Abstract
Context
Melanoma is the most deadly form of skin cancer and an important public health concern. Given the substantial health burden associated with melanoma, it is important to examine the economic costs associated with its treatment. The purpose of the current study was to systematically review the literature on the direct medical care costs of melanoma.
Evidence acquisition
A systematic review was performed using multiple databases including MEDLINE, Embase, CINAHL, and Econlit. Nineteen articles on the direct medical costs of melanoma were identified.
Evidence synthesis
Detailed information on the study population, study country/setting, study perspective, costing approach, disease severity (stage), and key study results were abstracted. The overall costs of melanoma were examined as well as per-patient costs, costs by phase of care, stage of diagnosis, and setting/type of care. Among studies examining all stages of melanoma, annual treatment costs ranged from $44.9 million among Medicare patients with existing cases to $932.5 million among newly diagnosed cases across all age groups.
Conclusions
Melanoma leads to substantial direct medical care costs, with estimates varying widely because of the heterogeneity across studies in terms of the study setting, populations studied, costing approach, and study methods. Melanoma treatment costs varied by phase of care and stage at diagnoses; costs were highest among patients diagnosed with late-stage disease and in the initial and terminal phases of care. Aggregate treatment costs were generally highest in the outpatient/office-based setting; per-patient/per-case treatment costs were highest in the hospital inpatient setting. Given the substantial costs of treating melanoma, public health strategies should include efforts to enhance both primary prevention (reduction of ultraviolet light exposure) and secondary prevention (earlier detection) of melanoma.
Context
Skin cancer is the most common form of cancer in the U.S. and is therefore an important public health concern.1 The most common form of skin cancer, non-melanoma skin cancer (NMSC), has been increasing annually. In 2006, the estimated incidence in the U.S. was 3.5 million, representing a doubling in incidence since 1994.1,2 Although not as common as NMSC, melanoma is the most deadly form of skin cancer, with 59,695 newly diagnosed cases in the U.S. and 8623 deaths in 2008, the most current data available from population-based cancer registries.3,4 Similar to NMSC, the incidence of melanoma also has been increasing. For example, melanoma incidence among the fair-skinned Caucasian population worldwide has been increasing at approximately 3%–7% per year.5–7 In the U.S., the average lifetime risk of developing melanoma has increased from 1 in 1500 in 1935 to 1 in 30 in 2009.8,9
Given the high and increasing incidence of skin cancer, it is important to understand its economic burden. Common measures of economic burden of disease include the following: direct medical costs, the cost of resources used for treating a particular disease; indirect costs, the value of resources lost due to a particular disease10; and years of life lost, the expected years of potential life lost because of a particular disease.11 A recent study12 has provided a comprehensive review of the indirect costs and years of life lost from both melanoma and NMSC. Additionally, recent studies13,14 have provided a review of the direct medical costs of NMSC.
Absent from the literature is a comprehensive review of the direct medical care costs of melanoma. Thus, the purpose of the current study is to fill this gap and review the literature on the direct medical care costs of melanoma. A comprehensive review is provided of the overall costs of melanoma, per-patient costs, and costs by phase of care, stage of diagnosis, and setting/type of care.
Evidence Acquisition
A systematic search was performed using multiple databases, including MEDLINE, Embase, CINAHL, and Econlit. The search strategy to identify relevant studies included the following terms: skin cancer, cancer of the skin, skin neoplasms, melanoma, cost of illness, health care costs, direct service costs, health expenditures, economics, pharmacoeconomics, costs of treatment, costs, health care, economic analysis, expenditures, burden of illness, economic impact. Additionally, a manual search was performed by reviewing the reference lists from retrieved articles and reports to ensure a comprehensive review of the literature.
The following were the preset inclusion criteria for the studies selected: published in English, full text available for review, and published between January 1990 and December 2011. Restricting inclusion to this time period allowed capture of current articles on melanoma cost. All titles and abstracts of the identified articles and reports meeting the initial search criteria were reviewed. Studies with no melanoma treatment cost estimates, review articles, and cost-effectiveness studies were excluded. A review of the full text articles and reports was then conducted to identify studies quantifying the direct medical costs of melanoma.
For each eligible study, detailed information on the country and setting, study population, study perspective, costing approach, and key study results were abstracted. Cost-of-illness studies can be conducted from several perspectives, with each including slightly different cost components. For example, common perspectives include costs to society, the healthcare system, or the individual.
The costing approach of each of the studies also was examined. Studies were classified as either using the treatment approach, net cost approach, regression approach, or the attributable cost approach.10 The treatment approach assesses health services and expenditures associated with specific tests, procedures, and drugs. The net cost approach calculates the difference in total healthcare expenditures for individuals with melanoma and a group of individuals without melanoma. The regression approach uses regression analysis to control for other factors that may affect cost. The attributable cost method uses a top–down approach partitioning total costs among specific diseases.10
Study results were presented in various ways in the literature. In several studies, the results included the aggregate medical costs of melanoma as well as the costs per patient. In studies where medical costs per patient were not reported, they were calculated by dividing the total medical costs by the number of patients reported in the study, when possible. Similarly, in studies where total medical costs were not reported, they were calculated by multiplying per-patient medical costs by the number of patients in the study population.
