Abstract
Introduction:
Many healthy elderly Indian men seek surgical treatment for localized prostate cancer. Quite often, radical surgery is not offered to the patients over 70 years of age due to the perception of increased side-effects and complications. We have previously reported our results of robotic radical prostatectomy in a study comprising 150 Indian patients, where almost a quarter of patients were elderly. This subgroup analysis was therefore focused on evaluating perioperative and continence outcomes in elderly men (≥70 years) with localized prostate cancer.
Materials and Methods:
Between April 2010 and August 2013, 153 men had robot-assisted radical prostatectomy performed by two surgeons. Of the 150 men analyzed, 39 (26%) were aged ≥70 years. All patients underwent robotic prostatectomy using a 4 arm da Vinci surgical system. Pre-operative, intraoperative and post-operative parameters were studied. Check cystogram was performed in all patients prior to catheter removal. Complications were categorized using the Clavien-Dindo classification system. Continence was defined as use of “no pad” or security liner only. All data were recorded prospectively and analyzed using SPSS version 20.
Results:
There were no significant intraoperative or perioperative complications in this group. Median blood loss during surgery was 150 mL. None of the patient required blood transfusion. There were two minor complications (5.1%) within the first 30 days of surgery: Minimal anastomotic site leak (one patient) requiring replacement and prolongation of Foley's drainage by 1 week and ileus (one patient). No patient had any cardiopulmonary or vascular complications in the post-operative period. The median duration of hospital stay was 3 days. The median duration of catheterization was 7 days. No patient had problem of bladder neck stenosis in the follow-up period. At 1 month, 3 months, 6 months and 1 year of follow-up, 66.7% (n = 26), 74.3% (n = 29), 87.9% (n = 34) and 94.8% (n = 37), respectively, were continent.
Conclusions:
Robotic surgery is safe and feasible in a select group of elderly patients. It has acceptable and minimal perioperative complications along with good continence outcome.
Keywords: Continence, elderly men, prostate cancer, robotic prostatectomy, robotic surgery
INTRODUCTION
Robot-assisted radical prostatectomy (RARP) as a means of treating clinically localized prostate cancer has been widely accepted.[1,2] RARP is recommended and usually offered to patients with more than 10 years of life-expectancy. The upper age limit for radical prostatectomy (RP) is not clearly defined; however, many surgeons shy away from offering radical surgery to patients older than 70 years.[3] As the population continues to age, limits that hitherto have guided decision making for managing prostate cancer are continuously being questioned.[4] It is expected that the elderly population will continue to increase considering changes in lifestyle and advancement in medicine. Thus, more elderly patients with longer life-expectancy and otherwise enjoying good health will be presenting with localized prostate cancer.[5,6] The situation in India is no different. More and more healthy Indian elderly men are seeking surgical treatment over hormonal or radiation therapy for prostate cancer disease. It seems many surgeons do not offer RP to patients over 70 years of age due to the perception of increased side-effects and complications in the elderly. We have previously reported our results of robotic radical prostatectomy in a study comprising 150 Indian patients, where almost a quarter of patients were elderly.[7] This subgroup analysis of the study was therefore focused on evaluating the perioperative and continence outcomes in elderly men (≥70 years) with localized prostate cancer who were found suitable for RARP and who chose to undergo surgery over radiotherapy or hormonal therapy.
MATERIALS AND METHODS
From April 2010 to August 2013, 153 patients underwent RARP by two surgeons at our institution. Three patients were excluded from the analysis due to poor follow-up information. Study details and continence outcomes of the complete cohort has been published earlier.[7] This study is the subgroup analysis of thirty-nine elderly patients (26%) (defined as being ≥70 years of age). Clinical staging included serum prostate-specific antigen (PSA), digital rectal examination, bone scan and magnetic resonance imaging of the abdomen and pelvis in most cases. Comorbidity was assessed using the age-adjusted Charlson Comorbidity Index scoring system. Risk categorization was performed using the D’ Amico Risk Criterion. All the patients underwent transperitoneal prostatectomy using a four-arm daVinci Si system (Intuitive Surgical, Sunnyvale, CA, USA). Extended template lymph node dissection was performed in high-risk cases while “Standard template” node dissection was performed in the remainder of the patients. Perioperative factors analyzed included total operating room time, estimated blood loss, blood transfusion rate and length of hospital stay and duration of catheterization. Complications were categorized using the Clavien-Dindo classification system.
