as well as in the groups of patients with primary (61.1%) and secondary (70.8%) outcomes. In both these groups, there was a predominance of UA, followed by NSTEMI and STEMI. Previous studies have demonstrated that CISR is not a benign event, presenting in most cases as an AMI or UA, both with BMS and DES7,16,17,21. Although CISR presentation with ACS has been associated in previous studies with increased incidence of adverse cardiovascular events, angiographic restenosis and new revascularization procedures22-24, such associations were not observed in our study, perhaps due to the small size of our cohort.
There was a predominance in the evaluated sample of the angiographic ISR pattern class III (proliferative; 34.5%), followed by class II (diffuse; 32.7%). Recurrence rates of restenosis are associated with the angiographic pattern, with higher rates of new revascularization found in diffuse lesions - type II (around 34.5%) and proliferative lesions - type III (around 50%). Even though the angiographic pattern of ISR based on Mehran’s classification20 has been associated with prognostic and therapeutic implications, we did not find a relationship between the angiographic pattern and the occurrence of primary or secondary outcomes.
One of the most significant findings of this study is the observation of an increased risk of death (HR = 4.36) or new nonfatal AMI (HR = 4.36) in patients presenting CISR with DES when compared with BMS, even after multivariate analysis. This finding is relevant, since the main advantage of DES is to reduce ISR and new revascularization rates. This has expanded in recent years the recommendations for PCI with approach of more complex lesions and in patients with comorbidities11,25. It has already been recognized in previous studies that ISR with DES is associated with greater severity, higher rates of MACE and new interventions due to its difficult approach26,27. The treatment of ISR with DES has not been defined yet and there are several options available, such as balloon PCI, BMS implantation, DES with a similar drug or a different drug, drug-eluting balloon and CAGB28-32. Thus, although less frequent, ISR with DES is associated with worse outcomes compared with ISR with BMS33-35. Since we did not evaluate the criteria for initial indication of DES implantation, it may have been due to an increased severity of the lesions which may have interfered with our result.
With DES, there is a delay in endothelialization and persistence of the inflammatory process caused by the antiproliferative drug which causes ISR to occur later, around twelve months after implantation11. New clinical and histological studies with DES have shown evidence of a continuous and late neointimal growth secondary to a process of neointimal hyperplasia associated with atherosclerotic changes at the stent site called neoatherosclerosis36. In this context, bioabsorbable stents seem to be an attractive therapeutic strategy, since they prevent the growth of neointimal tissue, without adding more metal structures to the vessel wall37.
Clinical treatment after the diagnosis of CISR, when compared with other forms of treatment, was associated with increased risk of adverse outcomes: a risk greater than ten times (HR = 10.62) of death or new AMI compared with other forms of treatment, and six times higher (HR = 6.28) of UA with hospital readmission or new revascularization (TVR and TLR). All seven (6.4%) patients who remained in clinical treatment after the diagnosis of ISR did not undergo a new revascularization procedure due to technical limitation. Our results corroborate the findings of Gottschall et al.38, who described that patients with CISR not treated with a new revascularization procedure and who remained in long-term clinical treatment showed higher rates of MACE (death, AMI and CAGB), compared with patients who underwent a new revascularization procedure.
Regarding the treatment of CISR and secondary events, we had a worse result in patients treated clinically or with BMS compared with those treated with DES implantation, balloon, or surgical treatment. Treatment of CISR with BMS was associated with a four-fold increased risk (HR = 4.08) of UA with hospital readmission or new revascularization (TVR and TLR) compared with other treatments. These results are in agreement with the state of the art in interventional cardiology, since the main advantage of DES is exactly the prevention of new interventions.
