Abstract
Aims
The aim of this pilot study was to generate an initial estimate of the prevalence and correlates of diabetic retinopathy in a racially and ethnically diverse sample of youth with Type 1 and Type 2 diabetes mellitus.
Methods
A pilot study was conducted among 222 individuals with Type 1 diabetes (79% non-Hispanic white, 21% other) and 43 with Type 2 diabetes (28% non-Hispanic white, 72% other), all of > 5 years duration (mean duration 6.8 years) who participated in the SEARCH for Diabetes in Youth study. Diabetic retinopathy was assessed using non-mydriatic retinal photography of both eyes.
Results
The prevalence of diabetic retinopathy was 17% for Type 1 diabetes and 42% for Type 2 diabetes (odds ratio 1.50, 95% CI 0.58–3.88; P = 0.40 adjusted for age, duration, gender, race/ethnicity, parental education and HbA1c. HbA1c was significantly higher among those with any diabetic retinopathy (adjusted mean 79 mmol/mol, 9.4%) vs. no diabetic retinopathy (adjusted mean 70 mmol/mol, 8.6%) (P = 0.015). LDL cholesterol was also significantly higher among those with any diabetic retinopathy (adjusted mean 107.2 mg/dl) compared with those without diabetic retinopathy (adjusted mean 97.9 mg/dl) (P = 0.04).
Conclusions
The prevalence of diabetic retinopathy in contemporary young individuals was substantial, particularly among minority youth and those with Type 2 diabetes. Further long-term study of diabetic retinopathy in youth is needed.
Keywords: childhood diabetes, diabetes complications, epidemiology, retinopathy
Introduction
Data on the epidemiology of diabetic retinopathy in youth with diabetes are limited. Estimates of the prevalence of diabetic retinopathy among individuals with Type 1 diabetes vary from 4.6% among youth in France (mean duration 4.8 years) [1] to 20% among youth from Australia (mean duration 6.8 years) [2]. Interestingly, the prevalence of diabetic retinopathy among Australian youth with Type 1 diabetes declined signifcantly over three time periods (1990–1994, 1995–1998 and 1999–2002) from 49% in the first time period to 31% in the second time period, and 24% in the third time period [3]. A recent study from Finland reported prevalence of diabetic retinopathy of 12% among youth with Type 1 diabetes (mean duration 4.9 years), with no decrease in prevalence over a 17-year period [4]. Therefore, it is important to determine the prevalance of diabetic retinopathy in a contemporary cohort of youth with Type 1 diabetes.
For youth with Type 2 diabetes, the published literature is very limited, with only one small study identified: in the Australian cohort, prevalence was 4% (n = 25, mean duration 1.3 years) [2]. It is also important to consider potential differences in prevalence according to race/ethnicity. From the most recent national estimate of prevalence of diabetic retinopathy among adults with diabetes in the USA [5], non-Hispanic white individuals had a crude prevalence of 26%; compared with 39 and 34% for non-Hispanic black and Hispanic individuals, respectively.
The SEARCH for Diabetes in Youth study comprises the largest contemporary cohort of youth with diabetes studied in the USA, with substantial racial and ethnic diversity. Here, we report findings from a pilot study of the prevalence and correlates of diabetic retinopathy in youth with either Type 1 or Type 2 diabetes who participated in SEARCH.
Subjects and methods
SEARCH includes individuals diagnosed with diabetes before the age of 20 years from six centres, whose diabetes was prevalent in 2001 or incident thereafter. Study methods [6] and the study cohort have been described [7]. Briefly, following medical record-based validation of the diabetes diagnosis and study eligibility, youth with diabetes or their parent/guardians were asked to complete a short initial survey that collected information on race and ethnicity, and diabetes-related factors. Self-reported race and ethnicity were collected using the 2000 US Census questions [8]. All youths who replied to the initial survey, excluding those whose diabetes was secondary to other conditions, were invited to a study visit during which questionnaires were administered, a brief physical examination was conducted and biological specimens were collected. Specific laboratory methods for these tests have been previously described [9,10]. All measures were conducted under standardized protocols by centrally trained and certified research staff. Youths with diabetes incident in 2002–2005 were invited to the baseline examination, plus up to three follow-up visits scheduled up to 60 months after baseline.