A number of studies categorized the treatment of melanoma patients into three clinically relevant phases of care (initial, continuing, and terminal) and provided estimates of the medical costs separately by phase. The initial phase is defined as the time period directly following diagnosis (typically up to 12 months), the terminal phase is defined as the final months of life (typically up to 12 months), and the continuing phase is defined as the period between the initial and terminal phases of care.15,16
Additionally, many of the studies reported medical costs by stage of diagnosis. In these studies, melanoma stage was defined as Stages 0, I, II, III, and IV; or local, regional, and distant. Lastly, melanoma direct medical costs by setting/type of care were abstracted from studies providing such estimates. For example, a number of studies provide separate estimates for the costs of inpatient and outpatient melanoma care.
To allow for greater comparability among studies and across countries, the Consumer Price Index (CPI) and purchasing power parity (PPP) were used. Costs were first adjusted to 2010 dollars using the CPI.17 For the 11 studies conducted outside the U.S., country-specific CPI from the Organization for Economic Co-operation and Development (OECD) was used to adjust costs to 2010 country-specific currency.18 Currency from other countries was converted to U.S. dollars by multiplying the adjusted currency by the PPP rate obtained from the OECD for each country.19 For non-OECD countries, data from the International Monetary Fund were used to convert currency.20 All costs reported in the current study are in 2010 U.S. dollars.
Evidence Synthesis
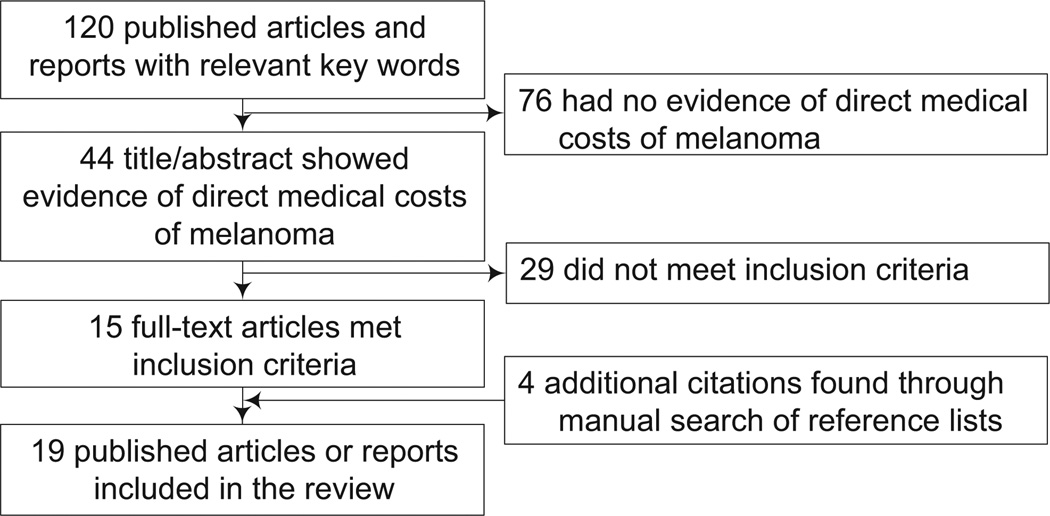
The initial literature search yielded 120 studies. After reviewing titles, abstracts, and full-text studies, 15 studies met the inclusion criteria. A manual search of the reference lists identified four additional studies meeting the inclusion criteria. In total, 19 articles and reports examining the direct medical costs of melanoma were included in the present review (Figure 1). These studies reported the direct medical care costs of melanoma in a number of countries, including Australia, Brazil, France, Germany, New Zealand, Spain, Sweden, the United Kingdom (UK), and the U.S.
Figure 1.
Flowchart illustrating the study selection process
Study Characteristics and Key Findings
The number of studies examining the treatment costs of melanoma increased over the study period. Although the search criteria covered 22 years, the majority of studies were published in the past 4 years, with no studies matching the inclusion criteria from 1990 to 1997. Table 1 displays the characteristics of the 19 studies included in this review. As shown, the study perspective, study population, treatment-cost approach, and duration of follow-up varied substantially across studies. Some studies focused on particular subpopulations characterized by stage, phase of care, treatment interventions, and settings of care. For example, two studies provide treatment costs by phase of care, eight studies provide estimates by stage of diagnosis, and 12 studies provide estimates specific to various treatment interventions and settings of care.
Table 1.