The profile of the patients who received clinical treatment did not differ much from that of patients in the general group. Patients treated clinically had an average age of 58.86 (± 5.6) years and were mostly males (85.7%). All patients in this group had hypertension and dyslipidemia, 28.6% were smokers, 42.9% had insulin-dependent DM and 14.3% had a prior CAGB. Presentation in these patients was as an ACS in 71.4%, UA in 57.1% and NSTEMI in 14.3%. None of the patients in this group presented with STEMI. When we analyzed the occurrence of previous AMI, we observed that it had occurred in 71.4% of the patients in this group, which was different from the rate in the general group, and that 71.4% of the patients who received clinical treatment were covered by SUS, but this comparison did not reach statistical significance.
Our choice of Braunwald class IIIB UA requiring admission for a secondary outcome was due to its greater severity, with a higher rate of long-term adverse cardiac events39,40, and the possibility of documentation of the events during the patient’s admission.
A unique aspect of our study was the finding that the type of stent (DES or BMS) used for the treatment of CISR differed according to the health coverage of the patient (SUS vs. supplementary health). Most patients with ISR treated with BMS were covered by SUS (21.8% vs. 1.8%), whereas most of the ones treated with DES were covered by supplementary health insurance (34.5% vs. 1.8%). Treatment with DES of two patients covered by SUS was determined by court order. This difference is a reflection of the fact that DES are not available for patients covered by SUS, a population that accounts for 80% of the PCIs performed in Brazil41, despite established evidence in the literature that the implantation of new BMS is not the best option for treatment of CISR28-30. Our study provides more evidence to the knowledge of complications that follow stent implantation in our population and can assist in the decisions of health providers regarding the treatment of coronary heart disease.
This study is limited by its observational nature and by the fact that it was conducted in a single center with a small number of patients and events, which explains the wide confidence intervals. Another limitation was the absence of intracoronary ultrasound (ICUS) evaluation in the angiographic analysis of ISR. However, as noted earlier, our results still contribute with knowledge to this area since there is limited information of the clinical course after CISR.
Conclusion
In conclusion, we observed in our cohort that ACS is the main presentation of CISR. Long-term predictors of MACE were clinical treatment of CISR and CISR after DES. Treatment of CISR with implantation of BMS and clinical treatment of CISR were predictors of UA requiring hospitalization and new revascularization. CISR is a major challenge in medical practice, requiring new studies to identify risk predictors and better therapeutic approaches.
Footnotes
Author contributions
Conception and design of the research:Marino BCA, Marino BCA, Ribeiro ALP. Acquisition of data: Marino BCA, Rabelo W. Analysis and interpretation of the data: Marino BCA, Marino BCA, Ribeiro ALP. Statistical analysis: Marino BCA, Ribeiro ALP. Writing of the manuscript: Marino BCA, Ribeiro ALP. Critical revision of the manuscript for intellectual content: Marino BCA, Ribeiro ALP. Angiographic Analysis: Nascimento GA, Marino MA.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
There were no external funding sources for this study.
Study Association
This article is part of the dissertation of master submitted by Bárbara Campos Abreu Marino, from Programa de Pósgraduação da Saúde do Adulto of Faculdade de Medicina da Universidade Federal de Minas Gerais.