A pilot study to assess diabetic retinopathy prevalence and correlates was conducted from December 2009 to September 2010 to inform plans for the SEARCH Cohort Study, which will commence in 2011. A convenience sample of incident cases (2002–2005) with ≥ 5 years of diabetes duration who were attending a SEARCH 60-month follow-up visit during the diabetic retinopathy pilot study time period were eligible. Diabetes duration and HbA1c did not differ between individuals who participated in the diabetic retinopathy pilot and those who attended a 60-month follow-up visit but who, primarily because of being outside the calendar time allotted for the diabetic retinopathy pilot, did not participate (P > 0.5 for both). Diabetic retinopathy was determined by grading 45° colour digital fundus images centred on the disc and macula of both eyes taken using a non-mydriatic camera (Visucam Pro N; Carl Zeiss Meditech, Jena, Germany) under a standardized protocol. The University of Wisconsin Ocular Epidemiology Reading Center (RK) was responsible for conduct of centralized training and certification of study staff, quality control of retinal photos and reading of the photos for diabetic retinopathy presence and severity. Diabetic retinopathy severity was based on the worse eye and categorized as none, minimal non-proliferative diabetic retinopathy, mild–moderate nonproliferative diabetic retinopathy to proliferative [11]. Institutional review board(s) for each of the centres approved the study protocol.
Generalized linear models and logistic regression were used to evaluate correlates of diabetic retinopathy and adjust for diabetes type, race/ethnicity, duration, HbA1c, gender, age and parental education; with statistical significance established at P < 0.05.
Results
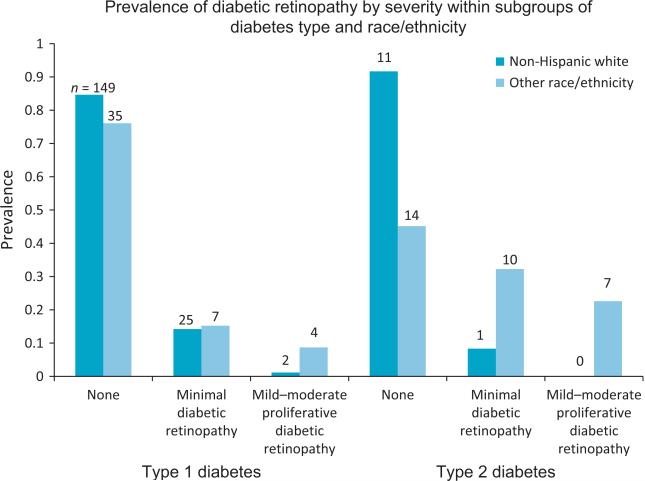
Participants included 222 individuals with physician-diagnosed Type 1 diabetes (176 non-Hispanic white, 46 other race/ethnicity) and 43 with Type 2 diabetes (12 non-Hispanic white, 31 other race/ethnicity) (Table 1). Figure 1 shows prevalence of diabetic retinopathy by severity within subgroups of diabetes type and race/ethnicity. The prevalence of any diabetic retinopathy was 42% for those with Type 2 diabetes [mean age 21.1 years (sd 2.8); mean time since diagnosis 7.2 years (sd 0.93)] compared with 17% for Type 1 diabetes [mean age 16.0 years (sd 4.4); mean time since diagnosis 6.8 years (sd 0.97)]. For both Type 1 and Type 2 diabetes, crude prevalence of both minimal diabetic retinopathy and mild-to-proliferative diabetic retinopathy was lower among non-Hispanic white indiviudals compared with those of other race/ethnicities.
Table 1.
