Abstract
Context:
Research is limited regarding the effects of injury or surgery history and sex on the Functional Movement Screen (FMS) and Y Balance Test (YBT).
Objective:
To determine if injury or surgery history or sex affected results on the FMS and YBT.
Design:
Cross-sectional study.
Setting:
Athletic training facilities.
Patients or Other Participants:
A total of 200 National Collegiate Athletic Association Division I female (n = 92; age = 20.0 ± 1.4 years, body mass index = 22.8 ± 3.1 kg/m2) and male (n = 108; age = 20.0 ± 1.5 years, body mass index = 27.0 ± 4.6 kg/m2) athletes were screened; 170 completed the FMS, and 190 completed the YBT.
Intervention(s):
A self-reported questionnaire identified injury or surgery history and sex. The FMS assessed movement during the patterns of deep squat, hurdle step, in-line lunge, shoulder mobility, impingement-clearing test, straight-leg raise, trunk stability push-up, press-up clearing test, rotary stability, and posterior-rocking clearing test. The YBT assessed balance while participants reached in anterior, posteromedial, and posterolateral directions.
Main Outcome Measure(s):
The FMS composite score (CS; range, 0–21) and movement pattern score (range, 0–3), the YBT CS (% lower extremity length), and YBT anterior, posteromedial, and posterolateral asymmetry (difference between limbs in centimeters). Independent-samples t tests established differences in mean FMS CS, YBT CS, and YBT asymmetry. The Mann-Whitney U test identified differences in FMS movement patterns.
Results:
We found lower overall FMS CSs for the following injuries or surgeries: hip (injured = 12.7 ± 3.1, uninjured = 14.4 ± 2.3; P = .005), elbow (injured = 12.1 ± 2.8, uninjured = 14.3 ± 2.4; P = .02), and hand (injured = 12.3 ± 2.9, uninjured = 14.3 ± 2.3; P = .006) injuries and shoulder surgery (surgery = 12.0 ± 1.0, no surgery = 14.3 ± 2.4; P < .001). We observed worse FMS movement pattern performance for knee surgery (rotary stability: P = .03), hip injury (deep squat and hurdle: P < .042 for both), hip surgery (hurdle and lunge: P < .01 for both), shoulder injury (shoulder and hand injury: P < .02 for both), and shoulder surgery (shoulder: P < .02). We found better FMS movement pattern performance for trunk/back injury (deep squat: P = .02) and ankle injury (lunge: P = .01). Female athletes performed worse in FMS movement patterns for trunk (P < .001) and rotary (P = .01) stability but better in the lunge (P = .008), shoulder mobility (P < .001), and straight-leg raise (P < .001). Anterior asymmetry was greater for male athletes (P = .02).
Conclusions:
Injury history and sex affected FMS and YBT performance. Researchers should consider adjusting for confounders.
Key Words: athletic injuries, surgery history, sex differences
Key Points
Compared with male athletes, female athletes performed better on the movement patterns of the Functional Movement Screen (FMS) that involved flexibility and balance but worse on movement patterns that involved core strength.
Neither injury nor surgery history affected overall Y Balance Test (YBT) performance.
Whereas male and female athletes had similar overall FMS and YBT scores, they differed in performance of some movement patterns of FMS and YBT anterior-reach asymmetry.
In athletes with a history of injury or surgery, researchers should evaluate movement patterns on the FMS and YBT rather than considering only their overall scores.
Musculoskeletal injuries are an inherent risk of participation in athletes. Noncontact injuries represent approximately 20% of all injuries sustained during games and 40% of injuries sustained during practices.1 Beck and Wildermuth2 theorized that noncontact injuries occur because of a coordination failure involving a combination of high velocity and momentary loss of normal protective muscle support. Therefore, researchers3–5 have suggested that risk factors for noncontact injuries are modifiable when identified through movement patterns, right-to-left asymmetry, or balance abnormalities. The Functional Movement Screen (FMS; Functional Movement Systems Inc, Chatham, VA) and Y Balance Test (YBT; Move2Perform, Evansville, IN) are examples of screening tools that are being used clinically to assess injury risk based on abnormal movement patterns, asymmetry, and dynamic balance.
The FMS was developed to evaluate movement performance during 7 movement patterns: deep squat, hurdle step, in-line lunge, shoulder mobility, straight-leg raise, trunk stability push-up, and rotary stability.6 These movement patterns are scored from 0 to 3 based on performance with or without pain or compensation, and the scores are summed for a maximal composite score (CS) of 21. This tool has been suggested to predict injury when a CS of 14 or lower is obtained in male7 and female8 athletes and male military candidates.9 However, the sensitivity (0.91) and specificity (0.54) of a CS of 14 to determine injury risk from the first published report7 has not been reproduced in the subsequent 2 studies, with one indicating a sensitivity of 0.58 and a specificity of 0.748 and the other indicating that no receiver operating characteristic curve was able to maximize sensitivity and specificity.9 These challenges to the ability of the FMS CS to identify injury risk, coupled with well-documented sex differences10–14 and neuromuscular changes in movement patterns after injury,15–17 suggest that although FMS CSs may be similar between women and men or injured and uninjured individuals, these scores may be obtained with different individual movement patterns. Therefore, men and women and injured and uninjured individuals may not actually perform similarly on the FMS. To date, authors of 1 study18 have reported no sex differences in FMS performance in a young active population; however, they evaluated only the CS. Additionally, reports in the literature conflict as to the effect of previous injury on FMS performance, which may be related to methodologic differences. Schneiders et al18 found no difference in the FMS CS between recreational female and male athletes with and without injury in the previous 6 months; however, injury was not defined or identified. Peate et al19 reported that firefighters with a history of documented musculoskeletal injury were 68% more likely to have lower FMS scores than those without a history of injury.
The YBT, which is a commercially available, highly reliable tool,20 was developed to standardize the modified Star Excursion Balance Test (SEBT). The SEBT was modified to improve efficiency in assessing dynamic balance and includes only 3 (anterior [ANT], posterolateral [PL], and posteromedial [PM]) of the original 8 SEBT reach directions.21 The YBT CS is calculated by summing the 3 reach directions and normalizing to lower extremity length, whereas asymmetry is the difference between right and left limb reach. Greater than 4 cm of ANT asymmetry during the SEBT has been suggested to predict which individuals are at risk of lower extremity injury; however, when evaluating the CS, Plisky et al22 found that only female athletes with a composite reach of less than 94% of limb length were at greater risk of injury. Recent evidence23 has shown that sensitivity (100%) and specificity (71.1%) were maximized using 89.6% of the YBT CS to predict injury in football players; scores of less than 89.6% were associated with an injury risk that was 3.5 times greater. These results may indicate that sex differences exist in the prediction of injury risk based on dynamic balance performance as assessed by the YBT. Additionally, Steffen et al24 reported that adherence to a neuromuscular-training program improved performance on the SEBT and decreased the injury risk in female youth soccer players.
