Abstract
A 9 year old girl presented to us with complaints of fever and pain in burn wounds with deteriorating health for one month. According to Lund and Broder's chart, burns spanned the posterior trunk (13%), right arm (1.5%), left arm (1.5%), and buttocks (2.5%). The wounds showed improper healing. She had previously underwent split-thickness skin grafting, using skin harvests from thighs and antimicrobial therapy with vancomycin, fluconazole and colomycin with limited clinical improvement. Analgesia was administered. Blood cultures and tissue cultures from the burns indicated polymicrobial wound infection and sepsis, including methicillin resistant Staphylococcus aureus, Klebsiella pneumoniae and Pseudomonas aeruginosa. Despite broad-spectrum antibiotics, fever persisted and condition deteriorated. Antifungals were also administered with no clinical improvement. Eventually another split-thickness skin grafting was done to provide fresh grafts. In due course, ultraviolet light exposure, of wavelength 32–40 nm/W/cm2, was considered for treatment. In prone position, the wounds were exposed to ultraviolet phototherapy 6–8 h daily for 8 days. Eventually, wound healing and sepsis improved. Antibiotics were optimized and high protein diet was started. Eventually the wounds showed fresh margins and visible signs of healing. With remarkable clinical improvement and no further fever spikes, the patient was eventually discharged. She was advised to shower regularly, apply bandages with acetic acid. On her last outpatient follow up, 2 weeks after discharge, she was doing well, with no complaints of pain or fever. Examination of burns showed clean wounds, with clear margins and good graft uptake. She did not require any further grafting or surgical procedures thereafter.
Keywords: Sepsis, Burns, Wound infection, Ultraviolet light, Antibiotics
Highlights
-
•
Potential use of ultraviolet light as an adjuvant therapy for antibiotic resistant wound infection.
-
•
Not only bactericidal, but ultraviolet light can also potentially reduce healing time for wounds.
-
•
Scientific studies should be carried out to formally investigate ultraviolet light for this purpose.
-
•
Scientific studies could potentially any harmful side effects to this therapy, if there are any present.
Introduction
Treating post-traumatic wound sepsis is one of the most challenging problems that physicians face. Even with recent advancements in medicine and availability of new antibiotics, doctors may still have difficulty treating certain wound infections and resulting sepsis which remains unresponsive to a wide range of antimicrobial drugs.1,2 The potential role of ultraviolet (UV) light in the treatment of chronically infected wounds has previously been explored in a reliable study which showed remarkable antimicrobial effect against bacteria colonizing the superficial layers of chronic wounds.2 It even proved to be impressively effective against drug resistant organisms as well, including Pseudomonas aeruginosa and methicillin resistant Staphylococcus aureus (MRSA) in the same study. We report the case of a female child having post-burn wound infection and consequent sepsis. Tissue cultures showed infection by multiple microorganisms and a variety of antibiotic regimens were administered but showed no remarkable clinical improvement. An improvised technique of wound exposure to surgical UV lamps was then utilized which resulted in a noteworthy clinical response with a favorable outcome.
Case Summary
A 9-year-old female child presented to the emergency room with a history of burns inflicted one month back. She was complaining of fever and pain in burn wounds reaching a score of 5/10 on the pain scale. The child had waning health as a result of post-traumatic sepsis occurring due to the severe burns. Fever was high grade, showing a spiking pattern intermittent in nature, going up till 40 °C. She was initially managed at a local hospital where she underwent split-thickness skin graft (STSG) procedure using skin grafts from thighs and empiric antimicrobial therapy consisting of vancomycin, fluconazole, meropenem and colomycin was administered. Past medical history revealed a developmentally normal child with an up to date immunization status and no significant medical issues.
Physical examination showed an alert child with heart rate of 90 beats/minute and respiratory rate of 20 breaths/minute. According to Lund and Broder's chart, burns spanned the posterior trunk (13%), right arm (1.5%), left arm (1.5%), and buttocks (2.5%). The wounds showed signs of improper healing.