Overall generalized linear model results for youth with Type 1 (n =222) and Type 2 diabetes (n = 43)*
| Potential risk factor† | Odds ratio (95% CI) | P-value | |
|---|---|---|---|
| Diabetes type (Type 2 vs. Type 1) | 1.50 (0.58-3.88) | 0.40 | |
| Race/ethnicity (Non-white vs. non-Hispanic white) | 2.05 (0.97-4.33) | 0.06 | |
| No diabetic retinopathy | Diabetic retinopathy, any severity | P-value | |
| Duration (years) | 6.9 | 7.1 | 0.25 |
| HbA1c | 70 mmol/mol | 79 mmol/mol | 0.015 |
| 8.6% | 9.4% | ||
| Systolic blood pressure (mmHg) | 106.3 | 107.1 | 0.66 |
| Diastolic blood pressure (mmHg) | 65.0 | 67.4 | 0.13 |
| Log albumin-to-creatinine ratio | 2.1 | 2.3 | 0.31 |
| BMI | 25.2 | 26.1 | 0.23 |
| Height (m) | 1.47 | 1.48 | 0.88 |
| NHANES waist circumference (cm) | 86.9 | 89.2 | 0.32 |
| Total cholesterol (mg/dl) | 170.0 | 180.0 | 0.10 |
| LDL cholesterol (mg/dl) | 97.9 | 107.2 | 0.04 |
| HDL cholesterol (mg/dl) | 49.3 | 48.4 | 0.71 |
| Log triglycerides | 4.5 | 4.6 | 0.22 |
Numbers vary slightly because of occasional missing data.
Adjusted for diabetes type, race/ethnicity, diabetes duration, HbA1c, gender, age and parental education.
FIGURE 1.
Prevalence and severity of diabetic retinopathy among participants in the SEARCH for Diabetes in Youth diabetic retinopathy pilot study: n = 222 with Type 1 diabetes and n = 43 with Type 2 diabetes. For proliferative diabetic retinopathy: n = 0 for Type 1 diabetes; n = 1 for Type 2 diabetes.
Because of small numbers in some cells, all subsequent analyses to adjust for potential confounding compare ‘any diabetic retinopathy’ vs. ‘no diabetic retinopathy’. Shown in Table 1, the difference in prevalence of diabetic retinopathy by diabetes type was not statistically significant (odds ratio 1.50, 95% CI 0.58–3.88; P = 0.40). The observed higher prevalence of diabetic retinopathy among minority youth was not fully explained by differences in HbA1c or other potential confounders, including duration of disease (odds ratio 2.05, 95% CI 0.97–4.33); however, the criteria for statistical significance was not satisfied (P = 0.06). HbA1c was significantly higher among those with any diabetic retinopathy (adjusted mean 79 mmol/mol, 9.4%) vs. no diabetic retinopathy (adjusted mean 70 mmol/mol, 8.6%) (P = 0.015). LDL cholesterol was significantly higher among those with any diabetic retinopathy (adjusted mean 107.2 mg/dl) than those without diabetic retinopathy (adjusted mean 97.9 mg/dl) (P = 0.04).
Discussion
From this pilot study, the estimate of prevalence of diabetic retinopathy among those with Type 1 diabetes (17%) was similar to that reported from Australia [2] from a cohort of similar duration. For those with Type 2 diabetes, we report a high prevalence of diabetic retinopathy (42%), which was surprising and may reflect high risk for diabetic retinopathy in population subgroups. Most (72%) of the SEARCH participants with Type 2 diabetes in the present study were of minority race/ethnicity and, from previous studies that also used retinal photography, high prevalence of diabetic retinopathy can be detected in non-Caucasian populations such as Pima Indians [12] or individuals with Type 2 diabetes from the island of Mauritius [13]. Of note, for the combined group of Type 1 and Type 2 diabetes, the higher prevalence of diabetic retinopathy among minority youth was not fully explained by differences in HbA1c or other potential confounders, including duration of disease. Interestingly, in Japan, individuals with early onset of Type 2 diabetes (< 30 years) appeared to have higher incidence of diabetic retinopathy, and greater risk for progression from background diabetic retinopathy to proliferative diabetic retinopathy [14], as well as higher incidence of diabetic nephropathy compared with individuals with Type 1 diabetes [15]. Thus, in the USA, minority youth who develop Type 2 diabetes relatively early in life may be particularly vulnerable to development of the microvascular complications of diabetes.