Gribble and Hertel25 reported differences among raw reach distances. Male participants reached farther than female participants in all 8 directions of the SEBT, but when the distances were normalized to leg length, the sex differences disappeared.25 Additional data suggested that men perform better on normalized posterior reach directions, but when all 3 reach directions were averaged, no sex differences existed.26 Gorman et al27 showed that men performed better in normalized reach distances; however, Gribble et al28 reported that women performed better in normalized reach distances. Discrepancies in the effect of sex on performance of dynamic balance may be due to small sample sizes, as the largest of the aforementioned studies included just 32 participants,26 or may be due to muscle-activation differences between women and men. Whereas researchers have documented that individuals with patellofemoral pain syndrome29 and chronic ankle instability30–32 perform worse on the SEBT, additional injuries or surgeries also alter normal neuromuscular control15–17; thus, individuals with histories of pathologic conditions that have not yet been studied may also have limitations in dynamic balance.
To date, gaps are apparent in the literature regarding the effect of injury history and sex on FMS and YBT performance in the collegiate population. Furthermore, if injury or surgery history and sex affect FMS and YBT performance in a large collegiate cohort, investigators may be able to identify an appropriate algorithm to more accurately use the outcomes of the FMS and YBT to predict injury risk in athletes. Therefore, the purpose of our study was to evaluate the effect of potential preexisting confounders of injury or surgery history and sex on performance of the FMS and the YBT in a large sample of National Collegiate Athletic Association Division I athletes. Our first hypothesis was that the sample of Division I female athletes would perform worse than the sample of Division I male athletes in FMS CS, FMS movement patterns, and YBT CS and demonstrate greater asymmetry in each of the 3 reach directions. Our second hypothesis was that the Division I participants with a history of lower extremity injury or surgery would perform worse on FMS CS and movement patterns of deep squat, hurdle step, in-line lunge, straight-leg raise, trunk stability, and rotary stability. Our third hypothesis was that the Division I participants with a history of upper extremity injury or surgery would perform worse on FMS CS and movement patterns of shoulder mobility, trunk stability, and rotary stability. Our fourth hypothesis was that the Division I participants with a history of lower extremity injury would perform worse on YBT CS and demonstrate greater asymmetry in each of the 3 reach directions.
METHODS
Research Design
This study was a cross-sectional design. The independent variables were injury or surgery history and sex. The dependent variables were FMS CS; FMS movement pattern score; YBT CS; and YBT ANT, PM, and PL asymmetry.
Participants
Two hundred Division I athletes (92 women: age = 20.0 ± 1.4 years, body mass index = 22.8 ± 3.1 kg/m2; 108 men: age = 20 ± 1.5 years, body mass index = 27.0 ± 4.6 kg/m2) were screened for study participation during preseason physical examinations. Individuals were excluded if they had a musculoskeletal injury at the time of the study that limited participation in workouts or if they were not wearing proper attire to perform the FMS or YBT (ie, not wearing shorts for FMS and YBT performance or sneakers for FMS performance). To be included in this study, participants had to be Division I athletes at the time of the study and between the ages of 18 and 24 years. All participants provided written informed consent, and the study was approved by the Institutional Review Boards at Northern Arizona University and Daemen College.
Health History Questionnaire
A health history questionnaire was used to assess self-reported history of injury and surgery (Figure 1). For this study, we defined injury as having experienced a previous injury and surgery as having undergone a previous surgery. Thus, for data reduction, athletes were grouped based on whether they indicated having had or not having had injuries or surgeries. For the injury and surgery history questionnaire, the participants were asked about each joint individually, except that the trunk and back were grouped together, to indicate if they had experienced injuries or surgeries. So that we could compare sexes, participants also were instructed to indicate sex.
Figure 1.
Sample of health history questionnaire used to assess self-reported injury history in participants.
The Functional Movement Screen
The FMS was used to assess 7 movement patterns (deep squat, hurdle step, in-line lunge, shoulder mobility, straight-leg raise, trunk stability push-up, and rotary stability) and 3 clearing tests (impingement, press-up, and posterior rocking).6 For scoring, we used the 4-point ordinal scale from 0 to 3 for each movement pattern, with a maximal score of 21 points. A score of 3 represented the ability to perform the functional movement pattern without compensations.6 A score of 2 was assigned if the participant performed the movement with compensations.6 A score of 1 was assigned if the participant was unable to perform the movement according to published guidelines, and a score of 0 was reserved for participants who had pain with the movement or presented with pain while performing a clearing test.6 The FMS has high interrater and intrarater reliability.33
The Y Balance Test
The YBT was used to assess dynamic balance in 3 reach directions: ANT, PM, and PL. It has been demonstrated to have high interrater and intrarater reliability.20
Procedures
During the preseason physical examinations, athletes were evaluated by the team physician and athletic training staff at the university. During this process, volunteers were recruited for study participation. They received an explanation of the study procedures and the benefits and risks of participation and could ask questions about the study. All volunteers completed health history questionnaires. The researchers then screened all volunteers meeting inclusion and exclusion criteria in performance of the FMS and YBT. Screens were performed in a convenience order, and participants were given adequate rest to account for fatigue. We performed screening with the FMS, and the YBT was performed according to published guidelines.6,34
The FMS was administered by a researcher (N.J.C. or C.A.S.) involved in a previous reliability study.33 All participants completed the FMS in the following order: deep squat, hurdle step, in-line lunge, shoulder mobility, impingement-clearing test, straight-leg raise, trunk stability push-up, press-up clearing test, rotary stability, and posterior-rocking clearing test. Participants performed all movement patterns in self-selected athletic shoes. They could perform each of the 7 functional movements a maximum of 3 times, and the best score obtained for each movement was recorded for data analysis. Each participant performed the clearing tests only once. Data from the 7 trials were summed to create the FMS CS; for movements that were scored on both the right and left limbs, the lower score was used to calculate the CS. Individual FMS movement patterns were analyzed using the raw ordinal-scale data obtained from each fundamental movement.
The YBT was assessed by a researcher (N.J.C., C.A.S., or M.W.) certified in YBT administration.35 Before screening, participants removed their socks and shoes, watched a short video on how to perform the YBT, and were allowed 4 to 6 practice trials on each limb in each of the 3 reach directions. After the practice trials, we measured lower extremity length from the inferior border of the anterior-superior iliac spine to the inferior border of the medial malleolus. Participants then performed dynamic balance on both the right and left lower extremities while they reached in the ANT, PM, and PL directions with the contralateral limb. Three successful reaches were performed; the maximal reach distance in each direction was used for data analysis. Asymmetry in right or left reach distance was determined by calculating the absolute difference in reach difference between the maximum right and left extremities in the ANT, PM, and PL directions. Values were expressed in centimeters. The YBT CS was determined by summing the average of the maximum right and left reach distances in each direction, dividing by 3 times the lower extremity length, and multiplying by 100 to obtain a percentage.
Data Processing
For joint injury or surgery data, participants were grouped based on each joint to determine if injury or surgery history affected FMS and YBT performance. Relationships were assessed between injury or surgery history in the lower extremity and trunk and FMS CS, deep squat, hurdle step, in-line lunge, straight-leg raise, trunk stability, rotary stability, YBT CS, and YBT asymmetries. Relationships were assessed between injury or surgery history in the upper extremity and FMS CS, shoulder mobility, trunk stability, and rotary stability.