Complete blood count (CBC) was remarkable for anemia and neutrophilia and C-reactive protein (CRP) levels were elevated. Tissue cultures of the burn wounds were sent and the patient was started on paracetamol, morphine and pethidine for pain relief. The wound dressings were changed and re-applied. Cultures grew methicillin resistant S. aureus (MRSA) and other Staphylococcus species. Intravenous (IV) antibiotics were administered accordingly, including vancomycin, however, there was no clinical improvement.
Repeat cultures of the wounds grew colonies of P. aeruginosa, Protease mirabilis and Klebsiella pneumoniae. Culture and sensitivity reports showed P. aeruginosa sensitive only to ceftazidime and amikacin; these drugs were included in the drug therapy for additional antibacterial coverage. The patient was also given parenteral micronutrients and transfused with packed red blood cells.
With continuing fever spikes and negligible clinical response, the child was transferred to the special care unit. Subsequent wound cultures also showed presence of Acinetobacter baumannii sensitive only to colomycin. Hence colomycin was reintroduced into the regimen. The patient was started on a high protein calorie diet with vitamin B6, B complex and zinc supplementation, with frequent blood transfusions. However she showed minimal response to medical management and her condition continually deteriorated. The fever pattern continued and she grew weak with signs of anxiety, for which diazepam was given. Repeat wound cultures showed persistence of infection. Polymyxin B was added to the management along with tramadol and ondansetron for relieving pain and nausea, respectively. Eventually she underwent another STSG procedure to provide fresh grafts for the burns.
After one week, in light of no response to the above mentioned antibiotics, fluconazole was added as fungal infection was also suspected after a consult from the infectious diseases team and further culture reports were ordered. Linezolid was also added to the regimen. Over the next three days, she showed increasing distress as fever spikes became more frequent and CRP remained elevated.
In due course, exposure to UV light, of wavelength between 32 and 40 nm/W/cm2 (calculated as lamp aperture), was considered as an adjuvant treatment option. With the child sedated in prone position, the wounds were uncovered and UV phototherapy was started, with a distance of 25 cm between the UV lamp and the child's skin, exposing the burn sites for 6–8 h daily over a period of 8 days. Antibiotics were continued. During this period, wound healing and sepsis improved, which was followed with blood cultures daily. IV antibiotics were optimized and high protein diet was continued. At the end of the 8-day-therapy, wounds showed fresh margins and visible signs of healing. The patient was subsequently discharged in the next few days and advised to shower, change bandages using acetic acid and follow up weekly in the outpatient clinic. On her last outpatient follow up, 2 weeks after discharge, she was doing well, with no complaints of pain or fever. Examination of burns showed clean wounds, with clear margins and good graft uptake. She did not require any further grafting or surgical procedures thereafter. Details of the patient's clinical course, including WBC counts, fever pattern and antibiotic schedule and dosing are provided (Fig. 1, Table 1).
Figure 1.
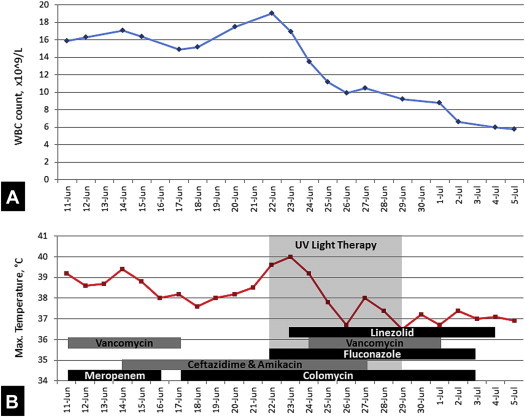
(A) Trend in the white blood cell count throughout the patient's hospital admission. (B) Trend in temperature recordings and details of the duration of antimicrobials used throughout the patient's hospital admission.
Table 1.