Major characteristics and key results of articles reporting melanoma treatment costs
| Study | Country and setting |
Sample characteristics | Perspective | Costing approach | Key results |
|---|---|---|---|---|---|
| U.S. studies | |||||
| Tsao (1998)21 | U.S. | 44,300 newly diagnosed patients in 1997 with all stages of melanoma | Payer | Treatment approach, melanoma-related care | The annual direct cost of treating newly diagnosed melanoma in 1997 was estimated to be $932.5 million ($23,140 per patient). |
| Hillner (2001)22 | U.S., UPCI | 100 patients with metastatic melanoma presenting at a referral center | Payer | Treatment approach, melanoma-related care incurred at UPCIa | The approximate cost per patient with metastatic melanoma was $101,166. |
| Housman (2003)23 | U.S., Medicare | An average of 51,669 patients per year aged ≥65 years from 1992–1995 with all stages of melanoma | Payer | Treatment approach, melanoma-related care | The average annual cost of melanoma care in Medicare from 1992–1995 was $44.9 million ($869 per patient). |
| Bickers (2006)24 | U.S. | All prevalent melanoma cases (approximately 720,000) in 2004 | Payer | Treatment approach, melanoma-related care | The annual cost of melanoma care in the U.S. in 2004 was $364.6 million ($506 per patient). |
| Yabroff (2008)15 | U.S., Medicare | 22,385 patients aged ≥65 years diagnosed in 2004 with all stages of melanoma | Payer | Net cost approach, costs of care among melanoma patients compared to average Medicare enrollee without cancer | The aggregate 5-year net costs of melanoma care for the cohort of elderly Medicare patients diagnosed in 2004 was $226.8 million ($10,131 per patient). |
| Alexandrescu(2009)25 | U.S. | Dynamic model assessing newly diagnosed melanoma patients with all stages over 5 years | Societal | Treatment approach, includes cost of treatment, surveillance, lost income, and terminal care | The costs of melanoma care increased dramatically by stage, with per-patient 5-year costs ranging from $4960 for in situ tumors to $170,515 for Stage-IV melanoma. |
| Davis (2009)26 | U.S., Medicare | 6470 high-risk and metastatic (Stage IIB/C, IIIA/B, IIIC, and IV) patients aged ≥65 years | Payer | Regression approach, all-cause healthcare costs | All-cause healthcare costs per patient per month were $12,687 for Stage-IV patients, compared with $2585, $3755, and $7615 for Stages IIB/C, IIIA/B, and IIIC, respectively. |
| Seidler (2010)16 | U.S., Medicare | 1858 patientsb aged ≥65 years from the SEER-Medicare data set from 1991 to 1996 with all stages of melanoma | Payer | Treatment approach, melanoma-related care over 5-year period | The annual cost of melanoma care in Medicare in 1996 was $424.6 million ($28,061 per patient). Per-patient lifetime costs were $48,013. |
| Non-U.S. studies | |||||
| Mathers (1998)27 | Australia | All melanoma cases in 1993 | Payer | Attributable costs, portion of total direct medical costs attributable to melanoma | Total costs for melanoma care in Australia were $67.9 million in 1993. |
| O’Dea (2000)28 | New Zealand | All melanoma cases in 1998 | Payer | Treatment approach, micro-costing of hospital costs, outpatient costs extrapolated from Australia data | The total cost of melanoma care in New Zealand was estimated at $9.4 million per year. |
| Nilsson (2003)29 | Sweden, Stockholm County | 2785 patients treated for melanoma in 1999 with all stages | Payer | Attributable costs, total costs attributable to prevalent cases of melanoma | The annual cost of melanoma care in Stockholm County, Sweden, in 1999 was $3.1 million ($1108 per patient). |
| Stang (2007)30 | Germany | 20,455 melanoma-related hospitalizations in 2003 | Payer | Treatment approach,c hospitalization costs | Annual hospital costs for melanoma care in Germany were estimated to be $68.6–$82.0 million in 2003. Melanoma in situ costs were estimated to be $3.1–$3.6 million. |
| Chevailer (2008)31 | France | 42,911 melanoma-related hospital stays in 2004 | Payer | Treatment approach, hospitalization costs | Annual hospital costs for melanoma care in France were estimated to be $74.1 million in 2004. |
| Tinghog (2008)32 | Sweden | All melanoma cases in 2005 | Payer | Attributable costs (inpatient), treatment approach (outpatient, primary care) | The cost of melanoma care in Sweden in 2005 was $29.8 million. |
| Souza (2009)33 | Brazil, Sao Paulo | 2740 cases of melanoma diagnosed from 2000 to 2007 with all stages of melanoma | Payer | Treatment approach, diagnosis and treatment costs | The total annual cost of diagnosing and treating melanoma among public insurance was $29.0 million ($10,586 per patient) and $66.8 million among private insurance ($24,394 per patient). |
| Almazan-Fernandez (2009)34 | Spain | Descriptive analysis of costs based on theoretic model | Payer | Treatment approach, diagnosis and treatment costs | Total costs of melanoma diagnosis and treatment per patient ranged from $11,863 to $13,588. |
| Morris (2009)35 | United Kingdom, England | 6928 patients newly diagnosed with melanoma in 2002 with all stages | Societal | Treatment approach, includes outpatient and hospital costs, travel costs, and lost earnings | The total cost of melanoma care in England in 2002 was estimated to be approximately $43.9 million ($6336 per patient). |
| O’Dea (2009)36 | New Zealand | All melanoma cases in 2006 | Payer | Treatment approach, micro-costing of hospital costs, outpatients costs extrapolated from Australia data | The total cost of melanoma care in New Zealand was estimated to be $4.0 million in 2006. |
| Leiter (2009)37 | Germany, University of Tuebingen | 1996 patients with Stage I, II, or III melanoma visiting the University of Tuebingen for follow-up | Payer | Treatment approach, cost of follow-up and detection of recurrences | Total costs of 2-year follow-up examinations of melanoma patients were estimated to be $635,726 in Germany (corresponding U.S. cost: $1.9 million). Per-recurrence costs were $3117 in Germany (corresponding U.S. cost: $9162). |
Note: All costs are in 2010 U.S. dollars.
The costs included from outside UPCI were for patients who underwent surgery or received radiation prior to referral.
Cost estimates were based on 1858 patients and results were applied to all patients aged ≥65 years with melanoma (n = 15,130).
Three different estimates were provided using three different sources of cost data. The range of three estimates is shown.
UPCI, University of Pittsburgh Cancer Institute
Estimates of the annual cost of melanoma care in the U.S. varied substantially depending on the study population and costing approach used. For example, among studies examining all stages of melanoma, estimates ranged from $44.9 million among Medicare patients with existing cases,23 to $932.5 million among newly diagnosed cases across all age groups.21 Additionally, annual per-patient costs ranged from $506 among prevalent cases of melanoma24 to $23,410 among newly diagnosed cases.21
Although comparison across countries is limited because of the heterogeneity associated with the study populations and methods, medical care costs of melanoma were generally lower in studies conducted outside the U.S. The annual cost of treating melanoma ranged from $3.1 million among prevalent cases of melanoma in Stockholm County, Sweden, estimated using the attributable cost approach29 to $66.8 million in Sao Paolo, Brazil, estimated using the treatment approach.33 Similar differences in study methodology led per-patient costs to range from $110829 to $24,39433 in studies conducted outside the U.S.