Statistical Analysis
We used independent-samples t tests to analyze mean FMS CS, YBT CS, and YBT asymmetry between participants with and without a history of injury or surgery. The Mann-Whitney U was used to analyze mean ranks of the FMS movement patterns. We calculated 95% confidence intervals (CIs) for participants reporting no history of injury, and the aggregate data of participants with a history of injury to the lower extremity, trunk/back, and upper extremity were plotted against the data of the uninjured participants for FMS CS, YBT CS, and YBT asymmetry. We used the minimal clinically important difference (MCID) to determine the smallest measurable difference in performance of FMS CS and YBT CS. We calculated the MCID using a distribution-based method of 0.5 standard deviation.36
Data were separated by sex for comparison of FMS and YBT performance. We used independent-samples t tests to compare mean FMS CS, YBT CS, and YBT asymmetry between sexes. The Mann-Whitney U was calculated to compare mean ranks of the FMS movement patterns. We calculated 95% CIs to analyze FMS CS, YBT CS, and YBT asymmetry between men and women.
Data were processed with SPSS software (version 20; IBM Corp, Armonk, NY), with an a priori α level of .05 indicating a difference between groups.
RESULTS
A total of 170 FMS and 190 YBT screens were completed (Table 1). The association between previous injury or surgery with FMS and YBT varied by individual joint (Table 2). Athletes with a history of hip (t168 = −2.880, P = .005), hand (t168 = −2.806, P = .006), or elbow (t168 = −2.309, P = .02) injury or shoulder surgery (t7.366 = −6.132, P < .001) performed worse on the FMS CS (Table 2). The MCID for FMS CS was 1.25. Analysis of individual FMS movement patterns revealed that participants with ankle injuries had better in-line lunge (P = .01; U = 2962; 95% CI for mean = 2.15, 2.38 [injured] versus 1.92, 2.18 [uninjured]), those with knee surgeries had worse rotary stability (P = 0.033; U = 1224; 95% CI for mean = 1.45, 2.05 [injured] versus 1.95, 2.10 [uninjured]), those with hip injuries performed worse on deep squat (P = .008; U = 899; 95% CI for mean = 0.92, 1.75 [injured] versus 1.68, 1.89 [uninjured]) and hurdle step (P = .04; U = 1117; 95% CI for mean = 1.58, 2.09 [injured] versus 1.97, 2.09 [uninjured]), those with hip surgeries had worse hurdle step (P = .002; U = 81.5; 95% CI for mean = −0.10, 2.77 [injured] versus 2.03, 2.15 [uninjured]) and in-line lunge (P = .01; U = 87.5; 95% CI for mean = −0.10, 2.77 [injured] versus 2.02, 2.19 [uninjured]), those with trunk/back injuries had better deep-squat performance (P = .02; U = 1695; 95% CI for mean = 1.74, 2.20 [injured] versus 1.56, 1.80 [uninjured]), those with shoulder injuries had worse shoulder mobility (P = .002; U = 1374.5; 95% CI for mean = 1.47, 2.25 [injured] versus 2.30, 2.57 [uninjured]), those with shoulder surgeries had worse shoulder mobility (P = .001; U = 84; 95% CI for mean = −0.24, 1.84 [injured] versus 2.26, 2.51 [uninjured]), and those with hand injuries had worse shoulder mobility (P = .02; U = 605; 95% CI for mean = 1.08, 2.42 [injured] versus 2.25, 2.51 [uninjured]) than participants without a history of injury or surgery. We found no differences in YBT CS or asymmetries when evaluating performance based on a history of lower extremity injury or surgery in individual joints (Table 2). The MCID for the YBT CS was 3.5%.
Table 1.
Functional Movement Screen and Y Balance Test Composite Scores Classified by Sport and Sex
| Sport |
Functional Movement Screen Composite Scorea |
Y Balance Test Composite Scoreb |
||||||
| Women |
Men |
Women |
Men |
|||||
| No. |
Mean ± SD |
No. |
Mean ± SD |
No. |
Mean ± SD |
No. |
Mean ± SD |
|
| Basketball | 2 | 14 ± 3 | 7 | 14 ± 2 | 2 | 98 ± 0 | 9 | 98 ± 6 |
| Cheer and dance | 2 | 14 ± 1 | NA | NA | 4 | 97 ± 8 | NA | NA |
| Cross country | 17 | 15 ± 2 | 11 | 14 ± 3 | 17 | 99 ± 5 | 13 | 101 ± 12 |
| Football | NA | NA | 61 | 14 ± 3 | NA | NA | 69 | 102 ± 7 |
| Golf | 1 | 15 ± 0 | NA | NA | 3 | 97 ± 3 | NA | NA |
| Soccer | 29 | 15 ± 2 | NA | NA | 28 | 102 ± 6 | NA | NA |
| Swimming and diving | 15 | 14 ± 2 | NA | NA | 17 | 102 ± 7 | NA | NA |
| Tennis | 4 | 12 ± 4 | 5 | 15 ± 2 | 5 | 99 ± 6 | 5 | 107 ± 5 |
| Track and field | 4 | 13 ± 5 | 5 | 15 ± 2 | 3 | 92 ± 14 | 7 | 106 ± 6 |
| Volleyball | 7 | 13 ± 2 | NA | NA | 8 | 99 ± 8 | NA | NA |
| Total | 81 | 89 | 87 | 103 | ||||
Abbreviation: NA, not applicable (sport not offered at university).
Functional Movement Screen (Functional Movement Systems, Inc, Chatham, VA) maximum = 21.
Y Balance Test (Move2Perform, Evansville, IN) is normalized to % lower extremity length.
Table 2A.