Start Dates, Stop Dates and Doses of Antimicrobials Used Duration the Patient's Hospital Admission.
| Antibiotic | Start Date | Stop Date | Dose |
|---|---|---|---|
| Meropenem | 11/06/13 | 16/06/13 | 400 mg/Q8H |
| Bacitracin | 14/06/13 | 5/07/13 | Topical use |
| Ceftazidime | 14/06/13 | 27/06/13 | 650 mg/Q8H |
| Amikacin | 14/06/13 | 27/06/13 | 300 mg/QD |
| Fluconazole | 22/06/13 | 03/07/13 | 100 mg/QD |
| Vancomycin | 24/06/13 | 01/07/13 | 300 mg/Q8H |
| Colomycin | 17/06/13 | 03/07/13 | 130 mg/Q12H |
| Linezolid | 23/06/13 | 04/07/13 | 260 mg/Q8H |
Discussion
The germicidal properties of UV light have been known, approximately, for a century. It is only recently that its medicinal value has been recognized in treating wound infections. Of the four spectrums that UV irradiation can be divided into, UV light C (200–280 nm) seems to be the most effective in being absorbed by the nucleic acids of a microorganisms and causing dimerization of pyrimidine molecules (especially thymine) that makes replication of the DNA impossible, hence making microorganisms more vulnerable.1
UV light has shown significant activity against the antibiotic-resistant bacteria highlighted in this report. It has been reported to be bactericidal against Pseudomonas infecting superficial layers chronic wounds.2 A. baumannii infected wounds in mice have been reported to improve up to 10 times better after treatment with UV light C in comparison to controls which were groups of infected mouse wounds not exposed to UV light C.3 Similar results have been obtained when investigating its activity against MRSA, being bactericidal within a time frame as short as 5 s.4 There are various clinical studies done which add to the evidence. The first clinical study was reported by Taylor et al5 who used UV light C irradiation (254 nm) for the disinfection of surgical wounds during total joint arthroplasty procedures. UV light C irradiation began on the open wounds 10 min after the procedure. Two different UV light C irradiances, 0.1 and 0.3 mW/cm2 were used. The average bacterial CFU in wounds was reduced by 87% with 0.1 mW/cm2 and 92% with 0.3 mW/cm2, compared with controls no exposed to UV light.
Shimomura et al6 examined the role of UV light C irradiation (254 nm) in prevention of catheter exit-site infections. Of the 68 continuous ambulatory peritoneal dialysis outpatients, UV light C irradiation was performed (twice per day, 30–60 s each time) in 18 cases that constantly revealed bacteria on culture at the catheter exit site. Ten cases (55%) became culture negative, three cases showed a microbial decrease and five cases remained unchanged. These results suggest that UV light C can eliminate bacteria and can be of prophylactic use for exit-site infections. Thai et al4 investigated the use of UV light C for the treatment of cutaneous ulcer infections. In this study, three patients with chronic ulcers infected with MRSA were treated with UV light C at 254 nm. UV light C irradiation was applied to each wound for 180 s, with the irradiance of 15.54 mW/cm2 (calculated at the UV lamp aperture). UV light C treatment reduced the relative amount of bacteria in wounds and facilitated wound healing in all patients.
Apart from its bactericidal activity, UV light C has been hypothesized to cause better wound healing in burns by activating melanocytes, which in turn cause the necessary changes in keratinocytes through their paracrine effects.7 This stimulates cellular proliferation, increased epidermal thickness and greater blood flow in the cutaneous capillaries.4
UV light when given to normal skin in mice has shown no gross changes. DNA lesions have been seen but they are mostly repaired within 24–72 h.8 Microorganisms have proven to be more sensitive to UV light C than native mammalian cells. This is attributed to the fact that damaged host cells have protective agents like DNA repair enzymes.1 In our case, the use of UV light did not show any adverse effects. However more work needs to be done to find any potential adverse effects of UV light C phototherapy for the treatment of infected wounds.
One of the early clinical studies in 1965 explored the effect of UV light C on wound healing. Freytes et al9 tested the use of UV light irradiation at 254 nm emitted for the treatment of indolent ulcers in three patients. All three showed reduced ulcer size, clean and with good granulation tissue. Nussbaum et al10 compared the use of UV light in combination with ultrasound (UVC/US) for wound healing of pressure ulcers with the use of low-level laser and standard nursing care alone. Results showed that UVC/US treatment had a greater effect on wound healing than nursing care, either alone or combined with laser. Conner-Kerr et al11 demonstrated the germicidal properties of UV light against antibiotic-resistant S. aureus and Enterococcus faecalis, in vitro, with up to 99.9% kill rates at exposures as short as 5 s.