Regarding associations of diabetic retinopathy with clinical variables, findings across studies are mixed [16,17] and further research is needed. From the Australian cohort, higher systolic and diastolic blood pressures were associated with development of background retinopathy, after adjustment for albumin excretion rate, HbA1c, duration of diabetes, age and height [16]. Cheung et al. [17] reported that, among young individuals with Type 1 diabetes, longer duration of diabetes, lower BMI and higher HbA1c were significantly associated with incidence of diabetic retinopathy, as was larger retinal arteriolar caliber; however, differences in mean arterial blood pressure, gender and albumin excretion rate did not significantly predict diabetic retinopathy. In the present study, higher HbA1c and higher LDL cholesterol concentrations were the strongest correlates of diabetic retinopathy, independent of diabetes type and other covariates.
This pilot study suggests that, despite advances in diabetes care, diabetic retinopathy remains an important concern both in terms of research and clinical care. The present results are preliminary, as is the nature of pilot studies. Motivated by these findings, the SEARCH Cohort Study will assess diabetic retinopathy in an estimated 3000 individuals with Type 1 or Type 2 diabetes who have previously participated in at least one SEARCH visit, inclusive of diverse race/ethnicities. Such studies will be critically important to advance our knowledge of the burden and correlates of diabetic retinopathy among youth, particularly those with Type 2 diabetes and those of minority race/ethnicity, and will provide much-needed evidence for the development of screening guidelines in contemporary youth with diabetes.
Acknowledgements
The SEARCH for Diabetes in Youth Study is indebted to the many youth and their families, and their healthcare providers, whose participation made this study possible. The SEARCH for Diabetes in Youth is funded by the Centers for Disease Control and Prevention (PA number 00097, DP-05-069 and DP-10-001) and supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Site contract numbers are Kaiser Permanente Southern California (U01 DP000246), University of Colorado Denver (U01 DP000247), Kuakini Medical Center (U01 DP000245), Children's Hospital Medical Center (Cincinnati) (U01 DP000248), University of North Carolina at Chapel Hill (U01 DP000254), University of Washington School of Medicine (U01 DP000244), Wake Forest University School of Medicine (U01 DP000250). The authors wish to acknowledge the involvement of General Clinical Research Centers (GCRC) at the Medical University of South Carolina (grant no. M01 RR01070); Seattle Children's and the University of Washington School of Medicine (grant nos M01RR00037 and M01RR001271); Colorado Pediatric General Clinical Research Center (grant no. M01 RR00069); and the Institutional Clinical and Translational Science Award (CTSA), NIH/NCRR at the University of Cincinnati (grant no. 1UL1RR026314-01).
Footnotes
Competing interests
Nothing to declare.
Previous publication
Mayer-Davis EJ, Klein R, Klein BE, Davis C, Saadine J, D'Agostino Jr R, Bell RA, Dabelea D, Dolan L, Garg S, Lawrence JM, Linder B, Marcovina SM, Pihoker C, Rodriguez BL. Diabetic retinopathy in the SEARCH for Diabetes in Youth Cohort: a pilot study. Diabetes 2011; 60: A182
References
- 1.Massin P, Erginay A, Mercat-Caudal I, Vol S, Robert N, Reach G, et al. Prevalence of diabetic retinopathy in children and adolescents with type 1 diabetes attending summer camps in France. Diabetes Metab. 2007;33:284–289. doi: 10.1016/j.diabet.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 2.Eppens MC, Craig ME, Cusumano J, Hing S, Chan AK, Howard NJ, et al. Prevalence of diabetes complications in adolescents with type 2 compared with type 1 diabetes. Diabetes Care. 2006;29:1300–1306. doi: 10.2337/dc05-2470. [DOI] [PubMed] [Google Scholar]