Histopathologic evaluation
All surgical specimens were weighed and external surfaces were inked before processing. The apex and bladder neck cones were amputated and sectioned in the saggital plane. The remaining specimen was sectioned transversely at 4-mm intervals. Pathologic factors analyzed included prostate weight, histology, pathologic stage, Gleason grade and margin status. Positive surgical margins (PSMs) were defined as the presence of tumor on the inked surface of the specimen. Histopathologic staging was performed according to the 2002 TNM system.
Perioperative care
All patients were evaluated by the physician and cardiologists for assessment and pre-operative optimization. All patients were started on incentive spirometry at least 1 day prior to surgery. Two 5 mg tablets of Bisacodyl were given on the evening before surgery and phosphate enema was given on the morning of surgery. Venous compression pumps were used during the surgery. No deep vein thrombosis prophylaxis was given as a routine. Patients were mobilized on the evening of surgery and started on oral liquids. Drain removal was performed after the patient was mobilized well and the output was serous and <100 mL/24 h. Patients were discharged on catheter once they had a bowel movement and started taking a soft diet.
Catheter removal and follow-up
Catheter removal is performed on an outpatient basis after a check cystogram (to look for anastomotic leak). This is done on post-operative Day 7 in most of the patients. In case of any significant anastomotic leak on check cystogram, catheter replacement is performed for another week.
Post-operative follow-up comprised a clinical examination and PSA levels at 6 weeks, at 3, 6, 9 and 12 months and then every 6 months thereafter. Continence status was defined as use of either “no pad” or just a security liner. Continence rate was assessed with the self-administered questionnaire during visits in the outpatient department or by e-mail/postal mail at 6 weeks and at 3, 6, 9, 12, 18 and 24 months.
All patients’ data were prospectively recorded in the hospital database. Statistical analysis was performed using SPSS (version 20, SPSS Inc., Chicago, IL, USA). Continuous parameteric variables were reported as the mean plus or minus standard deviations (SD) or as the median values and interquartile range (IQR). Mann–Whitney and Chi-square tests were used to compare continuous and categorical variables as appropriate.
RESULTS
Of the 150 men who were evaluated during the study period, 39 (26%) were elderly. In the study group, a minimal follow-up of 10 months was available in all patients, while 37/39 patients had more than 1 year of follow-up. Baseline clinical and pre-operative pathologic characteristics of the elderly patients are summarized in Table 1. Only four patients (10.5%) had clinical features of low risk according to the D’Amico's Risk Classification. Perioperative and pathologic characteristics as well as treatment outcomes are detailed in Table 2. The median operative time was 170 min (IQR 130–210). The median blood loss during surgery was 150 mL. None of the patients required blood transfusion. All the patients were mobilized and started on oral liquids on the evening of surgery. No patient had any cardiopulmonary or vascular complications (i.e. deep venous thrombosis or pulmonary embolism) in the post-operative period. There were two minor complications (5.1%) within the first 30 days of surgery: Minimal anastomotic site leak (one patient) requiring replacement and prolongation of Foley's drainage by 1 week and ileus (one patient). The median duration of hospital stay was 3 days. The median duration of catheterization was 7 days. No patient had a problem of bladder neck stenosis in the follow-up.
Table 1.
Clinical and pre-operative pathologic characteristics of elderly patients (≥70 years) undergoing RARP
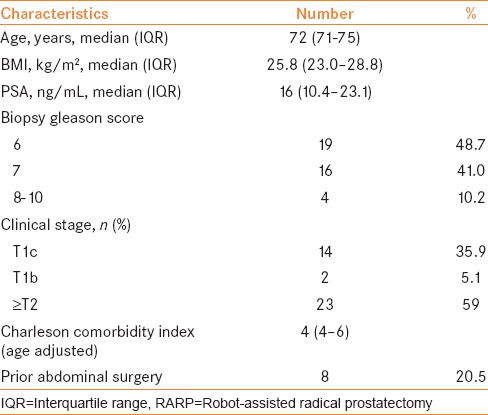
Table 2.