Costs by Phase of Care
Table 2 summarizes the findings from the two studies estimating per-patient melanoma treatment costs over the initial, interim, and terminal treatment phases. Both studies, conducted in the U.S., found costs to generally be highest in the terminal phase, less in the initial phase, and the least in the interim phase. Seidler et al.16 found that initial- and interim-phase costs were three to five times greater in Stages II, III, and IV than in Stage 0. Yabroff et al.15 found that initial and terminal phase costs were two to six times higher among distant-stage patients compared with local-stage patients.15
Table 2.
Melanoma direct medical costs per person by treatment phase (initial, interim, terminal), for those aged ≥65 years, U.S.
| Stage | Treatment costs, $ | ||
|---|---|---|---|
| Initial | Interim | Terminal | |
| Seidler (2010)6,a | |||
| All, per month | 2386 (4 months) | 980 | 4277 (6 months) |
| 0 | 1086 | 565 | 4684 |
| I | 2049 | 757 | 5048 |
| II | 3258 | 1644 | 4534 |
| III | 4415 | 1574 | 3567 |
| IV | 4325 | 2866 | 3680 |
| Yabroff (2008)15,b | |||
| All, men only, per year | 3977 (12 months) | 1437 | 28,545 (12 months) |
| All, women only | 3669 | 581 | 24,613 |
| Local | 4023 | 25,242 | |
| Regional | 13,634 | 32,847 | |
| Distant | 27,211 | 57,860 | |
Note: All costs are in 2010 U.S. dollars.
For patients surviving ≥1 year, the initial, interim, and terminal phases were 4, 8, and 6 months, respectively; for patients surviving <1 year, the phases were 4, 2, and 6 months.
The initial phase was defined as the first 12 months after diagnosis, the last year of life phase was defined as the final 12 months of life, and the continuing phase was defined as all months between the initial and last year of life phases of care. For patients surviving <24 months, the final 12 months of observation were allocated first to the last year of life phase. Net costs of melanoma care are presented.
Costs by Stage
Table 3 provides the direct medical costs of treating melanoma by stage of diagnosis. Of the eight studies reporting melanoma medical costs by stage, six were conducted in the U.S., one in Brazil, and one in Spain. Although study heterogeneity limits direct comparisons across the studies, higher treatment costs were found consistently among cases diagnosed in later stages compared with those diagnosed in earlier stages. For example, the annual per-patient costs for Stage IV melanoma were $34,103–$152,244 per year in the U.S.16,26 and $28,141–$28,753 in Brazil.33 In comparison, the annual cost for Stage-I melanoma was $2,169 –$14,499 in the U.S.16,21 and $487–$700 in Brazil.33
Table 3.
Melanoma direct medical costs per person by stage, $
| Study | Stage | ||||
|---|---|---|---|---|---|
| 0 | I | II | III | IV | |
| U.S. STUDIES | |||||
| Tsao (1998)21 | NA | 2,169 | 5,463 | 69,006 | 70,231 |
| Hillner (2001)22 | NA | NA | NA | NA | 101,167 per case |
| Davis (2009)26,a | NA | NA | 31,032b | 68,220c | 152,244 |
| Alexandrescu (2009)25,d | 992 | 3,351e | 14,733f | 36,111c | 34,103 |
| Seidler (2010)16 | 8,930 | 14,499 | 26,667 | 31,778 | 39,631 |
| Yabroff (2008)15,g | Local | Regional | Distant | ||
| Initial year | 4,023 | 13,634 | 27,211 | ||
| Last year | 25,242 | 32,847 | 57,860 | ||
| NON-U.S. STUDIES | 0 | I | II | III | IV |
| Almazan-Fernandez (2009)34 | NA | NA | NA | 12,730 per caseh | NA |
| Souza (2009)33 | |||||
| Public insurance | 338 | 700 | 999 | 27,189 | 28,141 |
| Private insurance | 155 | 487 | 793 | 86,875 | 28,753 |
Note: Annual per-patient medical costs are reported unless otherwise noted. All costs are in 2010 U.S. dollars.
Study reported monthly costs. To obtain annual costs, the monthly cost by was multiplied by 12. All-cause healthcare costs are reported.
Only includes those diagnosed with Stages IIB/C
Cost was computed by taking the average cost among those diagnosed with Stages IIIA/B and Stage IIIC.
Study reports 5-year costs. To obtain annual estimates, the costs were divided by five.
Cost was computed by taking the average cost among those diagnosed with Stage IA and Stage IB.
Cost was computed by taking the average cost among those diagnosed with Stage IIA, Stage IIB, and Stage IIC.
Net costs of melanoma care are presented.
Cost was computed by taking the average cost among those with lymph-node metastasis; does not include follow-up costs.
NA, not applicable
Costs by Intervention
Appendix A (available online at www.ajpmonline.org) presents the direct medical costs of melanoma by different treatment interventions and settings of care. Although each study breaks down the components of medical costs somewhat differently, there are some important similarities in the findings. In studies conducted in the U.S. and in other countries, aggregate costs were generally highest in the outpatient/office-based setting, whereas per-patient or per-visit costs were highest in the inpatient hospital setting.24,26,27,29,32,35,36 Although study heterogeneity limits direct comparisons across countries, in each setting of care, melanoma medical costs tended to be higher in studies conducted in the U.S. compared with those conducted outside the U.S.