Functional Movement Screen and Y Balance Test Performance Classified by Injury History
| Measure |
Injury History |
|||||||
| Ankle |
Knee |
Hip |
Trunk |
Shoulderb |
Elbowb |
Wristb |
Handb |
|
| Functional Movement Screen/Y Balance Test, No. of screened athletes with previous injuriesa | 90/100 | 59/64 | 18/18 | 32/35 | 29/NA | 7/NA | 25/NA | 12/NA |
| Functional Movement Screen composite score | ||||||||
| Previous injury, mean ± SD | 14.2 ± 2.4 | 13.9 ± 2.3 | 12.7 ± 3.1 | 14.1 ± 2.4 | 13.5 ± 2.6 | 12.1 ± 2.8 | 14.1 ± 2.2 | 12.3 ± 2.9 |
| No previous injury, mean ± SD | 14.2 ± 2.5 | 14.4 ± 2.5 | 14.4 ± 2.3 | 14.2 ± 2.4 | 14.3 ± 2.4 | 14.3 ± 2.4 | 14.2 ± 2.5 | 14.3 ± 2.3 |
| P Value | .88 | .20 | .005c | .74 | .10 | .02c | .80 | .006c |
| t Value | −0.156 | −1.292 | −2.880 | −0.0339 | −1.655 | −2.309 | −0.253 | −2.806 |
| 95% Confidence interval of difference | −0.798, 0.681 | −1.277, 0.267 | −2.880, −0.537 | −1.106, 0.782 | −1.790, 0.157 | −3.968, −0.310 | −1.176, 0.908 | −3.411, −0.594 |
| Y Balance Test composite score | ||||||||
| Previous injury, mean ± SD, % | 101 ± 8 | 101 ± 7 | 100 ± 10 | 102 ± 10 | NA | NA | NA | NA |
| No previous injury, mean ± SD, % | 101 ± 8 | 101 ± 8 | 101 ± 8 | 101 ± 7 | NA | NA | NA | NA |
| P Value | .68 | .49 | .53 | .37 | ||||
| t Value | 0.416 | 0.695 | −0.635 | 0.902 | ||||
| 95% Confidence interval of difference | −0.018, 0.027 | −0.015, 0.032 | −0.051, 0.026 | −0.018, 0.042 | ||||
| Anterior reach asymmetry during the Y Balance Test | ||||||||
| Previous injury, mean ± SD, cm | 4.5 ± 8.9 | 5.1 ± 11.6 | 3.1 ± 2.3 | 6.3 ± 14.3 | NA | NA | NA | NA |
| No previous injury, mean ± SD, cm | 4.2 ± 8.5 | 4.0 ± 6.9 | 4.5 ± 9.1 | 3.9 ± 6.9 | NA | NA | NA | NA |
| P Value | .78 | .40 | .51 | .34 | ||||
| t Value | 0.274 | 0.841 | −0.616 | 0.976 | ||||
| 95% Confidence interval of difference | −2.162, 2.860 | −1.512, 3.777 | −5.701, 2.852 | −2.593, 7.421 | ||||
| Posteromedial reach asymmetry during the Y Balance Test | ||||||||
| Previous injury, mean ± SD, cm | 4.4 ± 9.6 | 3.1 ± 2.6 | 4.3 ± 2.9 | 5.8 ± 15.6 | NA | NA | NA | NA |
| No previous injury, mean ± SD, cm | 3.5 ± 3.2 | 4.4 ± 8.7 | 3.9 ± 7.6 | 3.5 ± 3.2 | NA | NA | NA | NA |
| P Value | .39 | .24 | .83 | .40 | ||||
| t Value | 0.857 | −1.171 | 0.211 | 0.864 | ||||
| 95% Confidence interval of difference | −1.181, 2.994 | −3.059, 0.895 | −3.185, 3.947 | −3.095, 7.675 | ||||
| Posterolateral reach asymmetry during the Y Balance Test | ||||||||
| Previous injury, mean ± SD, cm | 3.6 ± 2.8 | 3.9 ± 3.1 | 3.9 ± 3.9 | 3.5 ± 2.7 | NA | NA | NA | NA |
| No previous injury, mean ± SD, cm | 3.7 ± 2.7 | 3.5 ± 2.6 | 3.6 ± 2.6 | 3.7 ± 2.8 | NA | NA | NA | NA |
| P Value | .91 | .40 | .78 | .74 | ||||
| t Value | −0.116 | 0.851 | 0.290 | −0.335 | ||||
| 95% Confidence interval of difference | −0.842, 0.749 | −0.514, 1.287 | −1.695, 2.240 | −1.198, 0.850 | ||||
Abbreviation: NA, not analyzed.
Functional Movement Screen (Functional Movement Systems, Inc, Chatham, VA); Y Balance Test (Move2Perform, Evansville, IN).
Upper extremity injuries were not assessed for differences with performance on the Y Balance Test composite score or anterior, posteromedial, or posterolateral reach asymmetry during the Y Balance Test because this study focused on the lower quarter Y Balance Test.
Indicates difference.
Table 3.
Differences in Functional Movement Screen and Y Balance Test Performance Classified by Sex
| Instrument |
Sex, Mean ± SD |
P Value |
95% Confidence Interval |
|
| Women |
Men |
|||
| Functional Movement Screen composite scorea | 14.3 ± 2.4 | 14.0 ± 2.5 | .37 | −0.404, 1.091 |
| Y Balance Test composite score, % lower extremity lengthb | 100 ± 6 | 102 ± 8 | .052 | −0.0412, 0.0002 |
Functional Movement Screen (Functional Movement Systems, Inc, Chatham, VA) composite score ranges from 0 to 21.
Y Balance Test (Move2Perform, Evansville, IN).
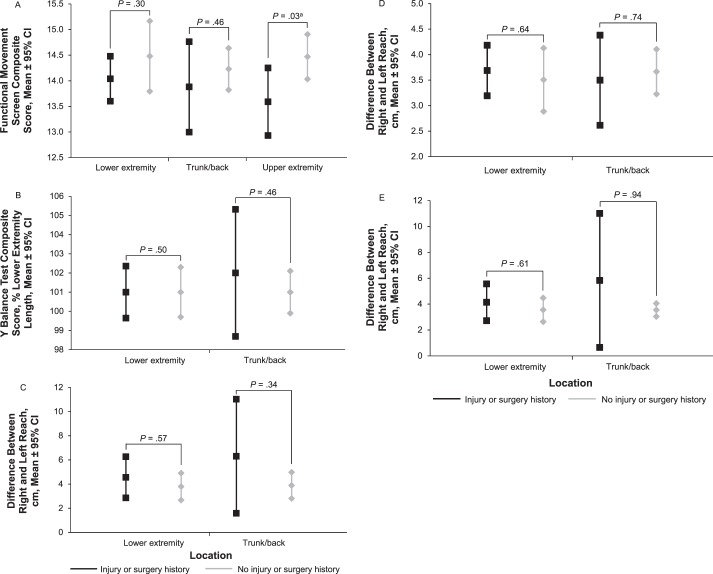
When individual joint injuries or surgeries were grouped as lower extremity, trunk/back, and upper extremity, we found no differences in FMS CS; YBT CS; or YBT ANT, PM, or PL asymmetry among participants with a history of lower extremity injury or surgery; however, a history of trunk/back injury contributed to larger asymmetry ranges in both the ANT and PM reaches (Figure 2). Participants with a history of upper extremity injury or surgery performed worse on the FMS CS (Figure 2).
Figure 2.
Functional Movement Screen (FMS) and Y Balance Test (YBT) performance based on injury or surgery history grouped as lower extremity, trunk/back, and upper extremity. A, FMS composite score. B, YBT composite score. C, YBT anterior reach asymmetry. D, YBT posterolateral reach asymmetry. E, YBT posteromedial reach asymmetry. Groupings represent all injuries or surgeries to the respective area. a Indicates difference. Abbreviation: CI, confidence interval.