Most of the studies so far report positive results of wound healing by UV light C light and none report any negative results with respect to wound healing. While pathogenic microorganisms impede the healing of infected wounds, one can expect that the eradication of microorganisms by UV light C would enhance wound healing in infected wounds in addition to its stimulating effect on melanocytes and consequent paracrine effects.1
As far as resistance is concerned, some bacteria have been reported to show resistance against UV light C when repeated cycles of phototherapy were given, however, it is not acquired very rapidly.1 Since such excessive repetitions in cycles of phototherapy are not expected while treating wounds, the risk of bacteria developing resistance remains low, however, actual microbiological studies need to be conducted to support this theory.
Conclusion
UV light shows great prospect as an adjuvant treatment coupled with antibiotics in dealing with infected wounds. Still, research and human clinical trials are needed to formulate a proper pharmacological and therapeutic basis for its medical application in humans and developing optimum protocols to implement its safe use and minimize side effects, if any.
Footnotes
Sources of funding: None.
Conflicts of interest: None to declare.
References
- 1.Dai T., Vrahas M.S., Murray C.K., Hamblin M.R. Ultraviolet C irradiation: an alternative antimicrobial approach to localized infections? Expert Rev Anti Infect Ther. 2012;10(2):185–195. doi: 10.1586/eri.11.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thai T.P., Keast D.H., Campbell K.E., Woodbury M.G., Houghton P.E. Effect of ultraviolet light C on bacterial colonization in chronic wounds. Ostomy Wound Manage. 2005;51(10):32–45. [PubMed] [Google Scholar]
- 3.Dai T., Murray C.K., Vrahas M.S., Baer D.G., Tegos G.P., Hamblin M.R. Ultraviolet C light for Acinetobacter baumannii wound infections in mice: potential use for battlefield wound decontamination? J Trauma Acute Care Surg. 2012;661(3):73. doi: 10.1097/TA.0b013e31825c149c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thai T.P., Houghton P.E., Keast D.H., Campbell K.E., Woodbury M.G. Ultraviolet light c in the treatment of chronic wounds with MRSA: a case study. Ostomy Wound Manage. 2002;48(11):52–60. [PubMed] [Google Scholar]
- 5.Taylor G., Bannister G., Leeming J. Wound disinfection with ultraviolet radiation. J Hosp Infect. 1995;30(2):85–93. doi: 10.1016/0195-6701(95)90148-5. [DOI] [PubMed] [Google Scholar]
- 6.Shimomura A., Tahara D., Tominaga M. The effect of ultraviolet rays on the prevention of exit-site infections. Adv Perit Dial. 1995;11:152–156. [PubMed] [Google Scholar]
- 7.Rennekampff H.O., Busche M.N., Knobloch K., Tenenhaus M. Is UV radiation beneficial in postburn wound healing? Med Hypotheses. 2010;75(5):436–438. doi: 10.1016/j.mehy.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 8.Dai T., Kharkwal G.B., Zhao J. Ultraviolet-C light for treatment of Candida albicans burn infection in mice. Photochem Photobiol. 2011;87(2):342–349. doi: 10.1111/j.1751-1097.2011.00886.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Freytes H.A., Fernandez B., Fleming W. Ultraviolet light in the treatment of indolent ulcers. South Med J. 1965;58(2):223–226. doi: 10.1097/00007611-196502000-00017. [DOI] [PubMed] [Google Scholar]
- 10.Nussbaum E.L., Biemann I., Mustard B. Comparison of ultrasound/ultraviolet-C and laser for treatment of pressure ulcers in patients with spinal cord injury. Phys Ther. 1994;74(9):812–823. doi: 10.1093/ptj/74.9.812. [DOI] [PubMed] [Google Scholar]
- 11.Conner-Kerr T.A., Sullivan P.K., Gaillard J., Franklin M.E., Jones R.M. The effects of ultraviolet radiation on antibiotic-resistant bacteria in vitro. Ostomy Wound Manage. 1998;44(10):50–56. [PubMed] [Google Scholar]