Discussion
In the review of the treatment costs of melanoma in the U.S. and a number of countries throughout the world, a great deal of heterogeneity across the studies was found in terms of the study settings, populations studied, types of services included, costing approaches, and study methods. This suggests that aggregate national estimates and international comparisons of the costs of melanoma treatment should be approached carefully. Despite this limitation, it is clear that the magnitude of the costs of melanoma treatment is substantial. Moreover, the burden of melanoma is likely to rise, as the incidence has been increasing worldwide.
Although the survival benefits of being diagnosed with early-stage melanoma have been documented clearly,41 it is also important to examine the economic impact of treating early- versus late-stage melanoma. It is clear from this review that the medical costs of melanoma are highest among people diagnosed with late-stage melanoma and during the terminal phase of care. For example, Tsao et al.21 found that 55% of the annual direct cost for treating melanoma is for patients with Stage-IV disease, and about one third of the total cost is related to treating melanoma at the end of life. Yabroff et al.15 found that the net costs of care in the last year of life among patients with distant disease were approximately double the costs among patients diagnosed with local disease.
The findings showing that aggregate costs for melanoma treatment are generally higher in the outpatient setting is consistent with the literature on cancer treatment patterns. A recent study has shown that cancer-related treatment costs have shifted away from the inpatient setting and toward the outpatient setting.42 In 2002–2003, the overwhelming majority (87%) of cancer patients visited physician offices.43 Although the per-patient/per-case costs are lower in the outpatient setting, the high volume of services provided makes it the most costly component of melanoma treatment at the aggregate level. However, treatment costs tend to be the highest in the inpatient hospital setting when examined on a per-patient/per-case basis, likely an effect of higher unit costs, and the likelihood that those treated in the inpatient setting are more advanced cases requiring more-intensive and costly treatment.24,26
In the U.S., diagnosis of melanoma in the outpatient setting has been shown to be one factor leading to the under-reporting of melanoma cases to central cancer registries, and the subsequent underestimate of disease burden.44 However, it is clear that melanoma treatment presents a substantial economic burden, particularly among late-stage diagnoses and during the terminal phase of care. Given the magnitude of these costs, increased efforts around primary and secondary prevention are warranted. If effective, these efforts have the potential to prevent melanoma cases, diagnose cases in earlier stages, increase survival, and reduce the health and economic burden associated with melanoma. For example, it has been estimated that if all melanoma patients were diagnosed in Stage 0 or I, the annual direct costs of melanoma treatment among those aged ≥65 years would be 40%–65% lower than their current value, resulting in substantial cost savings in Medicare.16
Given these findings, strategies must include efforts to enhance both primary prevention (reduction of ultraviolet [UV] light exposure) and secondary prevention (earlier detection). Although routine screening for early detection of skin cancer currently is not recommended by the U.S. Preventive Services Task Force and the National Health and Medical Research Council,45,46 screening among individuals at increased risk for melanoma has been shown to be cost effective and should be considered. For example, Freedberg et al.47 estimated a cost-effectiveness ratio of $29,170 per life-year saved for a one-time screening by dermatologists among high-risk individuals in the U.S. Similarly, in Australia the cost effectiveness of screening individuals aged ≥50 years by family practice doctors every 2 years was estimated to be $12,318 and $21,188 (U.S. dollars) for men and women, respectively.48
There are several effective primary prevention strategies that can be implemented to help reduce the burden of melanoma. Specifically, the Community Preventive Services Task Force recommends education and policy interventions in primary schools, and programs for adults in outdoor recreational or tourism settings in an effort to improve sun-avoidance or skin-covering behaviors.49 Additionally, a review by the U.S. Preventive Services Task Force has shown that primary care–relevant behavioral counseling can increase sun-protective behaviors and decrease indoor tanning.50
These prevention efforts have the potential to not only improve health but also to save money. For example, the SunWise School Program, a sun-safety education program developed by the U.S. Environmental Protection Agency to teach children how to protect themselves from overexposure to the sun could lead to substantial reductions in skin cancer incidence and mortality, while saving $2–$4 in medical care and productivity loss for each dollar invested in the program.51 Similarly, in Australia, the SunSmart public education program motivating sun-protection behavior through structural, environmental, and legislative initiatives is estimated to save 22,000 life-years in the future, while saving approximately $2 for every dollar invested.52
Although there are many risk factors that influence the likelihood of developing melanoma, the most preventable known risk factor is exposure to UV radiation, from the sun and artificial devices such as tanning beds.53,54 Despite recent evidence demonstrating the link between indoor tanning beds and melanoma, the use of indoor tanning devices remains common among both youth and adults in the U.S.38,39,55,56 Given the known health risk associated with indoor tanning, many organizations recommend regulations limiting access to such devices.57,58 In the U.S., more than 30 states have laws restricting minors’ access to tanning facilities,51 although the presence of such legislation has been shown to have limited effectiveness.59 Successful regulations could lead to both health and economic benefits. For example, in Australia it was estimated that stricter regulations on indoor tanning could avert an average of 24 melanoma cases per 100,000 people and $32,000 in medical costs in these same people.40
Given the rising incidence of melanoma, treatment of the disease will continue to be a substantial economic burden. In recent years, more-effective and expensive melanoma treatments have been introduced. An evaluation of the use of these newer expensive treatments and the impact of their use on melanoma survival, and the cost of melanoma care, will be an important area for future research. As treatment costs for advanced melanoma increase, prevention efforts should become even more cost effective. Additional research is needed to evaluate the impact of these prevention efforts, not only on the prevention and early detection of melanoma but also on the treatment costs of melanoma.