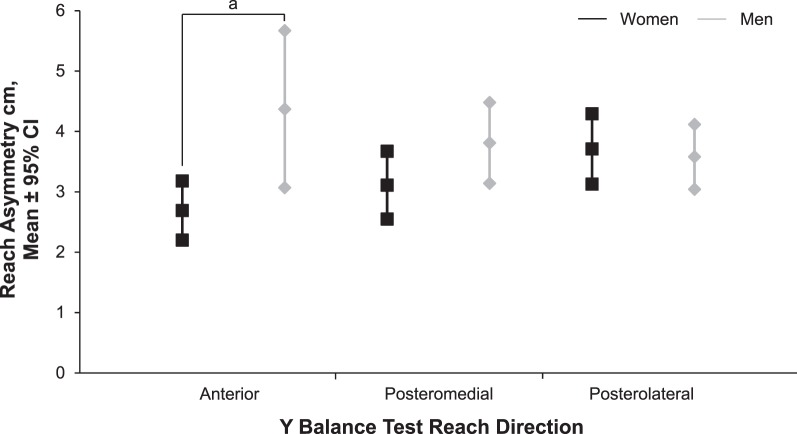
We found no differences between female and male athletes in FMS CS (t168 = 0.907, P = .37; Table 3). Female athletes performed worse than male athletes in trunk stability (P < .001; U = 2438; 95% CI for mean = 1.54, 1.99 [women] versus 2.18, 2.54 [men]) and rotary stability (P = .01; U = 3055.5; 95% CI for mean = 1.71, 1.92 [women] versus 1.87, 2.11 [men]); however, female athletes performed better than male athletes on in-line lunge (P = .008; U = 2928.5; 95% CI for mean = 2.03, 2.27 [women] versus 1.75, 2.03 [men]), shoulder mobility (P < .001; U = 2429.5; 95% CI for mean = 2.30, 2.67 [women] versus 1.81, 2.19 [men]), and straight-leg raise (P < .001; U = 2059; 95% CI for mean = 2.33, 2.68 [women] versus 1.87, 2.13 [men]). We found no differences in performance on the deep squat (P = .10; U = 3130; 95% CI for mean = 1.51, 1.80 [women] versus 1.66, 1.96 [men]) or hurdle step (P = .87; U = 3571; 95% CI for mean = 1.89, 2.06 [women] versus 1.87, 2.04 [men]) between female and male athletes. Their YBT CSs were similar (t188 = −1.920, P = .052; Table 3). However, female athletes demonstrated less asymmetry than male athletes in YBT ANT (t188 = −1.920, P = .02), whereas asymmetry was similar in YBT PM (t188 = −1.529, P = .13) and YBT PL (t188 = 0.322, P = .75; Figure 3).
Table 2B.
Functional Movement Screen and Y Balance Test Performance Classified by Surgery History
| Measure |
Surgery History |
|||||||
| Ankle |
Knee |
Hip |
Trunka |
Shoulderb |
Elbowb |
Wristb |
Handb |
|
| Functional Movement Screen/Y Balance Test, No. of screened athletes with previous surgeries | 4/4 | 20/22 | 3/3 | 0/1 | 5/NA | 3/NA | 4/NA | 4/NA |
| Functional Movement Screen composite score | ||||||||
| Previous injury, mean ± SD | 14.3 ± 2.9 | 14.1 ± 1.7 | 12.0 ± 2.6 | NA | 12.0 ± 1.0 | 13.3 ± 2.3 | 15.8 ± 1.7 | 12.5 ± 3.7 |
| No previous injury, mean ± SD | 14.2 ± 2.4 | 14.2 ± 2.5 | 14.2 ± 0.2 | NA | 14.3 ± 2.4 | 14.2 ± 2.4 | 14.2 ± 2.4 | 14.2 ± 2.4 |
| P Value | .96 | .78 | .12 | NA | <.001c | .54 | .20 | .16 |
| t Value | 0.046 | −0.281 | −1.584 | NA | −6.132 | −0.618 | 1.298 | −1.415 |
| 95% Confidence interval of difference | −2.378, 2.493 | −1.309, 0.982 | −5.017, 0.549 | NA | −3.124, −1.398 | −3.677, 1.924 | −0.830, 4.017 | −4.156, 0.686 |
| Y Balance Test composite score | ||||||||
| Previous injury, mean ± SD, % | 96 ± 4 | 100 ± 8 | 95 ± 3 | NA | NA | NA | NA | NA |
| No previous injury, mean ± SD, % | 101 ± 8 | 101 ± 8 | 101 ± 1 | NA | NA | NA | NA | NA |
| P Value | .20 | .56 | .20 | NA | NA | NA | NA | NA |
| t Value | −1.286 | −0.586 | −1.285 | NA | NA | NA | NA | NA |
| 95% Confidence interval of difference | −0.129, 0.272 | −0.046, 0.025 | −0.149, 0.031 | NA | NA | NA | NA | NA |
| Anterior reach asymmetry during the Y Balance Test | ||||||||
| Previous injury, mean ± SD, cm | 2.1 ± 1.4 | 6.7 ± 15.8 | 2.5 ± 3.5 | NA | NA | NA | NA | NA |
| No previous injury, mean ± SD, cm | 4.4 ± 8.8 | 4.3 ± 7.4 | 4.4 ± 8.8 | NA | NA | NA | NA | NA |
| P Value | .61 | .44 | .71 | NA | NA | NA | NA | NA |
| t Value | −0.512 | 0.790 | −0.368 | NA | NA | NA | NA | NA |
| 95% Confidence interval of difference | −10.995, 6.460 | −4.376, 9.765 | −11.929, −8.180 | NA | NA | NA | NA | NA |
| Posteromedial reach asymmetry during the Y Balance Test | ||||||||
| Previous injury, mean ± SD, cm | 1.6 ± 0.5 | 3.2 ± 2.6 | 3.0 ± 1.3 | NA | NA | NA | NA | NA |
| No previous injury, mean ± SD, cm | 4.0 ± 7.3 | 4.1 ± 7.7 | 4.0 ± 7.3 | NA | NA | NA | NA | NA |
| P Value | .52 | .61 | .82 | NA | NA | NA | NA | NA |
| t Value | −0.648 | −0.517 | −0.230 | NA | NA | NA | NA | NA |
| 95% Confidence interval of difference | −9.653, 4.881 | −4.117, 2.407 | −9.353, 7.401 | NA | NA | NA | NA | NA |
| Posterolateral reach asymmetry during the Y Balance Test | ||||||||
| Previous injury, mean ± SD, cm | 2.4 ± 1.9 | 3.1 ± 3.0 | 2.8 ± 1.8 | NA | NA | NA | NA | NA |
| No previous injury, mean ± SD, cm | 3.4 ± 2.8 | 3.7 ± 2.7 | 3.7 ± 2.8 | NA | NA | NA | NA | NA |
| P Value | .36 | .34 | .61 | NA | NA | NA | NA | NA |
| t Value | −0.925 | −0.952 | −0.509 | NA | NA | NA | NA | NA |
| 95% Confidence interval of difference | −4.055, 1.466 | −1.836, 0.641 | −4.006, 2.362 | NA | NA | NA | NA | NA |
Abbreviation: NA, not analyzed.
Trunk injuries were not assessed for differences with performance on Functional Movement Screen (Functional Movement Systems, Inc, Chatham, VA) composite score; Y Balance Test (Move2Perform, Evansville, IN) composite score; or anterior, posteromedial, or posterolateral reach asymmetry during the Y Balance Test because no previous surgeries were reported.
Upper extremity injuries were not assessed for differences with performance on the Y Balance Test composite score or anterior, posteromedial, or posterolateral reach asymmetry during the Y Balance Test because this study focused on the lower quarter Y Balance Test.