References
- 1.Serruys PW, de Jaegere P, Kiemeneji F, Macaya C, Rutsch W, Heyndrickx G, et al. A comparison of baloon-expandable-stent implantation with baloon angioplasty in patients with coronary artery disease. N Engl J Med. 1994;331(8):489–495. doi: 10.1056/NEJM199408253310801. [DOI] [PubMed] [Google Scholar]
- 2.De Labriolle A, Bonello L, Lemesle G, Steinberg DH, Roy P, Xue Z, et al. Clinical presentation and outcome of patients hospitalized for symptomatic in-stent restenosis treated by percutaneous coronary intervention: comparison between drug-eluting stents and bare metal stents. Arch Cardiovasc Dis. 2009;102(3):209–217. doi: 10.1016/j.acvd.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 3.Hoffmann R, Mintz GS, Dussaillant GR, Popma JJ, Pichard AD, Satler LF, et al. Patterns and mechanisms of in-stent restenosis: a serial intravascular ultrasound study group. Circulation. 1996;94(6):1247–1254. doi: 10.1161/01.cir.94.6.1247. [DOI] [PubMed] [Google Scholar]
- 4.Kuntz RE, Baim DS. Defining coronary restenosis: newer clinical and angiographic paradigms. Circulation. 1993;88(3):1310–1323. doi: 10.1161/01.cir.88.3.1310. [DOI] [PubMed] [Google Scholar]
- 5.Fischman DL, Leon MB, Baim DS, Schatz RA, Savage MP, Penn I, et al. A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. Stent Restenosis Study Investigators. N Engl J Med. 1994;331(8):496–501. doi: 10.1056/NEJM199408253310802. [DOI] [PubMed] [Google Scholar]
- 6.Serruys PW, van Hout B, Bonnier H, Legrand V, Garcia E, Macaya C, et al. Randomised comparison of implantation of heparin-coated stents with balloon angioplasty in selected patients with coronary artery disease (Benestent II) Lancet. 1998;352(9129):673–681. doi: 10.1016/s0140-6736(97)11128-x. [DOI] [PubMed] [Google Scholar]
- 7.Bainey KR, Norris CM, Graham MM, Ghali WA, Knudtson ML, Welsh RC, APPROACH investigators Clinical in-stent restenosis with bare metal stents: is it truly a benign phenomenon? Int J Cardiol. 2008;128(3):378–382. doi: 10.1016/j.ijcard.2007.06.024. [DOI] [PubMed] [Google Scholar]
- 8.Cohen DJ, Houser F, Mack M, Simon AW, Battaglia SL, Tarkington LG, et al. Practice and outcomes of percutaneous coronary intervention in the community before drug-eluting stents: a report from the HCA database. J Invasive Cardiol. 2003;15(3):121–127. [PubMed] [Google Scholar]
- 9.Cutlip DE, Chauhan MS, Baim DS, Ho KK, Popma JJ, Carrozza JP, et al. Clinical restenosis after coronary stenting: perspectives from multicenter clinical trials. J Am Coll Cardiol. 2002;40(12):2082–2089. doi: 10.1016/s0735-1097(02)02597-4. [DOI] [PubMed] [Google Scholar]
- 10.Lowe HC, Oesterle SN, Khachigian LM. Coronary in-stent restenosis: current status and future strategies. J Am Coll Cardiol. 2002;39(2):183–193. doi: 10.1016/s0735-1097(01)01742-9. [DOI] [PubMed] [Google Scholar]
- 11.Dangas G, Claessen BE, Caixeta A, Sanidas EA, Mintz G, Mehran R. In-stent restenosis in the drug-eluting stent era. J Am Coll Cardiol. 2010;56(23):1897–1907. doi: 10.1016/j.jacc.2010.07.028. [DOI] [PubMed] [Google Scholar]
- 12.Farooq V, Gogas BD, Serruys PW. Restenosis delineating the numerous causes of drug-eluting stent restenosis. Circ Cardiovasc Interv. 2011;4(2):195–205. doi: 10.1161/CIRCINTERVENTIONS.110.959882. [DOI] [PubMed] [Google Scholar]
- 13.Lemos PA, van Mieghem CA, Arampatzis CA, Hoye A, Ong AT, McFadden E, et al. Post-sirolimus-eluting stent restenosis treated with repeat percutaneous intervention: late angiographic and clinical outcomes. Circulation. 2004;109(21):2500–2502. doi: 10.1161/01.CIR.0000130173.63105.4E. [DOI] [PubMed] [Google Scholar]