Conclusion
The present study presents a detailed overview of the direct medical costs of treating melanoma. In summary, a great deal of heterogeneity was found across studies with regard to study settings, populations studied, costing approaches, and study methods. However, it is clear that the magnitude of the costs associated with melanoma treatment is substantial, particularly among patients diagnosed with late-stage disease and in the terminal phase of care. The information presented in this review can help inform public health decision makers as they develop health policy and comprehensive intervention programs to decrease both the health and economic burden of melanoma. Additionally, these estimates can be used by researchers in examining the cost effectiveness of melanoma prevention and control strategies.
Supplementary Material
Appendix
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.amepre.2012.07.031.
Footnotes
The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the CDC.
No financial disclosures were reported by the authors of this paper.
References
- 1.Rogers HW, Weinstock MA, Harris AR, et al. Incidence estimate of nonmelanoma skin cancer in the U.S., 2006. Arch Dermatol. 2010;146(3):283–287. doi: 10.1001/archdermatol.2010.19. [DOI] [PubMed] [Google Scholar]
- 2.Miller DL, Weinstock MA. Nonmelanoma skin cancer in the U.S.: incidence. J Am Acad Dermatol. 1994;30(5):774–778. doi: 10.1016/s0190-9622(08)81509-5. [DOI] [PubMed] [Google Scholar]
- 3.DHHS, CDC, National Cancer Institute. U.S. cancer statistics: 1999–2008 incidence, WONDER online database. 2011 wonder.cdc.gov/cancer-v2008.html.
- 4.CDC, National Center for Health Statistics. Underlying cause of death, 1999–2008, on CDC WONDER online database, released 2011. (Data compilation source is Multiple Cause of Death File for correponding year: for 2008, Ser. 20 No. 2N, 2011; for 2007, Ser. 20, No. 2M, 2010; for 2005–2006, Ser. 20, No. 2L, 2009; for 1999–2004, Ser. 20, No. 2J, 2007.) wonder.cdc.gov/ucd-icd10.html.
- 5.Diepgen T, Mahler V. The epidemiology of skin cancer. Br J Dermatol. 2002;146:1–6. doi: 10.1046/j.1365-2133.146.s61.2.x. [DOI] [PubMed] [Google Scholar]
- 6.Linos E, Swetter SM, Cockburn MG, Colditz GA, Clarke CA. Increasing burden of melanoma in the U.S. J Invest Dermatol. 2009;129(7):1666–1674. doi: 10.1038/jid.2008.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Vries E, Willem Coebergh J. Cutaneous malignant melanoma in Europe. Eur J Cancer. 2004;40(16):2355–2366. doi: 10.1016/j.ejca.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 8.Rigel DS. The effect of sunscreen on melanoma risk. Dermatol Clin. 2002;20(4):601–606. doi: 10.1016/s0733-8635(02)00024-4. [DOI] [PubMed] [Google Scholar]
- 9.Rigel DS. Trends in dermatology: melanoma incidence. Arch Dermatol. 2010;146(3):318. doi: 10.1001/archdermatol.2009.379. [DOI] [PubMed] [Google Scholar]
- 10.Segel JE. Working paper. RTI International; Cost-of-illness studies—a primer. www.rti.org/pubs/coi_primer.pdf. [Google Scholar]
- 11.Ekwueme DU, Guy GP, Jr, Li C, Rim SH, Parelkar P, Chen SC. The health burden and economic costs of cutaneous melanoma mortality by race/ethnicity—U.S., 2000 to 2006. J Am Acad Dermatol. 2011;65(5S1):S133–S143. doi: 10.1016/j.jaad.2011.04.036. [DOI] [PubMed] [Google Scholar]
- 12.Guy GP, Jr, Ekwueme DU. Years of potential life lost and indirect costs of melanoma and non-melanoma skin cancer: a systematic review of the literature. PharmacoEcon. 2011;29(10):863–874. doi: 10.2165/11589300-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 13.Higashi MK, Veenstra DL, Langley PC. Health economic evaluation of non-melanoma skin cancer and actinic keratosis. PharmacoEcon. 2004;22(2):83–94. doi: 10.2165/00019053-200422020-00002. [DOI] [PubMed] [Google Scholar]
- 14.Mudigonda T, Pearce DJ, Yentzer BA, Williford P, Feldman SR. The economic impact of non-melanoma skin cancer: a review. J Natl Compr Canc Netw. 2010;8(8):888. doi: 10.6004/jnccn.2010.0066. [DOI] [PubMed] [Google Scholar]
- 15.Yabroff KR, Lamont EB, Mariotto A, et al. Cost of care for elderly cancer patients in the U.S. J Natl Cancer Inst. 2008;100(9):630. doi: 10.1093/jnci/djn103. [DOI] [PubMed] [Google Scholar]
- 16.Seidler AM, Pennie ML, Veledar E, Culler SD, Chen SC. Economic burden of melanoma in the elderly population: population-based analysis of the Surveillance, Epidemiology, and End Results (SEER)-Medicare Data. Arch Dermatol. 2010;146(3):249. doi: 10.1001/archdermatol.2009.389. [DOI] [PubMed] [Google Scholar]
- 17.Bureau of Labor and Statistics. Consumer price indexes: Bureau of Labor Statisitcs. 2010 www.bls.gov/cpi/.