Indicates difference.
Figure 3.
Y Balance Test anterior, posteromedial, and posterolateral reach asymmetry between men and women. a Indicates difference between men and women. Abbreviation: CI, confidence interval.
DISCUSSION
The FMS and the YBT are being used clinically to identify athletes at risk of injury7–9,19,22,23 and subsequently to administer programs to decrease injury risk37; however, differences exist in movement patterns and balance between athletes who have and have not been injured and between female and male athletes.10–17,21,26–30,38–41 Therefore, the purpose of our study was to evaluate the effect of potential preexisting confounders of sex and injury or surgery history on performance of the FMS and the YBT in a large sample of Division I athletes.
We found no difference between female and male athletes in FMS CS; however, female and male athletes performed differently in all movement patterns of the FMS except for the deep squat and hurdle step. Researchers6 have suggested that the deep squat is a movement needed in most sports. If true, this may be why female and male Division I athletes appear to perform this task with similar scores. Division I female and male athletes also perform similarly in the hurdle step, which researchers have suggested requires coordination and stability between the hips and torso along with dynamic balance,6 and the YBT, which requires dynamic stability during contralateral limb reaching. These findings indicate that the female and male athletes in our study had similar dynamic balance. Researchers25,26 have demonstrated no difference between sexes in performance on the YBT with small sample sizes. Our study is the largest reported to date with adequate power (1.0), minimizing the risk of type II error. Our findings, coupled with those reported in smaller previous studies, show that sex differences likely do not exist in performance of the YBT when evaluating the CS.
Whereas we hypothesized that Division I female athletes would perform worse than Division I male athletes in the FMS CS and movement patterns, we found that they performed worse on tasks that may involve greater core coordination with an appropriate transfer of energy through the trunk (ie, trunk stability and rotary stability) but better on tasks that involve greater flexibility and joint mobility (ie, in-line lunge, shoulder mobility, and straight-leg raise). These findings may indicate that Division I female athletes have an increased risk of injury, as decreased core stability has been hypothesized to increase injury risk.42 Our results suggest that, although female and male Division I athletes performed similarly on the overall FMS score, FMS CS was not achieved in the same manner; this is similar to findings reported in recreational athletes.18 Therefore, future researchers should evaluate if sex biases the association between FMS CS and injury. They also need to observe differences in individual movement-pattern performance to truly determine individualized injury risk, as Kazman et al43 recently proposed that the FMS CS lacks internal consistency and validity. Additionally, assessing differences between women and men and specific FMS movement patterns may aid in structuring any subsequent training on an individualized, sex-specific basis.
Evaluation of sex as a confounder also may be necessary when assessing performance on the YBT, as Division I male athletes had greater ANT asymmetry than Division I female athletes (Figure 3). This finding directly contradicted our hypothesis that female athletes would demonstrate greater reach asymmetry than male athletes. Based on previous research,22 this may suggest that the Division I male athletes in our study could be at risk of lower extremity injury, as they had more than 4 cm of ANT asymmetry. However, the study design did not enable us to determine why men in our study had greater ANT asymmetry. Investigators44 have indicated that collegiate athletes participating in soccer, which requires reaching outside the base of support during functional activities, performed better in dynamic balance than athletes involved in basketball, which primarily stresses the sensorimotor system within the base of support. Perhaps participation in sport modulated symmetric performance in the ANT task in our study, as most of the male athletes whom we sampled were football players. In addition, the YBT possibly challenged the sensorimotor system more in the football players in our study and, thus, was associated with greater ANT asymmetry in male than female athletes. This may suggest that, when football players are in positions that are outside their base of support, they may have altered neuromuscular responses and, therefore, a greater risk for injury. Sport-related neuromuscular factors may influence performance on the SEBT; collegiate female soccer players reached farther than female nonsoccer recreational athletes in the ANT and posterior reach directions.45
In previous studies,7–9 the FMS has been used to predict injury. However, injury history, which has been suggested as the best predictor of injury risk,46,47 was not assessed in these studies. As such, poor performance on the FMS may actually reflect injury history rather than predict future injury risk. To date, athletes who score less than 14 on the FMS have experienced a higher proportion of injuries.7–9 Our results demonstrated that Division I athletes with a history of hip, elbow, or hand injury or shoulder surgery performed worse (FMS CS = 12.7, 12.1, 12.3, and 12.0, respectively) than athletes without a history of injury or surgery (FMS CS = 14.4, 14.3, 14.3, and 14.3, respectively; Table 2). If we did not account for injury or surgery history in these athletes, their FMS CSs would suggest, based on the literature,7–9 that they were at risk of future injury. However, they quite possibly are at risk for future injury based on their history, or the FMS CS may actually be detecting previous injury rather than predicting future injury risk. Therefore, clinicians need to look not only at scores on screening tools, such as the FMS and YBT, when evaluating injury risk but also need to assess previous history. Previous history may provide a more accurate predictor of performance on these screens and subsequent injury risk than assuming that, because an athlete performs poorly on these screens, he or she is at greater risk for injury.
Our results are similar to those of Peate et al,19 who reported that firefighters with previous injury were more likely to perform worse on the FMS, but contradicts the findings of Schneiders et al,18 who did not observe a difference in FMS performance by those who had sustained an injury in the 6 months before the study. Perhaps evaluating overall injury history rather than only injuries that have occurred recently is important. Discerning whether the risk of future injury is identifiable based on FMS performance or injury history is impossible if researchers have not assessed and accounted for injury history.
In addition, participants with a self-reported history of lower extremity injury or surgery performed worse on deep squat, hurdle step, in-line lunge, and rotary stability depending on the body part that was injured, whereas participants with a self-reported history of upper extremity injury or surgery performed worse on shoulder mobility. Interestingly, participants who self-reported a trunk/back injury performed better on the deep squat, and participants who self-reported an ankle injury performed better on the in-line lunge. Although we could not determine why participants with trunk/back and ankle injuries performed better on the deep squat and in-line lunge, respectively, this finding may reflect improved neuromuscular control or improved range of motion gained through effective postinjury rehabilitation. Inani and Selkar48 reported that patients with nonspecific low back pain had improved functional status after 3 months of core-stabilization exercises; thus, our participants may have had improved core stability, which was reflected in improved performance in the deep squat. Gutierrez et al15 found that individuals with chronic ankle instability demonstrated increased preparatory and reactive activation of the peroneal muscles in response to a supination event, suggesting an enhanced response to promote dynamic restraint. Macklin et al49 demonstrated that runners with ankle-joint equinus had improved ankle-joint dorsiflexion after a triceps surae stretching program. Perhaps our participants had enhanced dynamic restraint or ankle range of motion and, therefore, were able to perform better in the in-line lunge. Specific joint injuries or surgeries resulted in increased or decreased performance on select FMS movement patterns, again suggesting that performance on the FMS may actually reflect injury history rather than predict future injury risk.