- 14.Dawkins KD, Grube E, Guagliumi G, Banning AP, Zmudka K, Colombo A, et al. Clinical efficacy of polymer-based paclitaxel-eluting stents in the treatment of complex, long coronary artery lesions from a multicenter, randomized trial: support for the use of drug-eluting stents in contemporary clinical practice. Circulation. 2005;112(21):3306–3313. doi: 10.1161/CIRCULATIONAHA.105.552190. [DOI] [PubMed] [Google Scholar]
- 15.Pellegrini DO, Gomes VO, Lasevitch R, Smidt L, Azeredo MA, Ledur P, et al. Efficacy and safety of drug-eluting stents in the real world: 8-year follow-up. Arq Bras Cardiol. 2014;103(3):174–182. doi: 10.5935/abc.20140110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen MS, John JM, Chew DP, Lee DS, Ellis SG, Bhatt DL. Bare metal stent restenosis is not a benign entity. Am Heart J. 2006;151(6):1260–1264. doi: 10.1016/j.ahj.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 17.Nayak AK, Kawamura A, Nesto RW, Davis G, Jarbeau J, Pyne CT, et al. Myocardial Infarction as a presentation of clinical in-stent restenosis. Circ J. 2006;70(8):1026–1029. doi: 10.1253/circj.70.1026. [DOI] [PubMed] [Google Scholar]
- 18.Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007;115(17):2344–2351. doi: 10.1161/CIRCULATIONAHA.106.685313. [DOI] [PubMed] [Google Scholar]
- 19.Braunwald E. Unstable angina: a classification. Circulation. 1989;80(2):410–414. doi: 10.1161/01.cir.80.2.410. [DOI] [PubMed] [Google Scholar]
- 20.Mehran R, Dangas G, Abizaid AS, Mintz GS, Lansky AJ, Salter LF, et al. Angiographic patterns of in-stent restenosis: classification and implications for long term outcome. Circulation. 1999;100(18):1872–1878. doi: 10.1161/01.cir.100.18.1872. [DOI] [PubMed] [Google Scholar]
- 21.Chesebro JH, Knatterud G, Roberts R, Borer J, Cohen LS, Dalen J, et al. Thrombolysis in myocardial infarction (TIMI) trial, phase I: a comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge. Circulation. 1987;76(1):142–154. doi: 10.1161/01.cir.76.1.142. [DOI] [PubMed] [Google Scholar]
- 22.Assali AR, Moustapha A, Sdringola S, Denktas AE, Willerson JT, Holmes DR, Jr, et al. Acute coronary syndrome may occur with in-stent restenosis and is associated with adverses outcomes (the PRESTO trial) Am J Cardiol. 2006;98(6):729–733. doi: 10.1016/j.amjcard.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 23.Ogita M, Miyauchi K, Kurata T, Yokoyama K, Dohi T, Tuboi S, et al. Clinical impact of angiographic restenosis after bare-metal stent implantation on long-term outcomes in patients with coronary artery disease. Circ J. 2011;75(11):2566–2572. doi: 10.1253/circj.cj-11-0469. [DOI] [PubMed] [Google Scholar]
- 24.Garg S, Serruys PW. Coronary stents-current status. J Am Coll Cardiol. 2010;56(10):S1–42. doi: 10.1016/j.jacc.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 25.Rittger H, Brachmann J, Sinha AM, Waliszewski M, Ohlow M, Brugger A, et al. A randomized, multicenter, single-blinded trial comparing paclitaxel-coated balloon angioplasty with plain balloon angioplasty in drug-eluting stent restenosis: the PEPCAD-DES study. J Am Coll Cardiol. 2012;59(15):1377–1382. doi: 10.1016/j.jacc.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 26.Latib A, Mussardo M, Lelasi A, Tarsia G, Godino C, Al-Lamee R, et al. Long-term outcomes after the percutaneous treatment of drug-eluting stent restenosis. JACC Cardiovasc Interv. 2011;4(2):155–164. doi: 10.1016/j.jcin.2010.09.027. [DOI] [PubMed] [Google Scholar]