- 18.Organisation for Economic Co-operation and Development. Consumer price indices (CPI) for OECD countries and major non-member economies. www.oecd.org/LongAbstract/0,3425,en_2649_33715_37177216_1_1_1_1,00.html.
- 19.Organisation for Economic Co-operation and Development. Purchasing power parities (PPP) www.oecd.org/statisticsdata/0,3381,en_2649_34357_1_119656_1_1_1,00.html.
- 20.International Monetary Fund. 2011 World economic outlook. www.imf.org/external/pubs/ft/weo/2011/02/weodata/index.aspx.
- 21.Tsao H, Rogers GS, Sober AJ. An estimate of the annual direct cost of treating cutaneous melanoma. J Am Acad Dermatol. 1998;38(5):669–680. doi: 10.1016/s0190-9622(98)70195-1. [DOI] [PubMed] [Google Scholar]
- 22.Hillner BE, Kirkwood JM, Agarwala SS. Burden of illness associated with metastatic melanoma: an audit of 100 consecutive referral center cases. Cancer. 2001;91(9):1814–1821. doi: 10.1002/1097-0142(20010501)91:9<1814::aid-cncr1201>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 23.Housman TS, Feldman SR, Williford PM, et al. Skin cancer is among the most costly of all cancers to treat for the Medicare population. J Am Acad Dermatol. 2003;48(3):425–429. doi: 10.1067/mjd.2003.186. [DOI] [PubMed] [Google Scholar]
- 24.Bickers DR, Lim HW, Margolis D, et al. The burden of skin diseases: 2004: a joint project of the American Academy of Dermatology Association and the Society for Investigative Dermatology. J Am Acad Dermatol. 2006;55(3):490–500. doi: 10.1016/j.jaad.2006.05.048. [DOI] [PubMed] [Google Scholar]
- 25.Alexandrescu DT. Melanoma costs: a dynamic model comparing estimated overall costs of various clinical stages. Dermatol Online J. 2009;15(11):1. [PubMed] [Google Scholar]
- 26.Davis KL, Mitra D, Kotapati S, Ibrahim R, Wolchok JD. Direct economic burden of high-risk and metastatic melanoma in the elderly: evidence from the SEER-Medicare linked database. Appl Health Econ Health Policy. 2009;7(1):31–41. doi: 10.1007/BF03256140. [DOI] [PubMed] [Google Scholar]
- 27.Mathers C, Penm R, Sanson-Fisher R, Campbell E. Canberra: AIHW; 1998. Health system costs of cancer in Australia 1993–94. Health and welfare expenditure series. Cat. no. HWE 8. [Google Scholar]
- 28.O’Dea D. The costs of skin cancer to New Zealand. Wellington, New Zealand: Wellington School of Medicine, University of Otago; 2000. [Google Scholar]
- 29.Nilsson GH, Carlsson L, Dal H, Ullen H. Skin diseases caused by ultraviolet radiation: the cost of illness. Int J Technol Assess Health Care. 2003;19(4):724–730. doi: 10.1017/s0266462303000709. [DOI] [PubMed] [Google Scholar]
- 30.Stang A, Stausberg J, Boedeker W, Kerek-Bodden H, Jockel KH. Nationwide hospitalization costs of skin melanoma and non-melanoma skin cancer in Germany. J Eur Acad Dermatol Venereol. 2008;22(1):65–72. doi: 10.1111/j.1468-3083.2007.02334.x. [DOI] [PubMed] [Google Scholar]
- 31.Chevalier J, Bonastre J, Avril MF. The economic burden of melanoma in France: assessing healthcare use in a hospital setting. Melanoma Res. 2008;18(1):40–46. doi: 10.1097/CMR.0b013e3282f36203. [DOI] [PubMed] [Google Scholar]
- 32.Tinghog G, Carlsson P, Synnerstad I, Rosdahl I. Societal cost of skin cancer in Sweden in 2005. Acta Derm Venereol. 2008;88(5):467–473. doi: 10.2340/00015555-0523. [DOI] [PubMed] [Google Scholar]
- 33.Souza R, Mattedi A, Rezende M, Correa M, Duarte E. Anestimate of the cost of treating mlanoma disease in the state of Sao Paulo-Brazil. An Bras Dermatol. 2009;84(3):237–243. doi: 10.1590/s0365-05962009000300004. [DOI] [PubMed] [Google Scholar]
- 34.Almazán-Fernández F, Serrano-Ortega S, Moreno-Villalonga J. Descriptive study of the costs of diagnosis and treatment of cutaneous melanoma. Actas Dermosifiliogr. 2009;100(9):785–791. [PubMed] [Google Scholar]
- 35.Morris S, Cox B, Bosanquet N. Cost of skin cancer in England. Eur J Health Econ. 2009;10(3):267–273. doi: 10.1007/s10198-008-0127-0. [DOI] [PubMed] [Google Scholar]
- 36.O’Dea D. The costs of skin cancer to New Zealand. Wellington, New Zealand: Wellington School of Medicine, University of Otago; 2009. [Google Scholar]
- 37.Leiter U, Marghoob AA, Lasithiotakis K, et al. Costs of the detection of metastases and follow-up examinations in cutaneous melanoma. Melanoma Res. 2009;19(1):50–57. doi: 10.1097/CMR.0b013e32831bc41c. [DOI] [PubMed] [Google Scholar]
- 38.Guy GP, Jr, Tai E, Richardson LC. Use of indoor tanning devices by high school students in the U.S., 2009. Prev Chronic Dis. 2011;8(5):A116. [PMC free article] [PubMed] [Google Scholar]
- 39.CDC. Use of indoor tanning devices by adults—U.S., 2010. MMWR Morb Mortal Wkly Rep. 2012;61(18):323–326. [PubMed] [Google Scholar]