Perioperative parameters, pathologic characteristic and treatment outcomes of elderly (≥70 years) patients
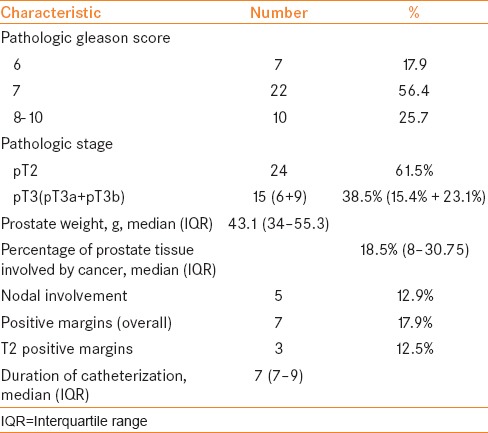
On final pathology, 20 men (51.28%) had organ-confined disease with negative surgical margin, three men had organ-confined disease with positive surgical margins (12.5%) while one patient had pathological pT2N1 disease. A total of 12 patients (30.76%) had extraprostatic disease with negative surgical margins. Five patients (12.8%) had positive lymph nodes on microscopic examination. One of the patients with positive node had pathologically T2 disease with Gleason (4 + 3) while the rest of the four patients with positive node had pT3 with Gleason ≥8. Four of five patients with positive nodal status had negative surgical margins.
Recovery of continence
7.9% (n = 3) of the patients were continent within 1 week after catheter removal [Figure 1]. 66.7% (n = 26) of the patients regained their continence after 4 weeks of surgery. At 3 months, 6 months and 1 year of follow-up, 74.3% (n = 29), 87.9% (n = 34) and 94.8% (n = 37), respectively, of the patients were continent. Comparative figures of continent status in the rest of the group (patients <70 years of age) were 17.6% at 1 week, 53.3% at 4 weeks, 79.4% at 3 months, 91.4% at 6 months and 93.6% at 1 year of follow-up.
Figure 1.
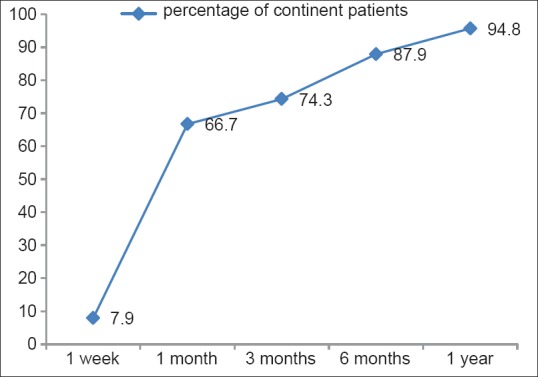
Graph showing percentage of patients in the group ≥70 years of age who achieved continence during follow-up
DISCUSSION
Prostate cancer is a disease of the elderly. With improving average life expectancy in India, more and more elderly Indian men are expected to seek treatment in the near future. According to a recent cancer registry, prostate cancer is the second most common cancer diagnosed in men in India, with a rising mean annual percentage change of 0.14–8.6.[8] Many such elderly men will be found suitable for RP based upon their disease profile, fitness status and life expectancy. Although RARP is increasingly being used in the surgical management of clinically localized prostate cancer in Indian patients, the use of RARP in the elderly population in India has not been described. In our series, approximately 26% (39/150) of the patients was ≥70 years. We found that with appropriate case selection and pre-operative preparation, there is minimal perioperative morbidity of the procedure even in men ≥70 years of age. None of our patients required blood transfusion, and majority of the patients were sent home on post-operative Day 3 (after bowel movement and starting them on a soft diet). Other than the minimally invasive surgical approach, the preventive steps in the form of incentive spirometery and early mobilization also probably helped us in avoiding many dreaded cardiorespiratory and vascular complications in the elderly. The recovery pattern in all the elderly patients was similar to that seen in younger individuals. Only two patients (5.1%) had minor complications in the perioperative period. None of the patients developed bladder neck stenosis.