- 3.Mohsin F, Craig ME, Cusumano J, Chan AK, Hing S, Lee JW, et al. Discordant trends in microvascular complications in adolescents with type 1 diabetes from 1990 to 2002. Diabetes Care 2005. 28:1974–1980. doi: 10.2337/diacare.28.8.1974. [DOI] [PubMed] [Google Scholar]
- 4.Kubin M, Tossavainen P, Hannula V, Lahti S, Hautala N, Falck A. Prevalence of retinopathy in Finnish children and adolescents with type 1 diabetes: a cross-sectional population-based retrospective study. Arch Dis Child. 2011;96:963–968. doi: 10.1136/adc.2011.210807. [DOI] [PubMed] [Google Scholar]
- 5.Zhang X, Saaddine JB, Chou CF, Cotch MF, Cheng YJ, Geiss LS, et al. Prevalence of diabetic retinopathy in the United States, 2005–2008. J Am Med Assoc 2010. 304:649–656. doi: 10.1001/jama.2010.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The SEARCH Study Group SEARCH for Diabetes in Youth: a multicenter study of the prevalence, incidence and classification of diabetes mellitus in youth. Control Clin Trials. 2004;25:458–471. doi: 10.1016/j.cct.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 7.Mayer-Davis EJ, Bell RA, Dabelea D, D'Agostino R, Imperatore G, Lawrence JM, et al. The many faces of diabetes in American youth: Type 1 and Type 2 diabetes in five race and ethnic populations: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2009;32:S99–S147. doi: 10.2337/dc09-S201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ingram DD, Parker JD, Schenker N, Weed JA, Hamilton B, Arias E, et al. United States Census 2000 population with bridged race categories. Vital Health Stat. 2003;2:1–55. [PubMed] [Google Scholar]
- 9.The SEARCH Study Group SEARCH for Diabetes in Youth: a multicenter study of the prevalence, incidence and classification of diabetes mellitus in youth. Control Clin Trials. 2004;25:458–471. doi: 10.1016/j.cct.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Kershnar AK, Daniels SR, Imperatore G, Palla SL, Petitti DB, Pettitt DJ, et al. Lipid abnormalities are prevalent in youth with type 1 and type 2 diabetes: the SEARCH for Diabetes in Youth Study. J Pediatr. 2006;149:314–319. doi: 10.1016/j.jpeds.2006.04.065. [DOI] [PubMed] [Google Scholar]
- 11.Klein R, Klein BE, Magli YL, Brothers RJ, Meuer SM, Moss SE, et al. An alternative method of grading diabetic retinopathy. Ophthalmology. 1986;93:1183–1187. doi: 10.1016/s0161-6420(86)33606-6. [DOI] [PubMed] [Google Scholar]
- 12.Nagi DK, Pettitt DJ, Bennett PH, Klein R, Knowler WC. Diabetic retinopathy assessed by fundus photography in Pima Indians with impaired glucose tolerance and NIDDM. Diabet Med. 1997;14:449–456. doi: 10.1002/(SICI)1096-9136(199706)14:6<449::AID-DIA367>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 13.Dowse GK, Humphrey AR, Collins VR, Plehwe W, Gareeboo H, Fareed D, et al. Prevalence and risk factors for diabetic retinopathy in the multiethnic population of Mauritius. Am J Epidemiol. 1998;147:448–457. doi: 10.1093/oxfordjournals.aje.a009470. [DOI] [PubMed] [Google Scholar]
- 14.Okudaira M, Yokoyama H, Otani T, Uchigata Y, Iwamoto Y. Slightly elevated blood pressure as well as poor metabolic control are risk factors for the progression of retinopathy in early-onset Japanese Type 2 diabetes. J Diabetes Complications. 2000;14:281–287. doi: 10.1016/s1056-8727(00)00114-8. [DOI] [PubMed] [Google Scholar]
- 15.Yokoyama H, Okudaira M, Otani T, Sato A, Miura J, Takaike H, et al. Higher incidence of diabetic nephropathy in type 2 than in type 1 diabetes in early-onset diabetes in Japan. Kidney Int. 2000;58:302–311. doi: 10.1046/j.1523-1755.2000.00166.x. [DOI] [PubMed] [Google Scholar]
- 16.Gallego PH, Craig ME, Hing S, Donaghue KC. Role of blood pressure in development of early retinopathy in adolescents with type 1 diabetes: prospective cohort study. Br Med J. 2008;337:a918. doi: 10.1136/bmj.a918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheung N, Rogers SL, Donaghue KC, Jenkins AJ, Tikellis G, Wong TY. Retinal arteriolar dilation predicts retinopathy in adolescents with type 1 diabetes. Diabetes Care. 2008;31:1842–1846. doi: 10.2337/dc08-0189. [DOI] [PMC free article] [PubMed] [Google Scholar]