- 40.Hirst N, Gordon L, Gies P, Green AC. Estimation of avoidable skin cancers and cost-savings to government associated with regulation of the solarium industry in Australia. Health Policy. 2009;89(3):303–311. doi: 10.1016/j.healthpol.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 41.Pollack LA, Li J, Berkowitz Z, et al. Melanoma survival in the U.S., 1992 to 2005. J Am Acad Dermatol. 2011;65(5S1):S78–S86. doi: 10.1016/j.jaad.2011.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tangka FK, Trogdon JG, Richardson LC, Howard D, Sabatino SA, Finkelstein EA. Cancer treatment cost in the U.S. Cancer. 2010;116(14):3477–3484. doi: 10.1002/cncr.25150. [DOI] [PubMed] [Google Scholar]
- 43.Richardson LC, Tangka FK. Ambulatory care for cancer in the U.S.: results from two national surveys comparing visits to physicians’ offices and hospital outpatient departments. J Natl Med Assoc. 2007;99(12):1350. [PMC free article] [PubMed] [Google Scholar]
- 44.Cartee TV, Kini SP, Chen SC. Melanoma reporting to central cancer registries by U.S. dermatologists: an analysis of the persistent knowledge and practice gap. J Am Acad Dermatol. 2011;65(5S1):S124–S132. doi: 10.1016/j.jaad.2011.05.032. [DOI] [PubMed] [Google Scholar]
- 45.Australian Cancer Network Melanoma Guidelines Revision Working Party. Clinical Practice Guidelines for the Management of Melanoma in Australia and New Zealand. Wellington, New Zealand: Cancer Council Australia and Australian Cancer Network, Sydney and New Zealand Guidleines Group; 2008. [Google Scholar]
- 46.U.S. Preventive Services Task Force. Screening for skin cancer. Rockville MD: Agency for Healthcare Research and Quality; 2009. [Google Scholar]
- 47.Freedberg KA, Geller AC, Miller DR, Lew RA, Koh HK. Screening for malignant melanoma: a cost-effectiveness analysis. J Am Acad Dermatol. 1999;41(5):738–745. doi: 10.1016/s0190-9622(99)70010-1. [DOI] [PubMed] [Google Scholar]
- 48.Girgis A, Clarke P, Burton R, Sanson-Fisher R. Screening for melanoma by primary health care physicians: a cost-effectiveness analysis. J Med Screen. 1996;3(1):47–53. doi: 10.1177/096914139600300112. [DOI] [PubMed] [Google Scholar]
- 49.Saraiya M, Glanz K, Briss P, et al. Interventions to prevent skin cancer by reducing exposure to ultraviolet radiation: a systematic review. Am J Prev Med. 2004;27(5):422–466. doi: 10.1016/j.amepre.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 50.Lin JS, Eder M, Weinmann S. Behavioral counseling to prevent skin cancer: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;154(3):190. doi: 10.7326/0003-4819-154-3-201102010-00009. [DOI] [PubMed] [Google Scholar]
- 51.Kyle JW, Hammitt JK, Lim HW, et al. Economic evaluation of the U.S. Environmental Protection Agency’s SunWise program: sun protection education for young children. Pediatrics. 2008;121(5):e1074–e1084. doi: 10.1542/peds.2007-1400. [DOI] [PubMed] [Google Scholar]
- 52.Shih S, Carter R, Sinclair C, Mihalopoulos C, Vos T. Economic evaluation of skin cancer prevention in Australia. Prev Med. 2009;49(5):449–453. doi: 10.1016/j.ypmed.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 53.Gilchrest B, Eller M, Geller A, Yaar M. The pathogenesis of melanoma induced by ultraviolet radiation. N Engl J Med. 1999;340(17):1341–1348. doi: 10.1056/NEJM199904293401707. [DOI] [PubMed] [Google Scholar]
- 54.Armstrong B, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B. 2001;63(1–3):8–18. doi: 10.1016/s1011-1344(01)00198-1. [DOI] [PubMed] [Google Scholar]
- 55.Lazovich D, Vogel R, Berwick M, Weinstock M, Anderson K, Warshaw E. Indoor tanning and risk of melanoma: a case-control study in a highly exposed population. Cancer Epidemiol Biomarkers Prev. 2010;19(6):1557. doi: 10.1158/1055-9965.EPI-09-1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.The International Agency for Research on Cancer Working Group on artificial ultraviolet light skin cancer. The association of use of sunbeds with cutaneous malignant melanoma and other skin cancers: a systematic review. Int J Cancer. 2007;120(5):1116–1122. doi: 10.1002/ijc.22453. [DOI] [PubMed] [Google Scholar]
- 57.Levine J, Sorace M, Spencer J, Siegel D. The indoor UV tanning industry: a review of skin cancer risk, health benefit claims, and regulation. J Am Acad Dermatol. 2005;53(6):1038–1044. doi: 10.1016/j.jaad.2005.07.066. [DOI] [PubMed] [Google Scholar]
- 58.Sinclair C. WHO. Artificial tanning sunbeds: risk and guidance. 2003 www.who.int/uv/publications/sunbedpubl/en/.
- 59.Cokkinides V, Weinstock M, Lazovich D, Ward E, Thun M. Indoor tanning use among adolescents in the U.S., 1998 to 2004. Cancer. 2009;115(1):190–198. doi: 10.1002/cncr.24010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.