- 27.Steinberg DH, Gaglia MA, Slottow TL, Roy P, Bonello L, de Labriolle A, et al. Outcome differences with the use of drug-eluting stents for the treatment of in-stent restenosis of bare-metal stents versus drug-eluting stents. Am J Cardiol. 2009;103(4):491–495. doi: 10.1016/j.amjcard.2008.09.107. [DOI] [PubMed] [Google Scholar]
- 28.Mattos LA, Lemos PA, Neto, Rassi A Jr, Marin-Neto JA, Sousa AG, Devito FS, et al. Diretrizes da Sociedade Brasileira De Cardiologia - Intervenção coronária percutânea e métodos adjuntos diagnósticos em cardiologia intervencionista (II Edição - 2008) Arq Bras Cardiol. 2008;91(6) supl.1:1–58. [Google Scholar]
- 29.Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011;124(23):e574–e651. doi: 10.1161/CIR.0b013e31823ba622. [DOI] [PubMed] [Google Scholar]
- 30.Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Folliguet T, et al. Task Force on Myocardial Revascularization of the European Society of Cardiology and the European Association for Cardio-Thoracic Surgery Guidelines on myocardial revascularization. Eur Heart J. 2010;31(20):2501–2555. [Google Scholar]
- 31.Douglas JS., Jr Drug-eluting stent restenosis: a need for new technology? JACC Cardiovasc Interv. 2012;5(7):738–740. doi: 10.1016/j.jcin.2012.03.019. [DOI] [PubMed] [Google Scholar]
- 32.Stefanini GG, Holmes DR. Drug-eluting coronary-artery stents. N Engl J Med. 2013;368(3):254–265. doi: 10.1056/NEJMra1210816. [DOI] [PubMed] [Google Scholar]
- 33.Whan Lee C, Kim SH, Suh J, Park DW, Lee SH, Kim YH, et al. Long-term clinical outcomes after sirolimus-eluting stent implantation for treatment of restenosis within bare-metal versus drug-eluting stents. Catheter Cardiovasc Interv. 2008;71(5):594–598. doi: 10.1002/ccd.21399. [DOI] [PubMed] [Google Scholar]
- 34.Kastrati A, Byrne R. New roads, new ruts: lessons from drug-eluting stent restenosis. JACC Cardiovasc Interv. 2011;4(2):165–167. doi: 10.1016/j.jcin.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 35.Ishikawa K, Aoyama Y, Hirayama H. Management of drug-eluting stent restenosis. J Invasive Cardiol. 2012;24(4):178–182. [PubMed] [Google Scholar]
- 36.Park SJ, Kang SJ, Virmani R, Nakano M, Ueda Y. In-stent neoatherosclerosis: a final common pathway of late stent failure. J Am Coll Cardiol. 2012;59(23):2051–2057. doi: 10.1016/j.jacc.2011.10.909. [DOI] [PubMed] [Google Scholar]
- 37.Kilic ID, Konstantinidis N, Pighi M, Mattesini A, Di Mario C. Stop adding metal layers: will bioabsorbable scaffolds become the gold standard for late in-stent restenosis and neo-atherosclerosis? Cardiovasc Revasc Med. 2014 Jul 31; doi: 10.1016/j.carrev.2014.07.003. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 38.Gottschall CA, Sarmento-Leite R, Welter D, de Quadros AS. Resultados clínicos de pacientes com reestenose intrastent não tratada com novo procedimento de revascularização. Rev Bras Cardiol Invasiva. 2010;18(4):419–423. [Google Scholar]
- 39.van Miltenburg-van Zijl AJ, Simoons ML, Veerhoek RJ, Bossuyt PM. Incidence and follow-up of Braunwald subgroups in unstable angina pectoris. J Am Coll Cardiol. 1995;25(6):1286–1292. doi: 10.1016/0735-1097(95)00009-S. [DOI] [PubMed] [Google Scholar]
- 40.Rizik DG, Healy S, Margulis A, Vandam D, Bakalyar D, Timmis G, et al. A new clinical classification for hospital prognosis of unstable angina pectoris. Am J Cardiol. 1995;75(15):993–997. doi: 10.1016/s0002-9149(99)80710-3. [DOI] [PubMed] [Google Scholar]
- 41.Piegas LS, Haddad N. Intervenção coronariana percutânea no Brasil: resultados do Sistema Único de Saúde. Arq Bras Cardiol. 2011;96(4):317–324. doi: 10.1590/s0066-782x2011005000035. [DOI] [PubMed] [Google Scholar]