Several previous reports have shown feasibility of RP in elderly patients and a comparable oncologic outcome of RP in elderly and younger men.[9,10,11] Other than perioperative morbidity of undergoing a major surgical procedure, one of the important considerations specific to this surgery that affects the quality of life is “urinary control.” In concordance to others, we have found a slight delay in recovery of urinary control in elderly compared with younger men.[12] In our patients, continence rates were lower in older men (7.9% in elderly vs. 17.6% in younger men) in the first week, but returned to levels equivalent to those of younger men at 4 weeks (59.5% vs. 53.3%), 3 months (74.3% vs. 79.4%), 6 months (87.9% vs. 91.4%) and 1 year of follow-up (94.8% vs. 93.6%). Difference in tissue resiliency of elderly men compared with younger men has been postulated as a possible reason for delayed recovery. Similar findings have also been reported from open RP data, showing that age is a risk factor for incontinence in men after RP.[13] Patients aged ≥70 years should therefore be counseled that there might be a delay in return to full incontinence compared with younger men.
Although we have not performed Quality of life (QoL) score assessment, other authors have found that a delay in achieving urine control affects the recovery of general QoL parameters dramatically and independent of the pathologic stage.[12,14]
In the present study, clinical and pathologic parameters suggest that men aged ≥70 years had more aggressive tumors at the time of surgery compared with younger men. Only four patients (10.5%) had clinical features of low risk according to the D’Amico's Risk Classification. The remaining patients were either intermediate or high risk (compared with 28.2% of low risk in the group <70 years; P value = 0.08). More than 80% of our elderly group patients had a Gleason score of 7 or more (with approximately 25% with Gleason 8–10). A higher pathological stage and higher Gleason scores among elderly men, suggesting a biologically more aggressive form of cancer, has been reported previously as well.[11,12,15,16,17] Poulakis et al. in their series reported that patients aged 71 years and older had prostate cancer with significantly higher clinical and pathologic stage, higher PSA and Gleason scores.[12] Thus, logically, elderly men with clinically localized disease and without significant comorbidities are likely to have morbidity and mortality from their prostate cancer if they are not treated aggressively. Therefore, surgical treatment of prostate cancer with curative intent should not be denied on the basis of age alone.
Our study has several limitations. First, this is a single-center, non-randomized study with a relatively small sample size. Second, there is an obvious selection bias because all the elderly patients who were offered the surgical treatment had acceptable comorbidity and enjoyed good health. Thus, the elderly patients in the study might not reflect the average patient of their same age. Third, the QoL assessment has not been performed in this study thus missing the opportunity to describe what percentage of patients achieves the baseline QoL score and how long after surgery. Also, it would have been ideal if the assessment of continence status was performed in a more objective manner like “pad weight.”