Although we did not find that injury or surgery history influenced performance on the YBT, these results are consistent with a recent report that injury history did not influence YBT performance in collegiate football players.23 Whereas injury or surgery history did not affect performance on the YBT or contribute to reach asymmetries, the 95% CIs indicate that participants with trunk/back injuries had greater variability in YBT reach asymmetry than participants without trunk/back injuries (Figure 2). The combination of reported altered neuromuscular control of the trunk as a predictor of knee-injury risk50 and our findings of greater variability in YBT performance may suggest that athletes with a history of trunk/back injury are at greater risk for lower extremity injury. Furthermore, the large deviations seen in YBT performance and reach asymmetry in participants with a history of trunk/back injury demonstrate that, when individuals are grouped, potentially meaningful asymmetric movement patterns may be lost. Therefore, individual injury histories should be examined before assuming that injury risk is similar based solely on scores obtained from the FMS and YBT.
We are the first to assess injury history and sex differences in the FMS CS and individual movement-pattern scores and YBT CS and reach asymmetries in a large sample of Division I collegiate athletes. Whereas our sample represented the percentage of athletes who participate in each sport relative to the total number of athletes in a Division I institution, most of our male participants were football players; this may have limited our findings, as the neuromuscular system is developed through previous experiences. Injury history was self-reported; we possibly did not have a complete picture of each athlete's previous injuries. However, self-report is the most common method of injury reporting used during collegiate preparticipation examinations. Additionally, although we asked about injury to each joint, we did not assess concussion history and did not ask about the types or numbers of previous injuries. We aimed to assess if participants had previous injuries or surgery; we did not classify injury or surgery based on type of injury or surgery type or time since injury or surgery had occurred. Injury severity, time since previous injury or surgery, or rehabilitation after injury or surgery may have affected findings. Future researchers should consider these factors.
CONCLUSIONS
Whereas Division I female and male athletes may perform similarly in FMS and YBT CS, differences appear in some FMS movement patterns and YBT ANT asymmetry. Female athletes performed better on FMS movement patterns involving flexibility and balance but worse on movement patterns associated with core strength. Investigators should consider assessing sex as a confounder in future research. Injury or surgery history did not affect overall YBT performance. It indicated differences in some FMS and YBT movement patterns but not necessarily the overall score. Therefore, evaluating FMS or YBT movement patterns rather than just overall scores in athletes with previous injury or surgery may be appropriate.
REFERENCES
- 1.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 2.Beck JL, Wildermuth BP. The female athlete's knee. Clin Sports Med. 1985;4(2):345–366. [PubMed] [Google Scholar]
- 3.Caraffa A, Cerulli G, Projetti M, Aisa G, Rizzo A. Prevention of anterior cruciate ligament injuries in soccer: a prospective controlled study of proprioceptive training. Knee Surg Sports Traumatol Arthrosc. 1996;4(1):19–21. doi: 10.1007/BF01565992. [DOI] [PubMed] [Google Scholar]
- 4.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 5.Fousekis K, Tsepis E, Vagenas G. Intrinsic risk factors of noncontact ankle sprains in soccer: a prospective study on 100 professional players. Am J Sports Med. 2012;40(8):1842–1850. doi: 10.1177/0363546512449602. [DOI] [PubMed] [Google Scholar]
- 6.Cook G. Movement: Functional Movement Systems: Screening, Assessment, and Corrective Strategies. Vol. 16. Aptos, CA: On Target Publications; 2010. pp. 28–32.pp. 79–106. [Google Scholar]
- 7.Kiesel K, Plisky PJ, Voight ML. Can serious injury in professional football be predicted by a preseason Functional Movement Screen? N Am J Sports Phys Ther. 2007;2(3):147–158. [PMC free article] [PubMed] [Google Scholar]
- 8.Chorba RS, Chorba DJ, Bouillon LE, Overmyer CA, Landis JA. Use of a functional movement screening tool to determine injury risk in female collegiate athletes. N Am J Sports Phys Ther. 2010;5(2):47–54. [PMC free article] [PubMed] [Google Scholar]
- 9.O'Connor FG, Deuster PA, Davis J, Pappas CG, Knapik JJ. Functional movement screening: predicting injuries in officer candidates. Med Sci Sports Exerc. 2011;43(12):2224–2230. doi: 10.1249/MSS.0b013e318223522d. [DOI] [PubMed] [Google Scholar]
- 10.Cho SH, Park JM, Kwon OY. Gender differences in three dimensional gait analysis data from 98 healthy Korean adults. Clin Biomech (Bristol, Avon) 2004;19(2):145–152. doi: 10.1016/j.clinbiomech.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Yamasaki M, Sasaki T, Torii M. Sex difference in the pattern of lower limb movement during treadmill walking. Eur J Appl Physiol Occup Physiol. 1991;62(2):99–103. doi: 10.1007/BF00626763. [DOI] [PubMed] [Google Scholar]
- 12.Hurd WJ, Chmielewski TL, Axe MJ, Davis I, Snyder-Mackler L. Differences in normal and perturbed walking kinematics between male and female athletes. Clin Biomech (Bristol, Avon) 2004;19(5):465–472. doi: 10.1016/j.clinbiomech.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 13.McLean SG, Walker KB, van den Bogert AJ. Effect of gender on lower extremity kinematics during rapid direction changes: an integrated analysis of three sports movements. J Sci Med Sport. 2005;8(4):411–422. doi: 10.1016/s1440-2440(05)80056-8. [DOI] [PubMed] [Google Scholar]
- 14.Joseph MF, Rahl M, Sheehan J, et al. Timing of lower extremity frontal plane motion differs between female and male athletes during a landing task. Am J Sports Med. 2011;39(7):1517–1521. doi: 10.1177/0363546510397175. [DOI] [PubMed] [Google Scholar]
- 15.Gutierrez GM, Knight CA, Swanik CB, et al. Examining neuromuscular control during landings on a supinating platform in persons with and without ankle instability. Am J Sports Med. 2012;40(1):193–201. doi: 10.1177/0363546511422323. [DOI] [PubMed] [Google Scholar]
- 16.Hung YJ, Darling WG. Shoulder position sense during passive matching and active positioning tasks in individuals with anterior shoulder instability. Phys Ther. 2012;92(4):563–573. doi: 10.2522/ptj.20110236. [DOI] [PubMed] [Google Scholar]
- 17.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schneiders AG, Davidsson Å, Hörman E, Sullivan SJ. Functional Movement Screen normative values in a young, active population. Int J Sports Phys Ther. 2011;6(2):75–82. [PMC free article] [PubMed] [Google Scholar]