CONCLUSIONS
The perioperative and continence outcomes of RARP in elderly men are largely comparable to those in younger men, with the exception of transient delay in return of continence. Thus, chronological age should not be a contraindication for RARP in clinically localized prostate cancer.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Montorsi F, Wilson TG, Rosen RC, Ahlering TE, Artibani W, Carroll PR, et al. Best practices in robot-assisted radical prostatectomy: Recommendations of the Pasadena Consensus Panel. Eur Urol. 2012;62:368–81. doi: 10.1016/j.eururo.2012.05.057. [DOI] [PubMed] [Google Scholar]
- 2.Hakimi AA, Feder M, Ghavamian R. Minimally invasive approaches to prostate cancer: A review of the current literature. Urol J Summer. 2007;4:130–7. [PubMed] [Google Scholar]
- 3.Lepor H. Selecting candidates for radical prostatectomy. Rev Urol Summer. 2000;2:182–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Thompson RH, Slezak JM, Webster WS, Lieber MM. Radical prostatectomy for octogenarians: How old is too old? Urology. 2006;68:1042–5. doi: 10.1016/j.urology.2006.05.031. [DOI] [PubMed] [Google Scholar]
- 5.Mandhani A. Early prostate cancer: Radical prostatectomy or watchful waiting. Natl Med J India. 2005;18:195–6. [PubMed] [Google Scholar]
- 6.Lalitha K, Suman G, Pruthvish S, Mathew A, Murthy NS. Estimation of time trends of incidence of prostate cancer--an Indian scenario. Asian Pac J Cancer Prev. 2012;13:6245–50. doi: 10.7314/apjcp.2012.13.12.6245. [DOI] [PubMed] [Google Scholar]
- 7.Gupta NP, Yadav R, Akpo EE. Continence outcomes following robotic radical prostatectomy: Our experience from 150 consecutive patients. Indian J Urol. 2014;30:374–7. doi: 10.4103/0970-1591.139575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.New Delhi: All India Institute of Medical Sciences; 2010. Cancer incidence and mortality in Delhi UT urban, 2006. Delhi cancer registry. Dr B. R. Ambedkar Institute of Rotary Cancer Hospital; p. 8. [Google Scholar]
- 9.Magheli A, Rais-Bahrami S, Humphreys EB, Peck HJ, Trock BJ, Gonzalgo ML. Impact of patient age on biochemical recurrence rates following radical prostatectomy. J Urol. 2007;178:1933–7. doi: 10.1016/j.juro.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 10.Malaeb BS, Rashid HH, Lotan Y, Khoddami SM, Shariat SF, Sagalowsky AI, et al. Prostate cancer disease-free survival after radical retropubic prostatectomy in patients older than 70 years compared to younger cohorts. Urol Oncol. 2007;25:291–7. doi: 10.1016/j.urolonc.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 11.Siddiqui SA, Sengupta S, Slezak JM, Bergstralh EJ, Leibovich BC, Myers RP, et al. Impact of patient age at treatment on outcome following radical retropubic prostatectomy for prostate cancer. J Urol. 2006;175:952–7. doi: 10.1016/S0022-5347(05)00339-3. [DOI] [PubMed] [Google Scholar]
- 12.Poulakis V, Witzsch U, de Vries R, Dillenburg W, Becht E. Laparoscopic radical prostatectomy in men older than 70 years of age with localized prostate cancer: Comparison of morbidity, reconvalescence, and short-term clinical outcomes between younger and older men. Eur Urol. 2007;51:1341–8. doi: 10.1016/j.eururo.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 13.Eastham JA, Kattan MW, Rogers E, Goad JR, Ohori M, Boone TB, et al. Risk factors for urinary incontinence after radical prostatectomy. J Urol. 1996;156:1707–13. [PubMed] [Google Scholar]
- 14.Kerr LA, Zincke H. Radical retropubic prostatectomy for prostate cancer in the elderly and the young: Complications and prognosis. Eur Urol. 1994;25:305–11. doi: 10.1159/000475307. [DOI] [PubMed] [Google Scholar]
- 15.Alexander RB, Maguire MG, Epstein JI, Walsh PC. Pathological stage is higher in older men with clinical stage B1 adenocarcinoma of the prostate. J Urol. 1989;141:880–2. doi: 10.1016/s0022-5347(17)41038-x. [DOI] [PubMed] [Google Scholar]
- 16.Nadler RB, Loeb S, Roehl KA, Antenor JA, Eggener S, Catalona WJ. Use of 2.6 ng/ml prostate specific antigen prompt for biopsy in men older than 60 years. J Urol. 2005;174:2154–7. doi: 10.1097/01.ju.0000181213.07447.8f. [DOI] [PubMed] [Google Scholar]
- 17.Jani AB, Johnstone PA, Liauw SL, Master VA, Brawley OW. Age and grade trends in prostate cancer (1974-2003): A Surveillance, Epidemiology, and End Results Registry analysis. Am J Clin Oncol. 2008;31:375–8. doi: 10.1097/COC.0b013e3181637384. [DOI] [PubMed] [Google Scholar]