- 19.Peate W, Bates G, Lunda K, Francis S, Bellamy K. Core strength: a new model for injury prediction and prevention. J Occup Med Toxicol. 2007;2:3. doi: 10.1186/1745-6673-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Plisky PJ, Gorman PP, Butler RJ, Kiesel KB, Underwood FB, Elkins B. The reliability of an instrumented device for measuring components of the Star Excursion Balance Test. N Am J Sports Phys Ther. 2009;4(2):92–99. [PMC free article] [PubMed] [Google Scholar]
- 21.Hertel J. Sensorimotor deficits with ankle sprains and chronic ankle instability. Clin Sports Med. 2008;27(3):353–370. doi: 10.1016/j.csm.2008.03.006. vii. [DOI] [PubMed] [Google Scholar]
- 22.Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36(12):911–919. doi: 10.2519/jospt.2006.2244. [DOI] [PubMed] [Google Scholar]
- 23.Butler RJ, Lehr ME, Fink ML, Kiesel KB, Plisky PJ. Dynamic balance performance and noncontact lower extremity injury in college football players: an initial study. Sports Health. 2013;5(5):417–422. doi: 10.1177/1941738113498703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steffen K, Emery CA, Romiti M, et al. High adherence to a neuromuscular injury prevention programme (FIFA 11+) improves functional balance and reduces injury risk in Canadian youth female football players: a cluster randomised trial. Br J Sports Med. 2013;47(12):794–802. doi: 10.1136/bjsports-2012-091886. [DOI] [PubMed] [Google Scholar]
- 25.Gribble PA, Hertel J. Considerations for normalizing measures of the Star Excursion Balance Test. Meas Phys Educ Exerc Sci. 2003;7(2):89–100. [Google Scholar]
- 26.Sabin MJ, Ebersole KT, Martindale AR, Price JW, Broglio SP. Balance performance in male and female collegiate basketball athletes: influence of testing surface. J Strength Cond Res. 2010;24(8):2073–2078. doi: 10.1519/JSC.0b013e3181ddae13. [DOI] [PubMed] [Google Scholar]
- 27.Gorman PP, Butler RJ, Rauh MJ, Kiesel K, Plisky PJ. Differences in dynamic balance scores in one sport versus multiple sport high school athletes. Int J Sports Phys Ther. 2012;7(2):148–153. [PMC free article] [PubMed] [Google Scholar]
- 28.Gribble PA, Robinson RH, Hertel J, Denegar CR. The effects of gender and fatigue on dynamic postural control. J Sport Rehabil. 2009;18(2):240–257. doi: 10.1123/jsr.18.2.240. [DOI] [PubMed] [Google Scholar]
- 29.Aminaka N, Gribble PA. Patellar taping, patellofemoral pain syndrome, lower extremity kinematics, and dynamic postural control. J Athl Train. 2008;43(1):21–28. doi: 10.4085/1062-6050-43.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Olmsted LC, Carcia CR, Hertel J, Shultz SJ. Efficacy of the Star Excursion Balance Tests in detecting reach deficits in subjects with chronic ankle instability. J Athl Train. 2002;37(4):501–506. [PMC free article] [PubMed] [Google Scholar]
- 31.Gribble PA, Hertel J, Denegar CR, Buckley WE. The effects of fatigue and chronic ankle instability on dynamic postural control. J Athl Train. 2004;39(4):321–329. [PMC free article] [PubMed] [Google Scholar]
- 32.Hoch MC, Staton GS, Medina McKeon JM, Mattacola CG, McKeon PO. Dorsiflexion and dynamic postural control deficits are present in those with chronic ankle instability. J Sci Med Sport. 2012;15(6):574–579. doi: 10.1016/j.jsams.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 33.Smith CA, Chimera NJ, Wright NJ, Interrater Warren M. and intrarater reliability of the Functional Movement Screen. J Strength Cond Res. 2013;27(4):982–987. doi: 10.1519/JSC.0b013e3182606df2. [DOI] [PubMed] [Google Scholar]
- 34.Y Balance Test lower quarter testing procedures. 2014 Y Balance Test Web site. http://www.ybalancetest.com/. Accessed February 14. [Google Scholar]
- 35.Y Balance Test: get certified. Y Balance Test Web site. 2014 http://www.ybalancetest.com/get-certified/. Accessed February 14. [Google Scholar]
- 36.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 37.Kiesel K, Plisky P, Butler R. Functional movement test scores improve following a standardized off-season intervention program in professional football players. Scand J Med Sci Sports. 2011;21(2):287–292. doi: 10.1111/j.1600-0838.2009.01038.x. [DOI] [PubMed] [Google Scholar]
- 38.Milosis DC, Siatras TA. Sex differences in young gymnasts' postural steadiness. Percept Mot Skills. 2012;114(1):319–328. doi: 10.2466/05.25.27.PMS.114.1.319-328. [DOI] [PubMed] [Google Scholar]
- 39.Di Stasi SL, Logerstedt D, Gardinier ES, Snyder-Mackler L. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am J Sports Med. 2013;41(6):1310–1318. doi: 10.1177/0363546513482718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chimera NJ, Castro M, Davis I, Manal K. The effect of isolated gastrocnemius contracture and gastrocnemius recession on lower extremity kinematics and kinetics during stance. Clin Biomech (Bristol, Avon) 2012;27(9):917–923. doi: 10.1016/j.clinbiomech.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 41.Lee HM, Cheng CK, Liau JJ. Correlation between proprioception, muscle strength, knee laxity, and dynamic standing balance in patients with chronic anterior cruciate ligament deficiency. Knee. 2009;16(5):387–391. doi: 10.1016/j.knee.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 42.Leetun DT, Ireland ML, Willson JD, Ballantyne BT, Davis IM. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc. 2004;36(6):926–934. doi: 10.1249/01.mss.0000128145.75199.c3. [DOI] [PubMed] [Google Scholar]
- 43.Kazman JB, Galecki JM, Lisman P, Deuster PA. O'Connor FG. Factor structure of the Functional Movement Screen in Marine officer candidates. J Strength Cond Res. 2014;28(3):672–678. doi: 10.1519/JSC.0b013e3182a6dd83. [DOI] [PubMed] [Google Scholar]
- 44.Bressel E, Yonker JC, Kras J, Heath EM. Comparison of static and dynamic balance in female collegiate soccer, basketball, and gymnastics athletes. J Athl Train. 2007;42(1):42–46. [PMC free article] [PubMed] [Google Scholar]
- 45.Thorpe JL, Ebersole KT. Unilateral balance performance in female collegiate soccer athletes. J Strength Cond Res. 2008;22(5):1429–1433. doi: 10.1519/JSC.0b013e31818202db. [DOI] [PubMed] [Google Scholar]
- 46.McKay GD, Goldie PA, Payne WR, Oakes BW. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35(2):103–108. doi: 10.1136/bjsm.35.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McHugh MP, Tyler TF, Tetro DT, Mullaney MJ, Nicholas SJ. Risk factors for noncontact ankle sprains in high school athletes: the role of hip strength and balance ability. Am J Sports Med. 2006;34(3):464–470. doi: 10.1177/0363546505280427. [DOI] [PubMed] [Google Scholar]
- 48.Inani SB, Selkar SP. Effect of core stabilization exercises versus conventional exercises on pain and functional status in patients with non-specific low back pain: a randomized clinical trial. J Back Musculoskelet Rehabil. 2013;26(1):37–43. doi: 10.3233/BMR-2012-0348. [DOI] [PubMed] [Google Scholar]
- 49.Macklin K, Healy A, Chockalingam N. The effect of calf muscle stretching exercises on ankle joint dorsiflexion and dynamic foot pressures, force and related temporal parameters. Foot (Edinb) 2012;22(1):10–17. doi: 10.1016/j.foot.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 50.Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med. 2007;35(7):1123–1130. doi: 10.1177/0363546507301585. [DOI] [PubMed] [Google Scholar]